Back to Journals » International Journal of Women's Health » Volume 15
Knowledge, Attitude, and Practice Regarding Supplemental Iron and Folic Acid Amongst Women Delivering in Edaga-Hamus Community Hospital: A Cross-Sectional Study in Asmara, Eritrea
Authors Tsegai MB , Berhe AH , Tesfaezgi SB, Weldemariam DG , Petros KT, Weldetinsae HB, Tesfamariam EH
Received 4 May 2023
Accepted for publication 30 September 2023
Published 20 October 2023 Volume 2023:15 Pages 1593—1609
DOI https://doi.org/10.2147/IJWH.S419813
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Everett Magann
Meron Berhe Tsegai,1 Abiel Habtom Berhe,2 Semhar Berhane Tesfaezgi,3 Dawit G Weldemariam,4 Kifleyesus Tedla Petros,5 Hana Bereket Weldetinsae,3 Eyasu H Tesfamariam6
1Planning Unit, Ministry of Health, Zoba Maekel Branch, Asmara, Eritrea; 2Department of Pharmacy, Edaga-Hamus Community Hospital, Asmara, Eritrea; 3Maternal & Child Health Unit, Edaga-Hamus Community Hospital, Asmara, Eritrea; 4Department of Pharmacy, Hazhaz Zonal Referral Hospital, Asmara, Eritrea; 5Department of Obstetrics and Gynaecology, Edaga-Hamus Community Hospital, Asmara, Eritrea; 6Department of Statistics, Biostatistics and Epidemiology, College of Science, Eritrean Institute of Technology, Mai-Nefhi, Eritrea
Correspondence: Meron Berhe Tsegai, Tel +291 7573197, Email [email protected]
Purpose: In Eritrea, every pregnant woman is provided with a supplemental iron and folic acid (IFA) tablet starting from the first antenatal visit throughout the end of pregnancy. In Zoba Maekel, two-third of first antenatal visits have been at either the second or third trimesters. This practice could limit pregnant women’s timely access to the nutritional supplement and its benefits. Therefore, this study aims to identify the knowledge, attitude, and practice of women delivering in Edaga-Hamus Community Hospital towards the supplemental IFA tablet.
Materials and Methods: A health facility-based cross-sectional study was carried out on 360 women delivering in Edaga-Hamus Community Hospital. Data were collected using a structured questionnaire through systematic sampling. Associated factors were identified using bivariate and multivariable logistic regression. Associations with a p-value < 0.05 were considered significant.
Results: Mothers with higher level of IFA knowledge and attitude held 52.8% and 65.4%, respectively. Health care workers were predominantly (92.3%) the main source for IFA information. Possible IFA side-effects were known by 64.8% of the mothers, even though only 28.2% knew reduction of side effects if taken with food. Almost all (96.1% and 97.0% respectively) believed IFA is beneficial and can prevent anemia. Only 27.9% had appropriately practiced taking the IFA supplement. Mothers who visited for antenatal care more than 8 times (AOR: 4.02, 95% CI: 1.45, 11.09) and 5 to 8 times (AOR: 2.87, 95% CI: 1.52, 5.41) had increased odds of appropriate IFA practice compared to those who visited for 1 to 4 times. Women who had planned pregnancies (AOR: 2.03, 95% CI: 1.01, 4.10) were more likely to have appropriate practice than their counterparts who had unplanned pregnancies.
Conclusion: The study indicated that further strategies need to be implemented to increase the current level of knowledge, attitude, and practice of IFA.
Keywords: iron and folic acid, knowledge, attitude, practice
Introduction
Adverse pregnancy outcomes are among the major public health concerns, especially in low- and middle-income countries.1,2 Currently, the most common cause of adverse pregnancy outcomes is maternal anemia which affects an estimated 41.8% of all pregnancies globally.3 Anemia amongst pregnant women is defined as a hemoglobin level of <11g/dl at sea level,4 and occurs when the number and oxygen carrying capacity of red blood cells subsides the body’s physiologic oxygen necessities. The major cause of anemia among pregnant women is iron deficient diet,5 succeeded by megaloblastic anemia due to folate deficiency,6 even though other causes can contribute to it. Maternal anemia increases the number of children born with reduced birth weight and heightens the risk of maternal mortality.7 Pregnant women need iron supplementation because of higher fetal demand, rapid tissue growth and increased cell mass.
The amount of iron required during pregnancy also depends on their iron store. Hence, most pregnant women need iron supplementation.8 It has been noted that iron supplementation during pregnancy has been shown to reduce maternal anemia by up to 70%, abating its consequent harm to both the baby and the mother.9 Therefore, every pregnant woman is recommended to take a supplemental tablet containing a combination of 30 mg or 60 mg of elemental iron and 400 µg (0.4 mg) of folic acid orally on a daily basis. This supplement is mainly recommended for the prevention of maternal anemia, puerperal sepsis, low birth weight, and preterm birth.10 Although according to Cochrane systematic review analysis, the use of intermittent iron supplementation has shown similar maternal and infant outcomes and fewer side effects,8 there are reports that non-compliance with iron-folic acid supplementation is also a considerable problem that could have a negative impact on the health of both the mother and the fetus.2
In Eritrea, Antenatal care (ANC) services are provided so as to prevent, detect, and manage problems and factors that adversely affect the health of a mother and infant. One of its major objectives is to lower the occurrence of iron and folic acid deficiency in pregnancy so as to prevent occurrence of anemia. According to the Eritrean population and health survey, in 2010, 23.8% of the overall women who participated in the study reported to experience anemia during their earlier pregnancies, and this existed among 25.7% participants from Zoba Maekel. These results were based on reports of anemia in their latest pregnancy by women aged 15–49 with live births in the 5 years preceding the survey. For the prevention of anemia and other purposes, all pregnant women in the country are required to have at least eight antenatal visits and take one dose of IFA tablet daily throughout their pregnancies. Therefore, during the first visit, optimally in the first trimester, a mother is provided with daily iron and folic acid supplements containing 30 mg to 60 mg of elemental iron (or 300mg of ferrous sulphate) and 400 µg (0.4 mg) of folic acid for the prevention of maternal anemia, puerperal sepsis, low birth weight, and preterm birth.
Knowledge about the importance of IFA supplementation and women’s attitude can contribute to its early use and overall practice. This is not only important in improving the health status of the baby but also that of the mother.11 In Eritrea, all pregnant women visiting for ANC service receive health education and IFA tablets starting on their first visit. According to the Eritrean Health Management Information System (HMIS) on average, in the last 5 years, 66% of all women visiting for ANC service in Zoba Maekel arrived in either their second or third trimester. This could hinder their timely access to the WHO-recommended nutritional supplement and could potentially lead to anemia and an increased probability of adverse pregnancy outcomes, unless they have preferred to getting it from other sources other than from ANC service.
To the best knowledge of the authors, published studies regarding the possible gaps in the practicality of timely and appropriate use of IFA supplementation have not been conducted in Eritrea or Zoba Maekel. Therefore, this study aims to assess the level of knowledge, attitude, and practice of women delivering in Edaga-Hamus Community Hospital on the supplemental IFA tablet.
Materials and Methods
Study Area and Population
The study was carried out on women delivering in EHCH, a government-owned health facility in Asmara. The facility is located in the Edaga-Hamus subzone and is accessible for pregnant women in the Eritrean capital and from the Maekel region. Following its recent enhancement, in addition to its suitable location, the hospital had had the highest rate of delivery in the Maekel region contributing an average delivery rate of 264 births per month in 2020; covering 61% of all deliveries by Maekel region in that year.
Study Design and Sampling
A hospital-based quantitative cross-sectional study was conducted from 1st September to 31st December 2021. The sample size was determined using the single population proportion formula with finite population correction, applying 95% confidence interval and a 5% margin of error. As there was no previous data concerning the KAP of women towards the use of IFA supplementation, the expected proportion while computing the sample size was taken as 0.5. Finally, considering a 5% non-response, the final sample size was 360 women. A linear systematic sampling technique was implemented for the selection of study participants, where the sampling interval was calculated using 2020 (from September up to December) delivery rate of EHCH, yielding a final value of 3 (ie, 1096/360). Therefore, every third of all mothers who delivered from 1st September to 31st December of 2021 were taken as study participants.
Data Collection
A self-developed structured questionnaire, customized by the primary researchers and translated to the local language Tigrigna, was implemented to assess the level of KAP of supplemental IFA tablets. The questionnaire captured information for demography, obstetric history, ANC visit and access history, level of knowledge and attitude of anemia, KAP of IFA, pregnancy diet history, and IFA side effect history. Mothers who delivered at the delivery wards of EHCH were assessed using the standardized questionnaire. The final questionnaire was designed and formatted for the open data kit (ODK) mobile application (app), in both English and Tigrigna, and data collection was conducted using the app. Data collectors were familirized with the perpuse of the study and trained on how to use the ODK mobile app during data collection. A ten-day preliminary data collection practice was conducted to test the functionality of the questionnaire and the mobile app.
Data Analysis
After the actual data collection, data were exported from the ODK app and converted into an excel file and imported to SPSS version 22 software for cleaning and analysis. Descriptive statistics for socio-demographic characteristics, obstetric history, and characteristics related to IFA supplementation were presented using frequency and cross-tabulations. Bivariate and multivariable analyses were implemented to assess the association between dependent and independent variables. In the first step, variables were selected based on review of literature, which included information on i. demographic background (age, address, educational level, occupation, marital status, and spouse’s education), ii. previous pregnancy history related variables (if had been pregnant before or not, history of previous pregnancy ANC visit, number of previous pregnancies, number of children, history of abortion or stillbirth, number of abortion and stillbirth), iii. current pregnancy related variables (status of planned pregnancy, number of current ANC visits, starting time of first ANC visit, distance of ANC service from home, occurrence of IFA side effects), iv. anemia knowledge focusing variables (knowing what normal Hb level is, knowing current Hb level, hearing about anemia, hearing about folic acid), v. diet-related variables (relative amount of food taken during pregnancy, regularly taking vitamin C rich foods, habit of drinking coffee, habit of drinking tea, habit of taking tea or coffee while eating, following non-vegetarian diet, including vegetables in meal, number of meals per day), vi. side effect of IFA related variables (occurrence of IFA side effects before pregnancy, occurrence of IFA side effects after pregnancy), and vii. variables assessing IFA knowledge, IFA attitude, anemia knowledge, and anemia attitude, were fitted into a bivariate logistic regression model at a p-value less than or equal to 0.1. All variables with p-value less than 0.1 in the first step and the dependent variable were then fitted in the multivariable model. At multivariable level, p-values less or equal to 0.05 were considered significant. Adjusted odds ratios with a 95% confidence interval (CI) were used to present the final result.
Operational Definitions and Variable Measurements
Knowledge of IFA Supplementation
The level of IFA tablet knowledge was assessed based on eleven questions, including yes/no, multiple-choice, and multi-selection questions. The questions covered topics related to the need for an IFA tablet, its benefit, when should it be started and stopped, the recommended dose and other related questions. Every right answer scored was given one point and respondents’ final score was assessed based on the percentage of right answers scored out of the total possible highest score. Finally, based on the overall median value (MD = 49.8), respondents were classified as having adequate or inadequate knowledge.
Attitude Toward IFA Supplementation
The level of attitude on the IFA tablet was assessed based on eight questions, comprising choices measuring the degree of agreement starting from strongly agree, to agree, neutral, disagree, and strongly disagree. The questions covered topics related to benefit of the IFA tablet; the importance of starting early, taking it on a daily basis and throughout pregnancy, if they think it is harmful and can prevent anemia; and other related questions. Every question was scored based on the Likert scale and respondents’ final score was assessed based on the percentage scored out of the total possible highest score. Finally, using the overall median value (MD = 77.0) as a cut-off point, respondents were classified as having favorable or unfavorable attitude.
Practice of IFA Supplementation
To assess the appropriateness of IFA practice, the study implemented the self-report method and categorized responders based on three items. The three items were: (i) start taking IFA tablet from the first trimester of pregnancy, (ii) taking one dose of 30–60 mg iron and 400 µg folic acid tablet, (iii) taking the tablet on a daily basis for the recommended period of time. All mothers who responded positively to the above-mentioned items were considered to have appropriate practice.
Knowledge of Anemia
Anemia knowledge assessment implemented ten yes/no, multiple-choice, and multi-selection questions; covering topics about the cause, symptoms, health effects and prevention of anemia. Every correct answer was given one point and the final score was assessed based on the percentage scored out of the highest possible score. Respondents were categorized based on the overall median value (MD = 53.0), as having adequate or inadequate knowledge.
Attitude of Anemia
The attitude of anemia was assessed using eight questions, based on choices measuring the degree of agreement starting from strongly agree, to agree, neutral, disagree, and strongly disagree. Questions implemented were about the importance of being aware of anemia during pregnancy, the seriousness of anemia, the relation between pregnancy and anemia, the possibility of treating anemia and others. Every question was scored based on the Likert scale and respondents’ final score was assessed using the percentage scored out of the total possible highest score. Finally, using the overall median value (MD = 63.6), respondents were classified as having favorable or unfavorable attitude.
Inclusion and Exclusion Criteria
All women who delivered at EHCH from 1st September to 31st December 2021 were eligible to participate in the study. Mothers who refused to participate, mentally impaired, referred mothers or severely ill mothers (critical mothers) were excluded from the sampling frame.
Ethical Considerations
Ethical clearance has been obtained from the health research proposal review and ethical committees of the Eritrean Ministry of Health. On starting the actual data collection, according to the declaration of Helsinki,12 an informed consent was verbally obtained from all study participants, after explaining the objectives, methods and benefits of the study. The subjects were informed on their right to abstain from participating, or withdrawing their consent at any time and only those who gave their consent for participation were included in the study. During data collection, participants were questioned privately and all questionnaires were filled anonymously using number coding to secure individual information confidentiality.
Results
Socio-Demographic Characteristics of Responders
Within the study period, a total of 358 mothers who delivered in the EHCH delivery ward consented to participate in the study; giving a response rate of 99.4%. Two-thirds (65.9%) of the study participants were within the age group of 25–34, followed by 75 (20.9%) and 47 (13.1%) for age groups 18–24 and 35–42 years, respectively. Complete socio-demographic profile is shown in Table 1.
 |
Table 1 Socio-Demographic Characteristics of Mothers Delivering in EHCH |
Obstetric History of Respondents
Table 2 shows the obstetric history of respondents. Of the 358 study participants, 285 (79.6%) were multigravida. Out of these multigravida mothers, 239 (83.9%) had been pregnant at least twice up to five times and 280 (98.2%) had had an ANC visit in their previous pregnancies.
 |
Table 2 Obstetric History of Mothers Delivering in EHCH |
Factors Related to IFA Supplementation
Among the study participants, only 24 (6.7%) had their first ANC visit during the first month of their pregnancy, 88 (24.6%) started during their second month and 99 (27.7%) visited during the third month. The time taken to reach their ANC-providing health facility was less than or equal to 30 minutes for 323 (90.2%) and more than half (58.7%) of the participants visited for ANC service five up to eight times. Factors on side effects, knowledge, attitude and practice of IFA supplementation are presented in Table 3
 |
Table 3 Factors Related to IFA Supplementation Among Mothers Delivering in EHCH |
IFA Knowledge and Associated Factors
Out of the 337 participants who had ever heard about IFA, the majority (93.3%) knew that all pregnant women needed to take IFA supplement, should take it in addition to a healthy diet (78.8%), when to start the tablet (63.4%), how often to take it (89.9%), what dose to take (84.6%), possible side-effects (64.8%), benefits of the tablet (88.8%), and where to get the tablet (92.7%). Of the eleven asked questions, the ones with the lowest correct answering rate and answers related to anemia questions is seen in Table 4.
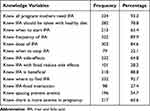 |
Table 4 Proportion of Mothers with Correct Response to IFA Knowledge Questions |
The Source of information for the mothers was mostly from health care workers (92.3%), followed by family and friends (55.7%), mass media (36.9%), and experience from previous pregnancies (34.2%). Other sources of information were, nutritionists, the internet, and others (Figure 1).
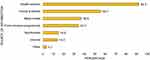 |
Figure 1 IFA knowledge source of information among Mothers Delivering in EHCH. |
Factors affecting knowledge of IFA supplements were identified using binary logistic regression. Then those factors with p-value <0.1 at bivariate analysis were retained for multivariable analysis.
At bivariate level, age (p=0.079), education (p=0.001), occupation (p=0.026), knowledge on current Hb level (p=0.072), planned pregnancy (p= 0.05), whether they heard about anemia (p<0.001), whether they heard about folic acid (p<0.001), knowledge of normal Hb level (p=0.009), presence of IFA side effects (p=0.086), anemia knowledge (p<0.001), anemia attitude (p<0.001), and history of abortion (p=0.066) had p-value <0.1.
At multivariable level, only those who heard about anemia (p=0.03) and those who had adequate anemia knowledge (p<0.001) were significant determinants of knowledge towards IFA supplementation. The odds of adequate knowledge of IFA were 3.44 times higher (AOR: 3.44, 95% CI: 1.13, 10.52) among pregnant women who heard about anemia as compared to those who had never heard. Likewise, the odds among those women who had adequate anemia knowledge was 4.15 (AOR: 4.15, 95% CI: 1.99, 8.64) times more than those who had inadequate anemia knowledge (Table 5).
 |
Table 5 Multivariate Logistic Analysis of Factors Influencing Knowledge of IFA Supplement Among Mothers Delivering in EHCH |
IFA Attitude and Associated Factors
From the questions measuring attitude, most participants agreed that visiting ANC (99.7%) and taking IFA (97.0%) is beneficial, and accepted the importance of taking the tablet early (89.6%), on a daily basis (91.4%), and throughout pregnancy (78.6%). Comparably, low portion of participants thought that coffee, tea, and milk (62.1%, 58%, and 23% in that order) can interfere with iron absorption (Table 6).
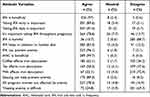 |
Table 6 Attitude of IFA and Anemia Among Mothers Delivering in EHCH |
In assessing the association between attitude scores and possible contributing factors, variables measuring occupation (p=0.005), knowledge of current Hb level (p=0.086), whether they heard about anemia (p<0.001), whether they heard about folic acid (p=0.009), Knowledge of normal Hb level (p=0.014), diet during pregnancy (p=0.06), non-vegetarian diet (p=0.003), inclusion of vegetables in meals (p=0.046), symptoms similar to IFA side effects prior starting IFA (p=0.004), IFA knowledge (p<0.001), anemia knowledge (p<0.001), anemia attitude (p<0.001), and history of abortion (p=0.066) were found to have p-value less than 0.1 at bivariate-level analysis. However, only women who had heard about anemia had odds of having favorable attitude score 3.65 (AOR: 3.65, 95% CI: 1.45, 9.18) times higher compared to those never heard, at multivariable level (Table 7).
 |
Table 7 Multivariate Logistic Analysis of Factors Influencing the Attitude of IFA Supplement Among Mothers Delivering in EHCH |
IFA Practice and Associated Factors
Out of all the mothers who delivered at EHCH, around three quarters (71.9%) had reported in taking the tablet regularly and at the prescribed dosage (75.3%), whereas only one-third (36.8%) had reported starting it at the proper time and almost ten percent (12.4%) stopped taking it at the right time. Participants dietary practice habits are shown in Table 8.
 |
Table 8 Percentage of Women Who Responded “Yes” to IFA Utilization and Foods Taken During Pregnancy Questions |
From the mothers who had side effects, majority (45%) had heartburn followed by nausea (25.9%) and vomiting (18.7%). Mal-digestion (7.6%) and gastrointestinal irritation (2.9%) were the side effects with the lowest occurrence (Figure 2).
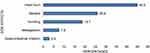 |
Figure 2 Types of Side-effects among Mothers Delivering EHCH. |
The most frequent reason respondents gave for starting time of their IFA supplement was because it was provided to them at the start of their ANC visit (71.6%) (Figure 3).
 |
Figure 3 Reason for Initiation Time of IFA among Mothers Delivering EHCH. |
Bivariate analysis for factors affecting appropriate practice of IFA showed patient’s characteristics such as age (p=0.10), occupation (p=0.008), being the first pregnancy (p= 0.001), number of current ANC visit (p<0.001), planned pregnancy (p= 0.012), knowledge of normal Hb level (p=0.09), whether they heard about anemia (p=0.027), whether they heard about folic acid (p=0.043), number of meals per day (p=0.074), drinking coffee (p=0.008), taking vitamin C reach foods (p=0.05), non-vegetarian diet (p=0.001), and attitude on IFA tablet (p=0.018) to have p-value less than 0.1.
At multivariable level, only number of current ANC visits (p=0.002), planned pregnancy (p=0.049), and depending on a non-vegetarian diet (p=0.029) were significant determinants of IFA supplement practice. The odds of appropriate IFA practice among pregnant women who visited more than 8 times and 5 to 8 times, respectively, were 4.02 (AOR: 4.02, 95% CI: 1.45, 11.09) and 2.87 (AOR: 2.87, 95% CI: 1.52, 5.41) times more compared to those who visited 1 to 4 times. The odds of appropriate practice among women who had planned pregnancy was 2.03 (AOR: 2.03, 95% CI: 1.01, 4.10) times more than those who had unplanned pregnancy. Moreover, the odds of appropriate practice among those mothers who had a non-vegetarian diet was 1.80 (AOR: 1.80, 95% CI: 1.06, 3.06) times more than those who mainly depended on a vegetarian diet (Table 9).
 |
Table 9 Multivariate Logistic Analysis of Factors Influencing Practice of IFA Supplement Among Mothers Delivering in EHCH |
Discussion
The study aimed to assess the KAP of women towards the benefits of supplemental IFA. The finding of this study showed that there is still work needed to be done to ensure an adequate level of knowledge, favorable attitude, and appropriate practice of the supplement.
In Eritrea, an educational program is provided for all attending mothers at the start of every ANC session. Accordingly, majority (ie, 94.1% and 81.6%) of the participants in this study had at least heard about IFA and anemia. However, the required adequate IFA and anemia knowledge scores were only achieved by 52.8% and 43.6% of the respondents, respectively. This could have happened as these respondents may have attended an educational session, but the session either failed to emphasize the necessity of the supplement to capture their attention, or the environment was unsuitable for information transmission at the time. Having adequate knowledge of IFA and anemia among women of child-bearing ages would be influential for their overall practice of taking the IFA supplement. As studies have shown, the need of educating women is not overstated, as it enhances the likelihood of having better maternal knowledge, practice and positive behavioral changes.13–15 The above mentioned findings of this study are in line with other studies, where 67.3% and 87.6% of the participants heard of IFA and anemia whilst only 40.9% and 50.4% had adequate knowledge scores, respectively.16,17
As findings of this study indicated, almost two-thirds of the respondents knew at least one side-effect of IFA, which is encouraging as one of the main reasons for noncompliance is out of fear of side effects.15,17,18 Even though respondents to this survey frequently experienced IFA adverse effects, just 28.2% were aware that taking the tablet with food might lessen side effects. Knowledge about how to mitigate the possible side-effects would likely give mothers confidence and encourage them to be more compliant, thus should be engrossed during education programs. Additionally, 78.8% of the respondents also stressed that there is a need for IFA supplementation with a healthy diet for all pregnant women. Understanding the importance of the supplement regardless of their diet could be an important contributor to the practice of taking it. This is greater than the finding of a research conducted in India, where 32.6% of respondents said iron supplements should be used on a daily basis despite eating a balanced diet.19
In this study, almost all of the participants could reach their ANC service within 30 minutes, and were also aware of the need for IFA during pregnancy, its benefits, where to find it and the time of initiation of the tablet, nevertheless, only 36% started taking it at the first trimester. Great portion (71.6%) of those who responded said they began taking the medication as a result of receiving it at their first ANC visit. This indicates the need of educational programs to emphasize the importance of the supplementation, especially starting during the early weeks of pregnancy, to fully grasp its nutritional benefits. Furthermore, as shown in this study, planned pregnancies made up 77.9% of all pregnancies, hence the currently ongoing establishment of preconception care in the country is also expected to contribute to the early initiation of the tablet.
The main source of IFA information was health care professionals, similar to findings in Kenya,3 Saudi Arabia,20 and the Philippines.21 Although health care providers are one of the main sources of information, additional sources like brochures and community health workers were also effectively used in other settings.3,16 In this study, more than 95% of the participants could read and write, therefore considering additional means of information dissemination such as pamphlets, smartphone applications, and other approachable ways that can serve as in-pocket references might be a useful strategy to boost maternal knowledge. This might be more efficient because health professionals can be too busy to provide specific information. However, given that healthcare professionals are the primary source of information in our findings, it is crucial to guarantee that all ANC visiting mothers participate in the education program that begins each ANC session. Additionally, it is important to keep an eye on the topics that education programs must cover to ensure that sufficient and up-to-date knowledge is conveyed. The quality of the material and the manner in which it is transferred may be improved by improving the knowledge and interpersonal abilities of health education providers through ongoing training or refreshers.
In the current study, two-third of the respondents were having a favorable attitude to IFA supplementation and anemia. Almost all agreed that IFA supplementation can prevent anemia and is beneficial for the health of the mother and fetus. Likewise, most of the respondents believe that ANC is beneficial. The majority of the respondents believed IFA supplementation should be taken despite having a healthy diet. In a comparable study, the respondents were having a favorable attitude toward ANC, the benefits of IFA, and a healthy diet.19 On the other hand, over one-quarter of the respondents think that treatment of anemia is difficult. Furthermore, despite the direct correlation of IFA’s lack of absorption with drinks like tea, coffee and milk, most respondents had no belief in the fact. As sufficient IFA and anemia knowledge was found to be significantly associated with a favorable attitude,13 individualized counselling of mothers can address concerns and improve pregnant women’s attitude through discussions and clarifications.
The overall usage of IFA among the majority of the respondents was not up to the required level. Even though 71.5% took it regularly, only one-fourth of the participants followed the overall appropriate IFA practice. This was due to the fact that these responders, despite taking their supplement regularly and at the proper dosage, did not begin taking it within the needed pregnancy period. Findings in another study revealed that 74.36% of the respondents had taken IFA regularly.19 Several studies done in different regions of Ethiopia showed that 40.9%,22 60.1%23 and 63.6%17 of the respondents were compliant with their IFA supplementation. In a similar study in Kenya, the level of compliance was found to be 32.7%.24 According to the above studies, medical advice, adequate knowledge of IFA and educational background were the predictors of IFA supplementation compliance; however, the overall practice level was not assessed in these studies.17,22,23 Other factors such as forgetfulness, fear of side effects, fear of increased baby size, frustration from many tablets and failure to get the adequate supplement from a health facility were also reported as reasons for noncompliance.25–27 The current study further highlighted the increased number of ANC visits and having planned pregnancy as significant associates with appropriate practice. Regular ANC follow-ups remain the key factor to curb the ongoing inappropriate practice of IFA supplementation. Results from studies conducted in Ethiopia, Egypt, and India also showed a strong relationship between compliance with IFA supplementation and the number of ANC follow-ups.27–30 Similarly, delayed initiation of ANC visit was found to be one of the factors that resulted in poor adherence of IFA.15,27,31,32 As increase in the number of ANC visits was not associated with adequate knowledge score in this study, the outcome might be explained by improved accessibility to the supplement concurrent to increase in number of ANC visits. Therefore, improving mothers’ knowledge so as to increase the conscious usage of the supplement remains a problem on hand.
The nutritional habits of the participants in the current study were positive in some ways, as 90.5% claimed eating foods high in vitamin C and 74% were including vegetables in their meals. Furthermore, 46.1% regularly depended on a non-vegetarian diet while an alarmingly 57.3% were taking tea or coffee during or shortly after eating. Including vegetables and animal products in the meal could contribute to attaining iron and folate, as vitamin C-rich foods can also aid in the absorption of iron. In contrary, drinking coffee or tea would lower iron absorption in addition to the heightened demand for the mineral during pregnancy.33 In this study, only 27.4% knew iron absorption can be affected if taken with coffee, tea, or milk. This demonstrates that educating mothers about meals and beverages that interfere with iron absorption may be a crucial step in preventing iron deficiency anemia during pregnancy. In a related study, only 33.2% of participants were aware that tea and coffee can impact how well iron is absorbed.19
The study’s anticipated drawbacks include the fact that it was conducted in a health institution that primarily served Asmara’s residents, and hence generalization is restricted within this area. Due to the study’s heavy reliance on verbal recollections from the participants, the findings were prone to recall bias and subjectivity.
Conclusion
The level of knowledge and the overall practice of IFA supplementation was low in the study, while responders’ level of attitude was relatively higher. Expanding initiatives to further enhance understanding of IFA among women could enhance the level of IFA knowledge among pregnant women. Health education should be provided through varying means. Health educators should be provided with updated information and ways to improve their communication skills. Hospital-based education should include topics related to the proper use, possible side effects and ways to alleviate them. In addition to the hospital-based education, other sources of information that can serve as an in-pocket source of reference, like brochures or mobile apps, should be considered. In addition, information about anemia should also be properly included during the education programs. The study findings further indicated that increasing the number of pregnant women’s antenatal care visits and working on improving family planning practices could have substantial effect in improving the practice of iron and folic acid supplement.
Abbreviations
ANC, Antenatal care; AOR, Adjusted Odds Ratio; App, Application; CI, Confidence Interval; COR, Crude Odds Ratio; DMHS, Demographic and Health Surveys; DNA, Deoxyribonucleic acid; EHCH, Edaga-Hamus Community Hospital; Hb, Hemoglobin; HMIS, Health Management Information System; IFA, Iron and Folic Acid; KAP, Knowledge, Attitude, and Practice; ODK, Open Data Kit; SPSS, Statistical Package for Social Science; WHO, World Health Organization.
Acknowledgments
Our sincere appreciation goes to the Ministry of Health Zoba Maekel branch, Zonal reproductive health focal person Mr. Huruy Weldemichael and all members of Edaga-Hamus Community Hospital, and all participants for their vital contribution.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li D, Huang L, Yang W, et al. Knowledge, attitude and practice level of women at the periconceptional period: a cross-sectional study in Shaanxi China. BMC Pregnancy Childbirth. 2019;19(1):1–12. doi:10.1186/s12884-019-2481-6
2. Sendeku FW, Azeze GG, Fenta SL. Adherence to iron-folic acid supplementation among pregnant women in Ethiopia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2020;20(1):1–9. doi:10.1186/s12884-020-2835-0
3. WHO/CDC. Worldwide Prevalence of Anaemia 1993–2005. WHO Global Database on Anaemia. Geneva: WHO/CDC; 2008.
4. World Health Organization. Nutrition Landscape Information System (NLIS) Country Profile Indicators: Interpretation Guide. World Health Organization; 2019.
5. World Health Organization. Assessing the Iron Status of Populations: Report of a Joint World Health Organization/Centers for Disease Control and Prevention Technical Consultation on the Assessment of Iron Status at the Population Level.
6. Moussa HN, Hosseini Nasab S, Haidar ZA, Blackwell SC, Sibai BM. Folic acid supplementation: what is new? Fetal, obstetric, long-term benefits and risks. Future Sci OA. 2016;2(2). doi:10.4155/fsoa-2015-0015
7. United Nations System Standing Committee on Nutrition Secretariat. Progress in Nutrition: Sixth Report on the World Nutrition Situation. Geneva: United Nations System Standing Committee on Nutrition Secretariat; 2010.
8. Peña‐Rosas JP, De‐Regil LM, Malave HG, Flores‐Urrutia MC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015. doi:10.1002/14651858.CD009997.pub2
9. World Health Organization. The Global Prevalence of Anaemia in 2011. Geneva: World Health Organization; 2015.
10. World Health Organization. WHO Antenatal Care Recommendations for a Positive Pregnancy Experience: Nutritional Interventions Update: Multiple Micronutrient Supplements During Pregnancy. World Health Organization; 2020.
11. Wald NJ, Law MR, Morris JK, Wald DS. Quantifying the effect of folic acid. Lancet. 2001;358(9298):2069–2073. doi:10.1016/S0140-6736(01)07104-5
12. World Medical Association. Declaration of Helsinki. World Medical Association; 2004.
13. Kamau M, Mirie W, Kimani S, Mugoya I, Ghose B. Effect of community based health education on knowledge and attitude towards iron and folic acid supplementation among pregnant women in Kiambu County, Kenya: a quasi experimental study. PLoS One. 2019;14(11):e0224361. doi:10.1371/journal.pone.0224361
14. Wu DY, Brat G, Milla G, Kim J. Knowledge and use of folic acid for prevention of birth defects amongst Honduran women. Reprod Toxicol. 2007;23(4):600–606. doi:10.1016/j.reprotox.2007.01.010
15. Desta M, Kassie B, Chanie H, et al. Adherence of iron and folic acid supplementation and determinants among pregnant women in Ethiopia: a systematic review and meta-analysis. Reprod Health. 2019;16(1):1–14. doi:10.1186/s12978-019-0848-9
16. Kamau MW, Mirie W, Kimani ST. Maternal knowledge on iron and folic acid supplementation and associated factors among pregnant women in a rural county in Kenya. Int J Afr Nurs Sci. 2019;10:74–80. doi:10.1016/j.ijans.2019.01.005
17. Nasir BB, Fentie AM, Adisu MK, Petry CJ. Adherence to iron and folic acid supplementation and prevalence of anemia among pregnant women attending antenatal care clinic at Tikur Anbessa Specialized Hospital, Ethiopia. PLoS One. 2020;15(5):e0232625. doi:10.1371/journal.pone.0232625
18. Lavanya P, Jayalakshmy R, Rajaa S, Mahalakshmy T. Adherence to iron and folic acid supplementation among antenatal mothers attending a tertiary care center, Puducherry: a mixed-methods study. J Fam Med Prim Care. 2020;9(10):5205. doi:10.4103/jfmpc.jfmpc_721_20
19. Nivedita K, Shanthini F. Knowledge, attitude and practices of pregnant women regarding anemia, iron rich diet and iron supplements and its impact on their hemoglobin levels. Int J Reprod Contracept Obstet Gynecol. 2016;5(2):425–431.
20. Al-Akhfash AA, Abdulla AM, Osman AM, Abdulgafar JI, Almesned AA. Maternal knowledge and use of folic acid among Saudi females. Saudi med j. 2013;34(11):1173–1178.
21. Yamashita T, Roces RED, Ladines-Llave C, et al. Maternal knowledge associated with the prevalence of iron and folic acid supplementation among pregnant women in Muntinlupa, Philippines: a cross-sectional study. Patient Prefer Adherence. 2021;15:501. doi:10.2147/PPA.S291939
22. Gebremichael TG, Welesamuel TG, Gebremedhin S. Adherence to iron-folic acid supplement and associated factors among antenatal care attending pregnant mothers in governmental health institutions of Adwa town, Tigray, Ethiopia: cross-sectional study. PLoS One. 2020;15(1):e0227090. doi:10.1371/journal.pone.0227090
23. Gebreamlak B, Dadi AF, Atnafu A, Räisänen SH. High adherence to iron/folic acid supplementation during pregnancy time among antenatal and postnatal care attendant mothers in Governmental Health Centers in Akaki Kality Sub City, Addis Ababa, Ethiopia: hierarchical negative binomial poisson regression. PLoS One. 2017;12(1):e0169415. doi:10.1371/journal.pone.0169415
24. Kamau MW, Mirie W, Kimani S. Compliance with Iron and folic acid supplementation (IFAS) and associated factors among pregnant women: results from a cross-sectional study in Kiambu County, Kenya. BMC Public Health. 2018;18(1):1–10. doi:10.1186/s12889-018-5437-2
25. Molla T, Guadu T, Muhammad EA, Hunegnaw MT. Factors associated with adherence to iron folate supplementation among pregnant women in West Dembia district, northwest Ethiopia: a cross sectional study. BMC Res Notes. 2019;12(1):1–6. doi:10.1186/s13104-019-4045-2
26. Assefa H, Abebe SM, Sisay M. Magnitude and factors associated with adherence to Iron and folic acid supplementation among pregnant women in Aykel town, Northwest Ethiopia. BMC Pregnancy Childbirth. 2019;19(1):1–8. doi:10.1186/s12884-019-2422-4
27. Gebre A, Mulugeta A, Etana B. Assessment of factors associated with adherence to iron-folic acid supplementation among urban and rural pregnant women in North Western Zone of Tigray, Ethiopia: comparative study. Int J Nutr Food Sci. 2015;4(2):161. doi:10.11648/j.ijnfs.20150402.16
28. Nigussie A, Minale S, Addis N. Adherence to iron–folic acid supplementation and associated factors among pregnant women at Felege Hiwot Compressive Specialized Hospital, Bahir Dar, Ethiopia. Ethiop J Reprod Health. 2021;13(4):11.
29. Dutta AJ, Patel P, Bansal R. Compliance to iron supplementation among pregnant women: a cross sectional study in urban slum. Natl J Commun Med. 2014;5(04):457–462.
30. Nasir BB, Fentie AM, Adisu MK. Assessment of adherence to iron and folic acid supplementation and prevalence of anemia in pregnant women. Med J Cairo Univ. 2011;79(2):115–121.
31. Abebaw B, Dessie Y, Baraki N, Oumer A, Gebru M. Adherence to iron and folic acid supplementation and associated factors among antenatal care attendants in Northwest Ethiopia. Int J Public Health. 2020;9(1):20–28.
32. Lyoba WB, Mwakatoga JD, Festo C, Mrema J, Elisaria E. Adherence to iron-folic acid supplementation and associated factors among pregnant women in Kasulu communities in north-western Tanzania. Int J Reprod Med. 2020;2020:1–11. doi:10.1155/2020/3127245
33. World Health Organization. Global Nutrition Targets 2025: Anaemia Policy Brief (WHO/NMH/NHD/14.4). Geneva: World Health Organization; 2014.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
