Back to Journals » Integrated Pharmacy Research and Practice » Volume 9
Knowledge, Attitude, and Practice on Over-the-Counter Drugs Among Pharmacy and Medical Students: A Facility-Based Cross-Sectional Study
Authors Bekele KM, Abay AM, Mengistu KA, Atsbeha BW , Demeke CA , Belay WS , Yimenu DK
Received 15 June 2020
Accepted for publication 17 August 2020
Published 15 September 2020 Volume 2020:9 Pages 135—146
DOI https://doi.org/10.2147/IPRP.S266786
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Jonathan Ling
Kidist Mulugeta Bekele, Ahmed Moges Abay, Kidist Abiye Mengistu, Berhanemeskel Weldegerima Atsbeha, Chilot Abiyu Demeke, Wudneh Simegn Belay, Dawit Kumilachew Yimenu
Department of Pharmaceutics and Social Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Dawit Kumilachew Yimenu
Department of Pharmaceutics and Social Pharmacy, School of Pharmacy, College of Medicine and Health Sciences, University of Gondar, Gondar, Amhara Regional State, Ethiopia
Tel +251 920 760 099
Email [email protected]
Background: Self-medication with over-the-counter (OTC) medications is common among medicine and health science students. For safe use of OTC medications, students are expected to have proper knowledge, attitude, and practice (KAP) towards OTC medications and subsequent adverse drug reactions (ADRs).
Objective: The aim of this study was to assess KAP of OTC medications use and related factors among medical and pharmacy students at the University of Gondar, Gondar, Northwest Ethiopia.
Methods: A cross-sectional study was conducted. Data were collected using a self-administered questionnaire and analyzed using Statistical Package for Social Sciences (SPSS) version 24. Chi-square analysis was conducted and multivariable logistic regression analysis was used to determine the association between KAP and OTC use and its related adverse effects. A P value of less than 0.05 was used to declare statistical significance.
Results: A total of 380 students (229 medical students and 151 pharmacy students) participated in the study. The majority of the respondents 303 (79.7%) reported that they have the practice of self-medication. Fever 69 (80.2%), headache 21 (24.4%), and abdominal cramp 20 (23.3%) were the most common conditions for which the students go for self-medication while paracetamol 51 (59.3%) followed by non-steroidal anti-inflammatory drugs (NSAIDs) 44 (51.2%) were the most commonly used classes of drugs. An intention for time-saving caused by the waiting time due to crowds in medical consultation rooms 212 (77.4%) and a desire for quick relief 171 (62.4%) were the main reasons for the self-medication practice with OTC medications.
Conclusion: Self-medication is widely practiced among medical and pharmacy students. Significant problems and malpractices were identified, such as sharing of OTC medications, the use of expired medicines, doubling the dose of medications when they were ineffective, storage of OTC medications, and not reading labels and expiry dates.
Keywords: self-medication, pharmacy students, medical students, over-the-counter, Gondar
Introduction
Despite all their benefits, improper use of medicines can bring potential health hazards and evidence continue to mount that adverse reactions to medicines are common, yet often preventable, cause of illness, and even death is evident.1 Self-medication (SM) can be defined as “the selection and use of medicines by individuals to treat self-recognized illnesses or symptoms without consultation of health care professionals”.2,3 Though it was previously considered unnecessary, responsible self-medication is regarded as an essential aspect of self-care.2
SM is prevalent in every age group, though its extent differs among individuals and regions. Self-medication assumes a special significance among pharmacy and medical students as they are the future health care practitioners and have a potential role in counseling their patients about the advantages and disadvantages of self-medication. They also differ from the general population because they are well-exposed to the knowledge about diseases and drugs.4
Globally, many studies have reported the prevalence of self-medication among healthcare professionals in both developing and developed countries.5–7 A cross-sectional, study conducted at Aga Khan University in Karachi, Pakistan showed that the prevalence of self-medication was 76%.8 The study also revealed that the most commonly used medicines were analgesics (88.3%), antipyretics (65.1%), and antibiotics (35.2%). Similar findings were also reported by studies conducted in Serbia and India in which the total prevalence of SM was 79.9% and 78.6% respectively.9,10 A more profound outcome was reported by a study conducted in Kuwait, in which the overall prevalence of self-medication was 97.8%.11
Different reasons were reported regarding the common motives for SM practice in which prior experience with the medications and for the treatment of mild symptoms being the most.2,8 In many of the studies, Over-the-counter (OTC) drugs were commonly used, though some of the studies had also reported the use of prescription-only drugs which are dangerous without professional counseling.2
Over-the-counter (OTC) medicines are medicines that may be sold directly to a consumer without a prescription from pharmacy personnel, as compared to prescription drugs, which are dispensed only to consumers possessing a valid prescription. Lack of adequate knowledge about OTC medications may directly lead to bad outcomes, such as overuse or non-compliance to treatment programs.12 There are several potential risks with the use of inappropriate self-medication such as the risk of adverse drug reactions, risk of wrong use of drugs, risk of missing the diagnosis, risk of drug dependence, risk of drug-drug, drug-food, drug-disease interactions, risk of overuse or toxicity.4,13–15
Significant variability has been reported in different studies regarding the knowledge, attitude, and practice of healthcare professional students towards self-medication use and associated ADRs.8,13,14,16 In the Ethiopian context, few studies have been conducted regarding self-medication. One systematic review revealed that the prevalence of self-medication practice in Ethiopia was between 12.8% to 77.1%, with an average of 36.8%.17 Other studies conducted in Addis Ababa and Mekelle showed that the prevalence of self-medication was 62.7% and 43.24% respectively.4 In the study conducted in Addis Ababa, it was also reported that nearly half of the respondents (47.3%) did not know the medication classification of OTC and prescription-only drugs.4
In Ethiopia, although the regulatory body (Food, Medicine & Health Care Administration & Control Authority of Ethiopia (FMHACA)), has recommended the list of medications to be available online,18 due to the poor enforcement of the regulatory system, almost every pharmacy sells drugs without a prescription.19 Many types of antibiotics, mild-analgesics, and many of the anti-inflammatory drugs are all available OTC. This, together with poor awareness, leaves the average person uninformed about the potentially lethal effects of some of these drugs.4 Also, the lack of an excellent primary health care system coupled with cost issues causes the general public to approach many other doors instead of doctors to seek help for a problem. Despite this, there is a paucity of literature regarding self-medication in Ethiopia, and no measures have been taken to address this problem.4 This study presents to assess the medical and pharmacy students’ knowledge, attitude, and practice towards OTC medication use and associated factors.
Materials and Methods
Study Area and Period
The study was conducted at the College of Medicine and Health Sciences (CMHS), University of Gondar, Gondar, Ethiopia. Gondar is a one of the most famous historical cities in Ethiopia, which is located in the northwestern part of the country, at 747 km away from Addis Ababa, the capital city of the country. The university was established in 1954 and it is the oldest medical training institutions in Ethiopia. At the time of the current study, the CMHS offers more than 11 undergraduate and 34 postgraduate pragmas for local and international students. The study was conducted from February 1 to April 30, 2019.
Study Design
A facility-based cross-sectional study was conducted by administering a structured questionnaire to the pharmacy and medical students enrolled at the CMHS, University of Gondar, Ethiopia.
Population and Sampling
Source Population
All students enrolled at the CMHS, University of Gondar.
Sample Population
All Medical and pharmacy students at the CMHS, University of Gondar.
Inclusion Criteria
Medical and pharmacy students at the CMHS, University of Gondar that started clinical practice/attachment; that is fourth year and above medical and fourth year and fifth year pharmacy students.
Exclusion Criteria
Students who did not volunteer to participate in the study.
Dependent Variables
Knowledge, Attitude, Practice.
Independent/Explanatory Variables
Socio-demographic characteristics (age, sex, year of study, academic field of study … )
Sample Size Determination and Sampling Technique
The sample size was determined using the single population proportion formula. A previous SM prevalence rate of 38.5% was used.5 Assuming a 95% confidence interval, 5% margin of error, and adding a 10% non-response rate, the final sample size was 400.
A simple random sampling technique was used to select study samples. In total there were 1112, 4th year, and above pharmacy and medical students. Those students were selected because the other (1st year to 3rd year) students might not be well familiar to their professional field of study as most of the courses they took are common courses and introductory courses which will not much contribute to their previous knowledge. The final sample size was distributed to both departments based on their proportional number of students. Each sampled student was selected from each of the departments by systematic random sampling technique, using the student’s first name in alphabetical order as a sampling frame.
Data Collection Tool and Technique
A self-administered, structured, and pre-tested questionnaire was used. The questionnaire was adopted from previously conducted similar studies and modified to fit with the current set-up.16,20 The data were collected by two data collectors who were well briefed about the data collection procedure and the purpose of the study. The questionnaire composed of four parts: socio-demographic characteristics (9 questions), knowledge-related questions (10 questions), attitude-related questions (8 questions), and practice-related questions (13 questions) respectively. The scores were calculated by adding the correct answers to the proposed questions and dividing them into the total number of questions. For the knowledge item questions, each correct answer counts “1” point while every wrong answer count “0”. An overall score of ≥5 was considered as good knowledge. The attitude part composed of 8 questions with a 5 Likert-scale. The responses were; strongly disagree, disagree, not sure, agree, and strongly agree each weighing 1–5 respectively for each positive statement. Total score ranges from 8 to 40, with an overall higher mean score indicating a positive attitude towards SM practice.
The fourth part (practice part) consisted of questions with many different options and each correct answer was given a score of “1” and “0” for the wrong answer. The total score ranged from 0–13, and a score of 7–13 demonstrated good practice and a score of 0–6 indicates poor practice concerning SM. The practice-related questions were specifically designed to assess the self-medication rate of the study participants and the association of their educational background to their practice. The questionnaire’s reliability was checked using Cronbach’s alpha test and the value was 0.613.
Data Processing and Analysis
Data were checked, sorted, categorized, and coded manually then transferred to Statistical Package for Social Sciences (SPSS) version 24 for analysis. Chi-square analysis was conducted and multivariable logistic regression analysis was used to determine the association between KAP and OTC use and its related adverse effects. A P-value of <0.05 was taken to declare statistical significance.
Data Quality Control
The data collectors were given 1 day of training on the data collection procedure and the purpose of the study. Pre-test of the data collection tool was conducted on 10 students (5 medical and 5 pharmacy students), 3 days before the actual data collection date, to check for the uniformity and understandability of the questionnaire. Any confusing issue and data with missing of important information were omitted. The collected data were checked for completeness and accuracy each day before entering into software for analysis.
Ethical Considerations
Ethical approval was obtained from the research and ethics review committee of the School of Pharmacy, the University of Gondar with an approval number SoP 487/2019. Informed verbal consent was also obtained from each respondent after explaining the purpose of the study and that verbal informed consent was acceptable and approved by the Ethics Review Committee of the School of Pharmacy, University of Gondar. Participant’s confidentiality was guaranteed by collecting the data anonymously.
Operational Definition
Good Knowledge
Score equal to or above the median knowledge cumulative score.
Poor Knowledge
Score below the median cumulative knowledge score.
Positive Attitude
Score above or equal to a cumulative attitude score of 20.
Negative Attitude
Score a cumulative attitude score below 20.
Risky Practice/Malpractice
A respondent was considered to have risky practice if he/she failed to check the expiry date of the medications or read labels, took more than the recommended dose, stored OTC medications improperly, or continued consuming OTC drugs even though he/she noticed unusual color, odor or shape changes.
Results
A total of 400 questionnaires were distributed to be filled by the study participants, and 380 were filled and collected, which gives a response rate of 95%. From the total study participants, 230 (60.5%) were male by gender and the majority of them 237 (62.4%) were within the age group of 23–25, with a mean age of 23.5 years (SD=6.521). Concerning the profession of education, 229 (60.3%) were medical students while 151 (39.7%) were pharmacy students. Almost all of the participants 377 (99.2%) were single by marital status. (Table 1)
 |
Table 1 Socio-Demographic Characteristics of the Study Participants; N=380 |
Knowledge of OTC Medications
The mean knowledge score was 6.59 (SD=1.32). About 257 (67.6%) of the respondents had good knowledge about the safety and effectiveness of the OTC medications. Significant differences were identified between the medical and pharmacy students regarding the type of diseases OTC medications were to be used for (P=0.004), in which the majority of them 337 (88.7%), (212 (62.9%) medical students and 125 (37.1%) pharmacy students) reported that they were usually used for treating minor illnesses and injuries. About 347 (91.3%) agreed that caution should be taken mostly when using over-the-counter drugs during pregnancy. Three-fourth of the respondents 285 (75%) reported that OTC medications should not be used after their expiry date. There was also a significant difference between the medical and pharmacy students (P=0.032). Besides, 228 (60.0%) of the respondents agreed that OTC medications should immediately be stopped if suspected side-effect(s) were seen.
A significant difference was identified between the medical and pharmacy students (P=0.001) about the conditions where caution should be taken while taking OTC medications, in which the majority of them reported pregnancy 347 (91.3%) and lactation 298 (78.4%) being the main situations to be cautious. (Table 2)
 |
Table 2 Knowledge of the Study Participants Towards OTC Medication Use; N=380 |
Attitude Towards OTC Medications
The mean attitude score was 26.62/40 (SD=3.42). From the total study participants, 46 (12.1%) strongly agree and 183 (48.2%) agree that OTC medications are cheaper and convenient to use. A significant difference was also identified among medical and pharmacy students (P=0.014). A total of 216 (56.9%) of the respondents were also positive on the appropriateness of sharing of OTC medications with others. About 40 (10.5%) strongly agree and 152 (40.0%) agree that it is appropriate to treat minor-ailments like a common cold with OTC medications. There was a significant difference among the medical and pharmacy students (P=0.049) concerning the appropriateness of seeking a pharmacist’s advice when someone has OTC medicines that he/she has never used before, in which nearly half of the study participants 179 (47.1) agreed to. Similar results were found concerning whether it was appropriate for someone who went to a pharmacy for OTC medication, he/she should bring all the medications he/she was currently taking, in which the majority of the study participants had agreed 107 (28.2%). A statistically significant difference was also identified among medical and pharmacy students (P=0.001). (Table 3)
 |
Table 3 The Attitude of the Respondents Towards OTC Medication Use; N=380 |
OTC Medication Practice
The majority of the respondents 303 (79.7%) had reported that they have at least once practiced SM with OTC medications (Figure 1). From a total of 303 study participants who have a history of SM, 263 (86.8%) of them reported that they have experienced some adverse effects from the OTC medications they took. On the other hand, while 150 (39.5%) of the study participants reported that they always read the instructions on the drug labels before use, 16 (4.2%) of them reported they never read them (Figure 2). Furthermore, about 20.79% of the respondents reported that they rarely or never check the expiry date of the OTC medications they took. (Figure 3).
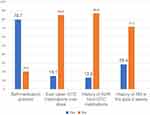 |
Figure 1 Self-medication utilization related characteristics of the study participants. Abbreviations: ADR, adverse drug reaction; OTC, over-the-counter; SM, self-medication. |
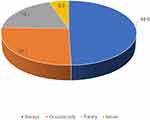 |
Figure 2 Premedication usage instruction reading behavior of the study participants. |
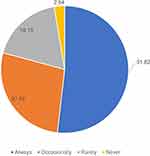 |
Figure 3 Premedication usage expiry date checking behavior of the study participants. |
When asked about “whom they consult before using OTC medications”, the majority of the respondents 174 (57.4%) reported that they consult pharmacists, followed by doctors 107 (35.3%), friend/relatives 82 (27.1%), internet and mobile applications 60 (19.8%), drug leaflets 27 (8.9%) and 46 (15.2%) reported they never consult anyone. Time-saving 212 (77.4%), quick relief 171 (62.4%), no need to visit a doctor for minor illnesses 136 (49.6%), economic issues 78 (28.5%), ease and convenience 73 (26.6%), and because of educational knowledge about drugs 15 (5.5%) were the most common reasons for using SM with OTC drugs.
When asked about what they will do if the OTC drug they used has failed, 161 (53.1%) answered that the will go to health facilities for consultation, 108 (35.6%) will change the drug to other powerful OTC medication, and 73 (24.1%) reported that they will double the dose. Paracetamol 51 (59.3%) followed by NSAIDs 44 (51.2%), antacids 19 (22.1%), albendazole 19 (22.1%), amoxicillin 15 (17.4%) and post pills 5 (5.8%) were the most commonly used OTC drugs among the study participants. Fever/headache and abdominal cramp were the most common illnesses for which the respondents consume OTC medications 69 (80.2%) and 21 (24.4%) respectively. Three-fourth of the study participants reported that they consume OTC medications when the symptoms were minor 228 (75.2), and there was a statistically significant difference among the students concerning their profession of study (P=0.044). A significant difference (P=0.001) was also identified among the medical and pharmacy students concerning the storage place for their medications, in which the majority of them reported in a bedroom table 196 (64.7%) followed by in a medicine box 140 (46.2%). (Table 4)
 |
Table 4 OTC Drugs Practice-Related Characteristics of the Study Participants |
Associated Factors Towards OTC Medication Use
Chi-square test results show a statistically significant association between the academic year of study and attitude of the students regarding OTC medications (P< 0.05). To assess the attitude towards OTC Self-medication among medical and pharmacy students the reference was formed as 1 odds ratio. Females had a better attitude 1.401 times more than males towards OTC self-medication; however, the association was not found to be significant (P=0.118). The association between years of study and the student’s attitude towards OTC medications revealed that there was a significant difference (P=0.006) between fourth and six-year (internship) students. (Table 5)
 |
Table 5 Association Between Attitude Towards Self-Medication and the Independent Variables |
Discussion
In the present study, the prevalence of SM with OTC medications was 79.7%. This result was consistent with similar studies conducted in Pakistan, Serbia, and India in which the prevalence of SM was 76%, 79.9%, and 78.6% respectively.8–10 Self-medication, when adopted effectively, can be beneficial as it may relieve acute pain, and reduce treatment cost and physician interaction time.15 However, it can also endanger human health and result in severe health-related complications when used inappropriately, such as in cases of self-treatment with prescription-only medications.21 The development of drug resistance to many antibiotics has also been associated with the frequent and inappropriate use of those medications that could be available without a prescription.22 Other harmful practices and associated consequences with the frequent use of OTC medications include inappropriate dosing, drug duplication, drug interaction, treatment failure, masking of health problems and symptoms, and delay in prescribing the appropriate treatment.23
In the present study, fever/headache 80.2%, and abdominal cramp 24.4% were the most common illnesses for which the respondents consume OTC medications. This finding was consistent with two studies conducted in Addis Ababa and a previous study conducted in Gondar.4,5 A study conducted in Jordan, also reported that headache (81.9%) was the most common reason for which students go for SM.24 This could be because these are the most prevalent illnesses that frequently affect many people and for which medications are usually available in pharmacies on as OTC.25
Paracetamol 59.3% followed by NSAIDs 51.2%, were the most commonly used OTC drugs among the study participants. This finding was also consistent with findings from previous studies conducted in Addis Ababa, Gondar and Mekelle in which paracetamol and other anti-pain medications were the most frequently used OTC medications.4,5,26 This is true because due to stress and other educational loads, medicine and health science students are usually victims of headaches and other stress-related factors that usually force them to seek medications on an OTC basis.27,28
In the present study, the most common reasons for the utilization of SM with OTC medications were; to save time 77.4%, Quick relief 62.4%, and for treatment of minor ailments 49.6%. Similar findings were reported by a study conducted in Saudi Arabia29 and Pakistan30 in which in the former case, a desire to avoid long waiting time to see physician 39% followed by a need to not burden the physician for minor illness 26% were the commonest reasons for SM, while in the latter one, mild nature of the disease 34.3% followed by the easy availability of the drugs (30.1%) were the most common reasons for SM practices. This is evident because the study participants being medicine and health science students make them familiar with diseases and their treatment (medications) which will in turn make them opt to treat themselves without consulting regular physicians.
In the current study, the mean knowledge score was 6.59. This finding was consistent with a study conducted in Nepal, which reported that more than half of the respondents were found to have good knowledge about self-medication and had a positive attitude.16 Similar findings were also reported by a study conducted in Saudi Arabia.29 Although the mean score was above the average [5], it was still not good enough. Medicine and pharmacy students are the ones who are expected to be experts of medications and thus took many medications related courses that could increase their knowledge and understanding about every aspect of medications utilization.
In the current study, 56.9% of the respondents were positive on the appropriateness of sharing of OTC medications with others. This should be a concern because as the main concerning health professionals regarding medications, medical and pharmacy students have the responsibility to be role models and advise others on the negative impacts of sharing medications. Medication sharing is one of the major reasons for the various adverse health consequences such as unmonitored adverse drug events, complications in clinical diagnosis, drug resistance, and delay in care-seeking.31–33
In the present study, the attitude of the respondents towards OTC self-medication was almost the same except regarding the year of study in which there was a significant difference between a fourth year and six-year (internship) students. This finding was consistent with a similar study conducted in Jordan, in which senior students were found to be more aware of the risk of self-medication than junior students.34 This could be because when the years of study increase, the students will become more familiar with the medications and clinical practice which will directly affect their attitude towards OTC medications and SM practice.
About 20.79% of the respondents in the current study reported that they rarely or never check the expiry date of the OTC medications they took. This finding was higher than a similar study conducted in Asmara, Eritrea in which 7.5% of the study participants reported that they never checked expiry dates.35 This is concerning because the practice of not checking the expiry date of the medications may lead to the accumulation of those expired medications in the household and the many detrimental effects of the medications.36
Although the numbers were not significant, when asked about what they will do if OTC drugs show a change in shape, color and or odor, some of the respondents had reported continue using till it expires 14.9%, and even some of them reported continue using even after the expiry date 3.3%. This is very much concern because of the professional background of the study participants who are expected to be role models to others and condemn these types of malpractices. Some ongoing researches showed that if stored under optimal conditions, many drugs retain 90% of their potency for at least five years after the labeled expiration date, and sometimes longer.37 However, The WHO has recommended that expired or unused pharmaceuticals should never be reused,38 and many other studies have also reported the dangerous consequences of taking expired medications.39,40 Due to a change in chemical composition or a decrease in potency, expired medications can be less effective or risky. Some products may also get degraded if used after their expiration date and the products of degradation are significantly more toxic than the original active pharmaceutical ingredient.39
Another risky behavior was also observed among the respondents in which a significant number of the participants reported that they will double the dose if the OTC medication they used has failed. Taking medications above their recommended dose is one of the most common factors for the various ADRs incurred by medications, and these kinds of malpractices have also been documented with the use of OTC medications.41
Regarding storage of the medications they took, a significant number of the respondents reported a medicine box (cabinet) (46.2%), and though it was not significant, some of them also reported to sore them in a bathroom (0.7%). Besides the dangers of accidental poisoning by children and other related risks associated with improper storage of medications, bathroom and medicine cabinet are not ideal places to store medications due to heat and humidity which can contribute to loss of potency and shortening of the shelf life of the medications.42
Limitations of the Study
Since the study was a cross-sectional study, the results of the study are dependent on the response given by the study participants and thus there may be respondent bias as the respondents may not tell their genuine behavior to some of the questions. The other limitation could be concerning the study participants, in which the study could have been more generalizable if other health professional students and/or students from the whole years of study (1st year to 6th year) were included.
Conclusion
Self-medication with OTC drugs is widely practiced among medical and pharmacy students. Significant problems and malpractices were identified such as; sharing of OTC medications, the use of expired medicines, doubling the dose of medications when they were ineffective, storage of OTC medications, and not reading labels and expiry dates.
Recommendation
Strategies should be implemented to improve some of the malpractices practiced by medical and pharmacy students. Medical and pharmacy students should also take huge responsibility and be role models to other students towards the utilization of medications as they are the experts on them to whom the others will infer to.
Data Sharing Statement
The data sets generated and/or analyzed during the current study are not available in public due to the requirement of confidentiality upon which the study was approved by the Ethical review committee and consent was secured from the study participants but is available from the corresponding author on reasonable request.
Acknowledgments
The authors would like to acknowledge the University of Gondar for its support and facilitating the study and all the study participants for their collaboration and participation in the study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. Aishwaryalakshmi K, Sasikala B, Sreelalitha N, Vigneshwaran E, Reddy YP. Assessment of knowledge perception and attitudes on medications in the general population. Editorial Board. 2012;6.
2. World Self-Medication Industry (WSMI). Responsible self-care and self-medication: a worldwide review of consumer surveys. Ferney-Voltaire: WSMI. Available from: http://www.wsmi.org/wp-content/data/pdf/wsmibro3.pdf.
3. Azhar MIM, Gunasekaran K, Kadirvelu A, Gurtu S, Sadasivan S, Kshatriya BM. Self-medication: awareness and attitude among the Malaysian urban population. Int J Collab Res Intern Med. 2013;5(6):436.
4. Beyene A, Getachew E, Doboch A, Poulos E, Abdurahman K. Knowledge, attitude and practice of self-medication among pharmacy students of rift Valley University, Abichu campus, Addis Ababa, Ethiopia. J Health Med Informat. 2017;8(269):2. doi:10.4172/2157-7420.1000269
5. Abay S, Amelo W. Assessment of self-medication practices among medical, pharmacy, health science students in Gondar University, Ethiopia. J Young Pharm. 2010;2(3):306–310. doi:10.4103/0975-1483.66798
6. Banerjee I, Bhadury T. Self-medication practice among undergraduate medical students in a tertiary care medical college, West Bengal. J Postgrad Med. 2012;58(2):127. doi:10.4103/0022-3859.97175
7. El Ezz N, Ez-Elarab H. Knowledge, attitude and practice of medical students towards self-medication at Ain Shams University, Egypt. J Prev Med Hyg. 2011;52(4):196–200.
8. Zafar SN, Syed R, Waqar S, et al. Self-medication amongst university students of Karachi: prevalence, knowledge and attitudes. J Pak Med Assoc. 2008;58(4):214.
9. Lukovic JA, Miletic V, Pekmezovic T, et al. Self-medication practices and risk factors for self-medication among medical students in Belgrade, Serbia. PLoS One. 2014;9(12):e114644. doi:10.1371/journal.pone.0114644
10. Kumar N, Kanchan T, Unnikrishnan B, et al. Perceptions and practices of self-medication among medical students in coastal South India. PLoS One. 2013;8(8):e72247. doi:10.1371/journal.pone.0072247
11. Al-Hussaini M, Mustafa S, Ali S. Self-medication among undergraduate medical students in Kuwait with reference to the role of the pharmacist. J Res Pharm Pract. 2014;3(1):23. doi:10.4103/2279-042X.132706
12. Eissa AT. Knowledge, attitudes and practices towards medication use among health care students in King Saud University. Nursing. 2013;31:
13. Dawood OT, Hassali MA, Saleem F, Ibrahim IR, Abdulameer AH, Jasim HH. Assessment of health seeking behaviour and self-medication among general public in the state of Penang, Malaysia. Pharm Pract (Granada). 2017;15(3).
14. Elbur A, Almalki NH, Alghamdi AA. Knowledge, attitudes and practices on medication use and safety among Saudi people: a public–based versus an internet–based survey in Taif; Kingdom of Saudi Arabia. Saudi J Med Pharm Sci. 2016;2:99–103. doi:10.21276/sjmps.2016.2.6.3
15. James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Princ Pract. 2006;15(4):270–275. doi:10.1159/000092989
16. Mehta RK, Sharma S. Knowledge, attitude and practice of self-medication among medical students. Age (Years). 2015;20(49):
17. Ayalew MB. Self-medication practice in Ethiopia: a systematic review. Patient Prefer Adherence. 2017;11:401. doi:10.2147/PPA.S131496
18. Food, Medicine & Health Care Administration & Control Authority of Ethiopia. Over the counter medicines list for ethiopia; 2012. Available from: http://www.fmhaca.gov.et/publication/over-the-counter-medicines-list-for-ethiopia-2nd-edition/.
19. Erku DA, Mekuria AB, Surur AS, Gebresillassie BM. Extent of dispensing prescription-only medications without a prescription in community drug retail outlets in Addis Ababa, Ethiopia: a simulated-patient study. Drug Healthc Patient Saf. 2016;8:65. doi:10.2147/DHPS.S106948
20. Susheela F, Goruntla N, Bhupalam PK, Veerabhadrappa KV, Sahithi B, Ishrar SM. Assessment of knowledge, attitude, and practice toward responsible self-medication among students of pharmacy colleges located in Anantapur district, Andhra Pradesh, India. J Educ Health Promot. 2018;7. doi:10.4103/jehp.jehp_177_17
21. Hughes CM, McElnay JC, Fleming GF. Benefits and risks of self medication. Drug Safe. 2001;24(14):1027–1037. doi:10.2165/00002018-200124140-00002
22. Al-Azzam SI, Al-Husein BA, Alzoubi F, Masadeh MM. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. 2007;20(4):373. doi:10.2478/v10001-007-0038-9
23. Zafar SN, Syed R, Waqar S, et al. Self-medication amongst university students of Karachi: prevalence, knowledge and attitudes. J Pak Med Assoc. 2008;58(4):214–217.
24. Alshogran OY, Alzoubi KH, Khabour OF, Farah S. Patterns of self-medication among medical and nonmedical University students in Jordan. Risk Manag Healthc Policy. 2018;11:169. doi:10.2147/RMHP.S170181
25. Zebenigus M, Tekle-Haimanot R, Worku DK, Thomas H, Steiner TJ. The burden of headache disorders in Ethiopia: national estimates from a population-based door-to-door survey. J Headache Pain. 2017;18(1):58. doi:10.1186/s10194-017-0765-7
26. Gutema GB, Gadisa DA, Kidanemariam ZA, et al. Self-medication practices among health sciences students: the case of Mekelle University. J Appl Pharm Sci. 2011;1(10):183.
27. Demirkirkan MK, Ellidokuz H, Boluk A. Prevalence and clinical characteristics of migraine in university students in Turkey. Tohoku J Exp Med. 2006;208(1):87–92. doi:10.1620/tjem.208.87
28. Nandha R, Chhabra MK. Prevalence and clinical characteristics of headache in dental students of a tertiary care teaching dental hospital in Northern India. Int J Basic Clin Pharmacol. 2013;2(1):51–55. doi:10.5455/2319-2003.ijbcp20130110
29. Al Essa M, Alshehri A, Alzahrani M, et al. Practices, awareness and attitudes toward self-medication of analgesics among health sciences students in Riyadh, Saudi Arabia. Saudi Pharm J. 2019;27(2):235–239. doi:10.1016/j.jsps.2018.11.004
30. Malik IJ, Bhatti AA, Din AT, et al. Assessment of knowledge, attitude, and practices regarding self-medication for acne among medical students. Cureus. 2019;11(8).
31. Mak´owka A, Zawiasa A, Nowicki M. Prescription medication sharing among family members: an unrecognized cause of a serious drug adverse event in a patient with impaired renal function. Clin Nephrol. 2015;83(3):196–200. doi:10.5414/CN108052
32. Dimitrov D. “Impact of pill sharing on drug resistance due to a wide-scale oral prep intervention in generalized epidemics,”. J AIDS Clin Res. 2013;1:S5. doi:10.4172/2155-6113.S5-004
33. Mayhorn CB, Goldsworthy RC. “Borrowing prescription medication: implications for healthcare warnings and communications”. Proc Hum Factors Ergon Soc Annu Meet. 2009;53(20):1608–1611. doi:10.1177/154193120905302014
34. Alkhatatbeh MJ, Alefan Q, Alqudah MA. High prevalence of self-medication practices among medical and pharmacy students: a study from Jordan. Int J Clin Pharmacol Ther. 2016;54(5):390. doi:10.5414/CP202451
35. Tesfamariam S, Anand IS, Kaleab G, et al. Self-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, Eritrea. BMC Public Health. 2019;19(1):159. doi:10.1186/s12889-019-6470-5
36. Annear B, Sinclair K, Robbé IJ. Response to ‘Returned medicines: waste or a wasted opportunity?’. J Public Health (Bangkok). 2008;30(2):209. doi:10.1093/pubmed/fdn006
37. American Medical Association. Pharmaceutical expiration dates. Report 1 of the Council on Scientific Affairs (A-01).
38. Gray RCF, Hogerzeil HV, Prüss AM, Rushbrook P. Guideline of Safe Disposal of Unused Pharmaceuticals in and After Emergencies. Geneva, Switzerland: World Health Organization; 1999:1–31.
39. Ogunshe A, Adinmonyema P. Evaluation of bacteriostatic potency of expired oral paediatric antibiotics and implications on infant health. Pan Afr Med J. 2014;19.
40. Stoppler MC, Ogbru A Taking expired medications: what’s the harm? [Online]; 2011. Available from: http://www.rxlist.com/expired_medications/drugscondition.htm.
41. Schmiedl S, Rottenkolber M, Hasford J, et al. Self-medication with over-the-counter and prescribed drugs causing adverse-drug-reaction-related hospital admissions: results of a prospective, long-term multi-centre study. Drug Safe. 2014;37(4):225–235. doi:10.1007/s40264-014-0141-3
42. Gikonyo D, Gikonyo A, Luvayo D, Ponoth P. Drug expiry debate: the myth and the reality. Afr Health Sci. 2019;19(3):2737–2739. doi:10.4314/ahs.v19i3.49
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
