Back to Journals » Adolescent Health, Medicine and Therapeutics » Volume 9
Knowledge and risk perception of sexually transmitted infections and relevant health care services among high school students in the Platfontein San community, Northern Cape Province, South Africa
Authors Nyasulu P , Fredericks M , Basera TJ, Broomhead S
Received 18 October 2017
Accepted for publication 17 January 2018
Published 16 November 2018 Volume 2018:9 Pages 189—197
DOI https://doi.org/10.2147/AHMT.S154401
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Alastair Sutcliffe
Peter Nyasulu,1,2 Mercedes Fredericks,2 Tariro J Basera,2 Sean Broomhead3
1Division of Epidemiology and Biostatistics, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa; 2School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa; 3Health Information Systems Program, Waterkloof Ridge, Pretoria, South Africa
Background: The historically marginalized Platfontein San youths have a high rate of teenage pregnancies and sexually transmitted infections (STIs). The aim of the study was to assess the knowledge and perception of male and female school-going youths in Platfontein of STIs and HIV/AIDS, and the health care services that are available to them.
Participants and methods: A descriptive cross-sectional survey with a sample of 201 learners in grades 6–12 at the !Xunkwesa Combined School in Platfontein was conducted in July 2007. A pretested self-administered questionnaire was used for data collection.
Results: The study found that STI knowledge was 70.1% and HIV and AIDS was 11.9%. Perceptions of risk among the learners were uniformly low; 24% for contracting a STI and 26% for HIV. About 59% (n=119) of the respondents were either unaware or not sure of the primary health care (PHC) services within the community. Overall, 65% of the students reported using PHC services while 35% exclusively used traditional healers. Slightly less than half (43%) of the learners acquired information about sexual and reproductive health through the Life Skills curriculum at school.
Conclusion: The study highlights the importance of increasing HIV awareness and inculcating sexual and reproductive health into the school curriculum. The study further shows the imperative need to recognize the role of traditional medicine in the health care choices of this community. Traditional value systems need to be incorporated into the way that education and health care is proposed to the community leaders, to increase acceptance and utilization of health services.
Keywords: sexually transmitted infections, school-going youths, Platfontein, knowledge, perceptions, San community
Introduction
Sexually transmitted infections (STIs) are a major public health problem disproportionately affecting young people given that STI notification rates peak at 15–24 years of age.1 In 2012, 498.9 million cases of STIs were reported among adults aged 15–49 years2 while two-thirds of new HIV infections occurred among youths, mostly young women aged 15–24.11 Sub-Saharan Africa has the highest STI burden in the world,2,4 and most youths tend to have a low perception of risk because STIs are asymptomatic.5,6 Platfontein is home to approximately 8,000 San from the !Xun and Khwe tribes. The Platfontein San have been on the periphery of socioeconomic and political systems including health services and awareness programs.7,8 STIs are associated with increased risk of HIV acquisition and transmission and other related reproductive complications such as pelvic infections and secondary infertility.9,10 STIs increase the sexual transmission of HIV among adolescents11; such that individuals infected with STIs are 5–10 times more likely to acquire or transmit HIV through sexual contact.12
The national HIV prevalence estimates in South Africa among adults aged 15–49 years generally increased from 15.3% to 17.9%.3 HIV prevalence estimates in the Northern Cape Province were 7.4%.13 However, there is limited data on the national burden of STIs among adolescents in South Africa.14 A study of adolescents in the Eastern Cape Province showed an overall prevalence of 15.8% for curable STIs among the 1,057 adolescents with a mean age of 17 years, whose biological samples were collected for STI screening.15 Few studies of HIV and AIDS have focused on the Platfontein San community. Reports from NGOs, staff at local clinic and community leaders indicate that HIV/AIDS and tuberculosis severely burden the communities, although statistics are not available.16,17 Risk factors for STIs such as unemployment, alcoholism, domestic violence and HIV reported previously on marginalized communities in South Africa18 were also entrenched among the Khwe and !Xun in Platfontein.19,20 The San Baseline study conducted by the AIDS Foundation of South Africa revealed that 73% of the Platfontein San respondents were not using condoms, had multiple sex partners, and they had low knowledge of HIV and AIDS.17
The declining age of sexual debut has been proffered as one possible explanation for the increase in numbers of STIs.5 According to data from a behavioral survey in South Africa, a significant number of youths reported sexual activity before the age of 13 years.13 Another explanation for the increase in rates of STIs could be the reluctance of young people to use condoms.15,21 A study conducted among young people in KwaZulu-Natal Province reports low perceptions of STIs, HIV and AIDS risk among both males and females and they did not perceive that transmission could be prevented by condom usage.22 Condoms have been reported to be used primarily for the prevention of pregnancy and not STIs, and they are inconsistently used when other contraceptives are used.23,24 The factors influencing health choices for Platfontein adolescents have not been documented. However, previous studies done in South Africa showed that traditional medicine plays an active role in the health care of San communities.17,25
De Jager et al observed that people in Platfontein have poor health-seeking behavior, frequently requiring medical care at a very late stage of disease.25 Sexual health outcomes in the community can further be exacerbated by the fact that adolescents are likely to encounter problems in getting the required STI information on prevention and treatment services.17,26 Knowledge, awareness and perceptions studies of STIs, HIV and AIDS, and the STI health care services that are available to the school-going youths of the San-groups of Platfontein are not well understood. Across Southern Africa, the indigenous San populations live in remote areas and they face many barriers to good health. Where health services are available, often health staff do not speak their languages and are involved in the running of local services.16 Based on the foregoing, we aimed to assess the knowledge and risk perceptions of STIs, HIV and AIDS in this indigenous population and their awareness of available local primary health care (PHC) services.
Methods
Study design
This study is a descriptive, cross-sectional survey of self-reported knowledge and perception levels of learners at the !Xunkwesa Combined School in Platfontein.
Study setting and population
The study was conducted in July 2007 at the school premises in Platfontein. The San community of Platfontein consist of approximately 8,000 !Xun and Khwe San who are part of a regional society of Africans, whose livelihood depended on hunting, gathering and pastoralism.7 Before being resettled in 2004, in the township of Platfontein situated in South Africa’s Northern Cape Province, the !Xun and Khwe San originally from Namibia and Angola, were forced off their land and lost the natural resources on which their livelihood depended.8 Although living conditions have improved in terms of housing and proximity to a large city, the communities continue to feel marginalized and neglected by the local government based on the poor quality and limited number of houses and poor provision of services.7 Poverty is a structural problem as 97% of the Khwe and !Xun live on less than one dollar/day and have an unemployment rate of 95%.19 All learners were from either the !Xun or the Khwe San community. Each community practices a different home language, but all teaching is done in Afrikaans. The !Xunkwesa Combined school opened in 2004 and it is the only school at the Platfontein farm, situated approximately 15 km from Kimberley and about 25 km from Barkly West in the Northern Cape Province. The curriculum includes Life Skills, which is part of school Life Orientation curriculum as prescribed by the South African Department of Basic Education.
Sampling and sample size
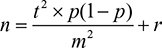
Of the 1,000 learners at !Xunkwesa Combined School, 201 male and female learners in grades 6–12 (ages 12–24 years) were randomly selected from the school records to complete the survey. Learners below grade-6 were excluded because the Life Skills curriculum in lower grades did not include sexual and reproductive health issues hence, they would not be able to relate to the contents of the questionnaire that was administered. Convenience sampling was used to randomly select pupils at the school due to the high absenteeism rate, we decided to select from those that were present at school on the day of the study. Simple random technique was used to draw a sample of 201 out of a total of 1,000 pupils registered from grade 6 to grade 12 at this rural school. All pupils from grade 6 above were eligible to be included in the study. Using the sample formula below we were expected to interview 278 pupils but due to logistical challenges at the time we only achieved a 72.3% response rate. In each class some sample pupils refused to participate compromising the response rate even further. A total of 201 adolescent males and females were then interviewed. The required sample size was determined using the following formula for prevalence surveys:
|
where: n=required sample size, t=confidence level at 95% (standard value of 1.96), p=estimated proportion of knowledge on STI among Platfontein San pupils which was put at 0.5, m=margin of error which was put at 5% and r=approximated non-response rate set at 20%. The estimated non-response rate was based on the school attendance as observed by the school administration but also the fact that pupils might not want to complete the questionnaire due to the inherent stigma that STIs carry because of their close association with HIV/AIDS transmission.
Data collection
Participants completed a self-administered questionnaire which elicited information about respondents’ demographic details and questions related to knowledge, attitudes, perceptions and behavior about STIs, HIV and AIDS and health care service availability for the target group. Other questions were related to the use of the services provided by traditional healers in contrast to the use of the conventional primary health services provided by the community clinic. The questionnaire was designed and pilot-tested among adolescents who frequently visited the local youth center (Roodepan Multi-Purpose Center in Kimberley). Appropriate adjustments to the questionnaire were made based on the observations noted during pilot-testing after which it was distributed to the participants. This approach helped us to assess validity and reliability of our questionnaire as the “measurement tool” that we used for the study. The questionnaire was completed privately and anonymously. The questionnaires were checked for completeness, legibility and for missing information on site.
Statistical analysis procedures
Statistical analysis was performed using Stata version 13. The school children were stratified into lower and higher grades (6–9 and 10–12, respectively). Comparisons were also made between girls and boys, and different age groups. Comparison of categorical variables was done using chi-squared test to determine difference between the variables; P-value <0.05 was regarded as significant.
Ethical considerations
Ethical approval was obtained from the University of Witwatersrand Human Research Ethics Committee (Ethics number: R14/49 Fredericks). Written and official authorization was sought from the Department of Education and the School Principal. Written informed consent was obtained from survey participants and parents or guardians prior to completing the questionnaires which were labelled with unique study numbers to maintain anonymity.
Results
Sample characteristics
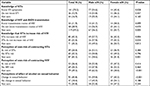
A total of 201 learners completed the questionnaires. Their demographics were as follows: 110 (55%) were male and 91 (45%) were female. Generally, 12% of the students were much older for their respective grades, with a mean age of 16.7 years (standard deviation 2.8) and a range of 12–26 years. There was no significant difference in the age distribution of the learners by sex except age for those in the 18–20 age category (P=0.002), (Table 1). Ethnic distribution showed that 68% of learners were of the Khwe group and 32% the !Xun group.
HIV- and STI-related knowledge
The HIV and STI knowledge levels of the learners are summarized in Table 2. Most (70.2%, n=141) of the learners indicated that they knew the signs and symptoms of STIs, 16.9% were unsure and 12.9% were not knowledgeable about STIs. More male learners knew about STI symptoms compared to female learners (P=0.028). Most learners had poor knowledge of HIV and AIDS, and more male learners were unsure about HIV and AIDS than female learners (P=0.005). Twenty-four (11.9%) learners knew about HIV transmission while, 68 (13.9%) of learners indicated that they knew that abstaining from sexual activity prevents HIV/AIDS and STIs in addition to condom use where abstinence may not be achieved; the majority of which were males (54%) (Figure 1). As shown in Table 2, only 42.3% of the learners were aware that STIs increase the risk of HIV infection with higher proportion of male learners being more aware compared to female learners (P=0.004). Most male learners (59.8%) perceived that alcohol use predisposed them to risky sexual behavior compared with 40.2% of their female counterparts (p=<0.001).
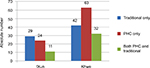  | Figure 1 Utilization of both primary health care and traditional health services. Abbreviation: PHC, primary health care. |
Perception of risk of contracting STI or HIV infection
As shown in Table 2, 87 students (43.3%) said they were not sure whether they were at risk of contracting an STI while 65 (32.3%) students reported that they did not think they were at risk of contracting an STI; 49 (24.4%) considered themselves at risk of contracting an STI with no differences between male and female learners (P=0.384). Most male learners were significantly unsure of their risk of acquiring HIV, 49 (62%) compared with female learners 30 (38%), P<0.001, and there were no significant differences between male and female learners who thought that they were at risk of contracting HIV (P=0.414) and those who said that they had no risk of contracting HIV (P=0.464).
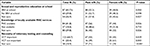
Source of knowledge of sexual and reproductive health
As shown in Table 3, 43.3% (n=87) of the learners indicated that they had been exposed to Sexual and Reproductive Health education (SRH) in school while 26.9% (n=54) were not sure where they had accessed SRH information. Sixty respondents (29.8%) indicated that they had not received any SRH education in school, with no differences between male and female learners (P=0.598).
Awareness of STI and HIV treatment and prevention services in the community
Knowledge on availability of PHC services was low with 84 (41.8%) of the respondents aware about availability of PHC services within their community (Table 3). More males than females viewed voluntary counseling and testing (VCT) as an important component in HIV prevention (P=0.029) (Table 3). The respondents were asked whether they had utilized the service of a traditional healer. Their responses are summarized in Figure 1, 71 (35.3%) of the learners indicated they had visited a traditional healer while 43 (21.4%) of the respondents had utilized both PHC and traditional healer services and 87 (43.3%) had used only PHC services.
Discussion
The aim of the study was to assess knowledge and risk perception of STI, HIV and AIDS among school-going youths in the !Xun and Khwe communities as well as the utilization of local PHC services. While the levels of knowledge of STIs were high, knowledge of HIV and AIDS was low. This finding on STI knowledge levels is consistent with that of a study conducted in Nigeria, in which 67% of the respondents were aware of STIs.27 The findings reflect inadequate coverage of HIV and AIDS education and communication at both the PHC clinic and educational institution. It is imperative that awareness be created about HIV and AIDS. The National Department of Health in South Africa has implemented a number of sexual and reproductive health programs targeting youths. Nonetheless, current evidence from studies conducted in South Africa between 2014 and 2015 indicate that HIV counseling and testing (HCT) has been low in South African adolescents, in particular among boys.6 A cross-sectional study of an out-patient clinic in Durban found low testing numbers (41%) with only 30% of 12–17-year-old males testing for HIV.28 Learners in South Africa bear a disproportionate burden of health problems including teenage pregnancy, HIV and STIs.15
In contrast other studies have reported high levels of knowledge of HIV29 and poor level of knowledge about STIs.26,29 This has been attributed to widespread publicity of HIV campaigns which masked other STIs. A vast majority of students knew about the relationship between STIs and HIV while most were unaware of the association between alcohol or drug use with STIs. These findings underscore the need to increase awareness on other risk behaviors beyond sexual intercourse, associated with contracting STIs including HIV.
The findings of this study showed low perception of risk of acquiring both HIV and other STIs. Similar findings were reported in studies conducted in South Africa and Tanzania.22,26 Utilization of PHC services was high even though a significant number of students utilized both PHC and traditional healer services. Similar findings were reported in a study of utilization of PHC vs traditional medicine in Platfontein.25 These findings are important as they highlight that traditional healers still play a role in the health care of this San community as such there is a need to impart STI and HIV/AIDS information education and communication materials and skills through seminars and workshops as they form an integral part of health care providers in the area. About 20% of the respondents reported that the PHC clinic was youth-friendly, and 28% were unaware that services at the PHC were free (data not shown). Similar findings were reported in a study conducted in India, where only 5.4% of respondents preferred to use the PHC clinic.29 This is also a reflection of poor adaptation and information dissemination by the PHC clinic to tailor services for adolescents. Regarding source of information about STIs and HIV, nearly 45% of students, stated that they got it from sexual and reproductive education in school. This shows the importance of the role of teachers in sex education and inculcating reproductive education in the school curricula. Other studies have reported other major sources of information about sexuality such as electronic media, books, magazines, parents and mass media.26,29,30
There is a need for a strong and relevant sexual and reproductive health education curriculum in schools31 as well as a need for youth-friendly health services programs in the Platfontein community. Risk reduction messages should recognize the cultural norms and values of the target population. In addition, messaging and education program should be tailored to individuals and their settings.32 Given that the education system is geared to teaching specific information in specific grades as suited to the age and grade of the learners, the older learners in the lower grades are thus at a disadvantage in receiving accurate and age-related information. The risk element is increased not only by the limitations on the sexual and reproductive education levels, but also by the likelihood that the older learners may not participate in discussions and debates with younger learners in the same grade. This emphasizes the importance of considering demographic and social determinants of sexual and reproductive health in curriculum design with more emphasis on age-based programs, rather than grade-based. A meta-analysis of school-based sex education and HIV prevention in low- and middle-income countries reported that comprehensive school-based education interventions adapted from effective interventions and those involving a range of school-based and community-based components as well as improved school curriculum incorporating basic STI/HIV preventive strategies seem to have the largest impact on changing HIV-related behaviors.33,34
The study remains the first to engage with health issues among adolescents in an indigenous population of San people in South Africa, a marginalized community with minimal access to health care services hence at an increased risk of STI/HIV transmission. However, when interpreting results of this study, the following limitations need to be taken into account: learners required the ability to recall specific information about STI/HIV and related health care services provided in the area. This approach posed a major challenge in that recall bias was a potential source of error in this study. The common spoken language in this area is Afrikaans requiring the questionnaire to be translated from English hence the quality of translation of the questionnaire into Afrikaans and the level of understanding of the Afrikaans language may have varied significantly among respondents. Since the study focused on the school-going section of the community, the results may not be applicable to the out-of-school youth who are in the majority in the San community. A study that includes the out-of-school youth will give a more accurate indication of how the youth in the San communities relate to the sexual and reproductive health education provided by both traditional and mainstream health care providers. In addition, the potential for occurrence of social desirability bias may not be underestimated due to inherent nature of self-reports.
Conclusions
The study confirms that the perception of risk of acquiring HIV and STIs among the school-going youth of Platfontein is extremely low. Knowledge of HIV and AIDS is lower than that of STIs. The high STI knowledge levels did not appear to have any effect on perceptions of risk of acquiring STIs or the relationship between STIs and HIV transmission. Younger respondents were more knowledgeable about sexual and reproductive health issues than older respondents. A major challenge at Platfontein will be to address the knowledge and perception gaps in older learners, which is compounded by the mixed age groups in each class. The results provide an opportunity to review the existing life skills and sexual and reproductive health curriculum so that it is more age appropriate as opposed to being grade appropriate. They also provide an opportunity for increasing HIV knowledge through community awareness and HIV education in schools and clinic settings. The importance of the use of traditional medicine and the need for this to be integrated within mainstream medicine is demonstrated; however, these study findings may not be generalized to other cultural groups in South Africa.
What is already know on this topic
The following information is already known on this topic: 1) The importance of better HIV awareness and its association to STIs; 2) linkage between STIs and HIV infection acquisition; and 3) low knowledge of HIV among primary school children in San communities
What this study adds
This study adds the following information essential in controlling STI/HIV in this indigenous population: 1) Low perceptions of risk of getting infected with STIs and HIV infection among school children in San communities, 2) the role of traditional medicine in the health care choices among San communities, and 3) impact of incorporating traditional value systems into the way that education and health care services are discharged.
Acknowledgments
We thank all learners who volunteered to participate in the study at the !Xunkwesa Combined School, Platfontein, Northern Cape Province, Republic of South Africa.
Author contributions
PN, MF designed the study. MF collected data. PN, MF did statistical analysis. PN, MF prepared the manuscript. PN, MF, TB, SB participated in interpretation of data and reviewed the manuscript for critical intellectual content. All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Bryant J, Ward J, Worth H, Hull P, Solar S, Bailey S. Safer sex and condom use: a convenience sample of Aboriginal young people in New South Wales. Sex Health. 2011;8(3):378–383. | ||
Newman L, Rowley J, vander Hoorn S, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and global reporting. PLoS One. 2015;10(12):e0143304. | ||
Joint United Nations Programme on HIV/AIDS. Global AIDS Monitoring 2018. Indicators for monitoring the 2016 United Nations Political Declaration on Ending AIDS. Geneva: UNAIDS; 2017. Available from: http://www.unaids.org/sites/default/files/media_asset/global-aids-monitoring_en.pdf. Accessed October 30, 2018. | ||
Kenyon C, Buyze J, Colebunders R. Classification of incidence and prevalence of certain sexually transmitted infections by world regions. Int J Infect Dis. 2014;18:73–80. | ||
Samkange-Zeeb FN, Spallek L, Zeeb H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: a systematic review of published literature. BMC Public Health. 2011;11:727. | ||
Black S, Wallace M, Middelkoop K, et al. Improving HIV testing amongst adolescents through an integrated youth centre rewards program: Insights from South Africa. Child Youth Serv Rev. 2014;45:98–105. | ||
Tempelhoff J. A first-generation African community grappling with urbanisation: the views of Platfontein’s San on water and sanitation service delivery. J Transdisc Res Southern Africa. 2014;10(4):32. | ||
den Hertog TN. Diversity behind constructed unity: the resettlement process of the !Xun and Khwe communities in South Africa. J Contemp African Stud. 2013;31(3):345–360. | ||
Johnson LF, Dorrington RE, Bradshaw D, Coetzee DJ. The role of sexually transmitted infections in the evolution of the South African HIV epidemic. Trop Med Int Health. 2012;17(2):161–168. | ||
Naidoo S, Wand H, Abbai NS, Ramjee G. High prevalence and incidence of sexually transmitted infections among women living in Kwazulu-Natal, South Africa. AIDS Res Ther. 2014;11:11. | ||
Newbern EC, Anschuetz GL, Eberhart MG, et al. Adolescent sexually transmitted infections and risk for subsequent HIV. Am J Public Health. 2013;103(10):1874–1881. | ||
da Ros CT, Schmitt CS, da Silva Schmitt C. Global epidemiology of sexually transmitted diseases. Asian J Androl. 2008;10(1):110–114. | ||
Shisana O. South African national HIV prevalence. Incidence and behaviour survey, 2012. Cape Town, South Africa: HSRC Press; 2014. http://www.hsrc.ac.za/uploads/pageContent/4565/SABSSM%20IV%20LEO%20final.pdf. Accessed October 16, 2018. | ||
Radebe F, Jemmott J, Klopper A, Jemmott L, O’Leary A, Ngwane Z et al. Incidence and prevalence of sexually transmitted infections among school students in the Eastern Cape, South Africa. Sex Transm Infect. 2011;87(Suppl 1):A30-1. | ||
Oni T, Tshitangano T. Risky sexual behaviors among rural teenagers in Vhembe District, South Africa. J Soc Sci. 2015;44(1):60–65. | ||
Den Hertog TN, de Jong M, van der Ham AJ, Hinton D, Reis R. “Thinking a Lot” Among the Khwe of South Africa: A Key Idiom of Personal and Interpersonal Distress. Cult Med Psychiatry. 2016;40(3):383–403 | ||
Miti M, Letsaolo T, Greehy P, Mpungose C, San Baseline Research Report, AIDS Foundation of South Africa, 2011. https://www.aids.org.za/wp-content/uploads/2018/02/San-Baseline-Research-Report.pdf. Accessed October 17, 2018. | ||
Basera TJ, Takuva S, Muloongo K, Tshuma N, Nyasulu PS. Prevalence and risk factors for self-reported sexually transmitted infections among adults in the Diepsloot informal settlement, Johannesburg, South Africa. J AIDS Clin Res. 2016;07:1. | ||
den Hertog TN, Gilmoor AR. Informal care for people with chronic psychotic symptoms: four case studies in a San community in South Africa. Health Soc Care Community. 2016;25(2):538–547. | ||
Sylvain R. Structural violence and social suffering among the san in southern Africa. Indigenous Affairs. 2007;16. | ||
Ramathuba DU, Khoza LB, Netshikweta ML. Knowledge, attitudes and practice of secondary school girls towards contraception in Limpopo Province. Curationis. 2012;35(1):1–7. | ||
Maharaj P. Reasons for condom use among young people in KwaZulu-Natal: prevention of HIV, pregnancy or both? Int Fam Plan Perspect. 2006;32(1):28–34. | ||
Hoque ME. Reported risky sexual practices amongst female undergraduate students in KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med. 2011;3(1). | ||
Adler MW. Sexually transmitted infections in Europe. Eurohealth. 2006;12:3–6. | ||
de Jager GF, Prinsloo EAM, Joubert G. Use of traditional medicine versus use of the community-based primary health care clinic by the San community at Platfontein. South African Family Pract. 2010;52(6):542–547. | ||
Mwambete KD, Mtaturu Z. Knowledge of sexually transmitted diseases among secondary school students in Dar es Salaam, Tanzania. Afr Health Sci. 2006;6(3):165–169. | ||
Aliyu A, Dahiru T, Ladan A, et al. Knowledge, sources of information, and risk factors for sexually transmitted infections among secondary school youth in Zaria, Northern Nigeria. J Med Trop. 2013;15(2):102. | ||
Ramirez-Avila L, Nixon K, Noubary F, et al. Routine HIV testing in adolescents and young adults presenting to an outpatient clinic in Durban, South Africa. PLoS One. 2012;7(9):e45507. | ||
Ruikar HA. Knowledge, attitude and practices about sexually transmitted infections – a study on undergraduate college students of Mumbai. WebmedCentral. 2013;4:2–15. | ||
Amu EO, Adegun PT. Awareness and knowledge of sexually transmitted infections among secondary school adolescents in Ado Ekiti, South Western Nigeria. J Sex Transm Dis. 2015;2015:1–7. | ||
Nsuami JM, Sanders LS, Taylor SN. Knowledge of sexually transmitted infections among high school students. Am J Health Educ. 2010;41(4):206–217. | ||
de Almeida MC, Aquino EM. The role of education level in the intergenerational pattern of adolescent pregnancy in Brazil. Int Perspect Sex Reprod Health. 2009;35(3):139–146. | ||
Fonner VA, Armstrong KS, Kennedy CE, O’Reilly KR, Sweat MD. School based sex education and HIV prevention in low- and middle-income countries: a systematic review and meta-analysis. PLoS One. 2014;9(3):e89692. | ||
Folasayo AT, Oluwasegun AJ, Samsudin S, Saudi SN, Osman M, Hamat RA. Assessing the knowledge level, attitudes, risky behaviors and preventive practices on sexually transmitted diseases among university students as future healthcare providers in the central zone of Malaysia: a cross-sectional study. Int J Environ Res Public Health. 2017;14(2):159. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.