Back to Journals » Breast Cancer: Targets and Therapy » Volume 12
Knowledge and Practice of Breast Self-Examination Among Young Women in Tertiary Education in Addis Ababa, Ethiopia
Authors Dinegde NG , Demie TG , Diriba AB
Received 30 August 2020
Accepted for publication 21 October 2020
Published 3 November 2020 Volume 2020:12 Pages 201—210
DOI https://doi.org/10.2147/BCTT.S279557
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Pranela Rameshwar
Negalign Getahun Dinegde,1 Takele Gezahegn Demie,2 Abdissa Boka Diriba1
1School of Nursing & Midwifery, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 2Department of Public Health, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Negalign Getahun Dinegde Email [email protected]
Background: Breast cancer is the top cancer among women both in the developed and the developing world. Many deaths can be avoided if breast cancer can be detected and treated early. The practice of breast self-examination (BSE) is a convenient, no-cost tool that can be used regularly for detecting breast cancer at an early stage. Therefore, this study sought to assess the knowledge and practice of breast self-examination among young females in Addis Ababa, Ethiopia.
Methods: Institutional-based cross-sectional study was conducted among 358 females using a pre-tested and self-administered questionnaire. The data were cleaned and analyzed using SPSS version 23, and the descriptive statistics, linear and logistic regression were used for analysis. The possible predictors were identified using the odds ratio with a 95% confidence interval and a P-value of 0.05.
Results: Almost half of 188 (52.5%) respondents had heard about breast cancer self-examination, while the media were the main source of information. The study revealed that only as little as 47 (13.1%) respondents did appropriate BSE. While confounding factors were controlled for, the linear multivariate regression analysis indicated that the healthcare providers as information sources about BSE (β = 1.9; CI= 0.62, 2.9; p < 0.01) makes the greatest unique contribution to explaining the BSE knowledge level. Moreover, the study indicated that the more age (β = 1.4; CI=1.1, 1.8; p < 0.01) and knowledge (β = 1.34; CI=1.1, 1.64; p < 0.01) the females have, the more likely it is that they will report practicing BSE.
Conclusion: This study showed that a few females implemented regular BSE. Further implementations are needed in addressing young females, making awareness and advocacy campaigns about BSE to increase early diagnosis of breast cancer that raises the chances for successful treatment in Ethiopia.
Keywords: breast cancer self-examination, knowledge, practice, Ethiopia
Introduction
Background of the Study
Globally, breast cancer is the leading cancer-related disease both in morbidity and mortality among women, affecting about a 2.1million annually, and over half a million died in 2018 at estimation.1 While breast cancer rates are higher among women in more developed regions, rates are increasing in every region internationally, including Ethiopia.2 According to global cancer estimates of Bray et al, compared to other regions, the extents of cancer mortalities in Asia (57.3%) and Africa (7.3%) were greater than the proportions of incidence (48.4% and 5.8%, respectively) because there were various spreading of cancer categories and advanced case fatality rates in these regions. Particularly, the study indicated a higher estimated cumulative risk of dying from cancer among women in the horn of Africa (11.4%).3
According to WHO 2018 report, the prevalence of breast cancer is increasing in the developing nations as a result of a rising number of senior citizens and lifestyle-related breast cancer risk factors like eating unhealthy foods, obesity, and using harmful substances.4,5 Moreover, the occurrence is mounting in the unindustrialized nations as a result of the rising lifespan, urbanization, and embracing of western lifestyles.4 Although early detection remains the cornerstone of breast cancer control to improve outcome and survival, in low- and middle-income countries breast cancer is diagnosed in very late stages.5 Generous commitment to public education about breast cancer screening and detection types, including the timely diagnosis, would save quite a lot of women’s live.5
Breast cancer is commonly related to late diagnosis due to delayed presentation by the patient and less expectation of the disease from physicians.6,7 According to a study done in the United States,8 breast cancer incidence in young females also differs according to race and ethnicity. The study indicated that Afro- American women below age 35 have twofold the incidence of invasive breast cancer and threefold breast cancer death than young white women. Besides, the study finding showed that the young women had a poor survival rate compared to those in older women and the younger age group were significantly associated with adverse outcome. Furthermore, studies revealed an advanced stage of breast cancer presentation was higher among women with low socioeconomic status.8,9
World Health Organization (WHO) recommends developing nations those suffering the dual saddle of cervical and breast cancer to implement economical and inexpensive interventions to confront these greatly preventable diseases.10 Although there is no proof of the worth of screening through BSE, the BSE practice has been appreciated to enable women, taking concern for their health.5 BSE is a suitable and cheap means that can be implemented regularly. The American Cancer Society and other leading cancer agencies recommended the monthly practice of BSE.11,12 A country with inadequate resource facilities and poor health systems ought to promote early diagnosis programs based on breast self-exam, awareness of early signs and symptoms, and prompt referral to diagnosis and treatment.11
For the reason of scarce data compilation, the accurate occurrence rate of breast cancer in Ethiopia is unclear.13 However, according to a study done in Tikur Anbessa specialized hospital, the largest teaching hospital and the only cancer referral center in Ethiopia, among 16,622 new cancer cases registered, 3460 (21.0%) were breast cancer new cases indicating about 216 cases annually.14,15 Breast cancer cases are among the top prevalent case (31.5%), followed by cervical cancer, which accounts for 14% among women in the country.16
A mixed-method study conducted on beliefs and practice around breast cancer in Ethiopia indicated that more than half the women were age 50 years or younger.17 Although there is no high quality national cancer registry in Ethiopia, studies also indicated that the mean age of women with breast cancer was 43 years at diagnosis.18 However, considering the low incidence of the disease at a younger age, women may ignore the warning signs of the disorder that can lead to late diagnosis and poorer outcomes as it is more aggressive and less likely to react to treatment in this age group.7
The screening and diagnosis of breast cancer have not been supported by contemporary laboratory examinations in numerous healthcare facilities in Ethiopia.19 In the least developed countries like Ethiopia, BSE would be an alternative method to prevent and control breast cancer morbidities and mortalities, even though mammography is the finest screening technique. Hence, the researcher conducted this study to assess the knowledge and practice of BSE among young women in tertiary education, Addis Ababa, Ethiopia.
Materials and Methods
Study Design, Period, and Setting
An institutional based cross-sectional study was conducted at Addis Ababa University from March to April 2018. The University was established in 1950 and has ten (10) colleges: college of social sciences, college of humanities, language studies, journalism, and communication, college of development studies, college of business and economics, college of law and governance studies, college of education and behavioral studies, college of natural and computational sciences, Skunder Boghossian college of performing and visual arts, college of veterinary medicine and agriculture, and college of health sciences. There were 50,534 enrolled students in 2018, among which 16,249 were female students by then. This study focused on young educated females who came from various ethnic, cultural, and geographic areas across the country. Consequently, empowering and enhancing awareness of young women will support the Ethiopian government’s national strategy for breast cancer screening promotion.
The Study Participants and Sampling
From a total of ten colleges, the college of natural sciences, college of social sciences, and college of business and economics were selected using simple random sampling. The total sample size was allocated to each selected college by proportion to the number of students. From each selected college, the study subjects were nominated by a simple random sampling technique from a list of students obtained from the university registrar office. Accordingly, the total number of female students in the participating college was 198 (college of natural sciences), 72 (college of social sciences), and 111 (college of business and economics).
Regular undergraduate program female students attending their education during the study period and those ≥18 years were included in the study. Students who were absent in the classroom during the data collection period and those attending their education in the college of health science field were excluded from the study.
The actual sample size for the study was determined using the single population proportion formula by assuming a 5% marginal error and 95% confidence interval and the prevalence was taken from other studies conducted in the Northern part of the country (38). Accordingly, the study was conducted on the total sample size of 381 females, including the 10% non-response rate.
Variables and Measurements
The dependent variables were BSE Knowledge and practice. The independent variables in this study were: sociodemographic (age, place of residence, family education level, marital status, religion, occupation, and study year), sources of information (healthcare provider, friends, media, and others), and breast cancer history-related factors (personal history of breast cancer, family history of breast cancer, and knew someone with breast cancer). The knowledge score was recorded as a continuous scale in the SPSS and a higher score indicated better knowledge. The BSE practice was analyzed being as a dichotomous dependent variable with two values yes or no.
Operational Definitions
BSE Knowledge
The respondents’ BSE knowledge score was assessed by the 28-items knowledge questionnaire. The total score was computed out of 100 which has a range from 0 to 100. A higher score indicated better knowledge.
BSE Practice
A participant who performed BSE at least once in a month consistently was considered as properly doing breast examination.11,20
Data Collection Tool and Methods
Data was collected in Amharic language using an interviewer-administered questionnaire. In this regard, the questionnaire was translated from English to the Amharic language by a bilingual translator and then back-translated to English by another bilingual translator. Before data collection, the pre-test of the instrument was done on the target population to assess the Amharic language version of the tool to ensure meaning equivalence with the original English version.19,21–24
The content of the questionnaire comprised: 9 socio-demographic characteristics items, 6 histories and information about breast cancer items, 28 knowledge of breast self- examination items, and 8 practice of breast self- examination items. The questionnaire items include true/false, yes/no, and multiple-choice questions.
Four diploma nurses were recruited for the data collection based on previous experience in data collection and fluency in the local languages. The data were collected using a self-administered method.
Data Quality Control
Pre-testing of the questionnaire was carried out on 5% of the calculated sample at St. Mary’s university college and based on the result obtained, the necessary modification was made for the final data collection. Besides, double data entry using the EpiData entry client was done to assure data consistency.
The principal investigator closely supervised the data collection process. In addition, training was given for the data collectors on how to check data completeness, handling ethical issues, and maintaining confidentiality and privacy.
Data Processing and Analysis
The collected data was entered into and cleared using Epi-data software version 4.1.1 and then exported to SPSS version 24 for further statistical analysis. The study analysis was done by descriptive statistics and regression analysis. Continuous variables were reported as means and standard deviations. Categorical variables were described as frequencies and percentages.
The inferential statistic linear regression analysis was used to examine the association between knowledge of BSE and independent variables (place of grew up, family history of breast cancer, knew someone suffering from breast cancer, heard about BSE, parent education, information sources, and study year). In addition, binary logistic regression analysis was used to control for confounding and to see for the impact of variables of interest on the practice of BSE. Furthermore, bivariate analysis was done for each independent variable, and significant predictors at p-value < 0.2 in bivariate analysis were exported to the multivariable linear and logistic regression model.
The magnitude of the association between the independent variables (socio-demographic characters, history and information of breast cancer) with the dependent variable (knowledge and practice of BSE) was measured using a 95% confidence interval (CI) and p-values below 0.05 were considered as statistically significant.
Ethical Consideration
Ethical approval was obtained from the Research and Ethics Committee (REC) of Addis Ababa University, College of Health Sciences. The official letter of cooperation was written to all selected colleges. All subjects provided written informed consent, and the study was conducted in accordance with the Declaration of Helsinki.
Results
The Socio-Demographic Characteristics of the Participants
From the total of 381 calculated sample size, the study included 358 participants with a 93.96% response rate. Table 1 depicts the socio-demographic variables (age, marital status, religion, place of grew up, family education, study year, and family history of breast cancer) frequency distribution and univariate analysis with BSE practice. The respondents’ age mean (SD) was 20.84 ( ,
, ,
, and
and  2) years, and the majority of the participants were single 305 (85.2%), orthodox Christian 240 (67%), and grew up in urban setting 278 (77.7%). The univariate analysis indicated that age (p-value < 0.01), place of grew up (pvalue=0.025) and study year (pvalue= 0.013) revealed statically significant association with BSE.
2) years, and the majority of the participants were single 305 (85.2%), orthodox Christian 240 (67%), and grew up in urban setting 278 (77.7%). The univariate analysis indicated that age (p-value < 0.01), place of grew up (pvalue=0.025) and study year (pvalue= 0.013) revealed statically significant association with BSE.
 |
Table 1 Correlation of Demographic Characteristics and the Practice of BSE Based on Univariate Analysis (n=358) |
Respondents’ Information About BSE
In this study, the majority of 337 (94.1%) of the participants had no family history of breast cancer. Among the participants who had a family history of breast cancer, a large number of 16 (76.2%) of respondents reported that they had extended family history while the rest 5 (23.8%) stated nuclear family history. Amid the 358 participants, only 10 (2.8%) reported a personal history of breast cancer. Almost half 188 (52.5%) of the respondents had heard about breast cancer self-examination, amongst which mass media (television and radios) was the commonest 104 (55.5%) source of information, followed by healthcare providers and friends, 55 (29.2%) and 29 (15.3%) respectively.
Moreover, 172 (48%) of the participants knew the types of breast cancer screening methods, among which slightly above half 95 (55.2%) of them stated BSE, followed by clinical breast examination and mammography, 48 (27.9%), and 29 (16.9%) respectively.
Practice of BSE
Among the respondents studied, 88 (22.9%) have ever performed BSE, however, only 47 (13.1%) did appropriate BSE. Twenty-five (29.8%) of the respondents practiced BSE once in a month, followed by 22 (26.2%) once in a week. Concerning the reason why performing the BSE, 39 (46.4%) of them reported for early detection. Among the participants ever performed BSE, a large number (90.5%) of the respondents indicated that they started practicing BSE before celebrating 25th years of age. Moreover, 32 (38.1%) of the females practiced BSE when it comes to their mind, followed by 30 (35.7%) practiced BSE two to three days after a session of menstruation (Table 2).
 |
Table 2 Description of Time and Intention of Performing BSE |
Regarding the reason why participants did not perform the BSE, 68 (24.6%) reported that they did not know how to do it, 67 (24.3%) stated due to forgetfulness, and 63 (22.8%) of them mentioned that they did not have any breast problem (Figure 1).
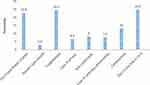 |
Figure 1 The reason why the females did not practice BSE. |
Factors Associated with the Assessment of Knowledge and Practice of BSE
The effect of several factors done by multiple linear regression to predict the extent of BSE knowledge (Table 3). R square statistic in the model described 14.1% of the variance, and the maximum value for Cook’s distance was 0.02. Tolerance, how much of the variability of the specified independent was not explained by the other independent variables in the model, is calculated for each variable. All the tolerance scores in the model were greater than 0.10, suggesting there were no possibilities of multicollinearity. Besides, Variance inflation factor (VIF) values were less than 10 that support the tolerance test result as there were no multicollinearity among independent variables.
 |
Table 3 Predictors of Knowledge of BSE Based on Adjusted Multiple Linear Regression Analysis Model (n=358) |
After the variance explained by all other variables in the model was controlled, the information sources about BSE make the greatest unique contribution to explaining the knowledge level, particularly participants those received health information from healthcare providers (β = 1.9; CI= 0.62, 2.9; p < 0.01). In addition, a study year (β = 0.14; CI= 0.3, 2.02; p < 0.01) was a significant predictors of the degree of BSE knowledge. Similarly, for the two significant variables (information source from healthcare provider and friends), the β values were positive. These indicated that a participant who heard about BSE through healthcare workers and friends high likely report having a good knowledge of BSE. The variable measuring the participants’ study year showed a positive β value (0.14). This indicated that the more women advance in the study year, the more likely it is that they will report having good knowledge about BSE.
Logistic regression analyzed the impact of a set of predictors on a BSE practice with a dichotomous variable (Table 4). Accordingly, the major factors influencing the participants’ BSE practice were age (β = 1.4; CI=1.1, 1.8; p < 0.01) and knowledge (β = 1.34; CI=1.1, 1.64; p < 0.01). Place of grew up, family history of breast cancer, information sources about BSE, and year of the study did not contribute significantly to the model. Moreover, the study indicated that the more age and knowledge the females have, the more likely it is that they will report practicing BSE.
 |
Table 4 Predictors of the Practice of BSE Based on Adjusted Multivariate Binary Logistic Regression Analysis Model (n=358) |
Discussion
The study indicated that a quarter of participants have ever performed BSE, nonetheless as little as 47 (13.1%) females implemented regular BSE. Studies conducted in Malaysia, Tamil Nadu, Cameroon, Iran, and Nigeria indicated comparable findings.22,25,27–30 Besides, this finding supports the researches done in Ethiopia which described a small number of the participants had performed BSE.19–21,31–33 On the other hand, the study conducted in Northern and southern Ethiopia found that 37% and 45.6% of the participants had practiced BSE respectively, which is slightly higher than the current study. Furthermore, other studies conducted in Iraq and Ghana reported 48.3%, and 80% of respondents practiced BSE respectively, which is in contrary to the present study.34,35 The reason for the inconsistency could be due to the health workers and health science students were the study population in the previous studies.36,37
This study revealed that half of the participants had heard about BSE. This is in line with studies done in Nigeria and Ethiopia that showed nearly similar findings.20,27,31,32 An analysis done on BSE among women in developing countries reported also nearly three-quarters of participants had previously heard about BSE.38 In contrast, the finding is also contrary to the studies done in Iraq and Ghana which indicated that a very large number of participants had heard of BSE.34,35 Moreover, the study done on predictors of BSE among female teachers in Ethiopia revealed only 52 (16.5%) of participants ever heard about BSE.21
Regarding the sources of information about BSE, the majority mentioned mass media (television and radios) was the commonest source of information in the current study. This confirmed the other study done in the country which revealed the main source of information was mass media,20 additionally research conducted in Ghana, Iraq, and Saudi also found out the main source of information being mass media.34,35,39
As stated by literature, the best time to do a monthly self-breast exam was about 3 to 5 days after the period starts.11 In the current study, as many as 38.1% of the females practiced BSE when it comes to their mind, and a third of them two to three days after a session of menstruation. Contrarily, slightly improved result from Ghana described that when respondents were asked about the appropriate time for performing BSE, more than half stated that the appropriate time to perform BSW was some days after menstruation, and a quarter stated that there was no particular time to perform BSE.35 Furthermore, a study done in Cameroon indicated as little as 10 (7%) participants knew the appropriate time to perform a BSE was a few days after menstruation.30
The majority stated the reason for performing BSE was for early detection and treatment, followed by health provider recommendation, fear of developing breast cancer, family history, and the previous breast problem. Likewise, the finding from Malaysia is closely in agreement with this study as the majority identified the reason was to check their breast regularly, accompanied by family and personal history.25 Moreover, the greatest reason for not practicing BSE was lack of knowledge of how to perform the technique correctly, then forgetfulness, and did not have any breast problem. This is in agreement with the studies done in Ethiopia, Iran, and Iraq.19,20,29,34,36
Regarding the associated factors of knowledge about BSE, healthcare workers, and friends as information sources about BSE and advanced study year were statistically associated with BSE knowledge. This is in line with the study done by Kumarasamy, Veerakumar28 in Tamil Nadu which was found to be significantly associated with educational attainment. Likewise, this finding confirmed the study done in Ethiopia which indicated as the year of stay in the University increases the knowledge about cancer increases.19 Moreover, a significant association was found between academic levels with knowledge of students regarding breast cancer self-examination. Although media was the most common source of information about the screening method, it was not statistically associated with the participants’ BSE knowledge. The reasons could be the transmission contents, regularity, and other limitations of nature of media like lack of face to face communications.
Significant knowledge insufficiencies can have a detrimental effect on the education of women on screening and early detection practices.40 In the current study, knowledge about BSE was found to be the major predictor for the practice of BSE, after other factors (place of grew up, family history of breast cancer, knew someone suffering from breast cancer, heard about BSE, family education, source of information source about BSE, and study year) were being controlled for. This finding supports the theory of taxonomy of educational objectives that displayed the learners’ manifest application by performing known concepts to certain and concrete situations, the learners manifest practice by translating known concepts.41 This outcome maintenances the investigation conducted by Birhane, Mamo,21 and Birhane, Alemayehu20 on predictors and practice of BSE among females in Ethiopia. Also, this finding is in line with the study done in Iran.29 Several studies also indicated that awareness deficit is the preceding bottleneck for having breast screening practice.33,42
Besides, the present study showed that age was statistically associated with the practice of BSE. A study done on barriers to BSE practice among Malaysian female students reported consistent results with this study.25 Likewise, a study done in Iran on the need for greater women awareness of warning signs and effective breast screening methods revealed matching results.29 The place of grew up, family history of breast cancer, knew some with breast cancer, and source of information about breast cancer did not show significant association with the practice of BSE, which is parallel with other study findings.43 According to a study conducted at Mexico-US Border on the impact of a family history of breast cancer on early detection practices, there were no significant differences between females with and without a family history in compliance with screening practice.44 On the contrary, some studies have indicated a positive association between positive family history of breast cancer and screening compliance.33 The finding is dreadful given females with a family history of breast cancer have a higher risk of acquiring breast cancer over their lifetime.
The study instrument was comprehensive, pretested, and modified before actual data collection. The data were double entered and validated using the latest EpiData entry client before analysis. However, since the findings are restricted to a sample of female university students, thus limiting their generalizability to the whole country. The research may also be limited by the fact that these were based on participants’ self-report thus the estimate of knowledge concerning how to perform a BSE may be an overestimate.
Conclusion
Overall, a few females implementing BSE regularly. The knowledge and practice of BSE could be considerably lower in communities having a more diversified female population and living in remote areas in the country. Further implementations are needed in addressing young females, making awareness and advocacy campaigns about BSE to increase early diagnosis of breast cancer, which raises the chances for successful treatment in Ethiopia.
Moreover, we have found that some studies indicated there were no significant differences between females with and without a family history in compliance with screening practice, including our study. On the contrary, some studies have indicated a positive association between positive family history of breast cancer and screening compliance. Therefore, we recommend researchers on the impact of a family history of breast cancer on early detection practices for future study.
Abbreviations
ANOVA, analysis of variance; ORADJUSTED, adjusted odds ratio; BSE, breast self-examination; CI, confidence interval; ORCRUDE, crude odds ratio; REC, Research and Ethics Committee; SPSS, Statistical Package for the Social Sciences; VIF, variance inflation factor; WHO, World Health Organization.
Data Sharing Statement
The datasets used and analyzed during the current study are available from the author on reasonable request.
Acknowledgment
We are grateful to Addis Ababa University for the provision of support to this research project.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funder role in the design, data collection, analysis, and interpretation of the study and in writing the manuscript.
Disclosure
The authors declare that there are no competing interests.
References
1. WHO. Breast cancer. 2018 [cited October 31, 2018]; Available from: http://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/.
2. Ethiopia W. Noncommunicable disease. 2014 [cited October 31, 2018]. Available from: https://afro.who.int/countries/ethiopia.
3. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
4. WHO. Africa cancer. 2018 [cited October 31, 2018]. Available from: https://afro.who.int/health-topics/cancer.
5. WHO. Breast cancer: prevention and control. 2018 [cited October 31, 2018]. Available from: http://www.who.int/cancer/detection/breastcancer/en/.
6. Simmons PS, Jayasinghe YL, Wold LE, et al. Breast carcinoma in young women. Obstet Gynecol. 2011;118(3):529. doi:10.1097/AOG.0b013e31822a69db
7. Clinic C. Breast cancer in young women. 2018. Available from: https://my.clevelandclinic.org/health/articles/16805-breast-cancer-in-young-women.
8. Anders CK, Johnson R, Litton J, et al. Breast cancer before age 40 years. Semin Oncol. 2009;36(3):237–249. doi:10.1053/j.seminoncol.2009.03.001
9. Torre LA, Islami F, Siegel RL, Ward EM, Jemal A. Global Cancer in Women: Burden and Trends. AACR; 2017.
10. WHO. Breast cancer control. 2018 [cited October 31, 2018]. Available from: http://www.who.int/cancer/detection/breastcancer/en/index3.html.
11. Breastcancer.org. Breast self-exam. 2018. Available from: https://www.breastcancer.org/symptoms/testing/types/self_exam.
12. society, A.c. Clinical breast exam, and breast self-exam. 2018.
13. Gemta E, Bekele A, Mekonen W, et al. Patterns of breast cancer among Ethiopian patients: presentations and histopathological features. J Cancer Sci Ther. 2019;11(2):038–042. doi:10.4172/1948-5956.1000581
14. Abate Y, Yilma Z, Assefa M, Tigeneh W. Trends of breast cancer in Ethiopia. Int J Cancer Res Mol Mech. 2016;2(1):1.
15. Assefa M. Ethiopia - Addis Ababa City cancer registry. Afr Cancer Registry Netrk. 2014.
16. Timotewos G, Solomon A, Mathewos A, et al. First data from a population based cancer registry in Ethiopia. Cancer Epidemiol. 2018;53:93–98. doi:10.1016/j.canep.2018.01.008
17. De Ver Dye T, Bogale S, Hobden C, et al. A mixed-method assessment of beliefs and practice around breast cancer in Ethiopia: implications for public health programming and cancer control. Glob Public Health. 2011;6(7):719–731. doi:10.1080/17441692.2010.510479
18. Getu MA, Kassaw MW, Tlaye KG, Gebrekiristos AF. Assessment of breast self-examination practice and its associated factors among female undergraduate students in Addis Ababa University, Addis Ababa, Ethiopia, 2016. Breast Cancer. 2019;11:21.
19. Segni MT, Tadesse DM, Amdemichael R, Demissie HF. Breast self-examination: knowledge, attitude, and practice among female health science students at Adama Science and Technology University, Ethiopia. Gynecol Obstet. 2016;6(368):932–2161.
20. Birhane K, Alemayehu M, Anawte B, et al. Practices of breast self-examination and associated factors among Female Debre Berhan University students. Int J Breast Cancer. 2017;2017:6. doi:10.1155/2017/8026297
21. Birhane N, Mamo A, Girma E, et al. Predictors of breast self - examination among female teachers in Ethiopia using health belief model. Arch Public Health. 2015;73(1):39. doi:10.1186/s13690-015-0087-7
22. Oladimeji KE, Tsoka-Gwegweni JM, Igbodekwe FC, et al. Knowledge and beliefs of breast self-examination and breast cancer among market women in Ibadan, South West, Nigeria. PLoS One. 2015;10(11):e0140904–e0140904. doi:10.1371/journal.pone.0140904
23. Robb K, Stubbings S, Ramirez A, et al. Public awareness of cancer in Britain: a population-based survey of adults. Br J Cancer. 2009;101(S2):S18. doi:10.1038/sj.bjc.6605386
24. Stubbings S, Robb K, Waller J, et al. Development of a measurement tool to assess public awareness of cancer. Br J Cancer. 2009;101(S2):S13. doi:10.1038/sj.bjc.6605385
25. Akhtari-Zavare M, Juni MH, Ismail IZ, et al. Barriers to breast self examination practice among Malaysian female students: a cross sectional study. SpringerPlus. 2015;4(1):692. doi:10.1186/s40064-015-1491-8
26. Al-Sharbatti SS, Shaikh RB, Mathew E, Al-Biate MA. Assessment of breast cancer awareness among female university students in Ajman, United Arab Emirates. Sultan Qaboos Univ Med J. 2014;14(4):e522–e522.
27. Balogun MO, Owoaje ET. Knowledge and practice of breast self-examination among female traders in Ibadan, Nigeria. Ann Ib Postgrad Med. 2005;3(2):52–56.
28. Kumarasamy H, Veerakumar AM, Subhathra S, et al. Determinants of awareness and practice of breast self examination among rural women in Trichy, Tamil Nadu. J Midlife Health. 2017;8(2):84. doi:10.4103/jmh.JMH_79_16
29. Montazeri A, Vahdaninia M, Harirchi I, et al. Breast cancer in Iran: need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med. 2008;7(1):6. doi:10.1186/1447-056X-7-6
30. Sama C-B, Dzekem B, Kehbila J, et al. Awareness of breast cancer and breast self-examination among female undergraduate students in a higher teachers training college in Cameroon. Pan Afr Med J. 2017;28(1):164. doi:10.11604/pamj.2017.28.91.10986
31. Kassa RT, Wakjira HT, Gebremariam MB, Tullu SA, Shehissa NK. Breast cancer knowledge and breast self-examination practice among female students in Rift Valley University, Adama campus, Adama, Ethiopia, 2017. J Womens Health Care. 2107;6(5).
32. Abeje S, Seme A, Tibelt A. Factors associated with breast cancer screening awareness and practices of women in Addis Ababa, Ethiopia. BMC Women Health. 2019;19(1):4. doi:10.1186/s12905-018-0695-9
33. Dagne AH, Ayele AD, Assefa EM, Kwenti TE. Assessment of breast self- examination practice and associated factors among female workers in Debre Tabor Town public health facilities, North West Ethiopia, 2018: cross- sectional study. PLoS One. 2019;14(8):e0221356. doi:10.1371/journal.pone.0221356
34. Alwan NAS, Al Attar WM, Eliessa RA, Madfaic ZA, Tawfeeq FN. Knowledge, attitude, and practice regarding breast cancer and breast self-examination among a sample of the educated population in Iraq. East Mediterr Health J. 2012;2012:337–345.
35. Sarfo L, Awuah-Peasah D, Acheampong E, Asamoah F. Knowledge, attitude, and practice of self-breast examination among female university students at Presbyterian University College, Ghana. Am J Res Communication. 2013;1(Suppl 11):395–404.
36. Azage M, Abeje G, Mekonnen A. Assessment of factors associated with breast self-examination among health extension workers in West Gojjam Zone, Northwest Ethiopia. Int J Breast Cancer. 2013;2013.
37. Minasie A, Hinsermu B, Breast Self-examination AA. Practice among female health extension workers: a Cross-Sectional Study in Wolaita Zone, Southern Ethiopia. Rep Syst Sex Disord. 2017.
38. Suh MAB, Atashili J, Fuh E, et al. Breast self-examination and breast cancer awareness in women in developing countries: a survey of women in Buea, Cameroon. BMC Res Notes. 2012;5(1):627. doi:10.1186/1756-0500-5-627
39. Ibnawadh S, Alawad M, Alharbi S, et al. Knowledge, attitude and practice of breast self-examination among females in medical and non-medical colleges in Qassim University. J Health Spec. 2017;5(4):219. doi:10.4103/jhs.JHS_137_16
40. Ramathuba DU, Ratshirumbi CT, Mashamba TM. Knowledge, attitudes and practices toward breast cancer screening in a rural South African community. Curationis. 2015;38(1):1–8.
41. Forehand M. Bloom’s taxonomy. Emerging Perspect Learn Teach Technol. 2010;41(4):47–56.
42. Agide FD, Garmaroudi G, Sadeghi R, et al. How do reproductive age women perceive breast cancer screening in Ethiopia? A qualitative study. Afr Health Sci. 1970;19(4):3009–3017. doi:10.4314/ahs.v19i4.22
43. Hamad KJ. Knowledge of breast cancer risk factors and practice of breast self examination among female students of soran technical institute. Poly J. 2018;8(3):203–218. doi:10.25156/ptj.2018.8.3.288
44. Bird Y, Banegas MP, Moraros J, King S, Prapasiri S, Thompson B. The impact of family history of breast cancer on knowledge, attitudes, and early detection practices of Mexican women along the Mexico-US border. J Immigr Minor Health. 2011;13(5):867–875.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
