Back to Journals » Clinical Ophthalmology » Volume 17
Kahook Dual-Blade Goniotomy with and without Phacoemulsification in Medically Uncontrolled Glaucoma
Authors Barkander A , Economou MA , Jóhannesson G
Received 9 March 2023
Accepted for publication 20 April 2023
Published 12 May 2023 Volume 2023:17 Pages 1385—1394
DOI https://doi.org/10.2147/OPTH.S409375
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Anna Barkander,1 Mario A Economou,2,3 Gauti Jóhannesson1,4,5
1Department of Clinical Sciences, Ophthalmology, Umeå University, Umeå, Sweden; 2Division of Ophthalmology and Vision, Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden; 3Department of Ophthalmology, Capio Sophiahemmet Hospital, Stockholm, Sweden; 4Wallenberg Centre for Molecular Medicine, Umeå University, Umeå, Sweden; 5Department of Ophthalmology, University of Iceland, Reykjavik, Iceland
Correspondence: Anna Barkander, Department of Clinical Sciences, Ophthalmology, Umeå University, Umeå, SE-901 85, Sweden, Tel +46 63 15 30 00, Email [email protected]
Purpose: To evaluate the 2-year efficacy and safety of Kahook dual-blade (KDB) goniotomy in patients with medically uncontrolled glaucoma.
Methods: This was a retrospective case-series study of 90 consecutive patients with primary open-angle glaucoma (POAG) or pseudoexfoliation glaucoma (PEXG) that underwent KDB goniotomy alone (KDB-alone group) or KDB goniotomy in combination with phacoemulsification (KDB-phaco group) during 2019– 2020. All patients were uncontrolled on three or more medications. Surgical success was defined as an IOP reduction ≥ 20% and/or a reduction of one or more medications at 24 months. We also report IOP levels and number of medications from baseline to 24 months, as well as the need for further glaucoma interventions.
Results: At 24 months, mean IOP had reduced from 24.8± 8.3 to 15.0± 5.3 mmHg in the KDB-alone group (P< 0.001) and from 22.3± 5.8 to 13.9± 3.0 mmHg in the KDB-phaco group (P< 0.001). Medications had reduced from 3.5± 0.6 to 3.1± 0.9 in the KDB-alone group (P=0.047) and from 3.3± 0.5 to 2.3± 1.1 in the KDB-phaco group (P< 0.001). An IOP reduction ≥ 20% and/or a reduction with one or more medications was achieved by 47% of eyes in the KDB-alone group and by 76% of eyes in the KDB-phaco group. Eyes with PEXG and POAG responded equally well to the success criteria. During the 24-month follow-up, additional glaucoma surgery or transscleral photocoagulation was performed in 28% of eyes in the KDB-alone group and in 12% of eyes in the KDB-phaco group.
Conclusion: In patients with medically uncontrolled glaucoma, KDB had a significant IOP-lowering effect after 24 months, but success rates were higher when KDB was performed in combination with cataract surgery compared to stand-alone treatment.
Keywords: Kahook dual blade, medically uncontrolled glaucoma, phacoemulsification, pseudoexfoliation glaucoma, primary open-angle glaucoma
Introduction
Glaucoma is affecting an increasing number of people worldwide, and its prevalence is estimated to reach 112 million by 2040.1 An increase in glaucoma prevalence will also increase the need for glaucoma surgery. Traditionally, filtering surgeries, such as trabeculectomies or tube shunts, have often been the chosen procedures when topical therapy is no longer sufficient to control the disease. However, filtering surgeries are demanding to perform and often require frequent follow-up. Patients may also experience long visual recovery times and are at risk of vision-threatening complications, such as hypotony, bleb-related infections, and scarring with subsequent failure.2
Therefore, there is a need for safer surgical alternatives with fewer postoperative controls that can be performed at an earlier stage of the disease. This has led to the development of microinvasive glaucoma surgery (MIGS).3–5 Kahook dual-blade (KDB; New World Medical, Rancho Cucamonga, CA, USA) surgery is one of these MIGS procedures, and it has been shown to be both effective and safe, with hyphema as the most common postoperative complication.6–8 The KDB removes a strip of the trabecular meshwork (TM) over multiple clock-hours, thereby facilitating aqueous drainage into Schlemm’s canal. Up to 75% of the aqueous drainage occurs through the TM,9 and Schlemm’s canal is therefore an interesting target for microinvasive surgical procedures. Contrary to other goniotomy-based procedures that make an incision in the TM, such as the Trabectome (Neomedix, Tustin, CA, USA),10 the KDB technique also involves removal of the excised material, which in theory reduces the risk of scarring and subsequent failure.11
KDB has shown an intraocular pressure (IOP)-lowering effect - as stand-alone and in combination with cataract surgery - in all stages of glaucoma.6,12,13 However, few studies have investigated the effect of KDB in glaucoma patients with maximal tolerated topical therapy and high preoperative IOP levels. Studies including pseudoexfoliation glaucoma (PEXG) patients are also rare, and when included, the PEXG cases have been few.6,8,13 PEXG is a prevalent form of glaucoma1,14 that is often more aggressive than primary open-angle glaucoma (POAG),15 and PEXG patients have been reported to have a higher failure rate and more complications after trabeculectomy than POAG patients.16,17 It is thus important to investigate the effect of KDB in both POAG and PEXG patients, and also to do so in eyes with maximal topical therapy and high preoperative IOP levels. The aim of this study was to investigate if KDB surgery - as stand-alone or in combination with phacoemulsification - can be a safe and effective surgical alternative in medically uncontrolled POAG and PEXG.
Methods
Data were collected from medical records of consecutive eyes with POAG and PEXG that had undergone goniotomy with a KDB - as stand-alone or in combination with cataract surgery - at the Östersund Hospital in Östersund, Sweden between September 1, 2019 and December 31, 2020. Inclusion criteria were mild–advanced POAG or PEXG with visual field progression or risk thereof due to elevated IOP despite three or more medications. To minimize bias, we included only the first operated eye in patients that had both eyes eligible. Eyes were classified according to the Hodapp–Parrish–Anderson criteria:18 early (mean deviation [MD] >6 dB), moderate (MD 6–12 dB), and advanced (MD <12 dB) glaucomatous loss. In nine eyes, visual field examination had not been performed or was unreliable, and these were classified as undetermined severity. The protocol of this study was approved by the Institutional Review Board of the Swedish Ethical Review Authority (dnr. 2121−02970) and adhered to the ethical tenets of the Declaration of Helsinki. The study being retrospective in nature and all information deidentified, informed consent was not required.
Baseline data were collected from the last preoperative visit before surgery and postoperative data at 1 week (days 2−14), 1 month (days 15−59), 3 months (days 60−120), 6 months (days 121−270), 12 months (days 271−547) and 24 months (days 548−912). Preoperative assessment and data collection included a review of the patient’s ophthalmic history, Snellen best-corrected visual acuity (BCVA), standard automatic perimetry using a Humphrey field analyzer (Carl Zeiss Meditec, Dublin, CA, USA), number of medications, and IOP measurements. Distance visual acuity was converted to the logarithm of the minimum angle of resolution before analysis, and IOP was in most cases measured using Goldmann applanation tonometry (GAT). In a few of the intermediate follow-up controls, rebound tonometry or noncontact tonometry had been used instead of GAT, but at month 24 there was only one patient that had IOP measured with noncontact tonometry. All measurements at baseline were measured with GAT.
We compared IOP levels and number of medications between eyes that received stand-alone KDB surgery (KDB-alone group) and eyes that received KDB surgery in combination with cataract surgery (KDB-phaco group), as well as between eyes with POAG and PEXG (irrespectively of whether they belonged to the KDB-alone or the KDB-phaco group). Surgical success was defined as an IOP reduction ≥20% and/or a reduction of one or more medications at 24 months without further surgery or added medications. Number of eyes requiring additional glaucoma surgery or transscleral cyclophotocoagulation (TCP) during follow-up was recorded, as well as adverse effects related to surgery, such as hyphema, IOP spike, excess inflammation, and postoperative macular edema. IOP spike was defined as an IOP elevation ≥10 mmHg from baseline or IOP level ≥30 mmHg at postoperative week 1. A postoperative hyphema was defined as blood pooling ≥1 mm in the anterior chamber within the first postoperative week. We also compared visual field MD between preoperative status and status at 24 months after surgery.
Kahook Dual-Blade Surgical Technique
All surgeries were performed by a single surgeon (AB). In the combined procedures, phacoemulsification was performed first in a standardized routine fashion. Thereafter, the anterior chamber was filled with a cohesive viscoelastic, the head of the patient turned counterclockwise, and the operating microscope turned against the surgeon to ensure an optimal view into the chamber angle. A gonioprism was placed on top of the cornea, and the KDB instrument inserted into the anterior chamber through a previously created clear corneal incision. The tip of the instrument was used to make an initial incision into the TM, and the knife was then moved in both directions, removing a third to a quarter of the TM nasally. The strip of TM was removed with forceps. Viscoelastic was evacuated with an irrigation–aspiration (IA) probe, and the eye was left with an IOP in the mid-20s to minimize blood reflux. In the stand-alone KDB procedures, a temporal incision was made, and thereafter the procedure was performed in the same manner as described above, except that a syringe with balanced salt solution was used to flush out the viscoelastic instead of an IA probe. One drop of pilocarpine 4% was also given prior to surgery in the stand-alone procedures. After surgery, patients were given a topical therapy of 0.1% dexamethasone (Isopto Maxidex) three times daily for 3 weeks, and if no contraindications were present, oral acetazolamide (Diamox) 250 mg twice daily for 3 days. Administration of IOP-lowering medications was continued after surgery, and the first decision to discontinue any medication was generally taken after the first postoperative month.
Statistical Analysis
All data were deidentified and analyzed using SPSS 28. Descriptive data are presented as means ± SD. To compare differences between groups at different time points, independent-sample t-tests or Mann–Whitney U tests were used, depending on if data were parametric or not. To compare changes from baseline, paired-sample t-tests or Wilcoxon’s signed-rank tests were used for parametric and nonparametric data, respectively. For comparison of postoperative complications, x2 or Fisher’s exact tests were performed. P<0.05 was considered statistically significant, and tests were two-tailed. Cumulative proportions of eyes that underwent reoperation were calculated using Kaplan–Meier methods and compared between groups with the Mantel–Cox log-rank test. Eyes included in the Kaplan–Meier plot that had undergone reoperation were removed from the IOP statistics for each of the visits following the reoperation.
Results
Demographics
A total of 90 patients were included, the baseline characteristics of which are shown in Table 1. All patients were Caucasian, with a mean age of 79.9±7.2 years in the KDB-alone group and 74.6±6.0 years in the KDB-phaco group (P<0.001). POAG and PEXG were equally common in both groups, as was advanced glaucoma. Eight patients had undergone a previously failed glaucoma operation or TCP in the KDB-alone group (two patients had had more than one previously failed glaucoma operation) compared with one eye in the KDB-phaco group. Anticoagulant therapy was used in 44% of patients in the KDB-alone group and in 29% of patients in the KDB-phaco group. All eyes in the KDB-alone group were pseudophakic, and the cataract operation had been performed on average 7.4±6.6 years prior to the KDB operation. At 24 months, data were not available for six patients in the KDB-alone group and two patients in the KDB-phaco group. The reasons for the missing data included death (n=4), comorbidity hindering examination (n=3), and moving to another city (n=1).
 |
Table 1 Baseline demographic and glaucoma status |
Reductions in IOP and Medications
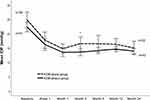
Mean IOP data for both groups at each time point are shown in Figure 1. In the KDB-alone group, mean IOP was reduced from 24.8±8.3 mmHg at baseline to 15.0±5.3 mmHg at month 24 (P<0.001). In the KDB-phaco group, mean IOP was reduced from 22.3±5.8 mmHg at baseline to 13.9±3.0 mmHg at month 24 (P<0.001). In both the KDB-alone and in the KDB-phaco groups, statistically significant reductions in IOP from baseline were seen in each of the postoperative time points at week 1, month 1, month 3, month 6, month 12, and month 24 (P<0.001). There were no significant differences in IOP levels between the groups at baseline or at 6, 12 and 24 months. At month 3, there was a small IOP difference in favor of the KDB-phaco group (P=0.031).
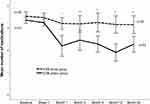
IOP-lowering medication reduction in each group at each time point is shown in Figure 2. In the KDB-alone group, the mean number of medications fell from 3.5±0.6 at baseline to 3.1±0.9 at month 24. After the first postoperative week, significant reductions from baseline were observed at month 1 (P=0.022), month 3 (P=0.011), month 12 (P=0.038), and month 24 (P=0.047), while no significant reductions were observed at month 6. In the KDB-phaco group, the mean number of medications fell from 3.3±0.5 at baseline to 2.3±1.1 at month 24. Significant reductions from baseline were observed at each postoperative time point after the first postoperative week (P<0.001). The mean number of medications was higher in the KDB-alone group than in the KDB-phaco group at all visits after the first postoperative week (Figure 2). In the KDB-alone group, 5% (one patient) was completely off medication at month 24 compared to 14% (six patients) in the KDB-phaco group. In the KDB-alone group, 6% (two patients) had a reduction of two or fewer medications at month 24 compared to 43% (21 patients) in the KDB-phaco group.
In Table 2, we report target IOP levels at baseline and at 24 months. The proportion of eyes with IOP levels ≤15, ≤18, and ≤21 mmHg at 24 months was 36%, 42%, and 48% for the KDB-alone group and 63%, 80%, and 86% for the KDB-phaco group. These IOP levels had to be reached without further surgery or added medications. IOP levels ≤12 mmHg were also achieved in 24% of eyes in both of the KDB groups. At 24 months, the success rate for an IOP reduction ≥20% and/or a reduction of one or more medications was 47% (15 eyes) for the KDB-alone group and 76% (37 eyes) for the KDB-phaco group, which was a significant difference (P=0.009).
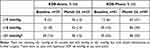 |
Table 2 Target IOP levels at baseline and at month 24 |
Reductions in IOP and Medications in Eyes with POAG and PEXG
At baseline, mean IOP was 21.7±7.3 mmHg in eyes with POAG and 24.4±6.8 in eyes with PEXG (P=0.079). Postoperative IOP levels were similar between eyes with POAG and PEXG at all postoperative time points, and there were significant IOP reductions from baseline in both groups (P<0.001). At month 24, mean IOP was 14.6±3.9 mmHg in eyes with POAG and 14.1±4.0 mmHg in eyes with PEXG. At baseline, the mean number of medications was 3.4±0.6 in eyes with POAG and 3.4±0.5 in eyes with PEXG. There were no differences in number of medications between these groups at any time point. At month 24, medications fell to 2.8±1.1 in eyes with POAG (P=0.007), and to 2.4±1.2 in eyes with PEXG (P<0.001). Regarding the success rate with an IOP reduction ≥20% and/or a reduction of one or more medications, 63% of eyes with POAG reached this goal, compared to 65% of eyes with PEXG (P=0.797). Interestingly, there were 20 eyes that had IOP reductions ≥40% at 24 months, and 75% of these eyes had PEXG. IOP reductions ≥50% and ≥60% were also observed in eleven and seven eyes, respectively, and all of these eyes had PEXG.
Safety and Adverse Events
Goniotomy using the KDB was generally safe and well tolerated. Hyphema and IOP spikes were the most common adverse events, although they were mostly self-limited without any negative effect on the results. A hyphema occurred in 26% (nine eyes) for the KDB-alone group and in 4% (two eyes) for the KDB-phaco group, which was a significant difference (P=0.008). A total of 10 patients did not come to an appointment at the eye clinic within the first postoperative week, so it is unknown if any of these also had a hyphema. However, in the event of a large hyphema, it is likely that the patients would have contacted the clinic due to poor vision. Anticoagulant therapy was associated with the presence of hyphema in the KDB-alone group (P=0.005), but not in the KDB-phaco group (P=0.485).
An IOP spike was seen in 11% of the KDB-alone group and in 8% of the KDB-phaco group in week 1 (P=0.481). One patient in each group required an aqueous tap through the existing paracentesis at the slit lamp due to elevated IOP and a hyphema. IOP was normalized and the hyphema gradually resolved within 1 month. One patient in the KDB-alone group had elevated IOP and a large hyphema that required anterior-chamber washout in the operating room on day 14 after surgery. That patient had advanced PEXG, cardiovascular disease, and diabetes, and was also on anticoagulant therapy. One patient in the KDB-phaco group had excess postoperative inflammation requiring corticosteroids beyond the third postoperative week, and one patient (also in the KDB-phaco group) developed a postoperative macular edema, which resolved within 3 months.
Within 24 months, additional glaucoma surgery or TCP was performed in 28% (11 eyes) in the KDB-alone group and in 12% (6 eyes) in the KDB-phaco group. Uncontrolled IOP or failure to achieve target IOP levels were the main reasons for additional surgery, and most of these eyes had moderate or advanced glaucoma. Figure 3 displays Kaplan–Meier cumulative survival by group. Eyes in the KDB-alone group were more likely to undergo further glaucoma surgery or TCP than eyes in the KDB-phaco group (P=0.026, log-rank test). However, in the KDB-alone group, eight patients had had a previously failed glaucoma operation or TCP compared to one patient in the KDB-phaco group. Five of those eight patients in the KDB-alone group went on to have further surgery or TCP again within 2 years after the KDB operation.
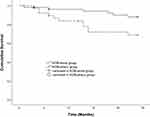 |
Figure 3 Kaplan–Meier cumulative survival in the KDB-alone and KDB-phaco groups. Notes: Eyes in the KDB-phaco group were less likely to need further surgery within 24 months (P=0.026, log-rank test). |
Visual field status at month 24 showed that patients in the KDB-alone group had a worsening in mean MD from −13.7±5.6 to −16.6±6.7 at month 24 (n=14, P=0.019). However, a worsening in MD was observed only in advanced glaucoma and not in mild or moderate disease. In the KDB-phaco group, MD was overall stable: −11.4±7.8 preoperative and −10.8±8.3 at month 24 (n=39, P=0.129). Even in patients with advanced glaucoma, MD remained stable in the phaco-KDB group: −17.9±6.5 preoperative and −17.8±1.5 at month 24 (n=18, P=0.955) However, there were 14 patients in the KDB-alone group and six patients in the KDB-phaco group that lacked visual field data at month 24 due to death (n=4), moving to another city (n=1) or comorbidities (n=15), and so lacked visual field examination data. Patients that had further surgery within 24 months were also excluded from assessment of visual field status at month 24 (n=17).
Discussion
In this study, we demonstrate that goniotomy with KDB can be a surgical alternative in medically uncontrolled glaucoma. We found that 47% of eyes in the KDB-alone group and 76% of eyes in the KDB-phaco group had an IOP reduction ≥20% and/or a reduction of one or more medications at 24 months. Sieck et al reported results for the same success criteria in 69% and 72% for KDB-alone and KDB-phaco in a previous study, but with shorter follow-up and including patients with less severe glaucoma.7 Furthermore, we found that 36% of the eyes in the KDB-alone group and 63% of the eyes in the KDB-phaco group achieved postoperative IOP levels ≤15 mmHg. This result after KDB-phaco is in accordance with Hirabayashi et al, who found that two thirds of eyes with severe glaucoma achieved an IOP ≤15 mmHg six months after KDB-phaco.6
Furthermore, our comparison of the postoperative IOP levels between eyes with POAG and PEXG showed no significant differences. However, we did see higher IOP reductions in the PEXG eyes, which may partly be explained by the higher preoperative IOP levels in this group. Higher preoperative IOP levels in PEXG eyes can possibly also explain the higher success rates in PEXG eyes than in POAG eyes in some previous studies.7,8 The higher IOP reductions seen in PEXG might also be explained by greater TM resistance in these eyes,19 indicating that the effect of KDB surgery may be more successful in PEXG than in POAG eyes.
In accordance with previous studies,7,20,21 we found significant IOP reductions after KDB surgery, even though all of the patients in our study had medically uncontrolled glaucoma and some also had surgically uncontrolled glaucoma. A high percentage of patients in the KDB-alone group needed further surgery or TCP within 24 months. One explanation for this is the fact that 21% had had a previously failed glaucoma operation or TCP in this group. In the KDB-phaco group, where 2% had had a previously failed glaucoma operation, 12% needed further glaucoma surgery within 2 years after KDB-phaco. This low rate of further surgery is an important finding, suggesting that KDB surgery in combination with phacoemulsification in medically uncontrolled glaucoma can be an alternative to a primary filtering procedure. KDB-alone may also be an alternative in cases when filtering surgery is unwanted, but it is unlikely to be successful in cases of previously failed glaucoma surgery. Part of the better results after KDB-phaco than KDB-alone is probably explained by baseline differences in glaucoma status, but it is likely that the phacoemulsification procedure, which has a known IOP-lowering effect,22,23 also contributes.
In the event that an IOP-lowering effect of KDB is not sustained over time and additional surgery is needed, filtering surgery can easily be performed, since the conjunctiva has not been compromised by the KDB procedure. It is particularly beneficial to perform KDB surgery in combination with cataract surgery, as there are several advantages in having a pseudophakic eye in case filtering surgery is needed in the future. These include the fact that trabeculectomy increases the risk of cataract development,24 and if phacoemulsification is performed after a filtering procedure, it may compromise the filtering surgery due to the increased risk of scarring.25 In addition to its IOP-lowering effect, we also found a reduction in glaucoma medications for both groups, with a mean reduction of 0.4 medications in the KDB-alone group and one medication in the KDB-phaco group. However, if the goal of surgery is discontinuation of all eye drops, filtering surgery should be considered instead of a goniotomy.
Regarding safety, KDB was generally well tolerated, with IOP spikes and hyphemas as the most common complications. IOP spike was equally common in both groups, while hyphema was more common in the KDB-alone group. We do not know if this increased occurrence of hyphema was caused by the stand-alone procedure, where a balanced salt–solution syringe was used to flush the anterior chamber, instead of an IA probe as in the combined surgeries. The different composition of the demographics of the two groups may be a confounding factor, since patients in the KDB-alone group were older and to a larger extent on anticoagulant therapy. Interestingly, anticoagulation therapy was associated with hyphema in the KDB-alone group, but not in the KDB-phaco group. It has not been clearly stated before if anticoagulation therapy is a significant risk factor for hyphema after goniotomy with KDB. Sieck et al found a slight trend toward more hyphemas in anticoagulated patients, but the trend was not statistically significant.7 Still, studies with larger samples are needed to clearly define the impact of anticoagulation therapy on the risk of excessive hyphema after KDB surgery. Some blood reflux is expected after angle-based surgery and also a sign of an unobstructed outflow pathway. Postoperative hyphema can be diminished by maintaining IOP in the mid-20s for up to 2 weeks postoperatively and by avoiding activities that increase episcleral venous pressure, such as valsalva maneuver or lowering the head below the level of the heart.26
One of the goals of glaucoma treatment is to preserve the visual field. In the KDB-alone group, MD was stable in mild and moderate disease, but not in advanced disease, while in the KDB-phaco group, MD was stable even in advanced disease stages. However, a large portion of the subjects, especially in the KDB-alone group, lacked visual field data, which makes it hard to draw conclusions on visual field outcome. A majority of patients in the KDB-alone group were of old age and/or had comorbidities, affecting the ability to perform reliable visual field examinations. Old age and advanced disease stage are known risk factors for glaucoma progression.27 Performing KDB surgery in younger patients and in those with more stable disease may help preserve visual field function, as has been shown after other forms of MIGS.28,29
This study has several strengths and weaknesses. The strengths include the real-world outcomes without exclusion due to glaucoma severity or comorbidity. Patients were consecutively evaluated and there were few lost to follow-up. All operations were also performed by the same surgeon. The retrospective design is a major limitation of the study, resulting in the lack of a standardized protocol for the procedure and the follow-up controls. There were also baseline differences between the two groups, which needs to be taken into consideration when the results are interpreted. Patients in the KDB-alone group were older and had had previously failed glaucoma surgery or TCP to a higher degree compared to patients in the KDB-phaco group. Furthermore, the follow-up time was limited to 2 years, which does not provide evidence for the longer-term effect of KDB surgery. However, there are sparse previous data on goniotomy with KDB surgery beyond the first postoperative year, and our results indicate a stable IOP-lowering effect in the longer perspective.
Conclusion
This study indicates that goniotomy with a KDB, especially in combination with phacoemulsification, can safely lower IOP to clinically acceptable levels and reduce the need for glaucoma medications in all stages of medically uncontrolled glaucoma. Therefore, in eyes with glaucoma progression despite maximal topical therapy and where IOP levels in the mid-teens are deemed clinically acceptable, KDB surgery can be considered as an alternative before pursuing filtering surgery. However, studies with longer follow-up and prospective design are needed to further investigate the effect of KDB surgery, and comparative studies are also needed to compare it to other microinvasive glaucoma surgeries.
Acknowledgments
Department of Research and Development, County Council of Jämtland Härjedalen.
Funding
Financial support was provided through grants from the Jämtland–Härjedalen and Västerbotten county councils and from the Knut and Alice Wallenberg Foundation. None of the supporting organizations had any role in the design or conduct of the research.
Disclosure
Gauti Jóhannesson has received speaking honoraria and/or consulting fees from Thea, Santen, Allergan, Alcon/Novartis, and AbbVie and is an equity owner of Oculis. Mario A Economou has received lecture fees from Glaukos and New World Medical. Anna Barkander has received consulting fees from iStar Medical, Santen and New World Medical.
References
1. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
2. Pillunat LE, Erb C, Jünemann AGM, Kimmich F. Micro-invasive glaucoma surgery (MIGS): a review of surgical procedures using stents. Clin Ophthalmol. 2017;11. doi:10.2147/OPTH.S135316
3. Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol. 2016;10:189–206. doi:10.2147/OPTH.S80490
4. Soohoo JR, Seibold LK, Radcliffe NM, Kahook MY. Minimally invasive glaucoma surgery: current implants and future innovations. Can J Ophthalmol. 2014;49(6):528–533. doi:10.1016/j.jcjo.2014.09.002
5. Saheb H, Ahmed IIK. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol. 2012;23(2):96–104. doi:10.1097/ICU.0b013e32834ff1e7
6. Hirabayashi MT, King JT, An JA. Outcome of phacoemulsification combined with excisional goniotomy using the Kahook Dual Blade in severe glaucoma patients at 6 months. Clin Ophthalmol. 2019;13. doi:10.2147/OPTH.S196105
7. Sieck EG, Epstein RS, Kennedy JB, et al. Outcomes of Kahook Dual Blade Goniotomy with and without phacoemulsification cataract extraction. Ophthalmol Glaucoma. 2018;1(1):75–81. doi:10.1016/j.ogla.2018.06.006
8. Wakil SM, Birnbaum F, Vu DM, McBurney-Lin S, ElMallah MK, Tseng H. Efficacy and safety of a single-use dual blade goniotomy: 18-month results. J Cataract Refract Surg. 2020;46(10):1408–1415. doi:10.1097/j.jcrs.0000000000000263
9. Civan MM, Macknight ADC. The ins and outs of aqueous humour secretion. Exp Eye Res. 2004;78(3):625–631. doi:10.1016/j.exer.2003.09.021
10. Ting JLM, Damji KF, Stiles MC. Ab interno trabeculectomy: outcomes in exfoliation versus primary open-angle glaucoma. J Cataract Refract Surg. 2012;38(2):315–323. doi:10.1016/j.jcrs.2011.08.043
11. Seibold LK, Soohoo JR, Ammar DA, Kahook MY. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am J Ophthalmol. 2013;155(3):524–529.e2. doi:10.1016/j.ajo.2012.09.023
12. Berdahl JP, Gallardo MJ, ElMallah MK, et al. Six-month outcomes of Goniotomy performed with the Kahook Dual Blade as a stand-alone glaucoma procedure. Adv Ther. 2018;35(11):2093–2102. doi:10.1007/s12325-018-0803-0
13. ElMallah MK, Seibold LK, Kahook MY, Williamson BK, Singh IP, Dorairaj SK. 12-month retrospective comparison of Kahook Dual Blade excisional goniotomy with Istent trabecular bypass device implantation in glaucomatous eyes at the time of cataract surgery. Adv Ther. 2019;36(9):2515–2527. doi:10.1007/s12325-019-01025-1
14. Åström S, Lindén C. Incidence and prevalence of pseudoexfoliation and open-angle glaucoma in northern Sweden: i. Baseline report. Acta Ophthalmol Scand. 2007;85(8). doi:10.1111/j.1600-0420.2007.00992.x
15. Ayala M. Comparison of visual field progression in new-diagnosed primary open-angle and exfoliation glaucoma patients in Sweden. BMC Ophthalmol. 2020;20(1). doi:10.1186/s12886-020-01592-w
16. Li F, Tang G, Zhang H, Yan X, Ma L, Geng Y. The effects of trabeculectomy on pseudoexfoliation glaucoma and primary open-angle glaucoma. J Ophthalmol. 2020;2020:1–7. doi:10.1155/2020/1723691
17. Ayala M. Lower success in trabeculectomies in exfoliation compared with primary open-angle glaucoma patients in Sweden. J Glaucoma. 2021;30(5):e237–e245. doi:10.1097/IJG.0000000000001818
18. Hodapp E, Parrish RK, Douglas R, Anderson DR. Clinical Decisions in Glaucoma. Mosby Incorporated; 1993:52–61.
19. Lee RK. The molecular pathophysiology of pseudoexfoliation glaucoma. Curr Opin Ophthalmol. 2008;19(2):95–101. doi:10.1097/ICU.0b013e3282f49cda
20. Elmallah MK, Berdahl JP, Williamson BK, et al. Twelve-month outcomes of stand-alone excisional goniotomy in mild to severe glaucoma. Clin Ophthalmol. 2020:14. doi:10.2147/OPTH.S256423
21. Dorairaj SK, Seibold LK, Radcliffe NM, et al. 12-month outcomes of goniotomy performed using the Kahook Dual Blade combined with cataract surgery in eyes with medically treated glaucoma. Adv Ther. 2018;35(9):1460–1469. doi:10.1007/s12325-018-0755-4
22. Zetterström C, Behndig A, Kugelberg M, Montan P, Lundström M. Changes in intraocular pressure after cataract surgery: analysis of the Swedish National Cataract Register Data. J Cataract Refract Surg. 2015;41(8):1725–1729. doi:10.1016/j.jcrs.2014.12.054
23. Chen PP, Lin SC, Junk AK, et al. The effect of phacoemulsification on intraocular pressure in glaucoma patients: a report by the American Academy of ophthalmology. Ophthalmology. 2015;122(7):1294–1307. doi:10.1016/j.ophtha.2015.03.021
24. Vesti E. Development of cataract after trabeculectomy. Acta Ophthalmol. 1993;71(6). doi:10.1111/j.1755-3768.1993.tb08599.x
25. Nguyen DQ, Niyadurupola N, Tapp RJ, O’Connell RA, Coote MA, Crowston JG. Effect of phacoemulsification on trabeculectomy function. Clin Exp Ophthalmol. 2014;42(5):433–439. doi:10.1111/ceo.12254
26. Pratte EL, Ramachandran M, Landreneau JR, An JA. Risk factors for hyphema following Kahook Dual Blade Goniotomy combined with phacoemulsification. J Glaucoma. 2022;32:165–170. doi:10.1097/IJG.0000000000002142
27. Jammal AA, Berchuck SI, Thompson AC, Costa VP, Medeiros FA. The effect of age on increasing susceptibility to retinal nerve fiber layer loss in glaucoma. Investig Opthalmology Vis Sci. 2020;61(13):8. doi:10.1167/iovs.61.13.8
28. Laroche D, Nkrumah G, Ugoh P, Ng C. Real world outcomes of Kahook Dual Blade Goniotomy in black and afro-latinx adult patients with glaucoma: a 6-month retrospective study. J Natl Med Assoc. 2021;113(2). doi:10.1016/j.jnma.2020.09.147
29. Laroche D, Oseni J, Nkrumah G, Ng C. Clear lensectomy with Hydrus stent in black and afro-latino patients: a 1-year retrospective study. J Ophthalmol. 2022;2022:1–7. doi:10.1155/2022/8011745
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.