Back to Journals » International Medical Case Reports Journal » Volume 16
Isolated Inferior Sagittal Sinus Thrombosis in Young Patient: Rare Case Report
Authors Sheikh Hassan M , Ahmed Ibrahim A, Nakus E, Ali Adam B , Osman Sidow N , Farah Osman Hidig M , Abdi Mohamed S, Ahmed Mohamed A, Abdullahi Adani A , Mohamed YG , Gedi Ibrahim I , Abdirahman Ahmed S
Received 27 September 2023
Accepted for publication 24 November 2023
Published 29 November 2023 Volume 2023:16 Pages 791—795
DOI https://doi.org/10.2147/IMCRJ.S442061
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ronald Prineas
Mohamed Sheikh Hassan,1,2 Abdiwahid Ahmed Ibrahim,1 Engin Nakus,1 Bakar Ali Adam,1 Nor Osman Sidow,1 Mohamed Farah Osman Hidig,1 Said Abdi Mohamed,1 Abdulkadir Ahmed Mohamed,1 Abdulkamil Abdullahi Adani,3 Yahye Garad Mohamed,4 Ismail Gedi Ibrahim,4 Said Abdirahman Ahmed5
1Department of Neurology, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 2Faculty of Medicine and Surgery, Mogadishu University, Mogadishu, Somalia; 3Department of Internal Medicine, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 4Department of Radiology, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia; 5Department of Cardiology, Mogadishu Somali Turkish Training and Research Hospital, Mogadishu, Somalia
Correspondence: Abdiwahid Ahmed Ibrahim, Email [email protected]
Abstract: Cerebral venous thrombosis (CVT) is a less common type of stroke, mostly in young patients. The majority of these cases are due to thrombosis of superior sagittal sinus and transverse sinus. Isolated thrombosis of the inferior sagittal sinus is very rare. Here, we report a 22-year-old male patient with no significant past medical history who presented to the emergency department of our hospital with a convulsion, decreased level of consciousness, and right side weakness. His laboratory investigations, including the coagulation profile, were normal. A non-contrast brain CT showed a 5 × 3 cm hematoma in the left parasagittal parietal lobe with no associated midline shift or intraventricular extension. The cerebral magnetic resonance (MR) angiogram did not show any underlying aneurysm or vascular lesion. However, the cranial MR venogram showed inferior sagittal sinus thrombosis, while other cranial veins and dural sinuses were patent. The patient was admitted to the hospital and managed with low-molecular-weight heparin and warfarin sequentially. He had significant improvement (consciousness and weakness have improved, and seizures are under control). This present case illustrates a rare case of isolated cerebral venous thrombosis and also reviews the known literature on this condition.
Keywords: cerebral venous thrombosis, inferior sagittal sinus, convulsion
Introduction
Cerebral venous thrombosis is uncommon form of stroke due to the occlusion of cerebral veins or dural sinuses by way of thrombosis.1 Risk factors for cerebral venous thrombosis include prothrombotic states such as pregnancy, the postpartum period, or those on oral contraceptives. About 34% of patients with cerebral venous thrombosis have inherited or acquired thrombophilia, according to the International Study on Cerebral Vein and Dural Sinus Thrombosis (ICSVT).2,3 CVT has variable presentation. Common presentations include a progressive headache, focal neurological deficit, seizures, or altered mental status.4 Headache is the most common symptom and usually precedes other clinical symptoms or signs, followed by seizures, altered mental status, and focal neurologic deficits.5 The diagnosis of cerebral venous thrombosis is based on the clinical presentation and confirmed by neuroimaging, especially MR or CT venography. Unlike other stroke forms caused by arterial occlusion, CVT has a better prognosis when diagnosed and treated early. In one registry study containing 624 patients with a diagnosis of CVT documented eight percent mortality.6 Most cerebral venous thrombosis are due to the occlusion of the superior sagittal sinus, transverse sinus, or cortical veins. To our knowledge only very few cases of isolated inferior sagittal sinus thrombosis have been reported in the literature. Here, we describe a young male patient with isolated inferior sagittal sinus thrombosis.
Case Presentation
A 22-year-old male patient with no significant past medical history came to the emergency department of our hospital because of a convulsion, decreased level of consciousness, and right side hemiparesis for 8 hours. He had a progressive diffuse headache without associated vomiting or visual disturbance in the last few days. He had three attacks of generalized tonic clonic seizure before presentation to the emergency room. He had no previous history of seizure disorder. The patient did not have a family history of cerebral venous thrombosis or intracerebral hemorrhage. On examination, he had decreased sensorium with a GCS of 12/15. Pupils were equal and reactive to light; likewise, other cranial nerve examinations were normal. He had right side weakness with a muscle strength of 4/5 (based on MRC). His laboratory investigation, including a full blood count, extensive biochemistry panel, and coagulation parameters, were within the normal limits. Thrombophilia screenings such as protein C and S levels could not be done due to the lack of availability in our laboratory. A non-contrast brain CT demonstrated a 5 × 3 cm hematoma in the left parasagittal parietal lobe with no associated midline shift or intraventricular extension (see Figure 1). Cranial MR angiogram did not show any underlying aneurysm or vascular lesion. However, the cranial MR venogram showed lack of flow in the inferior sagittal sinus consistent with thrombosis, while the rest of the cranial veins and dural sinuses were patent (see Figure 2). The patient was admitted to the neurology ward and managed with low molecular weight heparin, followed by warfarin sequentially. Mannitol was given to reduce intracranial pressure. Levetiracetam 500 mg BIDwas given to control the seizure. After two weeks of intrahospital treatment, He had significant improvement (consciousness was back to normal, weakness had improved, and seizures were under control). The patient is now fully functional and is under flow-up in the outpatient department.
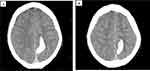 |
Figure 1 (A and B) Non-contrast brain CT showing hyperacute hematoma in the left parasagittal parietal lobe, involving the cortical and subcortical regions. |
Discussion
Cerebral venous thrombosis, which encompasses thrombosis of the cerebral veins and the dural sinuses, is a less frequent type of stroke that has been associated with higher mortality. Due to the widespread availability of magnetic resonance imaging and increased awareness, the incidence of CVT is increasing.7 Patients with CVT tend to be younger than those who experience arterial forms of stroke. According to the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT), only 8% of patients with CVT were above 65 years old, which found that the median age of patients with CVT was 37 years.8 CVTs have variable etiologies, clinical manifestations, and outcomes. Cerebral venous sinus thrombosis has been linked with hypercoagulable states, cranial or systemic infections, thyrotoxicosis, inflammatory bowel disease, cancer, dehydration, pregnancy, or the postpartum period.9,10 Head trauma, neurosurgical procedures, and bacterial meningitis may also lead to thrombosis of the cerebral veins and sinuses. Other conditions that may lead to cerebral venous thrombosis include antiphospholipid syndrome and genetic forms of hypercoagulable states such as protein C and protein S deficiency and prothrombin mutation.6 CVT can be caused by rheumatologic disorders such Behçet’s disease. Behçet’s disease is an inflammatory perivasculitis that is multisystemic, chronic, and recurrent. Despite being an uncommon symptom, neurological involvement (neuro-Behçet’s disease) is one of the most severe causes of long-term morbidity and can lead to cerebral venous thrombosis.11,12
The majority of cases of CVTs are due to thrombosis of the superior sagittal sinus, transverse sinuses, cortical veins, or a combination of sinuses. In the literature, there have been very few cases of isolated inferior sagittal sinus thrombosis. The first case of isolated inferior sagittal sinus thrombosis was reported by Elsherbiny et al in 1997,13 and since then a couple of cases have been published. A case report published by Erbas et al in 2006 reported a young female patient with a corpus callosum hematoma due to isolated inferior sagittal sinus thrombosis.14 Karakurum-Goksel et al reported a young female patient with isolated inferior sagittal sinus thrombosis due to a rare combination of elevated lipoprotein (a) and iron deficiency anemia.15
The presentation of cerebral venous thrombosis varies. Because of elevated intracranial pressure, CVT most frequently manifests as a new progressive headache. Other relatively common clinical presentations include decreased level of consciousness, papilledema, focal neurologic deficits, or seizures. Less frequent forms of presentation include cavernous sinus syndrome, SAH, and simultaneous cranial nerve palsies.16,17 Our present case presented to the emergency room with a progressive headache for days, followed by decreased level of consciousness, convulsions, and right side weakness. He had no associated visual disturbances or cranial nerve palsy.
Diagnosis is made by clinical presentation and neuroimaging. Non-contrast-brain CT may show hyperdense clot in the sinuses, venous infarction or hemorrhage, or an empty-delta sign when enhanced with contrast. Magnetic resonance imaging may demonstrate areas of infarction, hemorrhage, or associated focal swelling of brain tissue.18 The current gold standard to diagnose CVT is the combination of conventional magnetic resonance imaging with magnetic resonance venography, particularly with dynamic time-resolved angiographic techniques, such as time-resolved imaging of contrast kinetics (TRICKS) and time-resolved imaging with stochastic trajectories. The use of TRICKS provides excellent spatial resolution, as well as dynamic flow information that has not been previously obtained without more invasive studies, such as interventional angiography.19 Cerebral MR and CT venography are the best modalities to visualize a thrombosed vein or sinus. These days, digital subtraction angiography (DSA) is not required for diagnosis and is only made for patients whose endovascular management is considered.20 In the present case, a non-contrast brain CT showed hematoma in the left parasagittal parietal lobe, consistent with the territory of the inferior sagittal sinus. The cranial MR venogram demonstrated lack of flow in the inferior sagittal sinus, consistent with thrombosis, while other cranial veins and dural sinuses were patent. Parenchymal abnormalities such as vasogenic or cytotoxic edema may be observed in CVT and are occasionally seen together. Like intracerebral hemorrhage, CVT can be located in the subcortical areas, instead of the typical arterial vascular territory. Vasogenic edema, which may be reversible, develops as a result of raised retrograde venous pressure, whereas cytotoxic edema arises when the cerebral perfusion pressure falls and provokes tissue damage. Rarely, subarachnoid hemorrhage may occur during the subacute phase of CVT.21
Non-visualization of the inferior sagittal sinus may occur in up to 10% of cases of CVT. However, isolated thrombosis of the ISS is an extremely rare entity. The non-visualization of ISS and normal patency of other cerebral veins and sinuses, in addition to the clinical picture territory of the hematoma, yield the diagnosis of isolated inferior sagittal sinus thrombosis.
In conclusion, although it is rare, isolated ISS should be considered in the differential diagnosis of patients with parasagittal hematoma, especially young patients.
Ethical Approval and Patient Consent
In our institution, ethical approval is not required for case reports. However, informed written consent was obtained from the patient for publication of this case report and the accompanying images.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Weimar C, Holzhauer S, Knoflach M, et al. Cerebral venous and sinus thrombosis: S2k guidelines. Der Nervenarzt. 2019;90:379–387. doi:10.1007/s00115-018-0654-6
2. Einhäupl K, Bousser MG, de Bruijn SF, et al. Cerebral venous and sinus thrombosis. In: European Handbook of Neurological Management. 2006:501–509.
3. Ferro JM, Canhao P, de Sousa DA. Cerebral Venous Sinus Thrombosis. Evidence-Based Management of Stroke. Shrewsbury: TFM Publishing Limited; 2011:205–214.
4. Geisbüsch C, Lichy C, Richter D, Herweh C, Hacke W, Nagel S. Clinical course of cerebral sinus venous thrombosis: data from a monocentric cohort study over 15 years. Der Nervenarzt. 2014;85:211–220. doi:10.1007/s00115-013-4000-8
5. Krajíčková D, Klzo L, Krajina A, Vyšata O, Herzig R, Vališ M. Cerebral venous sinus thrombosis: clinical characteristics and factors influencing clinical outcome. Clin Appl Thromb Hemost. 2016;22(7):665–672. doi:10.1177/1076029615576739
6. Ropper AH, Klein JP, Longo DL. Cerebral venous thrombosis. N Engl J Med. 2021;385(1):59–64. doi:10.1056/NEJMra2106545
7. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;352(17):1791–1798. doi:10.1056/NEJMra042354
8. Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F. Cerebral vein and dural sinus thrombosis in elderly patients. Stroke. 2005;36(9):1927–1932. doi:10.1161/01.STR.0000177894.05495.54
9. Ferro JM, Aguiar de Sousa D. Cerebral venous thrombosis: an update. Curr Neurol Neurosci Rep. 2019;19(10):1–9. doi:10.1007/s11910-019-0988-x
10. Green M, Styles T, Russell T, et al. Non-genetic and genetic risk factors for adult cerebral venous thrombosis. Thromb Res. 2018;169:15–22. doi:10.1016/j.thromres.2018.07.005
11. Vieira RM, Nascimento FB, Barbosa Júnior AA, et al. Spectrum of central nervous system involvement in rheumatic diseases: pictorial essay. Radiologiabrasileira. 2018;51:262–267.
12. Sorgun MH, Rzayev S, Kural MA, Erdoğan S, Yücesan C. Cerebral venous thrombosis in Behcet’s disease patients compared to other causes of cerebral venous thrombosis: a retrospective study. Arch Rheumatol. 2016;31(3):248. doi:10.5606/ArchRheumatol.2016.5749
13. Elsherbiny SM, Grünewald RA, Powell T. Isolated inferior sagittal sinus thrombosis: a case report. Neuroradiology. 1997;39(6):411–413. doi:10.1007/s002340050434
14. Erbaş G, Oner AY, Akpek S, Tokgoz N. Corpus callosum hematoma secondary to isolated inferior sagittal sinus thrombosis. Acta Radiol. 2006;47(10):1085–1088. doi:10.1080/02841850600990318
15. Karakurum-Goksel B, Karaca S, Alkan O, Yildirim T. Isolated inferior sagittal sinus thrombosis caused by a rare combination of elevated lipoprotein (a) and iron deficiency anemia. Neurosci J. 2012;17(4):374–377.
16. Coutinho JM, Ferro JM, Canhao P, et al. Cerebral venous and sinus thrombosis in women. Stroke. 2009;40(7):2356–2361. doi:10.1161/STROKEAHA.108.543884
17. Goyal G, Charan A, Singh R. Clinical presentation, neuroimaging findings, and predictors of brain parenchymal lesions in cerebral vein and dural sinus thrombosis: a retrospective study. Ann Indian Acad Neurol. 2018;21(3):203. doi:10.4103/aian.AIAN_470_17
18. Ferro JM, Bousser MG, Canhão P, et al. European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis–endorsed by the European Academy of Neurology. Eur Stroke J. 2017;2(3):195–221. doi:10.1177/2396987317719364
19. Kahana A, Lucarelli MJ, Grayev AM, Van Buren JJ, Burkat CN, Gentry LR. Noninvasive dynamic magnetic resonance angiography with Time-Resolved Imaging of Contrast KineticS (TRICKS) in the evaluation of orbital vascular lesions. Arch Ophthalmol. 2007;125(12):1635–1642. doi:10.1001/archopht.125.12.1635
20. Dmytriw AA, Song JS, Yu E, Poon CS. Cerebral venous thrombosis: state of the art diagnosis and management. Neuroradiology. 2018;60:669–685. doi:10.1007/s00234-018-2032-2
21. Oliveira IM, Duarte JÁ, Dalaqua M, Jarry VM, Pereira FV, Reis F. Cerebral venous thrombosis: imaging patterns. Radiol Bras. 2022;55:54–61. doi:10.1590/0100-3984.2021.0019
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

