Back to Journals » Clinical Ophthalmology » Volume 17
Is There a Link Between Vitreous Cortex Remnants and Anatomic Outcome of Vitrectomy for Primary Rhegmatogenous Retinal Detachment?
Authors Assi A, Mansour AM , Charbaji AR , Battaglia Parodi M
Received 19 February 2023
Accepted for publication 25 May 2023
Published 29 May 2023 Volume 2023:17 Pages 1489—1496
DOI https://doi.org/10.2147/OPTH.S408871
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Alexandre Assi,1 Ahmad M Mansour,2 Abdul Razzak Charbaji,3 Maurizio Battaglia Parodi4
1Beirut Eye Clinic and VitreoRetinal Department, Beirut Eye Specialist Hospital, Beirut, Lebanon; 2Department of Ophthalmology, American University of Beirut, Beirut, Lebanon; 3Department of Statistics and Research Methodology, Lebanese American University, Beirut, Lebanon; 4Department of Ophthalmology and IRCCS Ospedale San Raffaele, University Vita-Salute, Milan, Italy
Correspondence: Ahmad M Mansour, Department of Ophthalmology, American University of Beirut, POB 113-6044, Beirut, Lebanon, Tel +9613377633, Email [email protected]
Purpose: To study the anatomic outcome of leaving vitreous cortex remnants (VCR) during pars plana vitrectomy (PPV) for primary rhegmatogenous retinal detachment (RRD).
Methods: The study comprised patients with RRD who had PPV by a single surgeon between January 2019 and December 2020 and followed for 6 months. After intravitreal injection of triamcinolone acetonide, the topographic pattern of VCR at the periphery (p) and macula (m) was divided into 2 types by extent: complete or 4 quadrants (pVCR4Q), and between 2 and 4 quadrants ≥ 2 quadrants (pVCR> 2Q), or by location > 1 inferior retinal quadrant (pVCR> 1InfQ), and at the macula (mVCR). Anatomical failure or retinal re-detachment within 6 months after surgery was the primary outcome measures. The occurrence of grade C proliferative vitreoretinopathy (PVR) and epiretinal membrane (ERM) were used as secondary outcome indicators.
Results: A 6-month prospective follow-up was performed on 103 patients. pVCR4Q was detected in 31 eyes, pVCR> 2Q in 40 eyes, pVCR> 1InfQ in 40 eyes and mVCR in 54 eyes. Recurrent RRD developed in 9 (8.7%) eyes, PVR grade C in 6 (5.8%) eyes and ERM in 11 (10.7%) eyes. According to multivariate regression analysis, the existence of any type of VCR did not correlate with anatomical failure, PVR or ERM.
Conclusion: The initial success rate of PPV and the growth of PVR or ERM do not appear to be impacted by keeping VCR.
Keywords: vitreous cortex remnants, pars plana vitrectomy, primary rhegmatogenous retinal detachment, epiretinal membrane, proliferative vitreoretinopathy
Introduction
Vitreoschisis is underdiagnosed due to the lack of routine use of triamcinolone acetonide (TA) during pars plana vitrectomy (PPV). As a result of vitreoschisis, vitreous cortical remnants (VCR) can occur at the retinal periphery (pVCR) and above the macula (mVCR).1–16 During an anomalous posterior vitreous detachment (PVD), the thickness of VCR changes depending on the plane of cleavage.17–27 Thick VCR can be removed in one piece, while thin diaphanous VCR can be removed in patches with more difficulty. The imaging of transparent VCR requires repeated injections of TA in the vitreous cavity. Preliminary data reported a high incidence of VCR in patients undergoing vitrectomy for RRD3 while other investigators suggested a link between VCR and the higher rate of PVR development,4–7 implying the need for more complete VCR removal during the initial PPV. The evidence for vigorous VCR removal in the hopes of improving the final anatomic outcome is currently counterbalanced by the necessity for more time and effort, as well as the increased risk of inner retinal trauma from retinal stretching or development of retinal breaks. Hereby, we discuss the results of a conservative approach for primary rhegmatogenous retinal detachment (RRD) that included documenting the presence of VCR and leaving VCR untouched throughout PPV. The 6-month outcome measures (surgical failure or retinal redetachment, PVR and ERM formation) after surgery will be correlated with the intraoperative VCR topographical distribution.
Methods
This was a prospective consecutive nonrandomized noncomparative study of acute primary uncomplicated RRD cases treated and followed by one surgeon (AA) between January 2019 and December 2020. Preoperatively, a non-contact SuperField NC slit-lamp lens (Volk, Mentor, OH) was used to look for the presence of a Weiss ring and confirm the presence of a so called clinically evident PVD. The extent of the detachment as well as the number of breaks were noted. But a more detailed documentation was made from the intraoperative findings using intraocular wide-angle illumination. Preoperatively in macula-on RRD and postoperatively in macula-off RRD, axial length (AL) measurements were taken using optical biometry (Aladdin Topcon, Tokyo, Japan). Eyes with AL>26mm were considered as high myopia, while eyes with AL 24–25.9mm were considered as low to moderate myopia.
Inclusion criteria included: fresh cases of RRD with symptoms of less than 10 days, presence of PVD by slit lamp biomicroscopy, a minimum follow-up of 6 months. Exclusion criteria included: absence of PVD, bilateral RRD, previous operation (laser retinopexy; pneumatic retinopexy, prior intravitreal injections), history of ocular trauma, presence of giant retinal tear, dialysis of the retina, cataract, maculopathy, diabetic retinopathy, keratoconus, uveitis, and vitreous hemorrhage. Cases of existent PVR grade>B28 were also excluded.
On all patients, a 3-port 23-gauge sutureless pars plana core vitrectomy (Geuder S4 HPS, Heidelberg, Germany) under local anesthesia was performed 3 to 4 mm from the limbus. No attempts were done to extend PVD to the periphery. Posterior vitrectomy was followed by thorough vitreous base shaving using 360° scleral depression. Then, 1 mL of triamcinolone acetonide (TA) (40 mg/mL Kenacort-A, Bristol-Myers Squibb, Spain) was injected anteriorly towards each retinal quadrant and then posteriorly and let to settle for 2 minutes. To clarify the retina view, the vitreous cavity was washed out thoroughly with a balanced salt solution. The topography of the VCR was documented in detail after the TA granules attached to it. The topographic pattern of VCR was divided into four types: by extent-4 quadrants (pVCR4Q, complete) and >2 quadrant (pVCR>2Q, incomplete or 2–4 quadrants); or by location >1 inferior retinal quadrant (pVCRinf, 1–2 inferior quadrants), and at the macula (mVCR). Perfluorocarbon liquid was not used, internal limiting membrane was not peeled and VCR around the retinal breaks or elsewhere were not removed. Internal drainage of subretinal fluid and complete fluid-air exchange was done using a flute silicone-tip needle. One row of endolaser photocoagulation surrounded the retinal tears, and this was followed by vitreous tamponade. In patients with attached retina, silicone oil was removed 3–6 months after initial surgery.
All patients underwent a complete ophthalmological evaluation by the same surgeon (AA) 1 day, 1 week, 1 month, 3 months, and 6 months after surgery. SD-OCT (3D-OCT 2000 Topcon, Topcon, Tokyo, Japan) was performed by the same operator (AA) at 1 month, 3 months and 6 months following vitrectomy.
The research protocol was authorized by Beirut Eye Specialty Hospital’s Institutional Review Board. The study adhered to the Declaration of Helsinki’s ethical requirements. A written informed consent was obtained from all patients.
Statistical Analyses
Continuous variables were expressed as mean ± standard deviation. Visual acuity data were converted to LogMAR values for statistical analysis. Chi-squared and Kruskal–Wallis tests were used to compare various clinical results in the absence and presence of VCR. Multivariate logistic regression analysis using ANOVA was performed to assess the effects of factors (primary anatomic failure or re-detachment within 6 months of PPV, PVR, and ERM formation) that were significant in the chi-squared or Kruskal–Wallis tests. The data were analyzed using the SPSS 24.0 software. Results with p<0.05 were considered statistically significant.
Results
A total of 134 eyes from 134 people who were treated in this trial were assessed. We eliminated 24 eyes due to a lack of complete follow-up (follow-up < 6 months) and another 7 eyes due to missing data. The 6-month clinical data on 103 eyes are summarized in Table 1. VCR was noted in a total of 61 eyes (59.2%): VCR was observed over the macula (mVCR) in 54 eyes (52.4%), and over the periphery (pVCR) in 40 eyes (38.8%); in other words, 37 eyes had combined mVCR with pVCR, 17 eyes had mVCR alone, and 3 eyes had pVCR alone.
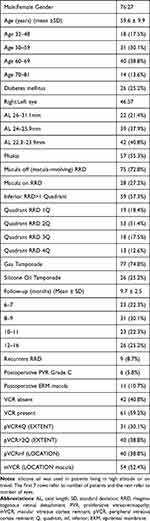 |
Table 1 Clinical Data on 103 Patients That Underwent Pars Plana Vitrectomy for Acute Primary Rhegmatogenous Retinal Detachment |
The primary outcome measure, ie, anatomic failure (retinal redetachment) occurred in 9 eyes (8.7%), while secondary outcome measures, ie, PVR Grade C and ERM occurred in 6 eyes (5.8%) and 11 eyes (10.7%) respectively. All 6 eyes with PVR developed retinal redetachment. Anatomic outcome did not correlate with any combination of VCR by ANOVA. However, anatomic outcome correlated with female gender (p=0.034) and macula off RRD (p=0.017) by ANOVA (Table 2): by gender, recurrent RRD occurred in 5 women (18.5%) vs 4 men (5.3%), while PVR occurred in 4 women (14.8%) vs 2 men (2.6%); by macular status, none (0%) of the 28 eyes with macula on developed anatomic failure or PVR. Out of 75 eyes with macula off, 8 (10.7%) had recurrent RRD and 6 (8.0%) had PVR. ERM in the macula did not correlate with mVCR (VCR macula) (p=0.345). ERM correlated inversely with age (p=0.01) by ANOVA (Table 2). PVR did not correlate with p-VCR but correlated with female gender (p=0.016) and marginally with macula off RRD (p=0.056).
 |
Table 2 Correlation Between Vitreous Cortex Remnant and Both Anatomic Outcome and Proliferative Vitreoretinopathy Using Multiple Regression Analysis by ANOVA |
Discussion
The current study is noncomparative and mostly observational since it follows eyes with (61 eyes) or without VCR (42 eyes) and tries to correlate the presence and topography of VCR to the 6-month anatomic outcome. Surgically, VCR was detected in 44–75% of cases undergoing various gauges of PPV for RRD.3,8 Histologically, Kishi et al9 found VCR in 44% of eyes with complete PVD. It has been postulated that vitreoschisis can induce various diseases related to the vitreoretinal interface including ERM.9–15 In our study, anatomic failure was recorded in 9 eyes (8.7%) with a significant (2.3-fold) female predilection. In other larger studies, the single operation success rate of small-gauge PPV was 95% in 312 eyes16 using wide-angle viewing system without scleral-depressed shaving of the vitreous base, and 84.4% in 615 eyes17 using a similar conservative approach.
The current investigation suggests no link between VCR and either anatomic failure or PVR development. The macula was found to be the most common site for VCR, followed by the peripheral vitreous. The presence of macula VCR (mVCR) did not correlate with subsequent formation of ERM, and likewise, peripheral VCR (pVCR) did not correlate with either anatomical failure or PVR. We believe that these preliminary findings indicating VCR and PVR are unrelated will be helpful to surgeons doing PPV, allowing for a quicker, safer, and less challenging surgery. Leaving VCR does not seem to prevent good anatomical results.
If our findings are confirmed, aggressive VCR shaving may not be necessary. Because PVR is unusual, a high number of eyes is needed to detect a pattern, the small number of eyes in the current series could have missed a trend for PVR. Again, the current data and findings from Tabandeh et al16 do not support the dogma that aggressive shaving of the vitreous base is essential for anatomic success. The vitreous base was previously thought to operate as a scaffold for anterior PVR, with base contraction leading to additional tears. It might be argued that cutting the vitreous base reduces vitreous volume, but it might also traumatize the retina, bringing the possible scaffold for future PVR closer to the retina. Peeling of the VCR produces considerable stretching of the vitreoretinal interface and might also damage the ILM and Muller cell footplate, leading to glial cell activation,18,19 which may predispose to formation of PVR membranes.20 Collagen type I, a key component of PVR, can be synthesized by these activated glial cells. One additional argument for a dissociation between VCR and PVR is the difference in collagen type between VCR and PVR membranes. VCR is made up of densely packed heterotypic fibrils primarily made up of type II collagens, with a tiny quantity of type V/XI and IX collagens,21 while In PVR membranes, collagen types I and III predominate.22
Rizzo et al4 collected 413 eyes with indications of p-VCR during PPV for primary RRD over a three-year period. The primary anatomical success rate in the first group without VCR removal was 91.5%, with re-detachment due to PVR occurring in 7.6% of eyes during the first three months (Table 3). Anatomical success was 95.4% in the second set of 190 eyes that had p-VCR removed, while PVR developed in 2.1% of eyes (p=0.01). This was the first and only comparative study of its kind, as well as the largest in terms of number of participants. In a retrospective comparative study by Wakabayashi et al,26 VCR removal in 86 eyes resulted in favorable functional and anatomic outcomes (90% single surgery success; PVR 9%) quite similar to their series of 101 eyes without any VCR (91% single surgery success; PVR 6%) in patients with RRD (Table 3). In a prospective non-consecutive case series of more complex RRD, van Overdam et al27 removed 23 membranes from the peripheral retinal surface just posterior to the vitreous base. The clinical aspect of the membranes varied from loose-meshed membranes suggestive of VCR (paucicellular, collagen-rich areas, with hyalocytes in primary RRD) to more fibrotic and adherent membranes resembling PVR (high cellularity comprising activated macrophages, and RPE cells in recurrent RRD). These authors suggest that VCR is the missing link to PVR formation.
 |
Table 3 Anatomic Outcomes in Eyes with Rhegmatogenous Retinal Detachment That Had VCR Removed Vs VCR Not Removed-Literature Review |
ERM development following vitrectomy for RRD has been estimated to range between 15% and 30% (Table 3).8 Similar to our current findings, Chen et al10 prospective investigation revealed no evidence that RRD patients with VCR will later develop ERM. Cho et al8 did provide data suggesting a potential relationship (2.3-fold) between ERM and VCR. They followed 80 eyes with RRD that were subject to PPV. While 3 of 20 eyes (15%) without mVCR developed ERM, 21 of 60 eyes (35%) with mVCR went on to develop ERM (p=0.091).
Strong evidence supports removing VCR in cases of RRD and high myopia because it may lessen retinal stiffness and enable stretching of the retina over a large globe. First, VCR seems to be more prevalent among high myopes.6,15,23,24 Second, it is generally accepted that removing VCR causes the retina to flatten, especially over a staphyloma.7
We contend that preserving the VCR in eyes with straightforward RRD may not promote the growth of PVR. This is because separating the VCR from the tightly adherent retina may cause retinal breaks to form or at the very least traumatize the inner retina, which would cause glial cells to become activated and proliferate, which would contribute to the formation of the PVR membrane.20 Eyes with RRD caused by round holes and without PVD rarely develop PVR.25
The number of lost to follow-up cases in this study was considered acceptable view a combination of COVID 19 pandemic (follow-up visit dropped by as much as 88% in a tertiary eye care center29), Beirut Port Ammonium Nitrate Explosion,30 and economic collapse.
The major limitations of this study include (a) a small sample size not allowing to detect a low rate PVR or ERM; (b) short follow-up; (c) selection bias for fresh simple RRD; (d) absence of an objective grading for VCR and absence of tools to measure VCR thickness; (e) absence of a comparative group where VCR was removed; (f) relatively large number of lost to follow-up. VCR can act as a source of hyalocytes and a scaffold for RPE cells, but the current data does not implicate the presence of VCR as a definite precursor for PVR and retinal re-detachment. It is still uncertain whether removing VCR reduces the rate of surgical success of PPV from re-detachment, PVR or ERM. In conclusion, additional research is needed to determine the exact role of VCR in either retinal protection or in the development of PVR.
Author Contributions
Assi: Conceptualization, Methodology, Data curation, Reviewing and Editing; Mansour: Data curation, Formal analysis, Writing—Original draft preparation; Charbaji: Data curation, Data analysis; Investigation, Reviewing and Editing; Parodi: Investigation, Writing—Original draft preparation. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study received no funding.
Disclosure
None of the authors had any financial/conflicting interests to disclose.
References
1. Sebag J. Vitreoschisis. Graefes Arch Clin Exp Ophthalmol. 2008;246:329–332. doi:10.1007/s00417-007-0743-x
2. Sebag J. Anomalous posterior vitreous detachment: a unifying concept in vitreo-retinal disease. Graefes Arch Clin Exp Ophthalmol. 2004;242:690–698. doi:10.1007/s00417-004-0980-1
3. Assi A, Khoueir Z. Prevalence of vitreous cortex remnants in eyes with primary rhegmatogenous retinal detachment undergoing vitrectomy. Retina. 2021;41:1403–1406. doi:10.1097/IAE.0000000000003056
4. Rizzo S, de Angelis L, Barca F, et al. Vitreoschisis and retinal detachment: new insight in proliferative vitreoretinopathy. Eur J Ophthalmol. 2021;32:11206721211057672. doi:10.1177/11206721211057672
5. van Overdam KA, Busch EM, Verdijk RM, Pennekamp CWA. The role of vitreous cortex remnants in proliferative vitreoretinopathy formation demonstrated by histopathology: a case report. Am J Ophthalmol Case Rep. 2021;24:101219. doi:10.1016/j.ajoc.2021.101219
6. Yamamoto N, Ozaki N, Murakami K. Triamcinolone acetonide facilitates removal of the epiretinal membrane and separation of the residual vitreous cortex in highly myopic eyes with retinal detachment due to a macular hole. Ophthalmologica. 2004;218:248–256. doi:10.1159/000078615
7. Spaide RF, Fisher Y. Removal of adherent cortical vitreous plaques without removing the internal limiting membrane in the repair of macular detachments in highly myopic eyes. Retina. 2005;25:290–295. doi:10.1097/00006982-200504000-00007
8. Cho EH, Ku HC, Il W, Lee EK. Residual vitreous cortex at the fovea during vitrectomy for primary rhegmatogenous retinal detachment repair. Retina. 2018;38:1549–1555. doi:10.1097/IAE.0000000000001734
9. Kishi S, Demaria C, Shimizu K. Vitreous remnants at the fovea after spontaneous vitreous detachment. Int Ophthalmol. 1986;9:253. doi:10.1007/BF00137539
10. Chen T, Yang C, Liu K. Intravitreal triamcinolone staining observation of residual undetached cortical vitreous after posterior vitreous detachment. Eye. 2006;20:423–427. doi:10.1038/sj.eye.6701892
11. Robbie S, Snead M. Intravitreal triamcinolone staining observation of residual undetached cortical vitreous after posterior vitreous detachment. Eye. 2007;21:285–286. doi:10.1038/sj.eye.6702533
12. Sonoda KH, Sakamoto T, Enaida H, et al. Residual vitreous cortex after surgical posterior vitreous separation visualized by intravitreous triamcinolone acetonide. Ophthalmology. 2004;111:226–230. doi:10.1016/j.ophtha.2003.05.034
13. Kimura H, Kuroda S, Nagata M. Premacular cortical vitreous in patients with a rhegmatogenous retinal detachment. Retina. 2004;24:329–330. doi:10.1097/00006982-200404000-00032
14. Hikichi T, Takahashi M, Trempe CL, Schepens CL. Relationship between premacular cortical vitreous defects and idiopathic premacular fibrosis. Retina. 1995;15:413–416. doi:10.1097/00006982-199515050-00007
15. Kato Y, Inoue M, Hirakata A. Effect of foveal vitreous cortex removal to prevent epiretinal membrane after vitrectomy for rhegmatogenous retinal detachment. Ophthalmol Retina. 2021;5:420–428. doi:10.1016/j.oret.2020.08.020
16. Tabandeh H, London NJS, Boyer DS, Flynn HW. Outcomes of small-gauge vitreoretinal surgery without scleral-depressed shaving of the vitreous base in the era of wide-angle viewing systems. Br J Ophthalmol. 2019;103:1765–1768. doi:10.1136/bjophthalmol-2018-313626
17. Wickham L, Bunce C, Wong D, Charteris DG. Retinal detachment repair by vitrectomy: simplified formulae to estimate the risk of failure. Br J Ophthalmol. 2011;95:1239–1244. doi:10.1136/bjo.2010.190314
18. Sebag J. Age-related differences in the human vitreoretinal interface. Arch Ophthalmol. 1991;109:966–971. doi:10.1001/archopht.1991.01080070078039
19. Creveling CJ, Colter J, Coats B. Changes in vitreoretinal adhesion with age and region in human and sheep eyes. Front Bioeng Biotechnol. 2018;6:153. doi:10.3389/fbioe.2018.00153
20. Charteris DG. Proliferative vitreoretinopathy: revised concepts of pathogenesis and adjunctive treatment. Eye. 2020;34:241–245. doi:10.1038/s41433-019-0699-1
21. Bishop PN. Structural macromolecules and supramolecular organisation of the vitreous gel. Prog Retin Eye Res. 2000;19:323–344. doi:10.1016/S1350-9462(99)00016-6
22. Feist RM, King JL, Morris R, et al. Myofibroblast and extracellular matrix origins in proliferative vitreoretinopathy. Graefes Arch Clin Exp Ophthalmol. 2014;252(2):347–357. doi:10.1007/s00417-013-2531-0
23. Liu HY, Zou HD, Liu K, et al. Posterior vitreous cortex contributes to macular hole in highly myopic eyes with retinal detachment. Chin Med J. 2011;124:2474–2479.
24. Itakura H, Kishi S, Li D, et al. Vitreous changes in high myopia observed by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2014;55(3):1447–1452. doi:10.1167/iovs.13-13496
25. Kuhn F, Aylward B. Rhegmatogenous retinal detachment: a reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014;51:15–31. doi:10.1159/000355077
26. Wakabayashi T, Mahmoudzadeh R, Salabati M, et al. Utility of removal of vitreous cortex remnants during vitrectomy for primary rhegmatogenous retinal detachment repair. Curr Eye Res. 2022;47(10):1444–1449. doi:10.1080/02713683.2022.2103154
27. van Overdam KA, van den Bosch TPP, van Etten PG, et al. Novel insights into the pathophysiology of proliferative vitreoretinopathy: the role of vitreoschisis-induced vitreous cortex remnants. Acta Ophthalmol. 2022;100:1749–1759. doi:10.1111/aos.15197
28. Machemer R, Aaberg TM, Freeman HM, et al. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991;112:159–165. doi:10.1016/S0002-9394(14)76695-4
29. Subathra GN, Rajendrababu SR, Senthilkumar VA, et al. Impact of COVID-19 on follow-up and medication adherence in patients with glaucoma in a tertiary eye care centre in south India. Ind J Ophthalmol. 2021;69:1264–1270. doi:10.4103/ijo.IJO_164_21
30. Mansour HA, Bitar E, Fares Y, et al. The Beirut Port explosion: injury trends from a mass survey of emergency admissions. Lancet. 2021;398(10294):21–22. doi:10.1016/S0140-6736(21)01246-0
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
