Back to Journals » Patient Preference and Adherence » Volume 17
Involuntary Hospitalizations in an Italian Acute Psychiatric Ward: A 6-Year Retrospective Analysis
Authors Di Lorenzo R , Reami M , Dragone D, Morgante M, Panini G, Rovesti S , Filippini T , Ferrari S , Ferri P
Received 25 August 2023
Accepted for publication 21 November 2023
Published 14 December 2023 Volume 2023:17 Pages 3403—3420
DOI https://doi.org/10.2147/PPA.S437116
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Rosaria Di Lorenzo,1 Matteo Reami,2 Diego Dragone,1 Martina Morgante,1 Giulia Panini,1 Sergio Rovesti,3 Tommaso Filippini,3,4 Silvia Ferrari,3,5 Paola Ferri3
1Mental Health Department and Drug Abuse, AUSL-Modena, Modena, Italy; 2School of Medicine & Surgery, Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy; 3Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy; 4School of Public Health, University of California Berkeley, Berkeley, CA, USA; 5Mental Health Department and Drug Abuse, AUSL-IRCCS Reggio Emilia, Reggio Emilia, Italy
Correspondence: Rosaria Di Lorenzo, Mental Health Department and Drug Abuse, SPDC in OCSAE, via P. Giardini, 1355, Baggiovara, Modena, 41126, Italy, Tel +393355410018, Email [email protected]; [email protected]
Purpose: We evaluated the differences between demographic (age, sex, nationality, employment, housing, schooling, support administrator), clinical (hospitalization reason, aggressive behaviour, length of hospitalization, psychiatric diagnosis and comorbidities, psychiatric medications, discharge destination, “revolving door” hospitalizations) and environmental (pre-and pandemic period) variables in voluntary (VHs) and involuntary hospitalizations (IHs) in an acute psychiatric ward during a 6-year period.
Patients and Methods: We retrospectively collected the selected variables concerning the hospitalizations of subjects over 18 years of age in the Service for Psychiatric Diagnosis and Care of Mental Health and Drug Abuse Department in Modena from 01/01/2017 to 31/12/2022.
Results: We observed a progressive and sharp reduction in the number of VHs (n = 1800; 61.41%) during the pandemic and a stability of IHs (n = 1131; 38.59%), which in 2022 became prevalent. We highlighted the following differences between VHs and IHs: an increase in hospitalization length in IHs (14.25 mean days ± 15.89 SD) in comparison with VHs (8.78 mean days ± 13.88 SD), which increased more during the pandemic; an increase in aggressive behavior in IHs, especially during the pandemic (Pearson Chi2 = 90.80; p = 0.000); a prevalence of schizophrenia and bipolar disorders (Pearson Chi2 = 283.63; p = 0.000) and more frequent maladaptive social conditions among subjects in IHs.
Conclusion: During the 6-year observation period, we underscored a trend of increasingly reduced recourse to VHs, whereas IHs increased even in the pandemic. Our results suggest that IHs in Psychiatry represented an extreme measure for treating the most severe psychopathological situations such as schizophrenia and bipolar disorders, characterized by aggressive behaviour and precarious social conditions, which needed longer stay than VHs, especially during the pandemic.
Keywords: nonadherence to treatment, involuntary psychiatric hospitalizations, pandemic, revolving door
Introduction
In most Western countries, the last 60 years have been characterized by a transition from an asylum-based psychiatric system to a community-based one, with a gradual reduction in psychiatric hospital beds and the implementation of community services. Nowadays, hospitalization in Psychiatry is resorted to only when it is strictly necessary and urgent, and where it is not possible to provide the individual with adequate home-based care, in order to avoid disrupting quality of life and favoring potential regressive behavior associated with hospitalization. Psychiatric hospitalizations no longer respond to a social need for order and custody, but to care needs that cannot be provided and guaranteed in an outpatient setting. However, rapid psychiatric deinstitutionalization has not always been followed by a simultaneous cultural and ethical change towards psychiatric treatments.1 In some countries, where the legislation is focused on “public safety” rather than individual freedoms, the use of coercive techniques and compulsory hospitalizations has been increased, reminiscent of old asylum practices.1 Many acute psychiatric conditions may require hospitalization specially when it is necessary to offer an alternative to treatment at home. These situations include the need to remove individuals from risky conditions such as highly conflictual family environments or excessively stimulating circumstances or stressful occurrences which cannot be managed elsewhere.2 In particular, hospitalization can represent a place where interpersonal relationships are focused on protection, safety, and support, and where it is possible to implement intensive pharmacological therapy. In any case, it is essential to consider the risks associated with hospitalization, including regressive behavior, feelings of frustration and social isolation, physical and psychological iatrogenic complications, and the risk of institutional dependence, which can lead to repeated and non-therapeutic hospitalizations.3 Crisis stabilization, in a safe place with a rapid discharge represents the main outcome in an acute inpatient stay.4 If hospitalization is necessary, the psychiatrist asks for the subject’s consent and full cooperation in the treatment, but if the subject refuses psychiatric hospitalization, the doctor must resort to coercive treatments only if the case meets the legal criteria for involuntary treatment.
Involuntary Hospitalizations (IHs)
Nonadherence to treatment, which can be particularly challenging in many psychiatric disorders, can be due to: psychotic symptoms, lack of illness awareness, helplessness, cognitive impairment, social isolation, conflicting familial relationship and stigma. Nonadherence to treatment is present in more than one-third of individuals with schizophrenia per annum and can increase the risk of relapse, re-hospitalization, self-harm and worsens quality of life.5 Moreover, nonadherence to treatment can result in compulsory or involuntary psychiatric treatment due to the severity of the cases and the need for urgent therapy. The use of involuntary psychiatric hospitalization varies widely between and within countries, where specific legislation enables the compulsory treatment of people with severe mental health conditions regardless of their consent. Involuntary or compulsory psychiatric treatment is a procedure mainly applied to people with mental disorders, unwilling to consent, when the intensity of the symptomatology is severe enough to jeopardize personal or social safety.6 The issue of compulsory treatment in Psychiatry is a highly debated topic due to its ethical, clinical and legal implications and is strictly regulated in each country.
Many studies have focused on the most common reasons for IHs. The most frequently associated risk factors for IHs are represented by psychotic disorders, substance abuse,7–12 and male sex, although not all authors agree on the latter point. Other risk factors include the lack of previous treatments before hospitalization,13 poor therapeutic compliance or no outpatient care for individuals with a psychiatric disorder,14–16 unemployment or lack of family support, positive psychotic symptoms, reduced insight into the illness, and police involvement in the hospitalization.17 Furthermore, IHs are generally associated with more difficult clinical management of treatment and longer duration of hospital stay compared to voluntary hospitalizations.18,19 Some studies also compared the implementation of IHs in different countries, but because of the different legislations, direct comparison is challenging.20 In a meta-analysis, Zhang et al, 2015 highlighted several differences between the Italian legislation and other international ones.21 The Italian Law is the only one among those analyzed which does not require “danger to oneself and others” as a necessary criterion for compulsory hospitalization, although also in Italy IHs are necessary in the most severe and acute clinical situations. In Germany, Denmark, and Norway, a second validating physician is not required for a compulsory hospitalization, as it is an administrative measure. In countries such as New Zealand, Germany, Denmark, Australia, Austria, and the UK, coercive medication is not permitted for hospitalized individuals. Even the use of physical restraint varies widely in terms of regulations and statistics among different countries. One study suggested correlations between involuntary psychiatric admission and several factors: length of hospital stay, aggressive behavior, occurrence of some psychopathologies, uses of coercive measures, psychiatric service activations after discharge, and quality of life.22
Some studies focusing on the efficacy of involuntary and voluntary hospitalizations highlighted that voluntarily admitted individuals were readmitted more often without any difference in hospital stay, suggesting that compulsory admissions might be helpful in reducing the risk for exacerbations in severe psychiatric disorders.23 Other authors did not find any consistent evidence that involuntary admission can reduce readmission or length of stay, but it can enhance outpatient treatment, increasing service provision.24 People involuntarily hospitalized were less likely to be victims of violent or non-violent crime, according to a Cochrane review.25
According to a recent systematic review,17 previous involuntary hospitalization and diagnosis of a psychotic disorder are the main risk factors for involuntary psychiatric hospitalizations. Another study highlighted that the presence of potential self-harm can be a greater risk for compulsory admissions than potential harm associated with other significant predictors: psychiatric syndrome, previous compulsory admissions, and the specific context of evaluation.26 On the opposite, another study underscored a decrease in involuntary hospitalizations associated with having experienced a suicide attempt and an increment associated with male gender, high-level education and psychiatric diagnosis of psychosis.27
Most studies highlighted that psychiatric IHs are often necessary to contain excessively aggressive behaviors, which are highly prevalent particularly among severe psychiatric disorders and can represent a major barrier to treatment and care, increasing institutionalization rates and reducing the quality of life of patients.28 The neuro-circuits underlying aggressive behaviors include prefrontal cortical regions and areas of the mesolimbic system, the hypothalamus, amygdala and periaqueductal gray matter. In particular, several clinical and preclinical studies highlighted that the habenula, which is a phylogenetically ancient, bilateral epithalamic structure surrounded by the third ventricle and the thalamus, is fundamental for the modulation of aggressive behaviors.28 Regarding the quality of life (QoL) in people with schizophrenia, another neuroimaging study through magnetization transfer imaging highlighted that the impairment of QoLis related to microstructural changes in an extended network (lower gray matter values compared to patients with preserved QoL in the bilateral temporal pole, bilateral insula, secondary visual cortex, vermis and cerebellum).29 A meta-analysis of structural neuroimaging across multiple psychiatric diagnoses highlighted a common neurobiological substrate in the anterior insula/dorsal anterior cingulate-based network, which may relate to executive function deficits observed across multiple psychiatric diagnoses.30 Recent advances in neuroscience focus on neural substrates to understand the neuro-pathophysiology of mental illnesses, exploring prefrontal cortex dysfunction that can result in mental illness symptoms.31 Although clinical and experimental medicine has made considerable progress in understanding pathogenesis, formulating precise diagnoses, searching for biomarkers and exploring new treatments for neuropsychiatric disorders, many issues remain unresolved in the treatment of people who suffer from a psychiatric disorder but refuse treatment.32
Objective
The objective of this study was to evaluate the differences between voluntary and involuntary hospitalizations in an acute psychiatric ward during an observation period of 6 years, comparing selected demographic, clinical and environmental variables related to the two admission states.
Materials and Methods
Study Design
This cohort study, with an observational, retrospective and single-center design, analysed demographic, clinical and environmental variables related to voluntary and involuntary hospitalizations in an acute psychiatric ward, the Service for Psychiatric Diagnosis and Care (SPDC) in Modena during an observation period of 6 years ranged between January 1, 2017, and December 31, 2022.
In accordance with the 180/78 and 833/78 Italian Laws, SPDC is located in a general hospital, provides fifteen beds for voluntary and involuntary hospitalizations of adults and is closely connected with the Mental Health and Drug Abuse Department to which it belongs.33,34
The catchment area of our SPDC includes a population of approximately 700,000 living in the province of Modena. The Mental Health and Drug Abuse Department in Modena includes seven Mental Health Centres (MHCs) and Substance Use Services (SUS).
Sample Eligibility Criteria
All adult subjects who were hospitalized at the SPDC in the Modena General Hospital during the study period were included in the sample. Individuals under the age of 18 were not considered for inclusion in the study in order to select a homogeneous sample (acceptance to hospitalization for minors is expressed by those who hold their parental authority and not by the adolescents themselves).
Study Duration
The study period spanned from January 1, 2017, to December 31, 2022. The period from the beginning of the study until March 8, 2020, is defined as the pre-pandemic period, while the period from March 9, 2020, until the conclusion of the study is defined as the pandemic period.
Selected Variables
We collected demographic variables of hospitalized subjects: age, sex, nationality, employment and housing conditions, educational level, presence of a support administrator (SA). In accordance with the Italian Law 6/2004, the functions of SA are not exclusively dedicated to individuals with mental illness and can be applied in all situations where a subject, due to physical or mental illness, is temporarily or permanently unable to take care of his/her interests and health.35
We selected the following clinical variables in order to report the characteristics of VHs and IHs in detail to better investigate the clinical issues linked to two modalities of hospitalization: clinical reason for hospitalization, aggressive behavior during hospitalization, length of hospital stay (in days), diagnosis at discharge (ICD 9-CM), substance use comorbidity, medical comorbidity, previous treatment and care, psychiatric medications and mono/polytherapy prescribed at discharge, discharge destination, revolving door (RD) hospitalizations, which are represented by 3 or more hospitalizations of an individual in a calendar year, in accordance with the literature.36,37 We considered the COVID-19 epidemic as an environmental variable and based on the moment of its onset we divided the study periods into “pre-pandemic period” (from January 1, 2017, to March 8, 2020) and “pandemic period” (from March 9, 2020, to December 31, 2022).
In Italy, on January 31, 2020, the first two cases of SARS-CoV-2 infection were confirmed, and a state of emergency was declared by the Prime Minister.38,39 This marked the beginning of the State of Emergency, which continued until April 1, 2022, involving “four waves” of infections, the implementation of social restrictions, stringent hygiene measures, and the development of a new vaccine.40
Study Procedure
Data were collected from the information system database used at SPDC and mandatory for the hospitalization of subjects. After data processing, the information was anonymized and entered into an Excel database. Each hospitalization was assigned a progressive identifying number based on the chronological order of discharge, and each subject was given a unique code following a chronological order, assigning the same value to repeated hospitalizations for the same individual. The sample of hospitalizations recorded in the study period was divided into voluntary and involuntary hospitalizations and the demographic, clinical and environmental variables of two sample subgroups were compared.
Statistical Analysis
The collected data were statistically analyzed as follows:
- Mean ± Standard Deviation (m ± SD) for continuous variables, t-test for the analysis of normally distributed continuous variables, which was previously assessed applying Shapiro–Wilk, Skewness-Kurtosis, and Shapiro-Francia tests; Non-parametric Kruskal–Wallis test for variables with non-normal distribution;
- Percentages and Pearson Chi-square test for categorical variables, using Standardized Residuals (SR) for determining what categories (cells) of variables were major contributors to reject the null hypothesis. When the absolute value of the SR is greater than 2.00, variable was a major influence on a significant Chi-square test statistic.
- Multiple logistic regression (forward and backward stepwise model) was applied between the dependent variable, hospitalization status (Voluntary=0, Involuntary=1), and the other selected variables as independent variables.
In case of occurrence of missing data, they were excluded from the analysis without implementing multiple imputation techniques. A p-value <0.05 was considered statistically significant. The data were analyzed using STATA12 (Stata Corp., College Station, TX, 2011).
Ethical Considerations
This study was conducted in accordance with the Declaration of Helsinki as a statement of ethical principles for medical research involving human subjects, including research on identifiable human material and data. The study was approved by the Ethics Committee of the Emilia Nord Health Area (Prot. 10826/2023) and authorized by AUSL-Modena (Prot. n. 688; 27/4/2023). As the study was conducted retrospectively, it was not possible to obtain written informed consent from the enrolled subjects, in accordance with the European GDPR 679/2016 and General Authorization no. 9/2016, extended by Provision no. 424/2018. Data access was granted to the study manager and collaborators, who were bound by confidentiality and data processing obligations under applicable regulations.
Results
Hospitalizations During the Observation Period
In the 6 years of the study, we collected 2954 hospitalizations at the SPDC in the Modena General Hospital referring to 1902 subjects, of which 57.05% males (n = 1085) and 42.95% females (n = 817), for a mean of 1.56 (± 2.08 SD) hospitalizations per subject in the observation period.
The sample was subdivided into voluntary hospitalizations (VHs) (n = 1800; 61.41%) and involuntary hospitalizations (IHs) (n = 1131; 38.59%). We observed a progressive decrease in the number of VHs per year during the observation period, with substantial stability of IHs (Pearson Chi2 = 51.03; p = 0.000) (Figure 1). A higher frequency of VHs was recorded in 2019 (SR = 3.08) and a higher frequency of IHs in 2022 (SR = 6.33). In the last year, a trend reversal was observed with more frequent IHs (n = 204) than VHs (n = 179) (Figure 1).
 |
Figure 1 Voluntary (VHs) and Involuntary Hospitalizations (IHs) per year in the Observation Period (Pearson Chi2 = 51.93, p = 0.000; *SR ≥ 2 or ≤ 2). |
A similar trend was observed between the pre-pandemic and pandemic periods (Pearson Chi2 = 35.79; p = 0.000) (Figure 2).
 |
Figure 2 Voluntary (VHs) and Involuntary Hospitalizations (IHs) in the Pre-pandemic and Pandemic Period. |
The frequency of RD phenomenon was higher among VHs in comparison with IHs (SR = 5.31) (Pearson Chi2 = 28.14; p = 0.000) (Figure 3).
 |
Figure 3 Revolving Door (RD) phenomenon among Voluntary (VHs) and Involuntary Hospitalizations (IHs) in the Observation Period. |
Demographic Characteristics of Hospitalized Subjects
The demographic characteristics of hospitalized subjects at their first admission to our ward during the observation period are shown in Table 1.
 |
Table 1 Demographic Variables of Hospitalized Subjects During the Observation Period |
The mean age of the subjects was 42.68 years (SD = 15.71), higher in females compared to males (44.22 ± 15.74 vs 41.22 ± 15.53) (Chi2 = 24.76; p = 0.041, Kruskal–Wallis test).
The majority of hospitalized subjects were Italians (n = 1466; 77.04%), followed by Extra-Europeans (n = 306; 16.08%) and non-Italian Europeans (n = 131; 6.88%). We observed a statistically significant difference between the two sexes among non-Italian subjects, with a predominance of the female sex between non-Italian Europeans (9.79% vs 4.70%) and of the male sex for Extra-Europeans (18,14% vs 13.34%) (Pearson Chi2 = 24.27; p = 0.000).
Only 3.07% of hospitalized subjects benefited from a support administrator. The majority of the sample was composed of unemployed individuals (25.98%) followed by employees (20.9%), whereas students (6.35%), pensioners by age (4.71%) and by disability (3.92%) were less represented.
The most frequent housing condition in our sample was living in the parental family (26.57%) followed by living in the acquired family (22.39%), whereas other locations were less frequent, as shown in Table 1. We found a statistically significant difference between males and females for housing status (Pearson Chi2 = 80.83; p = 0.000): males more frequently lived in the parental house whereas females more often lived in the acquired family, as shown in Table 1.
The most frequent educational levels in our sample were represented by middle school diploma 27.43% and high school diploma for 20.4%, with a statistically significant difference between males and females (respectively, 17.96% vs 23.65% for middle school diploma and 3.70% vs 6.03% for high school diploma) (Pearson Chi2 = 20.76; p = 0.001), as shown in Table 1.
However, it should be underlined that the data regarding employment, schooling and housing conditions are characterized by a percentage of unavailable data of over 20%.
Demographic Characteristics of Subjects Voluntarily and Involuntarily Hospitalized
We found the following statistically significant differences between the demographic characteristics of subjects voluntarily and involuntarily hospitalized (Table 2):
 |
Table 2 Demographic Variables of Subjects Voluntarily and Involuntarily Hospitalized |
- the age of individuals in IHs (42.26 m ± 15.31 SD) was higher than those in VHs (41.00 m ± 14.84 SD) in a statistically significant way (Chi2 = 4.18; p = 0.041; Kruskal–Wallis test);
- Italian nationality was prevalent (SR = 3.99) among the subjects in VHs and non-European among those in IHs (SR = 3.91) (Pearson Chi2 = 17.09; p = 0.000);
- a prevalence of individuals with disability pensions among subjects in VHs (Pearson Chi2 = 25.29; p = 0.000; 14.44% vs 9.03%; SR = 4.34);
- a higher frequency of people living alone (13.45% vs 10.22%; SR = 2.67) and a lower frequency of individuals living in community (11.68% vs 16.72%; SR = −3.74) among those in IHs (Pearson Chi2 = 28.31; p = 0.000);
- a higher frequency of people with a secondary school education level among subjects in VHs (23.33% vs 19.89%; SR = 2.19; Pearson Chi2 = 14.65; p = 0.012).
Clinical Reasons for Hospital Admissions and Discharge Diagnoses in Our Sample
The most frequent clinical reason for hospitalization was represented by acute psychosis (43.55%), followed by the risk of self-harm/attempted suicide (18.02%) and by manic excitement (15.84%), as shown in Table 3. In IHs, acute psychosis (SR = 16.30) and manic excitement (SR = 4.16) were observed more frequently, whereas other clinical reasons were less represented (Pearson Chi2 = 455.62; p = 0.000) (Table 3).
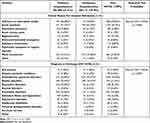 |
Table 3 Clinical Reasons for Hospital Admissions and Discharge Diagnoses in Our Sample |
The most frequent diagnosis at discharge in all hospitalizations was schizophrenia spectrum disorder (42.66%), followed by personality disorders (18.98%) and bipolar disorders (12.76%). We found that schizophrenic spectrum disorders (SR = 11.89) and bipolar disorders (RS = 4.64) were more frequent in IHs (Table 4). Conversely, depressive (SR = −9, 49), personality (SR = −8.46), adjustment (SR = −5.37) and pervasive developmental disorders (SR = −2.01) were more frequent in VHs (Pearson Chi2 = 283.63; p = 0.000), as shown in Table 4.
 |
Table 4 Clinical Variables of Voluntary and Involuntary Hospitalizations |
Clinical Variables of Voluntary and Involuntary Hospitalizations
We found the following statistically significant differences between VHs and IHs (Table 4):
- the duration of IHs (14.25 m ± 15.89 SD) was longer than that of VHs (8.78 m ± 13.88 SD) (Chi2 = 295.60; p = 0.000; Kruskal–Wallis test);
- the comorbid use of substances was less frequent in subjects voluntarily hospitalized (Pearson Chi2 = 18.79; p = 0.005), whereas alcohol abuse was more frequent among subjects involuntarily hospitalized (SR = −3.09) (Pearson Chi2 = 18.79; p = 0.005);
- previous treatment and care at MHC (SR = 2.62) and other outpatient services (SR = 2.13) was more frequent among subjects in IHs (Pearson Chi2 = 28.35; p = 0.000);
- more frequent aggressive behavior (Pearson Chi2 = 28.14; p = 0.000) and less frequent medical comorbidities among individuals in IHs (Pearson Chi2 = 7.48; p = 0.024) than those in VHs;
Seasonal differences were not statistically significant in our group.
Clinical Variables of Hospitalization Discharges in Our Sample
We found the following statistically significant differences between VHs and IHs (Table 5):
 |
Table 5 Clinical Variables of Hospitalization Discharges in Our Sample |
- the pharmacological therapy prescribed at discharge was less frequently represented by antidepressants (Pearson Chi2 = 133.05; p = 0.000), benzodiazepines (Pearson Chi2 = 6.77; p = 0.009) and other non-psychoactive drugs in IHs, whereas oral antipsychotic drugs (Pearson Chi2 = 4.11; p = 0.043) and LAI (Pearson Chi2 = 139.49; p = 0.000) were more frequently prescribed.
- more frequent destination at IHs discharge was represented by referral to MHC (36.90%) in comparison to VHs (27.02%), whereas less frequent were represented by sending to another acute psychiatric ward, psychiatric communities and SUS in comparison to VHs (Pearson Chi2 = 56.25; p = 0.000), as shown in Table 5. The data missing or concerning other unspecified categories is equal to 1.98%.
Multiple Logistic Regression
In the multiple logistic regression model (stepwise forward and backward model) between the dependent variable, VHs (=0) and IHs (=1), and the other selected variables as independent ones (Table 6), the following were statistically significantly associated:
- extra-European nationality with positive coefficient;
- living conditions in a psychiatric community with negative coefficient;
- depressive disorders, personality disorders and adjustment disorders as diagnoses at discharge with negative coefficient.
 |
Table 6 Multiple Logistic Regression (Forward and Backward Stepwise Model): Variables Statistically Significantly Associated with “Hospitalization Status” (Voluntary=0, Involuntary=1) |
Discussion
Our study aimed to analyse the demographic, clinical, environmental, and treatment adherence characteristics of hospital admissions at an acute psychiatric ward over 6 years, ranged between January 1, 2017, and December 31, 2022. Additionally, we assessed the impact of several variables on hospital admissions, including admission type, RD admissions, pre-pandemic and pandemic periods, aggression, and seasonality.
Regarding the demographic characteristics of the sample, we reported the prevalence of male sex among sample subjects. This finding is consistent with numerous studies in the literature.41,42 We also observed a sex difference in the average age of individuals since hospitalized females were older than males on average, confirming the literature report.43 We observed the prevalence of males among non-European individuals and females among non-Italian European individuals in line with the sex distribution within the foreign population residing in Emilia-Romagna region.44 Similarly, both housing condition and educational level reflect the distribution of these characteristics in the general population. Females tend to achieve higher levels of education compared to males in the general population, and more frequently live in an acquired family than males.45,46
The annual trend of admissions divided between VHs and IHs shows a progressive sharp decrease in VHs admissions, concurrent with the pandemic, while the number of IHs admissions remained relatively stable over time, surpassing the number of VHs admissions in absolute terms by the year 2022. This result clearly highlights that, despite the emergency situation, there was a portion of individuals whose admission was necessary and urgent due to acute and severe conditions, and this is in line with national and international studies,42,47–50 which reported a similar trend during pandemic with an increase in involuntary hospitalizations and coercive measures in Psychiatry. In accordance with most authors, we can hypothesize that, during pandemic, reduced availability of outpatient service activities and, at the same time, stressful conditions of isolation as well as reduced treatment of non-COVID-19 related disorders could have worsened many psychiatric disorders, in particular major psychotic disorders. This result put in evidence the need for regular psychiatric treatments and care which, if drastically interrupted or reduced as during lockdown, could negatively influence the long-term course of psychiatric conditions, fostering more dramatic and coercive interventions due to the lack of appropriate treatments.
In such an uncertain and ever-changing pandemic environment, the SPDC noticed a drastic reduction in the number of available beds, resulting in the need to prioritize less severe cases within the MHCS.47,51,52 Some of these studies also highlighted that, during the pandemic period, the number of emergency department visits for psychiatric reasons significantly decreased in the population without a previous psychiatric diagnosis, while the number of visits by individuals already receiving care at MHCs or enrolled in post-discharge programs increased. Other studies reported a 40% reduction in hospitalizations during the pandemic period compared to the previous years, although these cases tended to be more severe.53,54 Bahji et al, 2020 emphasized that this reduction was observed only in voluntary admissions, while the number of IHs remained almost unchanged compared to the pre-pandemic period.42 Other studies highlighted a worsening of the health status of individuals with a positive psychiatric history, who presented more frequent psychomotor agitation and suicide attempts during the emergency period.55 One study showed that the COVID-19 pandemic in 2020 was associated with a significant decrease in the number of hospital admissions and a greater use of seclusion.50 These results were confirmed by another study, which reported that while voluntary cases decreased considerably during the pandemic, involuntary cases increased slightly, indicating a deterioration in treatment quality during the pandemic.48 Another study further confirmed these results during the COVID-19 pandemic,49 suggesting an overall increased severity of mental disorders during the pandemic, due to deferrals of admissions or reduction of mental healthcare services interventions. This unexpected result underlines the need for regular and careful monitoring of the most serious psychiatric conditions, especially in the outpatient setting, particularly for preventing non-adherence to treatment, the main cause of involuntary hospitalization.17 Regarding the opposite trend between VHs and IHs reported by our study, we can hypothesize that the decrease in voluntary hospitalizations may have indirectly increased the need for involuntary hospitalizations, which represent the inescapable need for healthcare and treatment in serious clinical situations. Differently from other authors, we could not observe any seasonal trend which may have had a significant effect on the onset and exacerbation of psychopathology of severe mental illness and, therefore, on the need for psychiatric admissions, violence and the risk of mental health coercion.56,57 We can explain this different result with the relatively short duration of our observation period or with the particular occurrence of the pandemic epidemic, which may have distorted this possible correlation. Individuals involuntarily hospitalized in our sample were more frequently unemployed, living alone, and were more frequently treated by MHCS and social services, compared to those voluntarily hospitalized, probably due to more severe psychopathological conditions with negative impact on individual’s daily life. This result is in line with other research observations,17,22 which suggest close relationship between severity of psychiatric disorders and regressive and maladjusted behavior which result in coercive measures. Our regression model suggests that living in a protected structure such as a psychiatric community can be a protective factor for IHs, whereas non-European nationality can represent a voluntary condition probably due to difficult adaptive conditions and/or a cultural, social and language barrier. Nevertheless, these environmental conditions could represent by themselves risk factors for psychiatric acute episodes and treatment non-adherence in a sort of vicious cycle.2 Regarding age, our sample indicates that among IHs, subjects were older than those in VHs. The literature is not always consistent on this result,58 which could indicate longer negative course of psychiatric disorder probably resistant to treatment in accordance with most studies19,20,27
Clinical reasons for IH admissions, such as manic excitement and acute psychosis, are rarely present in the clinical reasons for voluntary admissions. Discharge diagnoses are also consistent with the clinical reasons for IH admissions: schizophrenia spectrum disorders and bipolar disorders were higher among IHs, whereas depressive disorders, personality disorders, adjustment disorders and pervasive developmental disorders were more common among VHs, as our regression model confirmed. These findings are supported by most studies.7–12 An international meta-analysis suggests that individuals voluntarily and involuntarily hospitalized can represent two distinct populations different for psychopathological profile and healthcare needs.17 Moreover, IHs presented a significantly longer duration, exceeding by more than 60% VH stay, probably due to poor treatment adherence and the severity of psychopathology; often their destination at discharge was represented by MHCs referral and no other facilities. In contrast, VHs had a shorter mean duration, often due to frequent transfer, accepted by the individuals themselves, to other psychiatric hospital facilities. The results are consistent with a previous study19 but differ from others58 due to differences in the healthcare organization. The greater severity in IHs can be highlighted by more frequent aggressive behaviour during the IHs, behavioral alterations often closely linked to the reasons for involuntary admissions and, due to the difficulties in its management, often the cause of delayed discharge, as observed in other studies,3,22 confirming that aggressive behaviour represents a major obstacle for treatment and care, increasing hospitalization rates and reducing quality of life.28
Looking at the pharmacological prescriptions, higher use of Long-Acting Injectable (LAI) antipsychotics can be noticed in IHs compared to VHs due to poor treatment adherence in severe psychosis cases. As a matter of that, LAIs are especially preferred when subject adherence is poor, as seen among individuals in IHs, in accordance with international guidelines.59,60
Both longer duration of hospital stays and more frequent use of LAIs can be explained by poor treatment adherence as well as the difficulty in managing treatments for severe psychiatric disorders, such as schizophrenia spectrum disorders and bipolar disorders, characterized by aggressive behavior.19,58 The duration of hospital stays increased further during the pandemic period compared to the pre-pandemic period and was associated with increased clinical severity, more frequent aggressive behavior, higher number of days in involuntary treatment, and major pathologies such as schizophrenia spectrum disorders and bipolar disorders. These results indicate a higher concentration of individuals with serious and complex conditions in hospital setting, probably due to organizational choices made during the pandemic period, as emphasized by other studies.47
In the psychiatric context, the term “Revolving Door” (RD), which refers to frequent hospital readmissions, began to be used in the 1970s to describe those individuals who, following discharge from psychiatric hospitals, repeatedly came into contact with mental health services, requiring frequent readmissions to hospital.61,62 Historical research revealed that individuals with psychotic disorders, personality disorders, and alcoholism were at higher risk.61,62 RD hospitalizations were less frequent among IHs confirming opposing attitudes regarding treatment and care among repeatedly or involuntarily hospitalized individuals. Nevertheless, IHs, as suggested by some authors, can reduce risk for re-exacerbations and following readmissions.23,63
The extensive recent literature64–66 highlights that the topic remains of high interest and that understanding the reasons behind frequent readmissions continues to be one of the current challenges for mental health services.67,68
Limitations and Advantages of the Study
Among limitations of our study, we enumerate the single-center design, which does not allow us to generalize our results to other national and international contexts;
The retrospective design which cannot allow us to make causal inferences nor to establish a clear causal relationship, but only to provide a trend based on association of variables;
Incomplete data, especially regarding demographic variables such as occupation, education and housing conditions, characterized by a percentage over 20%, which affect the result validity and hamper the implementation of possible stratified analysis.69
Regarding the advantages of our study, we note that this research is characterized by a relatively extended observation period and the inclusion of many variables related to hospitalization that allowed us to track the evolution over time of certain phenomena related to three important aspects which can have conditioned inpatient treatments: treatment adherence, repeated hospitalizations and the pandemic period. Another advantage is the real-world setting, which permitted us a detailed analysis of the daily practices of a psychiatric unit.
Conclusion
Our study shows a progressive decrease in voluntary hospitalizations over the 6-year observation period, whereas the number of involuntary hospitalizations remained stable and, by the end of the analyzed period, exceeded the number of voluntary admissions. This result highlights that the need for involuntarily hospitalization persisted even in challenging and stressful environmental situations like the pandemic, suggesting that severe psychiatric disorders are negatively influenced by extreme environmental situations like the pandemic and can be exacerbated by reduced attention and care.
During the 6-year observation period, we highlighted a trend of increasingly reduced recourse to voluntary psychiatric hospitalization, whereas involuntary hospitalizations reserved for very serious cases and with longer hospital stay increased. We observed the increase of aggressive behavior especially in involuntary hospitalizations and during pandemic period, further suggesting that involuntary hospitalization in Psychiatry represents the extreme measure for treating severe psychopathological situations characterized by behavior alterations.
In light of our results, we confirm the prevalence of schizophrenia and bipolar disorder diagnoses with poor therapeutic adherence, aggressive behavior and precarious social conditions among subjects involuntarily hospitalized. Our results suggest that IHs can represent an extreme therapeutic intervention aimed at reversing risk situations not otherwise treatable in individuals who, due to their disorder, fail to ask for help. It is therefore necessary to maintain respect for people involuntarily hospitalized, to avoid regressive coercive measures even in these conditions, but, on the contrary, to seek their acceptance of treatments as soon as possible, to encourage their participation in medical decisions, taking into account the subjects’ values and preferences, thus promoting their independent behavior.
During the pandemic period, we observed a reduction in revolving door admissions and an extension of the length of stay in involuntary hospitalizations, indicating the organizational needs during the environmental crisis to limit hospitalizations only to the most serious situations.
Our study allowed us to analyze the evolution of certain conditions, which significantly influenced the trend of psychiatric hospitalizations, modifying their organization over time. In particular, the observed reduction in voluntary hospitalizations during the lockdown period seems to have been implemented and later maintained by the healthcare system, indicating that the effects of an environmental crisis such as the pandemic will presumably continue to manifest themselves in the near future. Further prospective research on the rate of psychiatric hospitalizations, particularly IHs, will be needed in the coming years after the pandemic to make causal inferences and deepen our knowledge of these clinical observations.
Abbreviations
VHs, voluntary hospitalizations; IHs, involuntary hospitalizations; SPDC, Service for Psychiatric Diagnosis and Care; MHCs, Mental Health Centers; SUS, Substance Use Services; SA, Support Administrator; RD, Revolving Door; SD, Standard Deviation; LAI, Long-Acting Injectable.
Ethics Approval and Informed Consent
The study was approved by the Ethics Committee of the Emilia Nord Health Area (Prot. 10826/2023) and authorized by AUSL-Modena (Prot. n. 688; 27/4/2023).
Acknowledgments
The authors thank Orianna Raggioli for her precious help in language revision.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no actual or potential conflicts of interest in this work.
References
1. Gilhooley J, Kelly BD. Return of the asylum. Br J Psychiatry. 2018;212(2):69–70. doi:10.1192/bjp.2017.19
2. Asioli F. Emergenze in psichiatria. 2nd ed. Rome, Italy: il Pensiero Scientifico; 1992. National institute for health and care excellence. Psychosis and schizophrenia in adults treatment and management; 2014. Available from: https://www.nice.org.uk/guidance/cg178/evidence/full-guideline-490503565.
3. Di Lorenzo R, Montardi G, Panza L, et al. Retrospective analysis of factors associated with long-stay hospitalizations in an acute psychiatric ward. Risk Manag Healthc Policy. 2020;13:433–442. doi:10.2147/RMHP.S23874
4. Sharfstein SS. Goals of inpatient treatment for psychiatric. Disorders Annu Rev Med. 2009;60(1):393–403. doi:10.1146/annurev.med.60.042607.080257
5. Haddad PM, Brain C, Scott J. Nonadherence with antipsychotic medication in schizophrenia: challenges and management strategies. Patient Relat Outcome Meas. 2014;5:43–62. doi:10.2147/PROM.S42735
6. Adebiyia MO, Mosakub SK, Irinoyec OO, Oyeladec OO. Socio-demographic and clinical factors associated with relapse in mental illness. Int J Afr Nurs Sci. 2018;8:149–153. doi:10.1016/j.ijans.2018.05.007
7. Salize HJ, Dressing H. Epidemiology of involuntary placement of mentally ill people across the European Union. Br J Psychiatry. 2004;184(2):163–168. doi:10.1192/bjp.184.2.163
8. Wheeler A, Robinson E, Robinson G. Admissions to acute psychiatric inpatient services in Auckland, New Zealand: a demographic and diagnostic review. N Z Med J. 2005;118(1226):U1752.
9. Lay B, Nordt C, Rössler W. Variation in use of coercive measures in psychiatric hospitals. Eur Psychiatry. 2011;26(4):244–251. doi:10.1016/j.eurpsy.2010.11.007
10. Ng XT, Kelly BD. Voluntary and involuntary care: three-year study of demographic and diagnostic admission statistics at an inner-city adult psychiatry unit. Int J Law Psychiatr. 2012;35(4):317–326. doi:10.1016/j.ijlp.2012.04.008
11. Zhou JS, Xiang YT, Zhu XM, et al. Voluntary and Involuntary Psychiatric Admissions in China. Psychiatr Serv. 2015;66(12):1341–1346. doi:10.1176/appi.ps.201400566
12. Balducci PM, Bernardini F, Pauselli L, Tortorella A, Compton MT. Correlates of involuntary admission: findings from an Italian inpatient psychiatric unit. Psychiatr Danub. 2017;29(4):490–496. doi:10.24869/psyd.2017.490
13. Guzzetta F, Miglio R, Santone G, et al. First-ever admitted psychiatric inpatients in Italy: clinical characteristics and reasons contributing to admission: findings from a national survey. Psychiatry Res. 2010;176(1):62–68. doi:10.1016/j.psychres.2008.11.005
14. Mattioni T, Di Lallo D, Roberti R, et al. Determinants of psychiatric inpatient admission to general hospital psychiatric wards: an epidemiological study in a region of central Italy. Soc Psychiatry Psychiatr Epidemiol. 1999;34(8):425–431. doi:10.1007/s001270050164
15. Verdoux H, Lengronne J, Liraud F, et al. Medication adherence in psychosis: predictors and impact on outcome. A 2-year follow-up of first-admitted subjects. Acta Psychiatr Scand. 2000;102(3):203–210. doi:10.1034/j.1600-0447.2000.102003203.x
16. Priebe S, Katsakou C, Amos T, et al. Patients’ views and readmissions 1 year after involuntary hospitalisation. Br J Psychiatry. 2009;194(1):49–54. doi:10.1192/bjp.bp.108.052266
17. Walker S, Mackay E, Barnett P, et al. Clinical and social factors associated with increased risk for involuntary psychiatric hospitalisation: a systematic review, meta-analysis, and narrative synthesis. Lancet Psychiatr. 2019;6(12):1039–1053. doi:10.1016/S2215-0366(19)30406-7
18. Pauselli L, Verdolini N, Bernardini F, Compton MT, Quartesan R. Predictors of length of stay in an inpatient psychiatric unit of a general hospital in Perugia, Italy. Psychiatr Q. 2017;88(1):129–140. doi:10.1007/s11126-016-9440-4
19. Di Lorenzo R, Vecchi L, Artoni C, Mongelli F, Ferri P. Demographic and clinical characteristics of patients involuntarily hospitalized in an Italian psychiatric ward: a 1-year retrospective analysis. Acta Biomed. 2018;89(6–S):17–28. doi:10.23750/abm.v89i6-S.7392
20. Riecher-Rössler A, Rössler W. Compulsory admission of psychiatric patients--an international comparison. Acta Psychiatr Scand. 1993;87(4):231–236. doi:10.1111/j.1600-0447.1993.tb03363.x
21. Zhang S, Mellsop G, Brink J, Wang X. Involuntary admission and treatment of patients with mental disorder. Neurosci Bull. 2015;31(1):99–112. doi:10.1007/s12264-014-1493-5
22. Iudici A, Girolimetto R, Bacioccola E, Faccio E, Turchi G. Implications of involuntary psychiatric admission: health, social, and clinical effects on patients. J Nerv Ment Dis. 2022;210(4):290–311. doi:10.1097/NMD.0000000000001448
23. Hofmann AB, Schmid HM, Hofmann LA, et al. Impact of compulsory admission on treatment and outcome: a propensity score matched analysis. Eur Psychiatry. 2022;65:e6. doi:10.1192/j.eurpsy.2022.4
24. Barnett P, Matthews H, Lloyd-Evans B, Mackay E, Pilling S, Johnson S. Compulsory community treatment to reduce readmission to hospital and increase engagement with community care in people with mental illness: a systematic review and meta-analysis. Lancet Psychiatr. 2018;5(12):1013–1022. doi:10.1016/S2215-0366(18)30382-1
25. Kisely SR, Campbell LA, O’Reilly R. Compulsory community and involuntary outpatient treatment for people with severe mental disorders. Cochrane Database Syst Rev. 2017;3:CD004408. doi:10.1002/14651858.CD004408.pub5
26. Schneider M, Back M, Krückl JS, Moeller J, Lang UE, Huber CG. Compulsory psychiatric admissions in the canton of Basel-Stadt between September 2013 and April 2022: analysis of the cantonal database of the health department of Basel-Stadt. Int J Soc Psychiatry. 2023;69(4):865–874. doi:10.1177/00207640221141020
27. Silva M, Antunes A, Azeredo-Lopes S, et al. Factors associated with involuntary psychiatric hospitalization in Portugal. Int J Ment Health Syst. 2021;15(1):37. doi:10.1186/s13033-021-00460-4
28. Gouveia FV, Ibrahim GM. Habenula as a neural substrate for aggressive behavior. Front Psychiatry. 2022;13:817302. doi:10.3389/fpsyt.2022.817302
29. Faget-Agius C, Boyer L, Wirsich J, et al. Neural substrate of quality of life in patients with schizophrenia: a magnetisation transfer imaging study. Sci Rep. 2015;5(1):17650. Erratum in: Sci Rep. 2016;6:21055. Catherine, Faget-Agius [corrected to Faget-Agius, Catherine]; Jonathan, Wirsich [corrected to Wirsich, Jonathan]; Jean-Philippe, Ranjeva [corrected to Ranjeva, Jean-Philippe]; Raphaelle, Richieri [corrected to Richieri, Raphaelle]; Elisabeth, Soulier. doi:10.1038/srep17650
30. Goodkind M, Eickhoff SB, Oathes DJ, et al. Identification of a common neurobiological substrate for mental illness. JAMA Psychiatry. 2015;72(4):305–315. doi:10.1001/jamapsychiatry.2014.2206
31. Tanaka M, Szabó Á, Vécsei L. Integrating armchair, bench, and bedside research for behavioral neurology and neuropsychiatry: editorial. Biomedicines. 2022;10(12):2999. doi:10.3390/biomedicines10122999
32. Di Gregorio F, Battaglia S. Advances in EEG-based functional connectivity approaches to the study of the central nervous system in health and disease. Adv Clin Exp Med. 2023;32(6):607–612. doi:10.17219/acem/166476
33. Gazzetta Ufficiale. Legge 13 maggio 1978, n. 180. Accertamenti e trattamenti sanitari volontari e obbligatori. (GU Serie Generale n.133 del 16-05-1978). Available from: https://www.gazzettaufficiale.it/eli/id/1978/05/16/078U0180/sg.
34. Gazzetta Ufficiale. Legge 23 dicembre 1978, n. 833, “Istituzione del servizio sanitario nazionale”. Available from: https://www.gazzettaufficiale.it/eli/id/1978/12/28/078U0833/sg.
35. Gazzetta Ufficiale. Legge 9 gennaio 2004, n. 6 Introduzione nel libro primo, titolo XII, del codice civile del capo I, relativo all’istituzione dell’amministrazione di sostegno e modifica degli articoli 388, 414, 417, 418, 424, 426, 427 e 429 del codice civile in materia di interdizioni e di inabilitazione, nonché relative norme di attuazione, di coordinamento e finali. (GU Serie Generale n.14 del 19-01-2004). Available from: https://www.gazzettaufficiale.it/eli/id/2004/01/19/004G0017/sg.
36. Morlino M, Calento A, Schiavone V, et al. Use of psychiatric inpatient services by heavy users: findings from a national survey in Italy. Eur Psychiatry. 2011;26(4):252–259. doi:10.1016/j.eurpsy.2010.11.005
37. Di Lorenzo R, Sagona M, Landi G, Martire L, Piemonte C, Del Giovane C. The revolving door phenomenon in an Italian acute psychiatric ward: a 5-year retrospective analysis of the potential risk factors. J Nerv Ment Dis. 2016;204(9):686–692. doi:10.1097/NMD.0000000000000540
38. Gazzetta Ufficiale. DELIBERA DEL CONSIGLIO DEI MINISTRI 31 gennaio 2020 Dichiarazione dello stato di emergenza in conseguenza del rischio sanitario connesso all’insorgenza di patologie derivanti da agenti virali trasmissibili. (20A00737) (GU Serie Generale n.26 del 01-02-2020) Available from: https://www.gazzettaufficiale.it/eli/id/2020/02/01/20A00737/sg.
39. Gazzetta Ufficiale. DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 23 febbraio 2020 Disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19. (20A01228) (GU Serie Generale n.45 del 23-02-2020). Available from: https://www.gazzettaufficiale.it/eli/id/2020/02/23/20A01228/sg.
40. Gazzetta Ufficiale. DECRETO-LEGGE 24 marzo 2022, n. 24 Disposizioni urgenti per il superamento delle misure di contrasto alla diffusione dell’epidemia da COVID-19, in conseguenza della cessazione dello stato di emergenza. (22G00034) (GU Serie Generale n.70 del 24-03-2022) note: entrata in vigore del provvedimento: 25/03/2022. Decreto-Legge convertito con modificazioni dalla L. 19 maggio 2022, n. 52 (in G.U. 23/05/2022, n. 119). Available from: https://www.gazzettaufficiale.it/eli/id/2022/03/24/22G00034/sg.
41. Preti A, Rucci P, Santone G, et al. Patterns of admission to acute psychiatric in-patient facilities: a national survey in Italy. Psychol Med. 2009;39(3):485–496. doi:10.1017/S0033291708003607
42. Bahji A, Altomare J, Sapru A, Haze S, Prasad S, Egan R. Predictors of hospital admission for patients presenting with psychiatric emergencies: a retrospective, cohort study. Psychiatry Res. 2020;290:113149. doi:10.1016/j.psychres.2020.113149
43. American Psychiatric Association. The Diagnostic and Statistical Manual of Mental Disorders. In: Text Revision (DSM-5-Tr).
44. Osservatorio regionale sul fenomeno migratorio. L’immigrazione straniera in Emilia-Romagna; 2021. Available from: https://sociale.regione.emilia-romagna.it/documentazione/pubblicazioni/prodotti-editoriali/2021/limmigrazione-straniera-in-emilia-romagna.
45. Istituto nazionale di statistica. Al 31 dicembre 2015 I presidi residenziali socio-assistenziali e socio-sanitari; 2018. Available from: https://www.istat.it/it/files/2018/05/Presidi-residenziali_2015.pdf.
46. Istituto nazionale di statistica. Anno 2014 Le persone senza dimora; 2015. Available from: https://www.istat.it/it/files/2015/12/Persone_senza_dimora.pdf.
47. Carpiniello B, Tusconi M, Zanalda E, Di Sciascio G, Di Giannantonio M. Executive committee of the Italian society of psychiatry. Psychiatry during the Covid-19 pandemic: a survey on mental health departments in Italy. BMC Psychiatr. 2020;20(1):593. doi:10.1186/s12888-020-02997-z
48. Flammer E, Eisele F, Hirsch S, Steinert T. Increase in coercive measures in psychiatric hospitals in Germany during the COVID-19 pandemic. PLoS One. 2022;
49. Zielasek J, Lehmann I, Vrinssen J, Gouzoulis-Mayfrank E. Analysis of the utilization, processes, and outcomes of inpatient mental healthcare during the first three waves of the COVID-19 pandemic in the federal state of North Rhine-Westphalia, Germany. Front Psychiatr. 2022;13:957951. doi:10.3389/fpsyt.2022.957951
50. Wullschleger A, Gonçalves L, Royston M, et al. Admissions to psychiatric inpatient services and use of coercive measures in 2020 in a Swiss psychiatric department: an interrupted time-series analysis. PLoS One. 2023;18:e0289310. doi:10.1371/journal.pone.0289310
51. Di Lorenzo R, Frattini N, Dragone D, et al. Psychiatric emergencies during the Covid-19 pandemic: a 6-Month observational study. Neuropsychiatr Dis Treat. 2021;17:1763–1778. doi:10.2147/NDT.S307128
52. Di Lorenzo R, Fiore G, Bruno A, et al. Urgent psychiatric consultations at mental health center during COVID-19 pandemic: retrospective observational study. Psychiatr Q. 2021;92(4):1341–1359. doi:10.1007/s11126-021-09907-w
53. Boldrini T, Girardi P, Clerici M, et al. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog Neuropsychopharmacol Biol Psychiatr. 2021;110:110304. doi:10.1016/j.pnpbp.2021.110304
54. Piccinelli MP, Bortolaso P, Wilkinson GD. Rethinking hospital psychiatry in Italy in light of COVID-19 experience. World J Virol. 2022;11(1):73–81. doi:10.5501/wjv.v11.i1.73
55. Ambrosetti J, Macheret L, Folliet A, et al. Psychiatric emergency admissions during and after COVID-19 lockdown: short-term impact and long-term implications on mental health. BMC Psychiatr. 2021;21(1):465. doi:10.1186/s12888-021-03469-8
56. Rizavas I, Gournellis R, Douzenis P, et al. A systematic review on the impact of seasonality on severe mental illness admissions: does seasonal variation affect coercion? Healthcare. 2023;11:2155. doi:10.3390/healthcare11152155
57. Aguglia A, Moncalvo M, Solia F, Maina G. Involuntary admissions in Italy: the impact of seasonality. Int J Psychiatry Clin Pract. 2016;20(4):232–238. doi:10.1080/13651501.2016.1214736
58. Ielmini M, Caselli I, Poloni N, et al. Compulsory versus voluntary admission in psychiatry: an observational study. Minerva Psichiatrica. 2018;59:129–134. doi:10.23736/S0391-1772.18.01967-2
59. National Institute of Clinical Excellence. Psychosis and schizophrenia in adults: prevention and management. Clinical guideline [CG178]; 2014. Available from: https://www.nice.org.uk/guidance/cg178.
60. American Psychiatric Association. Practice guideline for the treatment of patients with schizophrenia 3rd ed. Available from: https://psychiatryonline.org/doi/pdf/10.1176/appi.books.9780890424841.
61. Woogh CM, Meier HM, Eastwood MR. Psychiatric hospitalization in Ontario: the revolving door in perspective. Can Med Assoc J. 1977;116(8):876–881.
62. Woogh CM. A cohort through the revolving door. Can J Psychiatr. 1986;31(3):214–221. doi:10.1177/070674378603100306
63. Setkowski K, van der Post LF, Peen J, Dekker JJ. Changing patient perspectives after compulsory admission and the risk of re-admission during 5 years of follow-up: the Amsterdam study of acute psychiatry IX. Int J Soc Psychiatry. 2016;62(6):578–588. doi:10.1177/0020764016655182
64. D’Orta I, Herrmann FR, Giannakopoulos P. Determinants of revolving door in an acute psychiatric ward for prison inmates. Front Psychiatry. 2021;12:626773. doi:10.3389/fpsyt.2021.626773
65. Gobbicchi C, Verdolini N, Menculini G, et al. Searching for factors associated with the “Revolving Door phenomenon” in the psychiatric inpatient unit: a 5-year retrospective cohort study. Psychiatry Res. 2021;303:114080. doi:10.1016/j.psychres.2021.114080
66. Koparal B, Ünler M, Utku HÇ, Candansayar S. Revolving door phenomenon and related factors in schizophrenia, bipolar affective disorder and other psychotic disorders. Psychiatr Danub. 2021;33(3):18–26. doi:10.24869/psyd.2021.18
67. Juven-Wetzler A, Bar-Ziv D, Cwikel-Hamzany S, Abudy A, Peri N, Zohar J. A pilot study of the “Continuation of Care” model in “revolving-door” patients. Eur Psychiatr. 2012;27(4):229–233. doi:10.1016/j.eurpsy.2011.05.003
68. Bravo J, Buta FL, Talina M, Silva-Dos-Santos A. Avoiding revolving door and homelessness: the need to improve care transition interventions in psychiatry and mental health. Front Psychiatr. 2022;13:1021926. doi:10.3389/fpsyt.2022.1021926
69. Rombach I, Gray AM, Jenkinson C, Murray DW, Rivero-Arias O. Multiple imputation for patient reported outcome measures in randomised controlled trials: advantages and disadvantages of imputing at the item, subscale or composite score level. BMC Med Res Methodol. 2018;18(1):87. Erratum in: BMC Med Res Methodol. 2018;18:107. doi:10.1186/s12874-018-0542-6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
