Back to Journals » Drug Design, Development and Therapy » Volume 13
Intraoperative dexmedetomidine infusion is associated with reduced emergence agitation and improved recovery profiles after lung surgery: a retrospective cohort study
Authors Kang X , Tang X, Yu Y, Bao F , Gan S, Zheng W, Zhang J, Zhu S
Received 19 November 2018
Accepted for publication 10 February 2019
Published 12 March 2019 Volume 2019:13 Pages 871—879
DOI https://doi.org/10.2147/DDDT.S195221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Qiongyu Guo
Xianhui Kang,1,* Xiaodong Tang,1,* Yang Yu,1 Fangping Bao,1 Shuyuan Gan,1 Wei Zheng,1 Jian Zhang,2 Shengmei Zhu1
1Department of Anesthesiology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang, China; 2Department of Anesthesiology, The Third People’s Hospital of Chengdu, Chengdu, Sichuan, China
*These authors contributed equally to this work
Purpose: This retrospective cohort study aimed to investigate the association between intraoperative dexmedetomidine infusion and emergence agitation (EA), and recovery profiles after lung surgery in adult patients. It was hypothesized that dexmedetomidine was associated with reduced EA and improved recovery profiles.
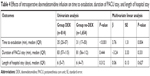
Patients and methods: A single-center chart review was conducted on elective lung surgeries in adults between January and December 2016. The primary outcome was the incidence of EA in postanesthesia care units (PACUs). The secondary outcomes included rescue analgesia, shivering, time to extubation, residual sedation, postoperative pulmonary events, duration of PACU stay, length of hospital stay, and intraoperative hemodynamic changes. Univariate and multivariate regression analyses were used to analyze data.
Results: Among 2,468 patients, 814 received an intraoperative dexmedetomidine infusion. Intraoperative dexmedetomidine infusion was associated with a lower incidence of EA (10.9% vs 15.0%; adjusted OR, 0.67; 95% CI, 0.51–0.87; P=0.003), rescue analgesia (7.6% vs 12.2%; adjusted OR, 0.63; 95% CI, 0.47–0.86; P=0.003), shivering (4.2% vs 6.6%; adjusted OR, 0.58; 95% CI, 0.38–0.88; P=0.010), and intraoperative bradycardia (18.6% vs 12.6%; adjusted OR, 1.51; 95% CI, 1.19–1.92; P=0.001). No differences were observed in residual sedation, duration of PACU stay, postoperative pulmonary events, and length of hospital stay between the groups.
Conclusion: This retrospective study suggested that intraoperative dexmedetomidine infusion was associated with a lower incidence of EA, rescue analgesia, and shivering in adults after lung surgery. Intraoperative bradycardia was the main side effect.
Keywords: dexmedetomidine, emergence agitation, intraoperative administration, lung surgery, recovery profiles
Introduction
Emergence agitation (EA) in the postanesthesia care unit (PACU) is a common complication after general anesthesia.1 In some extreme cases, it can cause self-extubation, accidental removal of catheters, increased pain, and bleeding.1,2 Thus, it increases the demand of human resources and imposes the risk of injury to patients and staff. Different studies have reported different incidences in adult populations, ranging from 3.7% to 21%, due to the variability in the patient population and the scale used to assess EA.1–4
Moreover, the incidence of EA in lung surgeries has been reported to be relatively higher, even up to 41% in one study.5 Lee et al also found that 14% of patients undergoing video-assisted thoracoscopic surgery (VATS) experienced severe EA (Riker score =7).6 This higher incidence could be attributable to remarkable psychological stress and acute postoperative pain. Consistently, inadequate analgesia could result in a higher incidence of agitation in patients undergoing radical resection of lung cancer.7
Dexmedetomidine is a highly selective α2-adrenoceptor agonist with sympatholytic, analgesic, sedative, and anxiolytic properties without respiratory depression.8 Recently, it is being increasingly used as an adjuvant for general anesthesia in adults. Its intraoperative use provides smooth and hemodynamically stable emergence and improves the quality of emergence from general anesthesia.9–12 Although the intraoperative infusion of dexmedetomidine could effectively prevent EA compared with the control group after nasal surgery,9,11,12 no published study has investigated the effects of dexmedetomidine on preventing EA in adult patients undergoing lung surgery.
This retrospective cohort study was performed in a tertiary teaching hospital, and its aim was to investigate the relationship between intraoperative dexmedetomidine infusion and EA, and the recovery profiles in adult patients after lung surgery. The hypothesis was that dexmedetomidine infusion was associated with reduced EA and improved recovery profiles in these patients.
Patients and methods
Study design
This study was approved by the Institutional Review Board of the First Affiliated Hospital, College of Medicine, Zhejiang University (IRB 2017[683]). The requirement for informed consent was waived by the IRB because this retrospective review was limited to preexisting data collected prospectively as part of the standard-of-care and documented by care providers (surgeons, anesthesiologists, and nurses), and covering patient data confidentiality was promised. This study was registered prior to data collection at the Chinese Clinical Trial Registry, www.chictr.org.cn (number ChiCTR-RRC-17013603). Adult patients (≥18 years) who underwent elective lung surgery under general anesthesia between January and December 2016 were screened for eligibility. Patients were excluded if they had central nervous system diseases (schizophrenia, epilepsy, dementia, or Parkinsonism), were directly admitted to the intensive care unit (ICU), or required reoperation. Patients with incomplete data were excluded (Figure 1).
  | Figure 1 Study population recruitment summary. |
Data collection
Data were retrieved from hospital electronic records and the Operative Room Scheduling Office System (McKesson Corporation, San Francisco, CA, USA) booking database and organized following the template of the Society of Thoracic Surgeons (STS) general thoracic surgery database data specifications. Researchers were trained before data collection and an independent investigator verified all data. Perioperative variables included demographics, individual history, comorbidities, intraoperative data, EA, and other postoperative outcomes.
Intraoperative data included induction sedatives (etomidate or propofol), combination of sevoflurane, intraoperative dexmedetomidine infusion, use of midazolam, prophylactic postoperative analgesics (opioids or nonsteroidal anti-inflammatory drugs [NSAIDs]), wound infiltration (10 mL of 0.75% ropivacaine), type of surgery (VATS or open thoracotomy), fluid intake, blood loss, duration of surgery, and body temperature at arrival in the PACU. Study drugs (dexmedetomidine hydrochloride, 200 μg/2 mL) were manufactured by Jiangsu Hengrui Medicine Co, Ltd (Jiangsu, China). In clinical practice, intraoperative dexmedetomidine administration was defined as a loading dose of 0.5–1 μg kg−1 within 10–15 minutes, continuous infusion at a rate of 0.2–0.7 μg kg−1 h−1, or both. Dexmedetomidine was administered according to the attending anesthesiologist’s decision.
The primary outcome of this study was EA. Secondary outcomes included rescue analgesia, shivering, time to extubation, residual sedation, postoperative pulmonary events, duration of PACU stay, length of hospital stay, and intraoperative hemodynamic changes. On the basis of the STS criteria and previous literature, the following definitions were used. EA was defined as restlessness, agitation, noncooperation, confusion, disorientation, or violent behavior in the early phase of recovery from general anesthesia.13 EA was assessed using the Riker sedation–agitation score:14 1, unarousable, no response to noxious stimuli; 2, very sedated, arouses to physical stimuli but does not follow commands; 3, sedated, awakens to verbal commands or gentle shaking but drifts off again; 4, calm, awakens easily, follows verbal commands; 5, agitated, anxious or mildly agitated, calms down to verbal instructions; 6, very agitated, requires physical restraint; and 7, dangerous agitation, pulling at the tracheal tube, trying to remove catheters, or striking at staff. EA assessment was a part of typical practice in the institution, and all patients presenting to the PACU underwent this type of assessment. EA was defined as a Riker score ≥5 after extubation in the PACU. Rescue analgesia was defined as the adoption of analgesics when a patient’s postoperative pain numerical rating scale was >3 after extubation in the PACU.15 Shivering was defined as detectable fasciculation or tremor of the face, jaw, head, trunk, or extremities.16 Residual sedation was defined as a sedation–agitation scale score ≤3 after extubation in the PACU.9 Postoperative pulmonary events included desaturation and respiratory failure: 1) indicates <90% on pulse oximetry and requiring only oxygen17 and 2) indicates whether the patient experienced respiratory failure in the postoperative period requiring mechanical ventilation and/or reintubation. Time to extubation was defined as the time from the cessation of anesthetics to extubation, and the length of hospital stay was the time duration from the day of surgery to hospital discharge. Intraoperative hemodynamic changes included the following: 1) bradycardia was defined as a heart rate of ≤50 beats per minute for >5 minutes;18 2) hypotension was defined as systolic blood pressure <90 mm Hg for >5 minutes;19 and 3) hypertension was defined as systolic blood pressure ≥160 mm Hg for >5 minutes.20
Statistical analyses
Categorical variables were summarized as frequencies and proportions, normally distributed continuous variables as mean (SD), and non-normally distributed continuous variables as median. An unpaired t-test was used to test for normally distributed continuous variables, Mann–Whitney U-test was used for variables without normal distribution, and the chi-square or Fisher exact tests were applied for categorical data as appropriate. Missing continuous variables of baseline parameters were ≤10% and replaced by median, as shown in Tables 1 and 2.
First, univariate characteristics between patients with and without EA were compared using unpaired t, Mann–Whitney U, or chi-square tests. Second, to adjust for potential confounders, a binary logistic regression analysis was conducted to identify association of intraoperative dexmedetomidine infusion with EA using the enter method. Also, univariate analysis was conducted to assess the unadjusted association of candidate variables with secondary outcomes. Variables with a statistical difference of P≤0.1 in the univariate analysis and candidate risk factors reported in previous literature were deliberately included in the following multivariate analysis to identify dexmedetomidine with secondary outcomes using the enter method. The binary logistic regression analysis was applied to assess rescue analgesia, shivering, residual sedation, postoperative pulmonary events, and intraoperative hemodynamic changes. The linear regression analysis was used to assess time to extubation, duration of PACU stay, and length of hospital stay including the same risk factors for EA.
The results were reported as OR with 95% CI or beta (β) with standard error (SE). Differences were considered to be statistically significant if the P-values were <0.05 (two-tailed). Statistical analysis was performed using SPSS version 23.0 (IBM Corporation, Armonk, NY, USA).
Sample size
The sample size was based on a 20% incidence of EA among the placebo group and a 30% reduction in EA incidence in the dexmedetomidine group. The assumption was considered to be conservative because the incidence of EA was described as 3.7%–41%.1–5 Regression for a dichotomous predictor of the influence of dexmedetomidine on EA was performed, and it was estimated that 1,488 patients were required to provide 80% power to detect a two-sided difference, with a type I error probability of 0.05. Analysis was computed using G-Power (version 3.1; Informer Technologies, Inc., Kiel, Germany).
Results
Baseline parameters and operative characteristics
A total of 2,468 patients were included. They were divided into two groups: dexmedetomidine group (n=814, 33.0%, group DEX) and no-dexmedetomidine group (n=1,654, 67.0%, group no-DEX). The average age of the entire cohort was 58 years (48.5% males), and 1.9% had an American Society of Anesthesiologists (ASA) score of 3 or 4.
The basic clinical features of the two groups are presented in Table 1. No statistical difference was observed in age, sex, body mass index (BMI), ASA score of 3 or 4, comorbidities (hypertension, diabetes, cerebrovascular history, cardiac disease, chronic respiratory disease, liver or kidney dysfunction, and peripheral vascular disease), cigarette smoking, and history of alcohol consumption of >10 years between the two groups.
Patients in group DEX were more exposed to the combination of sevoflurane (14.4% vs 7.9%, P<0.001) and more frequent administration of etomidate (92.4% vs 87.5%, P<0.001), NSAIDs (59.3% vs 40.3%, P<0.001), but less of tramadol (16.3% vs 22.8%, P<0.001). In addition, less fluid intake (1,421 vs 1,472 mL, P=0.012), more wound infiltration (42.9% vs 35.6%, P<0.001), longer duration of surgery (107 vs 99 minutes, P<0.001), and lower temperature at arrival in the PACU (36.0°C vs 36.1°C, P=0.039) were observed in patients in group DEX. Nevertheless, no significant difference was found between the two groups with reference to the administration of midazolam, oxycodone, dezocine, and other opioid analgesics; blood loss; and type of surgery (Table 2).
Postoperative EA and recovery profiles
Univariate analysis
A total of 337 patients (13.7%) experienced EA. Intraoperative dexmedetomidine infusion was associated with a significantly lower incidence of EA. Incidence of EA was 10.9% in group DEX (n=89) vs 15.0% (n=248) in group no-DEX (OR, 0.70; 95% CI, 0.54–0.90; P=0.006; Table 3). The intraoperative infusion of dexmedetomidine was associated with a significantly reduced incidence of rescue analgesia (7.6% vs 12.2%; OR, 0.60; 95% CI, 0.44–0.80; P=0.001), and shivering (4.2% vs 6.6%; OR, 0.62; 95% CI, 0.42–0.92; P=0.017). Moreover, it was associated with longer time to extubation (35 vs 31 minutes, P<0.001). No differences were seen in the incidence of residual sedation (0.5% vs 0.4%, P=0.638), duration of PACU stay (83 vs 81 minutes, P=0.444), postoperative pulmonary events neither in PACU (0.7% vs 0.5%, P=0.563) nor in the ward (0.1% vs 0.2%, P=0.736), and length of hospital stay (6 vs 6 days, P=0.312).
Multivariate analysis
The final multivariate regression model assessing EA included sex, age, BMI, ASA score of 3 or 4, hypertension, cigarette smoking, history of alcohol consumption of >10 years, intraoperative dexmedetomidine infusion, dezocine, NSAIDs, fluid intake, blood loss, wound infiltration, and duration of surgery. The multivariate regression model assessing rescue analgesia included age, diabetes, cerebrovascular history, intraoperative dexmedetomidine infusion, use of midazolam, other opioid analgesics, NSAIDs, fluid intake, type of surgery, duration of surgery, and temperature at arrival in the PACU. The multivariate regression model assessing shivering included sex, age, hypertension, diabetes, cigarette smoking, history of alcohol consumption of >10 years, intraoperative dexmedetomidine infusion, etomidate, tramadol, NSAIDs, type of surgery, duration of surgery, and temperature at arrival in the PACU. The results of the multivariate analysis are summarized in Table 3. The observed reduction in EA (adjusted OR, 0.67; 95% CI, 0.51–0.87; P=0.003) persisted after multivariate adjustment. The adjusted rates of rescue analgesia (adjusted OR, 0.63; 95% CI, 0.47–0.86; P=0.003) and shivering (adjusted OR, 0.58; 95% CI, 0.38–0.88; P=0.010) were also statistically significant between group DEX and group no-DEX.
Moreover, intraoperative dexmedetomidine infusion was associated with longer time to extubation (β=3.76, SE =1.31, P=0.004; Table 4). No statistically significant differences were observed in the incidence of residual sedation, postoperative pulmonary events in the PACU or in the ward, duration of PACU stay, and length of hospital stay between groups after adjustment for the difference.
Intraoperative hemodynamic changes
In the univariate analysis, intraoperative dexmedetomidine infusion was associated with an increase in intraoperative bradycardia (18.6% vs 12.6%; OR, 1.58; 95% CI, 1.26–1.99; P<0.001; Table 2). After multivariate adjustment, intraoperative bradycardia (adjusted OR, 1.51; 95% CI, 1.19–1.92; P=0.001) still increased in group DEX. However, no significant differences were found between the two groups in terms of hypotension and hypertension both in the univariate analysis and after multivariate adjustment (Table 3).
Discussion
This retrospective study reported an association between intraoperative dexmedetomidine infusion and a lower incidence of EA (primary outcome), rescue analgesia, and shivering in adult patients undergoing lung surgery. Intraoperative bradycardia was the main side effect.
EA is multifactorial, and one possible mechanism is variation in neurologic recovery rate in different brain areas.21 Surgery-induced neuroinflammation may be another cause of this functional change within the brain.22 Moreover, the association of EA with other factors, such as pain, inhalational anesthetics, preoperative anxiety, male gender, age, and type of surgical procedures, has been suggested.1–3
EA seemed to be more common after lung surgery; 41% of patients experienced it.5 A higher incidence could be attributed to acute postoperative pain. The pain that accompanies thoracic surgery is notable for its intensity, ranging from moderate to severe levels.23 Patients undergoing VATS also complain of a moderate degree of postoperative pain.6 Another reason may be severe preoperative anxiety. A study found that 43% of patients undergoing surgery for lung cancer experienced psychological distress and mood changes,24 and more stressful situations could be associated with a higher rate of EA.
However, in the present study, the overall incidence of EA in patients undergoing lung surgery was 13.7%. The low EA incidence could be explained as follows. First, the proportion of VATS was 79% in the present population, higher than 68% in a previous study,5 which could lead to less intense pain and a lower occurrence of EA. Second, anesthesia was maintained with intravenous propofol and remifentanil infusion in the population, and only ~10% was combined with sevoflurane. Fewer inhalational anesthetics could lead to a lower incidence of EA.21 Third, this could be partly attributed to the adoption of multimodal analgesia in postoperative pain treatment including prophylactic postoperative analgesics, wound infiltration, and patient-controlled analgesia device. It was a routine procedure for patients undergoing lung surgery in the institution, and the alleviated postoperative pain could reduce EA.7
Dexmedetomidine, an α2 adrenoceptor agonist, is well known for its two primary clinical effects of sedation and analgesia. In elderly patients admitted to the ICU, dexmedetomidine contributes to improved sleep quality pattern, reduced delirium, increased survival up to 2 years, and improved cognitive function and quality of life in 3-year survivors.25–27 Likewise, its intraoperative use has increased because it could reduce EA in pediatric patients after general anesthesia28 or in adults undergoing nasal surgery.9,11,12 However, evidence regarding the effects of dexmedetomidine on EA and recovery quality in adults after lung surgery is still lacking. The results of the present study showed that intraoperative dexmedetomidine infusion was associated with a decreased incidence in EA (10.9% vs 15.0%) in adult patients undergoing lung surgery. The incidence of EA was the primary outcome; after adjusting for covariates using the multivariate analysis, dexmedetomidine group still showed reduction of EA. Lee et al found that intraoperative dexmedetomidine infusion decreased the Riker score and incidence of severe EA in adults undergoing VATS.6 However, the effect of dexmedetomidine on EA was not their primary outcome. In other words, the present study was novel in demonstrating the association between dexmedetomidine and EA in patients undergoing lung surgery. The sedative property of dexmedetomidine is responsible for reducing the incidence of EA, through the inhibition of α2-adrenoceptor-mediated release of norepinephrine in the locus coeruleus and spinal cord.29,30
Nonetheless, patients receiving dexmedetomidine presented delayed extubation, and the inherent sedative property of dexmedetomidine accounted for it. Moreover, dexmedetomidine was not associated with residual sedation or duration of PACU stay. A possible explanation was that dexmedetomidine induced “cooperative sedation” rather than oversedation,31 unlike other commonly used sedatives such as midazolam or propofol. A recent study conducted on nasal surgery reported different results,11 and one possible reason was the maintenance of dexmedetomidine infusion until extubation. It indicated that an optimal dose of dexmedetomidine existed for preventing EA with minimal side effects.
In the present retrospective study, there was a limitation in dexmedetomidine administration. Specifically, three protocols were used for dexmedetomidine infusion: a loading dose of 0.5–1.0 μg kg−1 for 10–15 minutes, a continuous infusion of 0.2–0.7 μg kg−1 h−1, and both. These dosage regimens were demonstrated to be effective in preventing EA compared with placebo,6,9–11,32 and thus were all applied in clinical practice. The variation in the duration of continuous infusion for individuals receiving dexmedetomidine was decided by the anesthesiologist based on the specific condition of patients. These limitations might be a confounding factor while interpreting the main outcome, which needs future confirmation.
As better pain relief contributes to improvements in pulmonary function after thoracic surgery,33 pain has become one of the most important factors in the postoperative recovery of patients. In the present study, the administration of dexmedetomidine was associated with fewer patients requiring rescue analgesia in the PACU. In other words, it indicated that these patients who received dexmedetomidine presented better postoperative pain relief. Surgical trauma leads to the release of inflammatory mediators, thus causing pain.34 Dexmedetomidine could reduce the levels of circulating inflammatory cytokines both clinically and in rodent models.35,36 It was also demonstrated to modulate nociceptive transmission in the central nervous system by acting on the α2 adrenergic receptors located in both supraspinal and spinal sites.8,31 These might explain why dexmedetomidine was effective in controlling postoperative pain and thus reducing rescue analgesic requirements in the PACU.
Furthermore, the findings revealed that intraoperative dexmedetomidine was associated with a lower incidence of shivering. Shivering was frequent in the postoperative period and appeared to be modulated through central adrenergic receptors.37 The α-2B receptor subtype mediates the suppression of shivering centrally and causes peripheral vasoconstriction.31 Dexmedetomidine is an α2 agonist that has been confirmed to decrease vasoconstriction and the shivering threshold.38,39
Additionally, intraoperative bradycardia was the main adverse effect of dexmedetomidine. Dexmedetomidine can cause hemodynamic changes such as hypotension and bradycardia, coinciding with the reduction in the levels of plasma noradrenaline and adrenaline.8
Limitations
This study had several limitations. First, this was an observational cohort study. Multivariate analysis was used in this study to reduce evident biases; nonetheless, other potential confounding biases remained. Second, differences existed in the specific methods and doses of intraoperative dexmedetomidine administration. It was a routine practice in the institution and an inevitable limitation of this retrospective study. Third, no objective assessments were available in daily practice regarding the effects of dexmedetomidine on postoperative pulmonary function. However, no influence was found on postoperative pulmonary events occurring in the PACU or ward.
Conclusion
This study demonstrated that patients undergoing lung surgery and receiving intraoperative dexmedetomidine infusion were more likely to have a lower incidence of EA in the PACU. The intraoperative use of dexmedetomidine was also associated with less rescue analgesia and shivering. The main adverse hemodynamic side effect of dexmedetomidine was intraoperative bradycardia.
Data sharing statement
Data will not be shared because a further study based on the data will be subsequently carried out.
Acknowledgments
All authors thank Xianhong Huang, PhD (Statistician, Department of Social Medicine, Medical College of Hangzhou Normal University, Hangzhou, Zhejiang, China). This study was supported by the National Natural Science Foundation of China (81471171, 81771194), the Science Foundation of Zhejiang Province (Y19H310028), and a Zhejiang Provincial Medical and Health Grant (2015KYB118).
Disclosure
The authors report no conflicts of interest in this work.
References
Lepousé C, Lautner CA, Liu L, Gomis P, Leon A. Emergence delirium in adults in the post-anaesthesia care unit. Br J Anaesth. 2006;96(6):747–753. | ||
Munk L, Andersen G, Møller AM. Post-anaesthetic emergence delirium in adults: incidence, predictors and consequences. Acta Anaesthesiol Scand. 2016;60(8):1059–1066. | ||
Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anesth. 2010;57(9):843–848. | ||
Card E, Pandharipande P, Tomes C, et al. Emergence from general anaesthesia and evolution of delirium signs in the post-anaesthesia care unit. Br J Anaesth. 2015;115(3):411–417. | ||
Li C, Shi J, Wang K, Sun B, Gao G. Risk factors for inadequate emergence after non-cardiac thoracic surgery. J Clin Anesthesiol. 2016;32(1):33–37. | ||
Lee SH, Lee CY, Lee JG, Kim N, Lee HM, Oh YJ. Intraoperative dexmedetomidine improves the quality of recovery and postoperative pulmonary function in patients undergoing video-assisted thoracoscopic surgery: a CONSORT-prospective, randomized, controlled trial. Medicine. 2016;95(7):e2854. | ||
Lu J, Liu Z, Xia K, et al. Effect of preemptive analgesia with parecoxib sodium in patients undergoing radical resection of lung cancer. Int J Clin Exp Med. 2015;8(8):14115–14118. | ||
Bhana N, Goa KL, McClellan KJ. Dexmedetomidine. Drugs. 2000;59(2):263–268. | ||
Kim SY, Kim JM, Lee JH, Song BM, Koo BN. Efficacy of intraoperative dexmedetomidine infusion on emergence agitation and quality of recovery after nasal surgery. Br J Anaesth. 2013;111(2):222–228. | ||
Aouad MT, Zeeni C, Al Nawwar R, et al. Dexmedetomidine for improved quality of emergence from general anesthesia. Anesth Analg. Epub 2017 Dec 29. | ||
Garg A, Kamal M, Mohammed S, Singariya G, Chouhan DS, Biyani G. Efficacy of dexmedetomidine for prevention of emergence agitation in patients posted for nasal surgery under desflurane anaesthesia: a prospective double-blinded randomised controlled trial. Indian J Anaesth. 2018;62(7):524–530. | ||
Lee HS, Yoon HY, Jin HJ, Hwang SH. Can dexmedetomidine influence recovery profiles from general anesthesia in nasal surgery? Otolaryngol Head Neck Surg. 2018;158(1):43–53. | ||
Vlajkovic GP, Sindjelic RP. Emergence delirium in children: many questions, few answers. Anesth Analg. 2007;104(1):84–91. | ||
Riker RR, Picard JT, Fraser GL. Prospective evaluation of the Sedation-Agitation scale for adult critically ill patients. Crit Care Med. 1999;27(7):1325–1329. | ||
Polat R, Peker K, Baran I, Aydin GB, Guloksuz C, Donmez A. Comparison between dexmedetomidine and remifentanil infusion in emergence agitation during recovery after nasal surgery. Anaesthesist. 2015;64(10):740–746. | ||
Kiekkas P, Poulopoulou M, Papahatzi A, Souleles P. Effects of hypothermia and shivering on standard PACU monitoring of patients. AANA J. 2005;73(1):47–53. | ||
Conti D, Ballo P, Boccalini R, et al. The effect of patient sex on the incidence of early adverse effects in a population of elderly patients. Anaesth Intensive Care. 2014;42(4):455–459. | ||
Smith I, Monk TG, White PF. Comparison of transesophageal atrial pacing with anticholinergic drugs for the treatment of intraoperative bradycardia. Anesth Analg. 1994;78(2):245–252. | ||
Cheung CC, Martyn A, Campbell N, et al. Predictors of intraoperative hypotension and bradycardia. Am J Med. 2015;128(5):532–538. | ||
Charlson ME, MacKenzie CR, Gold JP, Ales KL, Topkins M, Shires GT. Preoperative characteristics predicting intraoperative hypotension and hypertension among hypertensives and diabetics undergoing noncardiac surgery. Ann Surg. 1990;212(1):66–81. | ||
Aouad MT, Nasr VG. Emergence agitation in children: an update. Curr Opin Anaesthesiol. 2005;18(6):614–619. | ||
Alam A, Hana Z, Jin Z, Suen KC, Ma D, Surgery MD. Surgery, neuroinflammation and cognitive impairment. EBioMedicine. 2018;37:547–556. | ||
Gottschalk A, Cohen SP, Yang S, Ochroch EA. Preventing and treating pain after thoracic surgery. Anesthesiology. 2006;104(3):594–600. | ||
Zabora J, Brintzenhofeszoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psycho-Oncology. 2001;10(1):19–28. | ||
Xh W, Cui F, Zhang C, et al. Low-dose dexmedetomidine improves sleep quality pattern in elderly patients after noncardiac surgery in the intensive care unit: a pilot randomized controlled trial. Anesthesiology. 2016;125(5):979–991. | ||
Su X, Meng ZT, Wu XH, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet. 2016;388(10054):1893–1902. | ||
Zhang DF, Su X, Meng ZT, et al. Impact of dexmedetomidine on long-term outcomes after noncardiac surgery in elderly: 3-year follow-up of a randomized controlled trial. Ann Surg. Epub 2018 May 8. | ||
Mahmoud M, Mason KP. Dexmedetomidine: review, update, and future considerations of paediatric perioperative and periprocedural applications and limitations. Br J Anaesth. 2015;115(2):171–182. | ||
Guo TZ, Jiang JY, Buttermann AE, Maze M. Dexmedetomidine injection into the locus ceruleus produces antinociception. Anesthesiology. 1996;84(4):873–881. | ||
Gerlach AT, Dasta JF. Dexmedetomidine: an updated review. Ann Pharmacother. 2007;41(2):245–254. | ||
Alam A, Suen KC, Hana Z, Sanders RD, Maze M, Ma D. Neuroprotection and neurotoxicity in the developing brain: an update on the effects of dexmedetomidine and xenon. Neurotoxicol Teratol. 2017;60:102–116. | ||
Kwon SY, Joo JD, Cheon GY, Oh HS, In JH. Effects of dexmedetomidine infusion on the recovery profiles of patients undergoing transurethral resection. J Korean Med Sci. 2016;31(1):125–130. | ||
Bauer C, Hentz JG, Ducrocq X, et al. Lung function after lobectomy: a randomized, double-blinded trial comparing thoracic epidural ropivacaine/sufentanil and intravenous morphine for patient-controlled analgesia. Anesth Analg. 2007;105(1):238–244. | ||
Julius D, Basbaum AI. Molecular mechanisms of nociception. Nature. 2001;413(6852):203–210. | ||
Tang C, Huang X, Kang F, et al. Intranasal dexmedetomidine on stress hormones, inflammatory markers, and postoperative analgesia after functional endoscopic sinus surgery. Mediators Inflamm. 2015;2015(6):1–9. | ||
Ma J, Chen Q, Li J, et al. Dexmedetomidine-mediated prevention of renal ischemia-reperfusion injury depends in part on cholinergic anti-inflammatory mechanisms. Anesth Analg. Epub 2018 Oct 19. | ||
Macario A, Weinger M, Carney S, Kim A. Which clinical anesthesia outcomes are important to avoid? The perspective of patients. Anesth Analg. 1999;89(3):652–658. | ||
Doufas AG, Lin CM, Suleman MI, et al. Dexmedetomidine and meperidine additively reduce the shivering threshold in humans. Stroke. 2003;34(5):1218–1223. | ||
Bicer C, Esmaoglu A, Akin A, Boyaci A. Dexmedetomidine and meperidine prevent postanaesthetic shivering. Eur J Anaesthesiol. 2006;23(2):149–153. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.