Back to Journals » Clinical Ophthalmology » Volume 16
Intraocular Pressure Measurement with Pneumatonometry and a Tonometer Tip Cover During Negative Pressure Application
Authors Brambilla E, Ferguson TJ , Chu N, Ammar D , Yoo P
Received 23 January 2022
Accepted for publication 13 April 2022
Published 26 April 2022 Volume 2022:16 Pages 1289—1300
DOI https://doi.org/10.2147/OPTH.S359605
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Enrico Brambilla,1 Tanner J Ferguson,2 Nathan Chu,1 David Ammar,3 Paul Yoo1
1Equinox Ophthalmic, Inc., Newport Beach, CA, USA; 2Vance Thompson Vision, Sioux Falls, SD, USA; 3Lions Eye Institute for Transplant & Research, Tampa, FL, USA
Correspondence: Tanner J Ferguson, Vance Thompson Vision, 3101 W. 57th St, Sioux Falls, SD, USA, Email [email protected]
Purpose: This is a 2-part study to investigate the agreement between pneumatonometry and direct pressure transducer intraocular pressure (IOP) measurements in a perfusion organ culture (POC) model where (1) the perfusion fluid column is open to atmospheric pressure, holding IOP constant to permit evaluation of the impact of negative pressure (NP) on IOP measurements, and (2) the perfusion fluid column is a closed system, allowing IOP to vary with NP application.
Methods: The first part incorporated a fluid column open to atmospheric pressure, maintaining IOP constant to permit evaluation of the effect of applied NP on IOP measurement accuracy. In the second part, the POC column was closed, allowing IOP to vary with NP application and permit evaluation of agreement between pneumatonometry and pressure transducer measurements. In each part, four perfused tissues were used in thirteen paired pre-set IOP (10, 20, 25, 30 mmHg) and NP (0, 5, 10, 15, 20 mmHg) combinations, resulting in a total of 1040 paired measurements (520 per study). The difference in IOP measurements (Δ IOP = Excursion tonometry – pressure transducer) was calculated at each paired configuration.
Results: During the first part, the mean Δ IOP was − 0.7 ± 1.6 mmHg across all measurements. During the second part, the mean Δ IOP across all measurements was +0.7 ± 1.4 mmHg. At NP settings of − 5, − 10, − 15, and − 20 mmHg, across all pre-set IOPs, the mean IOP reduction via Excursion tonometry was 3.1 ± 0.3, 5.6 ± 1.3, 8.5 ± 1.7 and 11.2 ± 1.8 mmHg, respectively.
Conclusion: Measurement of IOP via Excursion tonometry yields results within the accuracy range of the pneumatonometry device (per manufacturer) and is minimally impacted by NP application. The IOP-lowering results are consistent with previous studies and further support the effectiveness of the Multi-Pressure Dial in lowering IOP relative to atmospheric pressure.
Keywords: tonometry, intraocular pressure, IOP, multi-pressure dial, MPD, ophthalmic techniques, diagnostics
Introduction
Open-angle glaucoma (OAG) is a leading cause of global blindness and is projected to impact greater than 100 million people by the year 2040.1–3 Although glaucoma can occur at any level of IOP, elevated IOP is a significant risk factor and strategies targeting the reduction of IOP are the mainstay of treatment.1 Considerable innovation has occurred over the last decade with respect to treatment with the emergence of new medical and surgical options.4–6 However, the current treatment landscape does not include a non-pharmaceutical or non-surgical IOP-lowering option.
A novel device has recently been introduced known as the Multi-Pressure Dial System, or MPD (Equinox Ophthalmic, Inc., CA, USA). The MPD applies negative pressure in front of the eyes within the goggles to lower pressure inside the eye (ie, IOP) relative to the surrounding atmospheric pressure environment.7–9 The MPD is comprised of a pressure-modulating pump, which delivers and monitors negative pressure, and goggles designed to obtain a sealed environment over the eyes. This localized application of negative pressure leads to a corresponding decrease in IOP, which persists during the entire period of negative pressure application. The magnitude of negative pressure is determined and programmed independently for each eye by the physician based on individual patient needs.
The IOP reduction conferred by the MPD requires a sealed, negative pressure environment within the goggles. Because conventional tonometry methods, such as Goldmann applanation tonometry, require direct access to the front surface of the cornea, IOP measurements during MPD use are precluded due to the presence of the goggles. To evaluate the IOP-lowering effect of the MPD, a novel test method was developed, utilizing a specially adapted version of the MPD goggles. This modification includes placement of access holes in the goggles to permit access to the front surface of the cornea for a Reichert Model 30® pneumatonometer probe. To maintain a sealed vacuum environment, a silicone tube fitted with a Tono-Pen cover is positioned through the access holes. The Tono-Pen cover is positioned to lay on the front surface of the cornea without any tension so pneumatonometry can be performed during application of negative pressure. This test method is referred to as Excursion tonometry.10
A recent study investigated the precision and accuracy of Excursion tonometry with favorable results, supporting its use as a reliable method of IOP measurement.10 This present study aims to further evaluate Excursion tonometry by assessing the impact of localized negative pressure on both the accuracy of excursion measurement compared to intraocular transducer measurements and the IOP-lowering effect of the MPD in a perfusion organ culture (POC) system with cadaver eyes.11,12 To independently assess the accuracy of measurements, the first part of this study included a fluid column open to atmospheric pressure to ensure the set IOP values were constant and not impacted by the applied negative pressure. The second part involved a closed system to assess the effect of applied negative pressure on IOP.
Materials and Methods
Study Materials
- Reichert Technologies Inc. Model 30 Pneumatonometer
- Tono-Pen® Cover
- Cadaver Eye Test Fixture
- Excursion cartridge for Tono-Pen tip cover
- Reichert Technologies Inc. Test Column for calibration
- DMEM (Dulbecco’s Modified Eagle’s Media) Column Manometer
- Delta-Cal (Utah Medical Products Inc.)
- DelTran II blood pressure transducer (AD Instruments)
- Perfusion control and data acquisition system
- Desktop computer
- LabChart DAQ software (AD Instruments)
- 8-channel “Octal” bridge amplier (AD Instruments)
- PowerLab DAQ unit (AD Instruments)
- Reference Documents
- ANSI Z80.10–2014
- Reichert, Model 30 Pneumatonometer User’s Guide
Study Design
Excursion tonometry was developed to allow IOP measurements with the MPD during negative pressure application. Similar to other conventional tonometry methods, including Goldmann applanation tonometry, this method allows contact with the anterior corneal surface to obtain transcorneal pressure measurements, ie, the difference in pressure inside the eye vs outside the eye (atmospheric pressure) as measured across the cornea.
The Excursion MPD goggles, shown in Figure 1, consist of access ports (ie, holes) in each goggle lens that permit insertion of a silicone tube coupled with a Tono-Pen® tip cover to allow IOP measurement via pneumatonometry. This adaptation enables applanation of the cornea while maintaining a stable vacuum environment in the goggles. A previous study evaluated the precision and accuracy of Excursion tonometry and quantified the impact of the Tono-Pen cover on pneumatonometry measurements. This study aims to evaluate the following in a POC system that models fluid outflow in human scleral/corneal rims:
- The effect of negative pressure on the agreement between Excursion tonometry and pressure transducer measurements (IOP set with an open column system), and
- The agreement between Excursion tonometry and pressure transducer measurements when effect of negative pressure is allowed to affect IOP (closed column system).
The first objective of this study was to evaluate the effect of negative pressure on the accuracy of IOP measurements obtained through Excursion tonometry by way of comparison to IOP measurements obtained through a pressure transducer. To isolate negative pressure as a variable, IOP was set to specified levels using a fluid column open to atmospheric pressure. The open fluid column was specifically utilized to keep IOP constant during application of negative pressure. In other words, any differences in IOP measurements via Excursion tonometry compared to direct IOP measurements from a pressure transducer could be attributed to the excursion test method itself and the effect of negative pressure on the Excursion test method.
After establishing the impact of negative pressure on the accuracy of Excursion tonometry measurements, the second objective of the study was to quantify the agreement between Excursion tonometry and pressure transducer measurements when negative pressure is allowed to impact IOP in the POC model. To do this, the fluid column was closed off from atmospheric pressure, allowing the applied negative pressure application to affect IOP in the POC model. Figure 2 illustrates the perfusion model and the site of applied negative pressure, which simulates the negative pressure environment within the MPD goggles in a clinical setting.
For this study, human cadaver eyes were obtained from the Lion’s Eye Institute for Transplant & Research (Tampa, FL, USA). Informed consent for the eyes was obtained or verified through the eye bank. As this study did not include human subjects, institutional review board approval was not required. Healthy, non-glaucomatous eyes, obtained from a pool of donors within 48 hours of death, were mounted in a perfusion model platform. Prior to use of each donor tissue, each perfusion model was conditioned for 18–24 hours at a physiologic perfusion rate (2.5 μL/min) to confirm the corneal/scleral rim was capable of maintaining a constant IOP. Each POC model was then connected to a pressure transducer (Deltran II pressure transducer), which provides direct fluid pressure measurements to compare against measurements obtained via Excursion tonometry, both with reference to atmospheric pressure. Four eyes were used in each part of the study.
To test a broad range of IOP values, the IOP was adjusted and pre-set to specified levels using a DMEM “water” column by adjusting the height of fluid connected to the infusion port. Measurements were obtained at fixed IOP settings of 10, 20, 25 and 30 mmHg. Negative pressure was applied in front of the human scleral/corneal rim from −5 to −20 mmHg, the complete range of the MPD system. Paired (Excursion tonometry and pressure transducer) measurements were collected at each IOP configuration. In total, there were 13 paired IOP (10, 20, 25, 30 mmHg) and negative pressure (0, 5, 10, 15, 20 mmHg) combinations using 4 total donor eyes for each part of the study. The configurations for part 1 and 2 are included below:
Part 1 (Open to atmospheric pressure, IOP unaffected by negative pressure application)
- Intraocular pressure 10 mmHg. Negative pressure 0, −5 mmHg.
- Intraocular pressure 20 mmHg. Negative pressure 0, −5, −10 mmHg.
- Intraocular pressure 25 mmHg. Negative pressure 0, −5, −10, −15 mmHg.
- Intraocular pressure 30 mmHg. Negative pressure 0, −10, −15, −20 mmHg.
Part 2 (Isolated from atmospheric pressure, IOP affected by negative pressure application)
- Intraocular pressure 10 mmHg. Negative pressure 0, −5 mmHg.
- Intraocular pressure 20 mmHg. Negative pressure 0, −5, −10 mmHg.
- Intraocular pressure 25 mmHg. Negative pressure 0, −10, −15, −20 mmHg.
- Intraocular pressure 30 mmHg. Negative pressure 0, −10, −15, −20 mmHg.
Measurements began at the lowest paired setting (10 mmHg IOP, 0 mmHg negative pressure) and concluded at the highest paired setting (30 mmHg IOP, 20 mmHg negative pressure). One operator (masked to the settings and results) obtained pressure measurements via Excursion tonometry. To prevent bias, another individual independent from the operator was assigned as the reader. The reader was responsible for modifying test settings and recording the IOP values as measured by the operator for the pressure transducer and Excursion tonometry. For Excursion tonometry, the Model 30 pneumatonometer was set to “manual tonometry” mode, which displays the average and standard deviation of 40 readings per second for each successful measurement, and 10 IOP measurements were obtained for each eye.
Statistical Analysis
In summary, there were 13 configurations of paired IOP (10, 20, 25 and 30 mmHg) and negative pressure (0, 5, 10, 15, 20) settings. Measurements at each configuration generated matched pair of IOP (transducer, Excursion tonometry) values. The difference between the Excursion tonometry and direct transducer pressure, defined as Δ IOP, was calculated for each configuration. At each IOP setting, the values obtained via measurement were summarized by the mean, median, standard deviation (SD), 95% confidence interval, minimum and maximum.
A two-factor ANOVA was performed to assess the effect of negative pressure on the mean IOP values across all IOP settings between Excursion tonometry and the pressure transducer. Bland-Altman plots and Box plot graphs were created to visualize the comparison in IOP measurements between the two methods. Post hoc analyses were also performed to directly compare the mean IOP values obtained at each IOP setting. A P value less than 0.05 was considered statistically significant.
Results
Part 1
The first part of the study involved a POC system open to atmospheric pressure and was designed to evaluate the effect of negative pressure on Excursion tonometry measurements by ensuring that vacuum application did not alter IOP. For each configuration of pre-set IOP and negative pressure, IOP measurements via the pressure transducer were compared against Excursion tonometry for a total of 520 measurements. The difference in IOP measurements (Excursion tonometry IOP minus pressure transducer IOP, Δ IOP) was calculated at each paired configuration of pressure transducer/Excursion tonometry measurements and compared. At the IOP settings of 10, 20, 25 and 30 mmHg, the mean Δ IOP was 1.0 ± 1.4, −0.2 ± 1.4, −0.6 ± 1.1 and −2.0 ± 1.0 mmHg, respectively. Table 1 summarizes the paired IOP measurements and the statistical comparison between Excursion tonometry and the pressure transducer across all IOP settings.
 |
Table 1 Summary of IOP Measurements and Two-Factor ANOVA: Excursion Tonometry vs Pressure Transducer |
Across all 13 combinations and all 520 paired measurements, the mean Δ IOP and SD was −0.7 ± 1.6 mmHg. Of all 520 paired measurements, all Δ IOP values were within the range of ±5 mmHg when comparing Excursion tonometer versus the pressure transducer. Figure 3 demonstrates a Bland-Altman plot of the paired IOP measurements for all IOP settings and measurement combinations.
The difference in Excursion tonometry versus the IOP obtained via the pressure transducer was also evaluated across a range of external negative pressure levels with the MPD. The negative pressure levels ranged from 0 to −20 mmHg. At 0 mmHg, the mean Δ IOP was −0.5 ± 0.1. At −5 mmHg and −10 mmHg, the mean Δ IOP was 0.1 ± 0.1 and −1.0 ± 0.1 mmHg, respectively. At −15 mmHg and −20 mmHg, the mean Δ IOP was −1.1 ± 0.2 and −2.5 ± 0.1 mmHg, respectively. Table 2 summarizes the IOP values based on negative pressure settings.
 |
Table 2 Summary of Δ IOP by Negative Pressure at Multiple Pre-set IOP: Excursion Tonometry (ETM) vs Pressure Transducer (TD) |
Part 2
In the second part, which also included 520 measurements, Δ IOP was again evaluated in a closed POC model where IOP was permitted to vary with negative pressure application. Tables 3 and 4 summarize the IOP measurements obtained in this part of the study. At the preset IOP of 10 mmHg with 0 mmHg of negative pressure applied, the mean IOP was 10.4 ± 1.4 mmHg measured with Excursion tonometry and 10.1 ± 0.3 mmHg measured via the transducer. With −5 mmHg of negative pressure, the mean IOP was 7.6 ± 1.1 mmHg with Excursion tonometry and 7.2 ± 0.4 with the pressure transducer.
 |
Table 3 Summary of IOP Measurements: 10 mmHg and 20 mmHg Configurations |
 |
Table 4 Summary of IOP Measurements: 25 mmHg and 30 mmHg Configurations |
There were three paired configurations at the 20 mmHg IOP setting with negative pressure levels of 0, −5 and −10 mmHg. At 0 mmHg, the mean IOP via Excursion tonometry was 21.0 ± 1.5 mmHg and 20.2 ± 0.4 mmHg with the pressure transducer. At negative pressure settings of −5 and −10 mmHg, the Excursion tonometry mean IOP was 17.7 ± 1.5 and 15.9 ± 1.8 mmHg, respectively. For the pressure transducer, the mean IOP at negative pressure settings of −5 and −10 mmHg was 17.3 ± 0.6 and 14.9 ± 1.2 mmHg, respectively.
At the preset IOP of 25 mmHg, negative pressure levels of 0, −10, −15 and −20 mmHg were employed. At 0 mmHg, the mean IOP was 26.7 ± 1.2 mmHg via Excursion tonometry and 25.1 ± 0.4 mmHg as measured with the pressure transducer. At negative pressure settings of −10, −15 and −20 mmHg, the mean IOP via Excursion tonometry was 20.0 ± 2.0, 17.4 ± 1.7 and 14.5 ± 1.5 mmHg, respectively. For the mean IOP via the pressure transducer, the mean IOP at negative pressure settings of −10, −15 and −20 mmHg was 19.3 ± 1.1, 16.6 ± 1.3 and 13.6 ± 1.0 mmHg, respectively.
At the highest preset IOP of 30 mmHg, four different negative pressure levels were evaluated including 0, −10, −15 and −20 mmHg. At 0 mmHg of applied negative pressure, the mean IOP was 30.6 ± 1.4 with Excursion tonometry and 30.2 ± 0.4 mmHg with the pressure transducer. At negative pressure settings of −10, −15 and −20 mmHg, the mean IOP via Excursion tonometry was 25.9 ± 2.2, 23.3 ± 2.2 and 20.7 ± 2.1 mmHg, respectively. For the pressure transducer, at applied negative pressure levels of −10, −15 and −20 mmHg, the mean IOP was 25.1 ± 1.5, 22.5 ± 1.8 and 20.1 ± 1.7 mmHg, respectively.
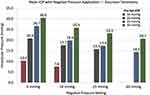
Across all preset IOPs and negative pressure settings, the mean IOP reduction as measured via Excursion tonometry was 3.1 ± 0.3 at −5 mmHg, 5.6 ± 1.3 at −10 mmHg, 8.5 ± 1.7 at −15 mmHg and 11.2 ± 1.8 at −20 mmHg. Figure 4 demonstrates the mean IOP at each negative pressure setting as measured via Excursion tonometry.
For all 520 measurements, Δ IOP was also evaluated to assess the agreement of Excursion tonometry relative to the pressure transducer during application of negative pressure. Overall, across all measurements, the mean Δ IOP was +0.7 ± 1.4 mmHg. Figure 5 demonstrates a box plot comparing the Δ IOP for all 13 configurations in the second part of this study.
Discussion
Open-angle glaucoma remains a challenging disease for patients and physicians alike owing to the difficulty in halting progression and the limitations of current treatment options.13 Approximately one in ten patients with glaucoma suffer vision loss despite treatment and more than 120,000 cases of blindness are attributable to glaucoma.14 Thus, continued innovation related to treatment is sought by providers, particularly if newly developed treatment options are non-invasive and titratable. The MPD represents a novel treatment device capable of immediate IOP reduction referenced to atmosphere while the device is worn with active application of negative pressure.7,9 However, the physical structure of the device while properly situated on a subject prevents IOP measurement with conventional tonometry methods and a modified technique, known as Excursion tonometry, was developed.10
A prior study10 investigated the reproducibility and repeatability of Excursion tonometry with favorable results indicating this recently described technique represents an acceptable and reliable method of IOP measurement. Importantly, this prior study also established that the Tono-Pen cover had minimal impact on pressure measurements and did not introduce a significant amount of bias at any IOP level. While this aforementioned study reported favorable results regarding the precision and accuracy of Excursion tonometry, this prior work did not include active negative pressure application during the study. Thus, the first part of this current study aimed to investigate the impact of localized negative pressure on the measurement accuracy of Excursion tonometry. To isolate the effect of negative pressure on the Excursion measurement, an open fluid column system was used to ensure applied negative pressure did not result in changes to the pre-set IOP. The second part of this study employed a closed system to evaluate the combined direct effect of negative pressure application on the measurement accuracy of Excursion tonometry and IOP.
In the first part of the study, the mean Δ IOP was −0.7 ± 1.6 mmHg across all 520 measurements, supporting the measurement accuracy throughout a range of IOP settings. Further, all paired measurements were within the range of ±5 mmHg when comparing the measurement obtained via the pressure transducer versus Excursion tonometry. These values are well within the acceptable limits (±5 mmHg of reference tonometer) set forth by the ANSI requirements for new tonometers (ANSI Z80.10). Further, statistical analysis revealed no statistically significant influence of negative pressure application (P > 0.05) between the IOP values measured by the reference pressure transducer versus the Excursion tonometry across all configurations. These results demonstrate that negative pressure application with the MPD has a negligible impact on the measurement accuracy of Excursion tonometry.
The second part of this study involved a closed POC model to evaluate the agreement between Excursion tonometry and in-line pressure transducer measurements as well as the response of IOP to applied negative pressure in a POC model. Prior work has highlighted the IOP-lowering ability of the MPD as measured via Excursion tonometry in a clinical setting and the results of this study align with what has been previously reported.7,9,15 In this study, there was a stepwise increase in IOP reduction with increased negative pressure levels across all 4 preset IOPs (10, 20, 25, 30 mmHg), highlighting the capability of the MPD to lower IOP in a titratable fashion. For instance, at the preset IOP of 25 mmHg, with applied negative pressure levels of −10, −15 and −20 mmHg, there was an IOP reduction of 6.7 (25%), 9.3 (35%) and 12.2 (46%) mmHg, respectively. Further, as observed in Figure 5, there was favorable agreement between the two measurement methods across all configurations with minimal overall bias (+0.7 ± 1.4) of Excursion tonometry relative to the transducer. Overall, the results of this study offer further support of Excursion tonometry as a reliable method of IOP measurement referenced to atmospheric pressure and suggest application of negative pressure has minimal to no impact on the measurement accuracy.
This study is not without limitations. The POC system is a well-studied and established model for laboratory investigation but does not perfectly emulate how a real cornea with specific morphologic features (thickness, curvature) and biomechanical properties would behave under the application of negative pressure. Moreover, it is well established that biomechanical properties of the cornea may affect IOP measurements but these parameters were not explored or collected in this present study. Despite these limitations, this study demonstrates that applied negative pressure has minimal to no impact on the measurement accuracy of Excursion tonometry and provides data supporting the IOP-lowering ability of the MPD in a benchtop setting.
Conclusion
This study provides additional evidence in support of Excursion tonometry as an accurate method of IOP measurement for the MPD system and the findings are consistent with the prior study10 evaluating the repeatability and reproducibility of this newly developed method of IOP measurement. Importantly, this present study demonstrates that application of negative pressure, which represents the IOP-lowering mechanism of the MPD, does not impact the measurement accuracy of Excursion tonometry. In addition, the IOP-lowering results in this study corroborate what has been demonstrated in a clinical setting and further support the effectiveness of the MPD in lowering IOP.
Data Sharing Statement
The data set collected and analyzed for this present study is available from the corresponding author per reasonable request.
Compliance with Ethics Guidelines
All procedures conducted were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Human eyes were obtained from the Lion’s Eye Institute for Transplant & Research (Tampa, FL, USA). Informed consent for the eyes was obtained or verified through the eye bank.
Acknowledgments
We thank the operators who performed the tasks described in this study to generate the data and study results.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
Article processing fees for this publication were funded by Equinox Ophthalmic, Inc and the study was sponsored by Equinox Ophthalmic, Inc. There were no other funding sources.
Disclosure
TJF, DAA are paid consultants for Equinox Ophthalmic, Inc. EB, NC and PY are employees of Equinox Ophthalmic, Inc. The authors report no other conflicts of interest in this work.
References
1. Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the early manifest glaucoma trial. Arch Ophthalmol. 2002;120(10):1268–1279. doi:10.1001/archopht.120.10.1268
2. Kingman S. Glaucoma is second leading cause of blindness globally. Bull World Health Organ. 2004;82(11):887–888. doi:10.1590/S0042-96862004001100019
3. Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121(11):2081–2090. doi:10.1016/j.ophtha.2014.05.013
4. Weinreb RN, Ong T, Sforzolini BS, Vittitow JL, Singh K, Kaufman PL. A randomised, controlled comparison of latanoprostene bunod and latanoprost 0.005% in the treatment of ocular hypertension and open angle glaucoma: the VOYAGER study. Br J Ophthalmol. 2014;99(6):
5. Lavia C, Dallorto L, Maule M, Ceccarelli M, Fea AM. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS One. 2017;12(8):e0183142. doi:10.1371/journal.pone.0183142
6. Shah M. Micro-invasive glaucoma surgery – an interventional glaucoma revolution. Eye Vis. 2019;6(1):29. doi:10.1186/s40662-019-0154-1
7. Swan RJ, Ferguson TJ, Shah M, et al. Evaluation of the IOP-lowering effect of a multi-pressure dial at different negative pressure settings. Transl Vis Sci Technol. 2020;9(12):19. doi:10.1167/tvst.9.12.19
8. Ethier CR, Yoo P, Berdahl JP. The effects of negative periocular pressure on intraocular pressure. Exp Eye Res. 2020;191:107928. doi:10.1016/j.exer.2020.107928
9. Goldberg JL, Jiminez-Roman J, Hernandez-Oteyza A, Quiroz-Mercado H. Short-term evaluation of negative pressure applied by the multi-pressure dial system to lower nocturnal IOP: prospective, controlled, intra-subject study. Ophthalmol Ther. 2021;10(2):349–358. doi:10.1007/s40123-021-00343-4
10. Ferguson TJ, Knier CG, Chowdhury UR, et al. Intraocular pressure measurement with pneumatonometry and a tonometer tip cover. Ophthalmol Ther. 2020;9(1):127–137. doi:10.1007/s40123-020-00235-z
11. Bahler CK, Fautsch MP, Hann CR, Johnson DH. Factors influencing intraocular pressure in cultured human anterior segments. Investig Opthalmology Vis Sci. 2004;45(9):3137. doi:10.1167/iovs.04-0154
12. Pang IH, McCartney MD, Steely TH, Clark AF. Human ocular perfusion organ culture: a versatile ex vivo model for glaucoma research. J Glaucoma. 2000;9(6):468–479. doi:10.1097/00061198-200012000-00009
13. Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003;121(1):48–56. doi:10.1001/archopht.121.1.48
14. Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. doi:10.1136/bjo.2005.081224
15. Ferguson TJ, Radcliffe NM, Van Tassel SH, et al. Overnight safety evaluation of a multi-pressure dial in eyes with glaucoma: prospective, open-label, randomized study. Clin Ophthalmol. 2020;14:2739–2746. doi:10.2147/OPTH.S256891
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.