Back to Journals » Clinical Ophthalmology » Volume 17
Intraocular Lens Formula Comparison of Flanged Intrascleral Intraocular Lens Fixation with Double Needle Technique
Authors Malach DS , Guest JM, Adam C, Joffe J, Le K, Kim C, Lin X
Received 19 October 2022
Accepted for publication 2 February 2023
Published 12 March 2023 Volume 2023:17 Pages 837—842
DOI https://doi.org/10.2147/OPTH.S389325
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Supplementary video of "Refractive outcomes of flanged double needle technique" [ID 389325].
Views: 131
Daniel S Malach,1 John Michael Guest,1 Christopher Adam,1 Jonah Joffe,2 Kim Le,2 Chaesik Kim,1 Xihui Lin1
1Kresge Eye Institute/Wayne State University Department of Ophthalmology, Detroit, MI, USA; 2Henry Ford Hospital Department of Ophthalmology, Detroit, MI, USA
Correspondence: Xihui Lin, Kresge Eye Institute/Wayne State University Department of Ophthalmology, 4717 St. Antoine, Detroit, MI, 48201, USA, Email [email protected]
Purpose: To analyze visual outcomes and accuracy of intraocular lens (IOL) calculation formulas in predicting postoperative outcomes in patients undergoing flanged intrascleral IOL fixation.
Design: Case Series.
Subjects: Twenty-three patients who had undergone secondary IOL placement using flanged intrascleral fixation technique.
Methods: Retrospective chart review.
Main Outcome Measures: Corrected distance visual acuity (CDVA) and postoperative spherical equivalent based on manifest refraction.
Results: Visual acuity improved from 20/577 to 20/58. Overall, the actual refraction was 0.06 D more myopic than predicted. Holladay 2, Sanders Retzlaff Kraff/Theoretical (SRK/T) and Barrett Universal II resulted in mild myopic surprise (− 0.55, − 0.18 and − 0.20 D). Haigis and Hill-RBF (Radial Basis Function) resulted in mild hyperopic surprise (+0.28 and +0.28 D). Hoffer Q and Holladay 1 were the most accurate (− 0.02D and − 0.08 D).
Conclusion: Flanged intrascleral IOL fixation improved vision even in patients with other posterior segment pathologies. The effective lens positioning is likely similar to in-the-bag positioning. Hoffer Q and Holladay 1 formulas with in-the-bag calculations were the most accurate.
Keywords: aphakia, cataract, flanged technique, refractive, secondary intraocular lens
Introduction
The ideal surgical outcome of cataract extraction results in intracapsular implantation of an intraocular lens (IOL). However, certain patient factors may preclude placement of an intracapsular lens, including Pseudoexfoliation Syndrome, Marfan Syndrome, ocular trauma with zonular loss or instability, and intraoperative challenges resulting in damage to the capsular bag or zonular apparatus. In these instances, several techniques exist to facilitate placement of asecondary IOL including anterior chamber or sulcus placement, iris fixation or scleral fixation.1,2 Anumber of methods of scleral fixation have been utilized, including suture fixation, fibrin glue, scleral pockets, or other sutureless techniques.3–6,8 Dr.Shin Yamane first introduced his flanged double needle technique for scleral fixation of an IOL at the World Ophthalmology Conference in 2014.8 Since that time, several studies have reported good visual outcomes with alow incidence of intra- and postoperative complications.8–11 Prior to the double needle technique, amodified version of the single needle Yamane technique had been used with repeated success.7 However, there is apaucity of literature regarding which currently available IOL formula is most accurate in predicting postoperative refractive outcomes in this patient population. The goal of this study is to analyze the refractive outcomes of patients undergoing flanged intrascleral intraocular lens fixation and to compare the accuracy of currently available IOL formulas in predicting postoperative refractive outcomes.
Methods
Electronic medical records of all adult patients at the Kresge Eye Institute, Detroit, Michigan, who had undergone secondary intraocular lens placement with the flanged intrascleral fixation technique from 2014 to 2019 were reviewed. In instances of successive bilateral surgery, both eyes were used in the study analysis individually. Exclusion criteria included insufficient follow-up data, surgical complications resulting in an inability to place ascleral-fixated lens, or ahistory of keratorefractive surgery. Study approval was obtained from the Wayne State University Institutional Review Board. Research adhered to the Tenets of the Declaration of Helsinki and Good Clinical Practice. Patient data collected for analysis included age, gender, ethnicity, ocular comorbidities, reason for secondary IOL, optical biometry measurements, axial length (AL) measurement, preoperative and postoperative corrective distance visual acuity (CDVA), preoperative and postoperative spherical equivalent based on manifest refraction, and intraoperative and postoperative complications. The axial length was measured using optical biometry (Carl Zeiss Meditec AG, IOLMaster® 500, Jena, Germany). In the instance of poor signal strength with optical biometry, applanation ultrasound biometry was used for AL measurements.
The predicted postoperative spherical equivalent was calculated using the Holladay 1, Holladay 2, Hoffer Q, Sanders Retzlaff Kraff/Theoretical (SRK/T), Haigis, Barrett Universal II, and Hill-RBF (Radial Basis Function) formulas based on in-the-bag placement of the IOL.
All patients underwent uneventful 25 gauge pars plana vitrectomy and secondary IOL placement using asimilar surgical technique with an Alcon® MA60AC (Alcon, Geneva, Switzerland) IOL fixated 2 millimeters posterior to the limbus. After acomplete pars plana vitrectomy with peripheral vitreous base shave, the intraocular lens was injected into the anterior chamber through a2.75mm superior limbal wound. Our own analysis of effective lens positioning data shows even 2mm has tendency of amore posterior effective lens positioning; thus, we are hesitant to use 2.5mm. Bent 27 gauge needles were used for haptic docking and high-temperature cautery was used for creation of flanged haptic bulbs (see Supplementary Video --> or key surgical steps). All patients were prescribed the same postoperative drop regimen of atopical fluoroquinolone (moxifloxacin), topical cycloplegic/mydriatic (homatropine 5%), and topical steroid (prednisolone acetate 1%). Patients were followed for 3 months postoperatively.
Statistical Analysis
Continuous demographic data were summarized as means and standard deviations, while categorical variables were tabulated as percentages and frequencies. Non-parametric linear regression was used to determine the correlation between predicted and postoperative spherical equivalent for each formula. Atwo-tailed independent t-test was performed to determine if the mean postoperative spherical equivalent for each formula was significantly different from the predicted value. Intraclass correlations (ICC) were performed to assess the reliability of each formula in predicting postoperative spherical equivalent. The percentage of patients with postoperative spherical equivalent within ± 0.25D, ± 0.50D, ± 0.75D and ± 1.00 Dof predicted spherical equivalent for each formula was calculated and compared using Cochran’s QTest. All statistical tests were two-sided and ap-value of <0.05 was used to determine statistical significance. All analyses were performed on IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp., Armonk, N.Y., USA).
Results
Twenty-four eyes of 23 patients (15 male, 8 female) were included in this study. The mean age at the time of surgery was 64.60 ±13.25 years. Demographic information can be found in Table1. Indications for secondary IOL included aphakia (8 eyes), traumatic or non-traumatic dislocated crystalline lens with zonulopathy (8 eyes), dislocated or subluxated Posterior chamber intraocular lenses (PCIOL) (7 eyes) or PCIOL exchange (1 eye). The one patient requiring aPCIOL exchange had developed corneal ectasia after implantation of amultifocal IOL and developed intolerable glare/haloes. There were no significant intraoperative complications. Asmall percentage of patients had comorbid retinal or corneal pathology that limited their ultimate CDVA. The mean axial length was 24.22 ± 2.01 millimeters.
 |
Table1 Patient Characteristics --> |
Overall, the mean CDVA significantly improved from logarithm of the minimum angle of resolution (logMAR) 1.46 (snellen 20/577) before surgery to logMAR 0.46 (snellen 20/58) after surgery (p= 0.0027). Postoperative complications were rare and were limited to cystoid macular edema (CME) (12.5%), postoperative transient intraocular pressure (IOP) spike (8.3%) and mild lens tilt (4.2%) that did not require reoperation. In the instance of post-op CME and IOP spike, all cases were successfully treated with topical medications. The mean postoperative residual refractive error for all formulas combined was −0.06 + 0.29 diopters. Most formulas had amild myopic surprise, except for Haigis and Hill-RBF. Table2 shows the descriptive statistics for predicted spherical equivalent and mean and absolute errors for each formula. There was no statistically significant difference between the predicted and actual postoperative spherical equivalents for all formulas (p> 0.05).
 |
Table2 Descriptive Statistics |
Table3 shows the ICC and R2 values for nonparametric regression analysis. All ICC values were less than 0.5, indicating poor repeatability for each formula. All R2 values were less than 0.3, indicating poor correlation between predicted and actual postoperative spherical equivalent for each formula.Table4 shows the percentage of patients for each formula that had apostoperative spherical equivalent within 0.25, 0.5, 0.75 and 1.00 diopters of the predicted spherical equivalent. Hoffer Qresulted in the highest percentage of patients within 0.5 and 1.0 diopters (27.8% and 77.8%, respectively); however, this result was not statistically significant.
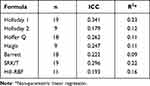 |
Table3 Intraclass Correlation and Regression Analysis |
 |
Table4 Distribution of Eyes Within Diopter Ranges of Predicted Spherical Equivalent |
Discussion
Sutureless transscleral fixation of aPCIOL with the modified double-needle technique is asafe and effective method of visual rehabilitation in patients with inadequate capsular or zonular support. As the utilization of the modified Yamane technique increases worldwide and patient expectations for surgical outcomes become more demanding, more data is needed to improve the accuracy of refractive outcomes. The large number of currently available IOL formulas is indicative of the difficulty in accurately predicting postoperative refractive targets.12–17 This is especially true in patients who undergo scleral-fixation of an IOL as opposed to traditional phacoemulsification with in-the-bag placement.18–22
A study from 2021 assessing the accuracy of lens calculation formulas using the flanged intrascleral intraocular lens fixation with the double needle technique pre dates ours. Results of the prior study found that refractive outcomes using the Yamane technique were less accurate when compared to standard cataract surgery.23 While our study further demonstrated the variability of this semi new technique. The Hoffer Q(−0.02D) formula had the smallest mean prediction error and highest percentage of patients within 0.50 and diopters of the predicted spherical equivalent among all formulas in this study, although this result was not statistically significant. None of the formulas utilized in this study had predictable and repeatable refractive outcomes, as all ICC values were less than 0.3 and all R2 values were less than 0.5. However, the mean prediction errors for each formula and for all patients were less than 0.5 Dand there was no statistically significant difference between the predicted and actual postoperative spherical equivalent on manifest refraction. Our data highlight the difficulty in obtaining repeatable refractive outcomes in this specific patient population. Although all of the surgeries included in this study were performed by the same surgeon utilizing asimilar surgical technique, certain patient-specific factors may have led to the variation in effective lens position and refractive outcomes. In addition, every patient underwent apars plana vitrectomy prior to IOL (Aclon MA60AC) insertion.
Although not required, this was undertaken to prevent any retinal complications as well as to allow for posterior placement of the balanced salt solution (BSS) infusion to facilitate surgical technique. In addition, from the authors’ experience, there is an increased risk of developing giant retinal tear associated retinal detachments in certain eyes if the vitreous base is not debulked through apars plana approach. Previous studies have demonstrated the unpredictable refractive outcomes in patients with previous or concurrent pars plana vitrectomy undergoing cataract phacoemulsification with IOL placement,24–29 which may play arole in the refractive variability in this patient population. Effective lens position for these flanged scleral fixated lenses is highly dependent on the integrity of the natural curvature of the prolene haptics as well as the angle of scleral insertion. Together, these two factors likely played apart in the variability of the data. This study has several limitations, including its retrospective nature and small sample size. The small sample size precluded subgroup analysis, specifically comparison of lens formulas in patients of differing axial lengths. Our study failed to show asignificant difference between predicted and actual spherical equivalent for each formula. However, this result may be due to small sample size. Several formulas had asmaller sample size than others due to the lack of anterior chamber depth measurements in aphakic patients that is required to calculate predicted spherical equivalent in newer generation formulas. There were also several patients included in the cohort that had macular or corneal pathology that limited their CDVA. However, as an aggregate, our data still highlighted important trends in the predicted refraction and the formulas. Specifically, although there is no statistical significance between the accuracy of the formulas, two of the formulas had asignificant hyperopic trend. We would recommend relying more on Hoffer Qor Holladay 1 and target for slight myopia.
In conclusion, the flanged intrascleral intraocular lens fixation with the double needle technique is asafe and effective method of IOL (Alcon MA60AC) fixation in patients requiring asecondary IOL. Refractive outcomes are variable and may be slightly more myopic than predicted with currently available IOL formulas, but are overall similar to in-the-bag placement. The most accurate formulas were Hoffer Qand Holladay 1 while Haigis and Hill-RBF had ahyperopic trend. Given this variability and the tendency of hyperopic surprises with certain formulas, it is safer to aim for slight myopia in these patients. In addition, they should be appropriately counseled preoperatively on the variability of refractive outcomes.
Data Sharing Statement
All data accessed complied with relevant data protection and privacy regulations.
Ethics and Consent Statements
This research study was approved by Wayne State University IRB. All research protocols followed the appropriate ethical standards. This was aretrospective comparative study that did not require direct patient contact. Thus, informed consent is not applicable.
Acknowledgments
American Academy of Ophthalmology Annual Meeting, San Francisco CA, 2019.
Funding
-->Non-restricted grant to the Department of Ophthalmology, Visual and Anatomical Sciences from Research to Prevent Blindness, Inc.
Disclosure
The authors report no conflicts of interest in this work.
References -->
1. WagonerMD, CoxTA, AriyasuRG, JacobsDS, KarpCL. Intraocular lens implantation in the absence of capsular support; areport by the American Academy of Ophthalmology (Ophthalmic Technology Assessment). Ophthalmology. 2003;110:840–859.
2. StarkWJ, GottschJD, GoodmanDF, etal. Posterior chamber intraocular lens implantation in the absence of capsular support. Arch Ophthalmol. 1989;107:1078–1083. doi:10.1001/archopht.1989.01070020140048
3. MonteiroM, MarinhoA, BorgesS, RibeiroL, CorreiaC. Scleral fixation in eyes with loss of capsule or zonule support. JCataract Refract Surg. 2007;33(4):573–576. doi:10.1016/j.jcrs.2006.10.073
4. MittelviefhausH, WitschelH. Transscleral suture fixation of posterior-chamber lenses after cataract extraction associated with vitreous loss. Ger JOphthalmol. 1995;4:80–85.
5. WallmanAC, MonsonBK, AdelbergDA. Transscleral fixation of afoldable posterior chamber intraocular lens. JCataract Refract Surg. 2015;41:1804–1809.
6. AgarwalA, KumarDA, JacobS, BaidC, AgarwalA, SrinivasanS. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. JCataract Refract Surg. 2008;34:1433–1438.
7. RandersonEL, BogaardJD, KoenigLR, HwangES, WarrenCC, KoenigSB. Clinical outcomes and lens constant optimization of the zeiss CT Lucia 602 lens using amodified Yamane technique. Clin Ophthalmol. 2020;14:3903–3912.
8. YamaneS, SatoS, Maruyama-InoueM, KadonosonoK. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmol. 2017;124:1136–1142.
9. StemMS, WaCA, TodorichB, WoodwardMA, WalshMK, WolfeJD. 27-gauge sutureless intrascleral fixation of intraocular lenses with haptic flanging: short-term clinical outcomes and adisinsertion force study. Retina. 2018;39:2149.
10. KelkarA, KelkarJ, KothariA, etal. Comparison of two modified sutureless techniques of scleral fixation of intraocular lens. JAMA Ophthalmic Surg Lasers Imaging Retina. 2018;49:e129–e134.
11. BruninG, SajjadA, KimEJ, etal. Secondary intraocular lens implantation: complication rates, visual acuity, and refractive outcomes. JCataract Refract Surg. 2017;43:369–376. doi:10.1016/j.jcrs.2016.12.024
12. MellesRB, HolladayJT, ChangWJ. Accuracy of intraocular lens calculation formulas. Ophthalmology. 2018;125:169–178. doi:10.1016/j.ophtha.2017.08.027
13. NorrbyS. Sources of error in intraocular lens power calculation. JCataract Refract Surg. 2008;34:368–376. doi:10.1016/j.jcrs.2007.10.031
14. GokceSE, CookeDL, WangL, KochDD, Al-MohtasebZ. Accuracy of 8 intraocular lens calculation formulas in relation to anterior chamber depth in patients with normal axial length. JCataract Refract Surg. 2018;44:362–368. doi:10.1016/j.jcrs.2018.01.015
15. ShrivastavaAK, BeheraP, KumarB, NandaS. Precision of intraocular lens power prediction in eyes shorter than 22mm: an analysis of 6 formulas. JCataract Refract Surg. 2018;44:1317–1320. doi:10.1016/j.jcrs.2018.07.023
16. KaneJX, Van HeerdenA, AtikA, PetsoglouC. Intraocular lens power formula accuracy: comparison of 7 formulas. JCataract Refract Surg. 2016;42:1490–1500. doi:10.1016/j.jcrs.2016.07.021
17. DarcyK, GunnD, TavassoliS, SparrowJ, KaneJX. Assessment of the accuracy of new and updated intraocular lens power calculation formulas in 10930 eyes from the UK National Health Service. JCataract Refract Surg. 2020;46:2–7. doi:10.1016/j.jcrs.2019.08.014
18. HayashiK, HayashiH, NakaoF, HayashiF. Intraocular lens tilt and decentration, anterior chamber depth, and refractive error after trans-scleral suture fixation surgery. Ophthalmology. 1999;106:878–882. doi:10.1016/S0161-6420(99)00504-7
19. SindalMD, NakhwaCP, SenguptaS. Comparison of sutured versus sutureless scleral-fixated intraocular lenses. JCataract Refract Surg. 2016;42:27–34. doi:10.1016/j.jcrs.2015.09.019
20. GanekalS, VenkataratnamS, DorairajS, JhanjiV. Comparative evaluation of suture-assisted and fibrin glue-assisted scleral fixated intraocular lens implantation. JRefract Surg. 2012;28:249–252. doi:10.3928/1081597X-20120221-01
21. KjekaO, BohnstedtJ, MebergK, SelandJH. Implantation of scleral-fixated posterior chamber intraocular lenses in adults. Acta Ophthalmol. 2008;86:537–542. doi:10.1111/j.1600-0420.2007.01095.x
22. MimuraT, AmanoS, SugiuraT, etal. 10-year follow-up study of secondary transscleral ciliary sulcus fixated posterior chamber intraocular lenses. Am JOphthalmol. 2003;136(5):931–933. doi:10.1016/S0002-9394(03)00893-6
23. McMillinJ, WangL, WangMY, etal. Accuracy of intraocular lens calculation formulas for flanged intrascleral intraocular lens fixation with double-needle technique. JCataract Refract Surg. 2021;47:855–858. doi:10.1097/j.jcrs.0000000000000540
24. LamsonTL, SongJ, AbazariA, WeissbartSB. Refractive outcomes of phacoemulsification after pars plana vitrectomy using traditional and new intraocular lens calculation formulas. JCataract Refract Surg. 2019;45:293–297. doi:10.1016/j.jcrs.2018.10.032
25. Falkner-RadlerCI, BeneschT, BinderS. Accuracy of preoperative biometry in vitrectomy combined with cataract surgery for patients with epiretinal membranes and macular holes; results of aprospective controlled clinical trial. JCataract Refract Surg. 2008;34:1754–1760. doi:10.1016/j.jcrs.2008.06.021
26. SuzukiY, SakurabaT, MizutaniH, MatsuhashiH, NakazawaM. Postoperative refractive error after simultaneous vitrectomy and cataract surgery. Ophthalmic Surg Lasers. 2000;31:271–275. doi:10.3928/1542-8877-20000701-03
27. KovácsI, FerenczM, NemesJ, SomfaiG, SalaczG, RécsánZ. Intraocular lens power calculation for combined cataract surgery, vitrectomy and peeling of epiretinal membranes for macular oedema. Acta Ophthalmol Scand. 2007;85:88–91. doi:10.1111/j.1600-0420.2006.00772.x
28. JeoungJW, ChungH, YuHG. Factors influencing refractive outcomes after combined phacoemulsification and pars plana vitrectomy: results of aprospective study. JCataract Refract Surg. 2007;33:108–114. doi:10.1016/j.jcrs.2006.09.017
29. ShioyaM, OginoN, ShinjoU. Change in postoperative refractive error when vitrectomy is added to intraocular lens implantation. JCataract Refract Surg. 1997;23:1217–1220. doi:10.1016/S0886-3350(97)80319-7
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
