Back to Journals » Infection and Drug Resistance » Volume 15
Intestinal Parasitic Infections Among Patients Who Visited Woldia Comprehensive Specialized Hospital’s Emergency Department Over a Six-Year Period, Woldia, Ethiopia: A Retrospective Study
Authors Rega S, Melese Y, Geteneh A , Kasew D , Eshetu T , Biset S
Received 7 April 2022
Accepted for publication 16 June 2022
Published 21 June 2022 Volume 2022:15 Pages 3239—3248
DOI https://doi.org/10.2147/IDR.S369827
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Solomon Rega,1 Yimer Melese,2 Alene Geteneh,3 Desie Kasew,4 Tegegne Eshetu,5 Sirak Biset4
1Department of Medical Laboratory Science, Woldia Comprehensive Specialized Hospital, Woldia, Ethiopia; 2Department of Medical Laboratory Science, Dessie Health Science College, Dessie, Ethiopia; 3Department of Medical Laboratory Science, College of Health Sciences, Woldia University, Woldia, Ethiopia; 4Department of Medical Microbiology, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 5Department of Medical Parasitology, School of Biomedical and Laboratory Sciences, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Sirak Biset, Tel +251 911-598-568, Email [email protected]
Background: Despite ongoing intensive public health intervention efforts, intestinal parasitic infections (IPIs) remain a major public health problem in developing countries, including Ethiopia. Having updated epidemiological data focusing on the top common IPIs that cause emergency visits is crucial for implementing area-specific and evidence-based intervention strategies. Hence, this study aimed to determine the prevalence of IPIs in Woldia Comprehensive Specialized Hospital’s (WCSH) emergency laboratory over a six-year period.
Methods: An institutional-based retrospective study was conducted to assess the prevalence of IPIs over a six-year period (2014– 2019) using a recorded saline wet-mount stool sample examination result in the laboratory logbook at WCSH’s emergency department.
Results: In this study, of the total of 11,281 clinically suspected individuals who were requested for stool sample examination, 3908 (34.6%) individuals were diagnosed with IPs. The majority of confirmed cases were caused by protozoan parasites (32.9%), followed by helminth infections (1.7%). A slight fluctuating trend in the prevalence of IPs was observed in the six-year study period, with the highest prevalence documented in the year of 2014 (41.3%) and the lowest in 2017 (28.0%). Entamoeba histolytica/dispar and Giardia lamblia accounts for 95% of the IPs. The prevalence of protozoan infection was significantly higher in females (p-value = 0.0101), while H. nana (p-value =0.0138) and E. vermicularis (p-value = 0.0201) infections were higher in males. The highest and the lowest IP prevalence were reported in the age groups of 45– 54 years (40%) and under five years (25.6%), respectively.
Conclusion and Recommendations: In the study area, nearly one-third of patients with emergency visits due to gastrointestinal symptoms were infected with IPs. This underlines the severity of the problem in the study area, which requires a collaborative effort of concerned bodies to minimize the burden of IP to the level where it is no longer a public health threat.
Keywords: intestinal parasite infection, protozoa, helminth, emergency, Ethiopia
Introduction
Although intestinal parasitic infections (IPIs) are preventable neglected tropical infections, they continue to be a major public health issue that blights the lives of billions of people worldwide.1 The public health consequences of IPIs are particularly pronounced in the tropical and subtropical regions of low-income countries where potable water is scarce, sanitation is poor, and people are experiencing substandard lifestyles.2 Soil-transmitted helminths like Ascaris lumbricoides (A. lumbricoides), Trichiuris trichiuria (T. trichiuria), and hookworms are among the most prevalent helminth infections whereas Entamoeba histolytica (E. histolytica) and Giardia lamblia (G. lamblia) are the predominant protozoan infection.3,4 In particular, protozoan parasites account the majority causes of IPIs than helminths in developing countries.3 Globally, an estimated 3.5 billion people are affected; 450 million are symptomatic, and more than 200,000 people deaths are reported annually due to IPIs.5,6 Infections with IPs are not only responsible for morbidity and mortality but they also cause nutritional problems (such as stunted growth, low vitamin A, iron deficiency anemia, weight loss, and chronic blood loss), as well as compromise psychological and social well-being. Mental development impairment also the other public health challenges of IPIs, particularly in children (such as impaired growth, decreased school attendance, cognitive impairment, decreased educational achievement, and adult productivity).1,6 In particular, Sub-Saharan Africa (SSA) countries disproportionately take the lion share of the global burden of the IPIs in association with poor socio-economic status, lack of pure water supply, poor sanitation, inadequacy of healthcare center, poor community awareness as well as the prevailing bad climatic and environmental conditions.4,7,8 Existing evidence indicates that the prevalence of IPIs in different areas of SSA exceeds 50%.9
Among SSA countries, Ethiopia ranks second only to Nigeria in the prevalence of IPIs, accounting for approximately 50,000 deaths annually in the country.1,10 However, the World Health Organization (WHO) continues to face challenges in achieving its goal of eliminating or reducing IPs, many of which are Neglected Tropical Diseases (NTDs), to the point where they no longer pose a public health threat in endemic areas due to a lack of updated epidemiological data on the burden of IPs and delivering alternative intervention packages.11 Thus, conducting longitudinal studies in different localities are crucial in designing and implementing effective preventive and control strategies for IPs in Ethiopia, where there is a significant economic constraint on medicine purchase and mass treatment. Furthermore, identifying the common parasitic infections that cause people to visit emergency healthcare facilities in a particular community is critical for developing area-specific, evidence-based public health intervention programs. Despite this, compiled epidemiological findings on the magnitude of IPIs in the study area and surrounding community have not previously been disseminated in the scientific community, and the current study is the first to our knowledge. However, although the burden of parasitic infections in the study area has not previously been well documented in scientific journals, health professionals working in the area report that a significant number of individuals visiting the emergency department are due to parasitic infection. Therefore, this study was designed to determine how many clinical cases in the community that require immediate medical care are due to IPI and to prioritize the top IP species among patients who visited WCSH’s emergency department between 2014 and 2019.
Materials and Methods
Study Area
This study was conducted in WCSH’s emergency department in Woldia town, Northeastern Ethiopia. Woldia serves as the administrative center of the North Wollo zone of Amhara regional state. The town is located at a latitude of 11° 46′ 50 “N and a longitude of 39° 36′ 0”E with an elevation of 2112 meters above sea level. According to the 2014 national population project conducted by the central statistical agency of Ethiopia (CSA), there are about 180,000 inhabitants in the town. Regarding the health infrastructure, the town has one public hospital, two public health centers, and more than fifteen private clinics. The hospital has been serving the residents of North Wollo as well as nearby populations from the Tigray and Afar regions.
Study Design and Population
A hospital-based retrospective study was conducted to determine the prevalence and distribution of IPIs over the last six years at the emergency department of WCSH. All individuals suspected of having an IPI who provided stool samples for examination using the direct wet mount laboratory method and were registered in the hospital’s emergency laboratory logbook were included in the study population.
Inclusion and Exclusion Criteria
Participants who had full recorded data such as age, sex, and year of diagnosis were included in the study, whereas individuals who had incomplete recorded information in the logbook were excluded.
Data Collection Tools and Techniques
Prior to extracting our variable of interest for this study, a data extraction sheet that was specifically designed to extract participants’ demographic data (age, gender), year of diagnosis, and laboratory investigation results was prepared using Microsoft Excel. Then, clients’ gender, age, date of diagnosis, and species of parasite detected were transferred from the laboratory logbook to the preprepared data extraction excel sheet. Only data from individuals with a complete record of data in the laboratory logbook were collected. Based on this, we extracted data for only 11, 281 clinically suspected individuals for intestinal parasitic infections who had stool examinations between 2014 and 2019. All extracted stool examination results were examined using the direct saline wet-mount laboratory technique, which is the only laboratory method used in the hospital laboratory for the diagnosis of intestinal parasites. To assure the quality and consistency of the data, data collectors were trained regarding the data extraction tool, variables of interest, and the objective of the study. Besides, every activity of the data extraction and entry process was supervised by the study team members.
Data Processing and Analysis
Data were coded and checked for completeness using Epi-data software before being transferred to SPSS software for statistical analysis. Descriptive statistics were used to show the distribution of IP in terms of individuals’ sex, age, and diagnosis year. A Pearson’s X2 test was used to assess the association between variables, and a p-value of < 0.05 was considered statistically significant. The results were displayed using text, graphs, and tables.
Result
Over the six-year period, a total of 11,281 patients were requested stool sample for the diagnosis of IPs at the Woldia hospital emergency laboratory. Of these, the majority, 5968 (52.9%), were females. The age of the patients ranged from 1 to 95 years, with a mean age of 24.68 (±16.62 SD) years. The highest proportion of patients visiting the hospital emergency laboratory unit for IP examinations was within the age group of 15–24 years (28.5%), followed by 25–34 (21.8%) and 5–14 (14.6%) years. Overall, infection with intestinal parasite was found to be 34.6% (3908/11,281) with a fluctuated trend prevalence across years ranged from 28.0% to 41.3%. The highest prevalence of intestinal infections was recorded in the year of 2014 (41.3%) while the least case in 2017 (28.0%) (Figure 1). The IP infection rate was found to be higher in patients with an age group of 45–54 years (40%), followed by >54 years (39.2%) and 25–34 (37%) years (Table 1).
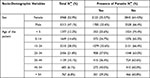 |
Table 1 Distribution of IPIs Prevalence of Among Participants’ Gender and Age Diagnosed at the Emergency Department of WCSH, 2014–2019 |
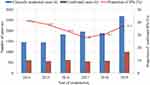 |
Figure 1 Trend prevalence of IPIs among individuals requested for stool examination at the WCSH’s emergency department from 2014–2019 (n=11,281). |
The Proportion of IPs
Overall, eight IP species were detected in this study. Of these, two were protozoan parasites, which were responsible for the majority of the case in the study area, 3716 (95%). Entamoeba histolytica/dispar 2306 (59%) was the leading IP responsible for emergency admission, followed by G. lamblia 1174 (30%), and mixed infection (Entamoeba histolytica/dispar and G. lamblia) 236 (6%). While helminthic infections account the least case among individuals who visited emergency unit for immediate medical care with the predominant species of Ascaris lumbricoides (1.9%) (Figure 2).
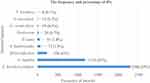 |
Figure 2 The frequency of IPs detected from emergency patients at the WCSH, 2014–2019 (n=11,281). |
The Gender Based Prevalence and Distribution of IPs
The rate of IPIs was significantly higher in females than males (P-value = 0.0277). The overall prevalence of protozoan infections was significantly higher in females (34%) than males (31.7%) (P-value = 0.0101). The rate of E. histolytica/dispar infection in female patients was higher than their counterparts (P-value = 0.0163). However, H. nana (P-value = 0.0138) and E. vermicularis (P-value = 0.0201) infection rates were higher in male patients (Table 2).
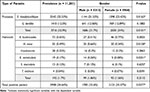 |
Table 2 Gender-Based Distribution and Prevalence of IPs Detected from Emergency Patients at WCSH, 2014–2019 |
The Distribution of IPs in Different Age Groups
The overall IP positivity rate was slightly increased as the age of the patient increased. Furthermore, an increased protozoan infection rate with age was seen. The highest intestinal protozoan infection rate was observed in patients aged 55 years and above, followed by the 45–54 age groups and the 25–34 age groups. However, the highest helminth infection rate was observed in patients aged between 5 and 14 years, followed by the 45–54 age group and the 15–24 age group. The highest prevalence of E. histolytica/dispar, G. lamblia, A. lumbricoides, and H. nana was found in the age group >54 (26.73%), 5–14 (14.55%), 45–54 (1.61%), and 5–14 (1.33%) years, respectively (Table 3).
 |
Table 3 The Distribution of IPs Among Individuals Who Attended the Emergency Department of WCSH, 2014–2019 |
Discussion
Protozoa and helminths are among the etiologies of diarrheal diseases, and infections due to these pathogens are the major public health problems worldwide, especially in the developing world where poverty, lack of drinking water, lack of health education, or lack of sanitation facilities are prevalent.7,8,12 In the present study, we performed a six-year retrospective analysis of IP at the emergency laboratory of WCSH, Woldia, Northwest Ethiopia. The results showed that IPs are one of the major reasons for emergency admission. About 34.6% (95% CI = 33.8–35.5%) of patients admitted to WCSH’s emergency department were infected with at least one IP. This figure indicates that nearly one-third of emergency admissions among emergency admitted patients with gastrointestinal symptoms are due to IPs.
The overall prevalence of IP in the present study is supported by studies conducted in other location of Ethiopia; 34.5% in Addis Ababa13 and 35.5% in Axum.14 However, the overall finding in the current study considerable higher than those previously reported studies in different location of Ethiopia; 6.23% in Bale Robe,15 9.3% in Mojo,16 16.6% in Bale Goba,17 16.65% in Wonago,18 20.6% in Jimma,19 and 27.3% in Debre Tabor.20 Moreover, overall finding of the present study also considerable higher than studies conducted in Ghana (10%),21 Saudi Arabia (0.5%),22 Iran (4.4%),23 Nepal (15.17%),24 India (7.6%).25 On the other hand, it was lower than other reports in Ethiopia; 41.3% in Gondar,26 45.6% in Gondar,27 47.9% in Hawassa,28 53.3% in Dembia,29 and Tanzania 57.1%.30 Differences in IP prevalence rates in various studies could be related to variations in lifestyle of the study populations, the target populations, the availability of quality water supply in the study area, sanitary or hygiene practices, socioeconomic status, the study period, geographic areas, and the methods employed for stool examination could affect the IP prevalence rate.
In the present study, eight different types of IPs were detected among individuals who had a stool sample examination in the emergency laboratory. The protozoan parasites, E. histolytica/dispar and G. lamblia, accounted for 95% of the parasites, and the remaining 5% were helminths. E. histolytica/dispar was the leading parasite, which accounted for about 65%, followed by G. lamblia, which accounted for 30%, and Ascaris lunmbricoides (1.9%). Although a huge variation in numbers was seen, regarding the predominant parasites, similar findings were also reported in other parts of Ethiopia.13,15,17,27 The higher prevalence of intestinal protozoa infections in this and other studies might be due to the presence of inadequate water supply, sanitation activities, food safety, and hygiene behaviors in the population.31–34 Lack of safe drinking water and sanitation facilities such as toilets is highly associated with a high risk of intestinal E. histolytica/dispar35 and G. lamblia36 infections. Furthermore, the very high proportions of intestinal protozoa infections in this study might also be associated with the population that participated in the study; all the data was taken from emergency patients. Protozoan parasites such as E. histolytica can cause severe watery or bloody diarrhea with reduced appetite and weakness and lead to hospital emergency visits.37,38 The lower prevalence of intestinal helminth infections in most of the Ethiopian studies could be due to a deworming program, particularly for soil-transmitted helminths, initiated long ago in Ethiopia.39
The overall prevalence of protozoan infections (32.9%) was higher than helminth infections (1.7%). Similar to the present study, reports from other parts of Ethiopia showed that protozoan infections were more prevalent than helminth infections.15,27,28 The rates of overall IP infection and protozoan infection were significantly higher in females (35.57% and 34%) than in males (33.6% and 31.7%), P-values = 0.0277 and 0.010, respectively. Despite the lack of compelling scientific reasons, this disparity could be explained by the fact that this study was limited to the emergency diagnosis center, as well as the highest burden of E. histolytica, which accounts for the majority of the estimated prevalence of IPIs in the study area. The main reason why we relate this disparity with the highest cases of E. histolytica and the study center is that existing evidence suggests that males are more asymptomatic carriers of E. histolytica than females.40 Because of this, females are more likely than males to visit an emergency treatment center to receive immediate medical care. Surprisingly, this finding is not supported by other previously published research works,16,20,27,29,41 where males were more affected than females. Other few reports also revealed that there was no association between gender and IPIs.42,43
Regarding the distribution of IPs among age groups, it was higher in the age groups of 45–54 years (40%), > 54 years (39.2%), and 25–34 years (37%). However, it was lower in age groups < 5 years (25.6%), 15–24 years (33.6%), and 5–14 years (34.7%). The prevalence of IPIs among <15, 15–35, and > 35 years was 30.6%, 35.3%, and 39.6%, respectively. In the current study, the age-specific prevalence trend of protozoan parasite infections was increased with age. However, a fluctuating age-specific prevalence trend of helminth infections was found. The higher proportion of PIs in the older population may be attributable to a variety of factors, including agricultural practices and, thereby, migration for labor work, which force them to drink contaminated water and may leave them unable to exercise proper personal and environmental hygiene.
In this study, we have seen a fluctuating prevalence rate of IP infection throughout the diagnosis years. The rate of infection ranged from 28.0% in 2017 to 41.3% in 2014. The infection burden decreased slightly over four consecutive years (2014–2017) but began to rise again in the last two years (2018–2019). Similarly, this fluctuating trend prevalence of IPIs was also supported by other previously conducted research works.16,26,27 The activities towards prevention and control of infections, education, as well as the quality of life of the population in different years, related to the socioeconomic status of the population, could explain the likely trend variation.
Limitation
This was a retrospective study that did not identify important factors such as water source, sanitary and hygiene habits, latrine availability, the presence of other comorbidities, and whether the patients had been dewormed. Moreover, only wet mount microscopy was employed for the diagnosis, which could underdiagnose parasitic infections in cases of light parasitic load.
Conclusion and Recommendation
The rate of IPI in the WCSH’s emergency setting is high. Protozoan parasites E. histolytica and G. lamblia were the most common causes of emergency hospital visits, underlining the need for a safe water supply and food preparation to reduce their burden. The high infection rate calls for a joint effort of healthcare workers and managers as well as other stakeholders for the provision of health education, effective health policy implementation, and public mobilization. Further studies which focus on the risk factors of IPIs in the study area while employing more sensitive laboratory methods should be encouraged.
Abbreviations
IP, intestinal parasite; IPI, intestinal parasite infection; NTD, neglected tropical diseases; WCSH, Woldia Comprehensive Specialized Hospital; WHO, World Health Organization.
Data Sharing Statement
All data generated or analyzed during this study were included in this article. Data that support the findings of this study are also available from the corresponding author upon reasonable request.
Ethical Approval and Consent to Participate
Before the commencement of the study, we obtained ethical clearance from Institutional Review Board of Woldia University, and an official letter of cooperations was provided to WCSH. Before data collection, we explained the study objectives to the heads of the hospital and laboratory unit. Since we used secondary data for this study, we didn’t require the patient’s informed consent. We conducted the study following the Declaration of Helsinki.44 To maintain the confidentiality of information from participant’s record, we didn’t record any personal identifiers on the data collection sheet rather we used specific identification code for each recorded participant data, and secured data from participant records were not available to anyone except for the investigators.
Acknowledgments
We thank all the Medical Laboratory staff working at the emergency laboratory of WCSH for their support during the data collection period.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no conflicts of interest in relation to this work.
References
1. Assemie MA, Shitu Getahun D, Hune Y, et al. Prevalence of intestinal parasitic infection and its associated factors among primary school students in Ethiopia: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2021;15(4):e0009379. doi:10.1371/journal.pntd.0009379
2. Harhay MO, Horton J, Olliaro PL. Epidemiology and control of human gastrointestinal parasites in children. Expert Rev Anti Infect Ther. 2010;8(2):219–234. doi:10.1586/eri.09.119
3. Haque R. Human intestinal parasites. J Health Popul Nutr. 2007;25(4):387–391.
4. Sitotaw B, Shiferaw W. Prevalence of intestinal parasitic infections and associated risk factors among the first-cycle primary schoolchildren in Sasiga District, Southwest Ethiopia. J Parasitol Res. 2020;2020:1–13. doi:10.1155/2020/8681247
5. Taghipour A, Ghodsian S, Jabbari M, Olfatifar M, Abdoli A, Ghaffarifar F. Global prevalence of intestinal parasitic infections and associated risk factors in pregnant women: a systematic review and meta-analysis. Trans R Soc Trop Med Hyg. 2021;115(5):457–470. doi:10.1093/trstmh/traa101
6. Feleke DG, Alemu Y, Bisetegn H, Mekonnen M, Yemanebrhane N. Intestinal parasitic infections and associated factors among street dwellers and prison inmates: a systematic review and meta-analysis. PLoS One. 2021;16(8):e0255641. doi:10.1371/journal.pone.0255641
7. Tegen D, Damtie D, Hailegebriel T. Prevalence and associated risk factors of human intestinal protozoan parasitic infections in Ethiopia: a systematic review and meta-analysis. J Parasitol Res. 2020;2020:1–15. doi:10.1155/2020/8884064
8. Wong LW, Ong KS, Khoo JR, Goh CBS, Hor JW, Lee SM. Human intestinal parasitic infection: a narrative review on global prevalence and epidemiological insights on preventive, therapeutic and diagnostic strategies for future perspectives. Expert Rev Gastroenterol Hepatol. 2020;14(11):1093–1105. doi:10.1080/17474124.2020.1806711
9. Yoseph A, Beyene H. The high prevalence of intestinal parasitic infections is associated with stunting among children aged 6–59 months in Boricha Woreda, Southern Ethiopia: a cross-sectional study. BMC Public Health. 2020;20(1):1270. doi:10.1186/s12889-020-09377-y
10. Hajare ST, Gobena RK, Chauhan NM, Eriso F. Prevalence of intestinal parasite infections and their associated factors among food handlers working in selected catering establishments from Bule Hora, Ethiopia. Biomed Res Int. 2021;2021:1–15. doi:10.1155/2021/6669742
11. WHO. Working to overcome the global impact of neglected tropical diseases: first WHO report on neglected tropical diseases. World Health Organization; 2010. Available from: https://apps.who.int/iris/handle/10665/44440.
12. Omarova A, Tussupova K, Berndtsson R, Kalishev M, Sharapatova K. Protozoan parasites in drinking water: a system approach for improved water, sanitation and hygiene in developing countries. Int J Environ Res Public Health. 2018;15(3):495. doi:10.3390/ijerph15030495
13. Tssema A, Yitayew B, Kebede T. Intestinal parasitic infections at Tikur Anbessa University Hospital, Ethiopia: a 5-year retrospective study. Int J Infect Dis Ther. 2017;1(1):22–26.
14. Feleke DG. Prevalence of intestinal parasitic infections in St. Marry Hospital, Axum, Northern Ethiopia: a retrospective study. J Trop Dis. 2017;05(01). doi:10.4172/2329-891X.1000235
15. Chala B, Retrospective A. Analysis of the results of a five-year (2005–2009) parasitological examination for common intestinal parasites from Bale-Robe Health Center, Robe Town, Southeastern Ethiopia. ISRN Parasitol. 2013;2013:1–7. doi:10.5402/2013/694731
16. Chala B. Prevalence of intestinal parasitic infections in Mojo Health Center, Eastern Ethiopia: a 6-year (2005–2010) retrospective study. Epidemiol Open Access. 2013;03(01). doi:10.4172/2161-1165.1000119
17. Abdulkerim A. Prevalence of intestinal parasitic infections among patients with diarrhea at Bereka Medical Center, Southeast Ethiopia: a retrospective study. Fam Med Med Sci Res. 2014;03(03). doi:10.4172/2327-4972.1000131
18. Tefera G. Prevalence of intestinal parasitic infections among patients with diarrhea at Wonago Health Center, Southern Ethiopia: a retrospective study. Immunol Infect Dis. 2015;3(1):1–6.
19. Belete YA, Kassa TY, Baye MF. Prevalence of intestinal parasite infections and associated risk factors among patients of Jimma health center requested for stool examination, Jimma, Ethiopia. PLoS One. 2021;16(2):e0247063. doi:10.1371/journal.pone.0247063
20. Workineh L, Almaw A, Eyayu T. Trend analysis of intestinal parasitic infections at Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia from 2017 to 2021: a five-year retrospective study. Infect Drug Resist. 2022;15:1009–1018. doi:10.2147/IDR.S350456
21. Appiah MA, Adzaklo EE, Agboli E. A retrospective study of intestinal parasite among patients in the Ho Teaching Hospital, Ghana. Int J Trop Dis Heal. 2019;6:1–8.
22. Amer OSO, Al-Malki ES, Waly MI, AlAgeel A, Lubbad MY. Prevalence of intestinal parasitic infections among patients of King Fahd Medical City in Riyadh Region, Saudi Arabia: a 5-year retrospective study. J Parasitol Res. 2018;2018:1–8. doi:10.1155/2018/8076274
23. Teimouri A, Alimi R, Farsi S, Mikaeili F. Intestinal parasitic infections among patients referred to hospitals affiliated to Shiraz University of Medical Sciences, southern Iran: a retrospective study in pre- and post-COVID-19 pandemic. Environ Sci Pollut Res. 2022;29(24):36911–36919. doi:10.1007/s11356-021-18192-w
24. Singh GK, Parajuli KP, Shrestha M, Pandey S, Yadav SC. The prevalence of intestinal parasitic infestation in a tertiary care hospital-a retrospective study. J Nobel Med Coll. 2013;2(1):13–17. doi:10.3126/jonmc.v2i1.7666
25. Mir RF, Peerzada BY, Samad L, Shah A. Prevalence of intestinal parasitic infections in a tertiary care hospital in Kashmir India-five year retrospective study. IP Int J Med Microbiol Trop Dis. 2022;8(1):69–72.
26. Ayelgn M, Worku L, Ferede G, Wondimeneh Y. A 5 year retrospective analysis of common intestinal parasites at Poly Health Center, Gondar, Northwest Ethiopia. BMC Res Notes. 2019;12(1):697. doi:10.1186/s13104-019-4735-9
27. Derso A, Yenealem G, Addisu A. A five-year trend of intestinal parasite prevalence among students attending clinic at University of Gondar, Northwest Ethiopia. J Parasitol Res. 2021;2021:1–5. doi:10.1155/2021/8897935
28. Menjetta T, Simion T, Anjulo W, et al. Prevalence of intestinal parasitic infections in Hawassa University students’ clinic, Southern Ethiopia: a 10-year retrospective study. BMC Res Notes. 2019;12(1):702. doi:10.1186/s13104-019-4747-5
29. Addisu A, Zeleke AJ, Bayih AG, et al. Trends and seasonal patterns in intestinal parasites diagnosed in primary health facilities in Northwest Ethiopia. J Infect Dev Ctries. 2020;14:58S–65S. doi:10.3855/jidc.11729
30. Mazigo HD, Ambrose EE, Zinga M, et al. Prevalence of intestinal parasitic infections among patients attending Bugando Medical Centre in Mwanza, north-western Tanzania: a retrospective study. Tanzan J Health Res. 2010;12(3). doi:10.4314/thrb.v12i3.54205
31. Speich B, Croll D, Fürst T, Utzinger J, Keiser J. Effect of sanitation and water treatment on intestinal protozoa infection: a systematic review and meta-analysis. Lancet Infect Dis. 2016;16(1):87–99. doi:10.1016/S1473-3099(15)00349-7
32. Strunz EC, Addiss DG, Stocks ME, Ogden S, Utzinger J, Freeman MC. Water, sanitation, hygiene, and soil-transmitted helminth infection: a systematic review and meta-analysis. PLoS Med. 2014;11(3):e1001620. doi:10.1371/journal.pmed.1001620
33. Baldursson S, Karanis P. Waterborne transmission of protozoan parasites: review of worldwide outbreaks – an update 2004–2010. Water Res. 2011;45(20):6603–6614. doi:10.1016/j.watres.2011.10.013
34. Li J, Wang Z, Karim MR, Zhang L. Detection of human intestinal protozoan parasites in vegetables and fruits: a review. Parasit Vectors. 2020;13(1):380. doi:10.1186/s13071-020-04255-3
35. Atabati H, Kassiri H, Shamloo E, et al. The association between the lack of safe drinking water and sanitation facilities with intestinal Entamoeba spp infection risk: a systematic review and meta-analysis. PLoS One. 2020;15(11):e0237102. doi:10.1371/journal.pone.0237102
36. Fakhri Y, Daraei H, Ghaffari HR, et al. The risk factors for intestinal Giardia spp infection: global systematic review and meta-analysis and meta-regression. Acta Trop. 2021;220:105968. doi:10.1016/j.actatropica.2021.105968
37. Ünal E, Arslan S, Onur MR, Akpinar E. Parasitic diseases as a cause of acute abdominal pain: imaging findings. Insights Imaging. 2020;11(1):86. doi:10.1186/s13244-020-00892-5
38. Stanley SL. Amoebiasis. Lancet. 2003;361(9362):1025–1034. doi:10.1016/S0140-6736(03)12830-9
39. MoH. Second Edition of Ethiopia National Master Plan for Neglected Tropical Diseases.
40. Acuna-Soto R, Maguire JH, Wirth DF. Gender distribution in asymptomatic and invasive amebiasis. Am J Gastroenterol. 2000;95(5):1277–1283. doi:10.1111/j.1572-0241.2000.01525.x
41. Tigabu A, Taye S, Aynalem M, Adane K. Prevalence and associated factors of intestinal parasitic infections among patients attending Shahura Health Center, Northwest Ethiopia. BMC Res Notes. 2019;12(1):333. doi:10.1186/s13104-019-4377-y
42. Ramos JM, Rodríguez-Valero N, Tisiano G, et al. Different profile of intestinal protozoa and helminthic infections among patients with diarrhoea according to age attending a rural hospital in southern Ethiopia. Trop Biomed. 2014;31(2):392–397.
43. Eyayu T, Kiros T, Workineh L, et al. Prevalence of intestinal parasitic infections and associated factors among patients attending at Sanja Primary Hospital, Northwest Ethiopia: an institutional-based cross-sectional study. PLoS One. 2021;16(2):e0247075. doi:10.1371/journal.pone.0247075
44. World Medical Association. World Medical Association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;79:310.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
