Back to Journals » Journal of Hepatocellular Carcinoma » Volume 6
Intermediate stage hepatocellular carcinoma: a summary review
Authors Elshaarawy O , Gomaa A , Omar H, Rewisha E, Waked I
Received 14 March 2019
Accepted for publication 14 June 2019
Published 11 July 2019 Volume 2019:6 Pages 105—117
DOI https://doi.org/10.2147/JHC.S168682
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmed Kaseb
Omar Elshaarawy, Asmaa Gomaa, Hazem Omar, Eman Rewisha, Imam Waked
Department of Hepatology and Gastroenterology, National Liver Institute, Menoufia University, Shebeen El-Kom, Egypt
Abstract: It is well known that intermediate stage hepatocellular carcinoma (HCC) encompasses the widest class of patients with this disease. The main characteristic of this special sub-group of patients is that it is extensively heterogenous. This substantial heterogeneity is due to the wide range of liver functions of such patients and variable tumor numbers and sizes. Real world clinical data show huge support for transarterial chemo-embolization (TACE) as a therapeutic modality for intermediate stage HCC, applied in 50%–60% of those class of patients. There are special considerations in various international guidelines regarding treatment allocation in intermediate stage HCC. There is an epidemiological difference in HCC in eastern and western cohorts, and various guidelines have been proposed. In patients with HCC, it has frequently been reported that there is poor correlation between the clinical benefit and real gain in patient condition and the conventional way of tumor response assessment after locoregional treatments. This is due to the evaluation criteria in addition to the scoring systems used for treatment allocation in those patients. It became clear that intermediate stage HCC patients receiving TACE need a proper prognostic score that offers valid clinical prediction and supports proper decision-making. Also, it is the proper time to study more treatment options beyond TACE, such as multimodal regimens for this class of patients. In this review, we tried to provide a summary of the challenges and future directions in managing patients with intermediate stage HCC.
Keywords: staging, scores, liver, cancer, TACE, BCLC
Introduction
Hepatocellular carcinoma (HCC)1 is the second leading cause of global cancer-related deaths, especially in patients with liver cirrhosis, and it is the sixth most common malignancy worldwide. Staging of HCC plays a vital role in treatment strategy assignment according to international guidelines.
Intermediate stage or Barcelona Clinic Liver Cancer (BCLC) stage B HCC includes multiple tumorous lesions confined to the liver without vascular invasion in a patient with preserved liver functions and good performance status. The most common treatment modality for patients in this stage is transarterial chemo-embolization (TACE). Due to the heterogeneity in the population with this stage, the benefits and the outcome of TACE are considered variable.2 Patients with good reservoir of liver functions and small size tumor have better prognosis than those with poor liver functions and larger tumor size. The 2-year survival rate may reach 63% in patients with good matching criteria.3
Intermediate stage HCC and TACE
It is well known that intermediate stage HCC encompasses the widest class of patients with this disease. The main characteristic of this special sub-group of patients is that it is extensively heterogenous. This substantial heterogeneity is due to the wide range of liver functions of such patients and variable tumor numbers and sizes.
Although the most commonly used therapeutic approach for such patients is TACE,2 there is a wide gap between guidelines and applied clinical practice, many therapeutic approaches, such as downstaging such patients with percutaneous ablation or radio-embolization followed by radical resection, have been reported.4–6
In general, guidelines have concluded that the limitations of TACE are due to the extensive heterogeneity within the cohorts. The technique has also been found to have varying results as wide differences were noticed regarding range of selectivity of embolization, emulsifying agents, and degree of treatment delivery. These result in the wide range of responses and benefits obtained from TACE. Also, the differences in liver function capacity and tumor burden between subgroups with this intermediate stage resulted in the fact that not all patients were exposed to the same risk. Consequently, the risk benefit ratio in this case is not accurate or easily evidenced from clinical studies.7
Staging systems resemble the corner stone in the process of patient selection and treatment allocation which determine the prognosis. The more efficient the staging or scoring system, the better the outcome. Staging systems such as Okuda, Child-Pugh, TNM, CLIP, and BCLC have been extensively validated in various cohorts. However, they did not properly fit a heterogenous cohort such as intermediate stage HCC patients. It is rare to find a staging system that correlates with prognosis and treatment allocation. Such systems provide more accurate prognosis and survival prediction.8
Here comes the debate, which patient is the best candidate for TACE? This depends on the residual liver functions and proper assessment of the liver capacity. There have been many prognostic scores that tried to offer a proper TACE-specific prognosis, however, they still lacked validity and TACE specificity.7
Real world clinical data show huge support for TACE as a therapeutic modality for intermediate stage HCC applied in 50%–60% of those class of patients.2,9 It needs to be taken into account that most of the contraindications for TACE lie behind the poor liver functions of the patients and background liver disease progression,10 as the tumor size limit is up to 10 cm, which is not frequently a contraindication. A sub-classification of intermediate stage HCC has been proposed by Bolondi et al.11 They sub-classified BCLC stage B into four sub-groups, as shown in Table 1. Later in 2016, Kudo et al proposed another simplified modification named “Kinki criteria”, it sub-classifies BCLC B stage into only three sub-classes according to Child-Pugh score plus Milan and upto-7 criteria, as shown in Table 2.
 |
Table 1 Bolondi’s subclassification for Barcelona Clinic Liver Cancer (BCLC) B |
 |
Table 2 Kinki criteria |
There are special considerations in various international guidelines regarding treatment allocation in intermediate stage HCC. There is an epidemiological difference in HCC in eastern and western cohorts, and various guidelines have been proposed. HCC originates in middle eastern and Asian countries mostly with a background of viral hepatitis, predominantly HBV or HCV infections. Whereas in western countries, it is mostly due to alcoholic liver disease. Also, there is no well established national HCC screening program in many of the middle eastern and Asian countries, except for highly specialized centers. Here comes the impact of etiology on survival and prognosis, as reported by Piscaglia and Ogasawara.7
The primary background of HCC is cirrhosis, however, the etiology of cirrhosis has been found to impact the prognosis of patients with HCC. This was not considered in all guidelines and prognostic scores. HBV as an etiology accounts for 54.4% of all diagnosed HCC cases globally while HCV accounts for 31.1%, however, around 55% of HCV infected patients were reported as alcoholics.12,13 The impact of viral hepatitis on survival was reported by Zhou et al in a meta-analysis that encompassed 4,744 patients where 2,008 were HBV positive and 2,222 were HCV positive, while 514 were HBV and HCV negative. They reported a poor prognosis in patients with viral hepatitis in comparison to patients with negative serology. They also recommended adjuvant antiviral therapy post-HCC treatment to prevent tumor recurrence.14
Waked et al in 2017, reported vascular invasion as another important factor that should be considered in prognostic scoring systems. The authors also validated the parameters of ALBI grade as well as hepatoma arterial-embolization prognostic (HAP) score in 3,030 patients undergoing TACE.15 Noteworthy, predictors of poor prognosis in literature included liver functions, vascular invasion, AFP, and tumor size. However, the current available scoring systems lack vascular invasion as a parameter.
Response evaluation after TACE
Overall survival is the primary target of any cancer research. Nevertheless, evaluating the efficacy of response to treatment is usually assessed by imaging which plays a vital role in this process. It has been challenging to have a well established morphologic response criterion for the target lesion, starting from the WHO criteria in 1997 then the Response Evaluation Criteria in Solid Tumors (RECIST) criteria in 2000. Both have standardized methods to assess radiological tumor response to treatment using a quantitative and defined algorithm. They offered a simple way to assess the anatomic tumor size and changes in the target lesion either through bilinear product approach16 or single linear summation (RECIST).
Although both criteria were originally proposed for the assessment of cytotoxic agents, they do not offer ways to evaluate anti-tumor activity, except through the decrease in primary tumor size. However, RECIST criteria addressed that this changes in tumor size only could be misleading when it is applied to tumorous targeted therapeutics or any other interventional therapy. In patients with HCC, it has been frequently reported that there is poor correlation between the clinical benefit and real gain in patient condition and the conventional way of tumor response assessment after locoregional treatments.
Twenty years ago, a commission for HCC considering the decline in residual activity of the tumor using contrast enhanced computed tomography (CT) scanning or magnetic resonance imaging17 was proposed by European Association for the Study of the Liver (EASL) to find a proper way to assess tumor response. This proposal has been subsequently endorsed by the American Association for the Study of Liver Diseases (AASLD). Even the AASLD practice guidelines stated that the decrease in total viable tumorous tissue should be taken into consideration, not only the overall size of the tumor, which further offered a proper assessment of the tumor response to treatment.
In 2008, modification of the RECIST criteria was proposed which focuses on the residual viable tumor tissue to assess the response to locoregional and anti-angiogenic therapies. There have been growing evidence and reports about the prognostic power of the modified RECIST (mRECIST) for patients with HCC in addition to predicting overall survival. A significant degree of concordance has been reported between mRECIST and EASL criteria that has been used for a longer time. Response to TACE and sorafenib has been extensively studied according to RECIST and has been shown to be a proper predictive tool. Table 3 shows, in detail, how to evaluate response according to mRECIST. According to the previously discussed criteria, assessment of response to treatment is the main pillar to declare either success or failure of the treatment. However, identifying the optimal timing to stop TACE cycles is challenging. Of note, declaring TACE failure has been agreed to be after failure of two successive cycles.2,7,18
 |
Table 3 Illustrating response evaluation according to modified Response Evaluation Criteria in Solid Tumors (mRECIST) |
Recently, Shim et al conducted a retrospective analysis to determine the optimum radiologic response criteria to precisely predict the outcome of 332 patients with intermediate stage HCC after TACE. Of note, they selected patients with intermediate stage HCC which were classified as BCLC stage B according to BCLC system as a control for tumor burden and Child-Pugh grade A to control for liver function. All the included patients were treated similarly with conventional TACE and followed-up with CT scans which were evaluated using WHO, RECIST, EASL, and mRECIST criteria. They reported that patients with a complete response by enhancement-based criteria (EASL or mRECIST) had longer survival than those who had any other type of response. Moreover, a follow-up assessment according to EASL (p<0.001) and mRECIST (p<0.001) criteria was found to be an independent predictor of survival. Of note, these findings could not be achieved for WHO and RECIST criteria which are size-based.19
In addition, Kim et al performed a retrospective analysis which included 314 patients with intermediate stage HCC (BCLC B and Child-Pugh grade A) to assess predictors of treatment outcome. Noteworthy, they standardized the treatment protocol and follow-up regimen using conventional TACE and contrast enhanced imaging. They evaluated the responses only by mRECIST criteria. In multivariate analysis, they reported that both the initial response according to mRECIST criteria (p<0.001; defined as the response at the first follow-up scan) and the best response by mRECIST (p<0.001; defined as response after on-demand retreatment when necessary) were independent predictors of overall survival.20
The current situation regarding TACE-specific scores
Actual survival fit the predicted survival in many studies better when patients received the recommended treatment according to BCLC 0/A compared to other stages such as BCLC B, C or D. This was found to be better after subclassification of BCLC B according to Bolondi or Kinki criteria,11 Kudo, 2016 #321,.22 However, this was still not the optimum prognosis achieved for this intermediate stage. According to the current prognostic scores and the evolution of many TACE-specific scores which are tailored to intermediate stage HCC, there is strong growing evidence that the optimum score should include tumor number, size, vascular invasion, etiology, and TACE response in addition to liver function parameters such as serum albumin and bilirubin. Some of these were already proposed in HAP score and its modification.15,23–26
In general, many recently developed scoring systems such as ALBI, PALBI, ALBI-T, and modified ALBI-T have shown better performance compared to conventional Child-Pugh score and BCLC staging system. Also, indocyanine green retention test has been reported by several studies as a beneficial tool to predict liver failure. However, the performance of most of these scores was not optimum in patients with intermediate stage HCC, especially those undergoing TACE in comparison to other TACE-specific scores such as HAP score and its modified versions.15,26
Recently, Campani et al conducted a comparative study that included 1,058 patients with intermediate stage HCC where they compared TACE-specific scores such as HAP, mHAP II, and mHAP III to other general grading systems such as ALBI and PALBI grades. They concluded that mHAP III was superior to all of these scores including ALBI and PALBI grades. Noteworthy, even HAP and mHAP II were superior to ALBI and PALBI grades. So, the future direction is toward TACE-specific scores which would offer more precise patient selection and improve response to therapy.26
Among the cohort classified as “ideal candidates” for TACE, an expected median survival in the order of 30 months was quoted, but even within this patient group there was a wide variation in survival.27–29 However, in practice, many patients receive TACE outside the guideline criteria. For example, because TACE is apparently “safe” even in the presence of vascular invasion, the latter is not always considered a contraindication.30 In this expanded population, variation in survival may be even greater. This wide variability in survival has led to attempts to define the prognostic features and combine these into scores (or “models”) that can be applied to assess prognosis at a sub-group or individual patient level. One frequently quoted aim is to identify the sub-group that responds poorly to TACE, which may be more appropriately treated with less aggressive therapies.31,32
For years, many scores have been proposed and despite the scientific criticism of the Child-Pugh score, guidelines still adopt it in the assessment of liver functions. It is clear that a variable percentage of patients with HCC do not have cirrhosis, but they have a range of liver pathology varying from mild pathological changes to advanced fibrosis, and the resultant liver dysfunction relies on the state of the non-tumorous liver and extent of the tumor. Child-Pugh score's weak points appear in the subjective assessment of encephalopathy and amount of ascites together with the inclusion of inter-related variables such as ascites and serum albumin level. In addition, the individual parameters are scored based on arbitrarily defined and predetermined cutoff points.33–36
Of note, one of the reasons for the concrete adherence to Child-Pugh score is that it is easily calculated and uses daily routine parameters. Nowadays, smart phones are abundant and hospital information systems can include any complex calculator. This was shown in MELD score which is widely used regardless of having a complex equation. Despite the lack of validation of any of these scores to fit clinical decision-making, there was an agreement on the need for a substitute for the Child-Pugh score to assess liver functions in patients with HCC, in addition to a reliable specific score to predict response to treatment.
Scores for initial TACE
One of the first TACE-specific scores was the HAP score, which is based on baseline pre-TACE serum bilirubin >17 mmol/L, albumin <36 g/dL which are, respectively, the upper and lower limits of the normal range; AFP >400 ng/mL and tumor size >7 cm in order to guide initial TACE treatment. Kadalayil et al proposed this score after reviewing 114 sequential patients with HCC who received TACE/TAE and the minimum follow-up was 6 months. The patients received one point for each, where HAP A stage has 0 points and HAP D stage has >2 points (Table 4). They concluded that HAP stages C and D had bad prognosis and benefited poorly from TACE.37
 |
Table 4 Hepatoma arterial-embolization prognostic (HAP) score |
Of note, Park et al proposed a modification of the previously published HAP score (Table 5) by removing the bilirubin parameter and incorporating portal vein involvement and mRECIST criteria response. Further validation of the score showed no superiority compared to HAP score.38 Nevertheless, Cappelli et al also modified the HAP score by incorporating tumor number, where single tumor receives 0 points while two or more lesions receive 1 point. The proposed model showed a Harrell’s c‐statistic of 0.649 (95% CI: 0.610–0.688), which was more significant than that of the original HAP score (0.589; 95% CI: 0.552–0.626; P=0.001), in addition to better performance in comparison to the modified HAP‐II score (0.611; 95% CI: 0.572–0.650; P=0.005).39
 |
Table 5 Modified hepatoma arterial-embolization prognostic (mHAP) II score |
In addition, Ogasawara et al proposed CHIP score (Table 6) which consists of CP score of the patients together with number of tumors and presence of HCV as an etiology. CHIP score also included presence of hepatitis C viremia as a factor which might be good for patients receiving direct-acting antivirals. However, we come again to the weak points due to the presence of CP score and the predetermined cut-off points.
 |
Table 6 Chiba HCC in intermediate-stage prognostic (CHIP) score |
In late 2017, Op den Winkel et al proposed Munich TACE (Table 7) score which included AFP, serum bilirubin, prothrombin concentration, creatinine, CRP, and tumor extension. The score gives 0–6 points for each element, resulting in three stages. In early 2018, they also did further validation of the proposed score and it showed AUROC of 0.71 which was superior to TACE-tailored CLIP, HAP, JIS, GETCH, BCLC, CP, Okuda, and STATE scores.40,41
 |
Table 7 Munich-transarterial chemo-embolization (TACE) score |
Scores for retreatment with TACE
The first score to highlight the importance of retreatment strategies with TACE was the Assessment for Retreatment with TACE (ART) score, Table 8. It was proposed by Sieghart et al in a cohort of 107 patients with BCLC stage A and B who had received at least two TACE cycles within 90 days. The score included the increase in pre-TACE 2 Child-Pugh score +1 or ≥2 points (+1.5 or +3 points, respectively), AST increase >25% (+4 points) and the absence of radiological tumor response (+1 point). They defined two groups (0–1.5 and >2.5 points) with survival significantly higher in the first group (23.5 vs 6.6 months; P<0.001).32
 |
Table 8 Assessment for Retreatment with TACE (ART) score |
One of the strong points of this score is the consideration of the dynamic change in liver function status and the radiologic response of the tumor. Unfortunately, the liver function assessment was still performed with Child-Pugh score, which raises a lot of concerns, as discussed earlier. One of the pitfalls of the ART score is the presence of significant difference for different TACE techniques (p=0.002).42,43
Indeed, it became clear that intermediate stage HCC patients receiving TACE need a proper prognostic score that offers valid clinical prediction and supports proper decision-making. Hucke et al, proposed the STATE score and START strategy where they made use of the predictive power of ART score for treatment response and supported it with more parameters to identify patients unfit for TACE as a treatment modality from the start. The STATE score included serum albumin level (g/L) as a set of points, which is further subtracted by 12 points each, if the tumor volume is beyond the up-to-7 criteria and/or CRP levels are ≥1 mg/dL.31
The STATE score identified two groups (<18, ≥18 points) with prognosis of 5.3 vs 19.5 months respectively, P<0.001. Maehringer-Kunz et al validated the STATE score and START strategy and they concluded that the STATE score was an unreliable tool to determine the suitability for first TACE, but the START strategy offered a slight increase in the prognostic ability of ART score. However, other studies concluded the limited ability of the single use of either of them.44
In 2015, Adhoute et al proposed ABCR score (Table 9) based on baseline BCLC stage (A =0, B =+2 and C =+3 points) and AFP level (>200 ng/mL =+1 point) in addition to pre-second TACE Child-Pugh score (≥2-point increase =+2 points) and radiologic tumor response (if yes =−3 points). They concluded that patients with ABCR score ≥4 prior to the second TACE will not benefit from the intervention.45 Unfortunately, Kloeckner et al reported the poor prognostic ability of ART and ABCR scores in a validation study which included 176 patients, they also reported that these scores were not sufficient to rely on for valid clinical decision-making regarding stopping TACE sessions.43
 |
Table 9 ABCR score |
Consequently, Pinato et al validated and compared both ART and HAP scores in a cohort of 660 patients. They showed that HAP score had better prognostic power while ART score had better prediction of TACE failure. This conclusion is consistent with the factors on which both scores are based, as ART score considers the radiologic response which is an important indicator of treatment failure with TACE.46,47
Retreatment of refractory cases with TACE
The key point in retreatment of patients with TACE after declaring failure is considering the potential risk and benefits as survival outcomes. This should be guided using prognostic scores, especially those considered for retreatment such as ART or ABCR score. Patients with >2.5 points in ART score were found to have shorter survival and more adverse events after second TACE. Likewise, patients with ABCR score of ≥4 were found to be at higher risk, with no benefit of retreatment. However, the predictive power of those scores has been questioned and it is doubtful whether they led to accurate decision-making in many studies. Noteworthy, in a large validation study of 627 Japanese patients, ART score was also found to be non-predictive of outcomes after the second TACE.42 In another study, ABCR and ART scores were validated and both of them were found to be of no aid in clinical decision-making regarding further TACE sessions. In this context, it has been agreed that this poor performance of ART and ABCR scores is due to the lack of response to TAE as a parameter in both scores.43,48,49
To guide decision-making regarding retreatment, we should take into consideration that TACE also has an impact on liver functions. It has been found that time to decompensation was shorter in those patients who had retreatment with TACE than those who switched to sorafenib.50 Also, it has been reported that overall survival was better in patients who received <2 unsuccessful TACE procedures than those who had three or more successive TACE procedures before sorafenib administration.2 This was also evidenced in another study that showed the association of progressive increase in CP score and retreatment with TACE. With the emergence of regorafenib and the better outcomes achieved, it is a must to reconsider the benefits and risk of retreatment with TACE.51
Treatment modalities beyond conventional TACE for intermediate stage HCC
Drug-eluting bead (DEB)-TACE and transarterial radioembolization (TARE) vs conventional TACE
TACE has been the standard of care for intermediate stage HCC for many years. However, other treatment modalities have been debated for a long time. In Table 10, we summarized different studies which comparted different treatment options in terms of objective response and patient’s survival. Noteworthy, DEBs provided a great option to overcome the drawbacks of conventional TACE and increased the intensity and duration of ischemia in the target lesion in addition to improving drug delivery to the tumor without significant systemic action.52 Despite the previously mentioned positive effects, in a meta-analysis by Facciorusso et al in 2016 which included eight studies and 1,449 patients with intermediate stage HCC, they reported that DEB-TACE showed no superiority over conventional TACE in terms of survival.53 One of the limitations of DEBs is that it needs proper size selection so that small particles can reach the tumor, and it requires a super-selective approach which is not feasible in all centers.52 The only positive result that was noted in several randomized controlled trials in favor of DEB-TACE, was the better safety profile with significant decrease in serious liver-related adverse events and systemic side effects, particularly alopecia, in comparison to conventional TACE.54 Recently, DEBs are beyond loading with conventional anti-neoplastic drugs. Recent studies reported using tyrosine kinase inhibitors, bevacizumab and new compounds such as SW43-DOX.55,56
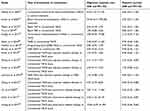 |
Table 10 Summary of different studies comparing different treatment options for patients with intermediate stage hepatocellular carcinoma |
In the meantime, conventional TACE is the standard treatment option for patients with intermediate stage HCC.1 TARE is not included in the BCLC staging system guidelines. On the contrary, TARE is frequently used in western countries and has increasing indications. The ongoing randomized controlled trials are supposed to “build a basis“ of the role of TARE in the management of HCC. Unfortunately, the overall survival is comparable between conventional TACE and TARE.57 However, TARE showed longer time-to-progression, better quality of life, and less hospitalization time in comparison to conventional TACE.58 One of the common complications of TARE is radiation-induced ulcer which is refractory to treatment and radiation-induced cholecystitis and pneumonitis.59
Upward and downward stage migration and multimodal treatment strategies
Surgical treatment for intermediate stage HCC
Indeed, hepatic resection for single tumors >5 cm has been in discussion for many years since the BCLC guidelines. This was supported with data reported from 173 patients with BCLC B stage with resectable HCC outside Milan criteria.60 They reported 51.5% 3-year survival rate vs 18.1% after TACE. Hsu et al reported the better 5-year survival rate in intermediate stage HCC patients undergoing resection vs TACE (43% vs 15%, P<0.001).61 In line with these findings, Liang et al, in 2017, conducted a meta-analysis that included 2,619 Asian patients with intermediate stage HCC from nine studies where they compared TACE to surgical resection. Noteworthy, they concluded that surgical resection showed better overall survival than TACE in Asian patients with intermediate stage HCC. However, no significant difference was noticed in the pooled OR in post-operative complications and 30-day mortality between both groups. Also, they recommended validation of these findings in Western patients.
A lot of strategies have been developed for liver transplantation beyond Milan criteria. This includes several downstaging strategies. These strategies aim to super select patients who could have favorable intermediate stage lesions and are more likely to have better outcome after liver transplantation. Surprisingly, patients with HCC within the University of California San Francisco (UCSF) downstaging criteria have achieved 92.1% 4-year survival post-transplantation.62 Of note, Kamo et al conducted a study on 56 patients with intermediate stage HCC who underwent liver transplantation. They reported 1-, 3-, and 5-year overall survival and recurrence rates of liver transplantation for intermediate stage HCC of 88%/64%/58% and 22%/34%/44%, respectively.63
Locoregional ablative therapies in intermediate stage HCC
Likewise, percutaneous treatments are recommended for patients in early stages. However, clinical practice studies have proposed treatment migration from TACE to ablative percutaneous therapies. D’Avola et al, in a cohort that included 101 treatment-naïve BCLC B patients, 55 received TACE and 35 received curative therapies including radiofrequency ablation (RFA). They reported significantly better survival in patients who received curative therapies including RFA (71 vs 24 months, p<0.001).64 In a very recent meta-analysis by Yang et al, which included eleven studies, they compared the impact of combined TACE and RFA to TACE only regimen in patients with intermediate stage HCC with diameter >5 cm. They reported that the combined therapy group (TACE plus RFA) showed higher 2-year survival rate than TACE only group (RR =1.675, 95%CI: 1.233–2.275, P=0.001). Also, they concluded that combined therapy is beneficial for patients with intermediate stage HCC and tumor size >5 cm diameter. Also, Morimoto et al investigated 37 patients with intermediate HCC and concluded that combined RFA and TACE decreased local tumor progression.65 Of note, Veltri et al followed-up survival in 51 patients who had RFA after TACE, they showed a survival rate of 89.7% at 1-year follow-up.66
It is still problematic to declare curative therapies as an option for intermediate stage HCC, and we are still in need of a fixed algorithm to help proper allocation of therapies such as surgical and percutaneous therapeutic options for this class of patients. The main task right now, for research studies, is to propose strategies that would enable proper patient selection for these radical treatments.2
Systemic therapy in intermediate stage HCC
Noteworthy, multimodal treatments as combining curative measures as resection or RFA with TACE. In addition to adding systemic therapies which seems quite reasonable as TACE causes local hypoxia that upregulates HIF and VEGF. Thus, it is reasonable to add multikinase inhibitors such as sorafenib, that downregulates VEGF, to the regimen.21,67,68 Li et al, in 2018, reported in their meta-analysis that combination therapy was better than TACE alone in terms of time to progression, but not in terms of overall survival as there was no significant difference.69 Also, another randomized controlled trial reported that concurrent sorafenib and TACE did not improve progression-free survival in patients with unresectable HCC in 20 different hospitals in the UK.70 In contrast, a meta-analysis by Li et al, which included 27 studies, concluded that Asian patients with unresectable HCC may benefit from combined TACE and sorafenib therapy in terms of disease control rate and time to progression.69 Also, Pawlik et al reported that the safety of combined DEB-TACE and sorafenib was similar to the safety of sorafenib alone, as most side effects were related to sorafenib dosing.71 We believe that this multimodal strategy still needs more fine-tuning and validation for better treatment outcomes.
Other combined treatment options
Yoon et al investigated the efficacy and safety of TACE plus external beam radiotherapy (RT) vs sorafenib in 90 patients with liver-confined HCC lesions and macroscopic vascular invasion. They showed that the combined TAC and RT group had a significantly higher radiologic response rate than the sorafenib group at 24 weeks (15 [33.3%] vs 1 [2.2%]; P<0.001). Also, they had a significantly longer median time to progression (31.0 vs 11.7 weeks; P<0.001), and significantly longer overall survival (55.0 vs 43.0 weeks; P=0.04). Noteworthy, curative surgical resection was performed in five patients (11.1%) in the TACE-RT group due to tumor downstaging. Notably, no patients in the TACE-RT group stopped treatment due to liver decompensation.
High intensity focused ultrasound (HIFU) was investigated in combination with TACE vs TACE alone in intermediate stage HCC patients. The combined TACE and HIFU group showed better overall survival and tumor-free survival.72
Locoregional treatments such as TACE, TARE, and ablative therapies increase tumor immunogenicity by releasing huge amounts of tumor-associated antigens and induction of inflammation. Indeed, combined immunotherapy (immune check-point inhibitors) and TACE would be a promising combination.73,74 In a recent human study, anti-CTLA-4 antibody tremelimumab in combination with TACE (BCLC B) or thermal ablation (BCLC C) showed better overall survival and promising time-to-progression of the disease.75
Conclusion
To sum-up, intermediate stage HCC still needs precise tailoring of staging systems that would help proper treatment allocation. Studies investigating combined therapies in various sub-groups of this stage are highly recommended. We should consider differences in cohorts and liver disease etiology in different guidelines. Further, an optimum TACE-specific score should include parameters as in mHAP III score in addition to vascular invasion, age, gender, and etiology. Finally, first TACE response according to mRECIST criteria would be a significant addition to a score that would guide either the process of retreatment with TACE or early shift to targeted therapies. The availability of different treatment options requires prospective comparative randomized controlled studies to tailor better treatment algorithms that encompass the new strategies and fit the patient’s stage.
Disclosure
Imam Waked reports personal fees from Gilead, Novartis, Abbvie, Merck Sharp & Dohme, Pharco, Eva Pharma, and Inspire Pharma, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Levi Sandri GB, Ettorre GM, Aldrighetti L, et al. Laparoscopic liver resection of hepatocellular carcinoma located in unfavorable segments: a propensity score-matched analysis from the I Go MILS (Italian group of minimally invasive liver surgery) registry. Surg Endosc. 2019;33(5):1451–1458. doi:10.1007/s00464-018-6426-3
2. Galle PR, Tovoli F, Foerster F, Wörns MA, Cucchetti A, Bolondi L. The treatment of intermediate stage tumours beyond TACE: from surgery to systemic therapy. J Hepatol. 2017;67:173–183. doi:10.1016/j.jhep.2017.03.007
3. Golfieri R, Bargellini I, Spreafico C, et al. Patients with barcelona clinic liver cancer stages B and C hepatocellular carcinoma: time for a subclassification. Liver Cancer. 2019;8:78–91. doi:10.1159/000489791.
4. Guo JG, Zhao LP, Rao YF, et al. Novel multimodal analgesia regimen improves post TACE pain in patients with hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2018. doi:10.1016/j.hbpd.2018.08.001
5. Iezzi R, Cesario V, Siciliani L, et al. Single-step multimodal locoregional treatment for unresectable hepatocellular carcinoma: balloon-occluded percutaneous radiofrequency thermal ablation (BO-RFA) plus transcatheter arterial chemoembolization (TACE). Radiol Med. 2013;118:555–569. doi:10.1007/s11547-012-0914-7
6. Guo W, He X, Li Z, et al. Combination of transarterial chemoembolization (TACE) and radiofrequency ablation (RFA) vs. Surgical Resection (SR) on survival outcome of early hepatocellular carcinoma: a meta-analysis. Hepatogastroenterology. 2015;62:710–714.
7. Piscaglia F, Ogasawara S. Patient selection for transarterial chemoembolization in hepatocellular carcinoma: importance of benefit/risk assessment. Liver Cancer. 2018;7:104–119. doi:10.1159/000485471
8. Pinato DJ, Howell J, Ramaswami R, Sharma R. Review article: delivering precision oncology in intermediate-stage liver cancer. Aliment Pharmacol Ther. 2017;45:1514–1523. doi:10.1111/apt.14066
9. White JA, Gray SH, Li P, et al. Current guidelines for chemoembolization for hepatocellular carcinoma: room for improvement?. Hepatol Commun. 2017;1:338–346.
10. Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353:2254–2261. doi:10.1056/NEJMoa044456
11. Bolondi L, Burroughs A, Dufour JF, et al. Heterogeneity of patients with intermediate (BCLC B) hepatocellular carcinoma: proposal for a subclassification to facilitate treatment decisions. Semin Liver Dis. 2012;32:348–359. doi:10.1055/s-0032-1329906
12. Budny A, Kozlowski P, Kaminska M, et al. [Epidemiology and risk factors of hepatocellular carcinoma]. Pol Merkur Lekarski. 2017;43:133–139.
13. Ghouri YA, Mian I, Rowe JH. Review of hepatocellular carcinoma: epidemiology, etiology, and carcinogenesis. J Carcinog. 2017;16:1. doi:10.4103/jcar.JCar_9_16
14. Zhou Y, Si X, Wu L, Su X, Li B, Zhang Z. Influence of viral hepatitis status on prognosis in patients undergoing hepatic resection for hepatocellular carcinoma: a meta-analysis of observational studies. World J Surg Oncol. 2011;9:108. doi:10.1186/1477-7819-9-108
15. Waked I, Berhane S, Toyoda H, et al. Transarterial chemo-embolisation of hepatocellular carcinoma: impact of liver function and vascular invasion. Br J Cancer. 2017;116:448–454. doi:10.1038/bjc.2016.423
16. WHO. European Status Report on Alcohol and Health 2010. 2010.
17. Ahmad W, Ijaz B, Gull S, et al. A brief review on molecular, genetic and imaging techniques for HCV fibrosis evaluation. Virol J. 2011;8:53. doi:10.1186/1743-422X-8-53
18. Raoul J-L, Gilabert M, Piana G. How to define transarterial chemoembolization failure or refractoriness: a European perspective. Liver Cancer. 2014;3:119–124. doi:10.1159/000343867
19. Shim JH, Lee HC, Kim SO, et al. Which response criteria best help predict survival of patients with hepatocellular carcinoma following chemoembolization? A validation study of old and new models. Radiology. 2012;262:708–718. doi:10.1148/radiol.11110282
20. Kim BK, Kim SU, Kim KA, et al. Complete response at first chemoembolization is still the most robust predictor for favorable outcome in hepatocellular carcinoma. J Hepatol. 2015;62:1304–1310. doi:10.1016/j.jhep.2015.01.022
21. Lencioni R, Llovet JM, Han G, et al. Sorafenib or placebo plus TACE with doxorubicin-eluting beads for intermediate stage HCC: the SPACE trial. J Hepatol. 2016;64:1090–1098. doi:10.1016/j.jhep.2016.01.012
22. Kudo M. Heterogeneity and subclassification of barcelona clinic liver cancer stage B. Liver Cancer. 2016;5:91–96. doi:10.1159/000367768
23. Vincenzi B, Di Maio M, Silletta M, et al. Prognostic relevance of objective response according to EASL criteria and mRECIST criteria in hepatocellular carcinoma patients treated with loco-regional therapies: a literature-based meta-analysis. PLoS One. 2015;10:e0133488. doi:10.1371/journal.pone.0133488
24. Wang W, Bai W, Wang E, et al. mRECIST response combined with sorafenib-related adverse events is superior to either criterion alone in predicting survival in HCC patients treated with TACE plus sorafenib. Int J Cancer. 2017;140:390–399. doi:10.1002/ijc.30451
25. Wang X, Wang Z, Wu L. Combined measurements of tumor number and size helps estimate the outcome of resection of barcelona clinic liver cancer stage B hepatocellular carcinoma. BMC Surg. 2016;16:22. doi:10.1186/s12893-016-0135-4
26. Campani C, Vitale A, Dragoni G, et al. Time-varying mHAP III is the most accurate score in predicting survival in patients with hepatocellular carcinoma (HCC) undergoing trans-arterial chemoembolization (TACE). Digestive Liver Dis. 2019;51:e6. doi:10.1016/j.dld.2018.11.047
27. Burrel M, Reig M, Forner A, et al. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using drug eluting beads. Implications for clinical practice and trial design. J Hepatol. 2012;56:1330–1335. doi:10.1016/j.jhep.2012.01.008
28. Malagari K, Pomoni M, Moschouris H, et al. Chemoembolization with doxorubicin-eluting beads for unresectable hepatocellular carcinoma: five-year survival analysis. Cardiovasc Intervent Radiol. 2012;35:1119–1128. doi:10.1007/s00270-012-0394-0
29. Cabibbo G, Genco C, Di Marco V, et al. Predicting survival in patients with hepatocellular carcinoma treated by transarterial chemoembolisation. Aliment Pharmacol Ther. 2011;34:196–204. doi:10.1111/j.1365-2036.2011.04694.x
30. Chung GE, Lee J-H, Kim HY, et al. Transarterial chemoembolization can be safely performed in patients with hepatocellular carcinoma invading the main portal vein and may improve the overall survival. Radiology. 2011;258:627–634. doi:10.1148/radiol.10101058
31. Hucke F, Pinter M, Graziadei I, et al. How to STATE suitability and START transarterial chemoembolization in patients with intermediate stage hepatocellular carcinoma. J Hepatol. 2014;61:1287–1296. doi:10.1016/j.jhep.2014.07.002
32. Sieghart W, Hucke F, Pinter M, et al. The ART of decision making: retreatment with transarterial chemoembolization in patients with hepatocellular carcinoma. Hepatology. 2013;57:2261–2273. doi:10.1002/hep.26256
33. Cai XR, Chen ZH, Liu MM, et al. Modified CLIP score with the albumin-bilirubin grade retains prognostic value in HBV-related hepatocellular carcinoma patients treated with trans-catheter arterial chemoembolization therapy. J Cancer. 2018;9:2380–2388. doi:10.7150/jca.22925
34. Carling U, Rosok B, Line PD, et al. ALBI and P-ALBI grade in Child-Pugh A patients treated with drug eluting embolic chemoembolization for hepatocellular carcinoma. Acta Radiol. 2018;60(6):702–709.
35. Elshaarawy O, Alkhatib A, Elhelbawy M, et al. Validation of modified albumin-bilirubin-TNM score as a prognostic model to evaluate patients with hepatocellular carcinoma. World J Hepatol. 2019;11(6):542-552.
36. Ho CHM, Chiang CL, Lee FAS, et al. Comparison of platelet-albumin-bilirubin (PALBI), albumin-bilirubin (ALBI), and child-pugh (CP) score for predicting of survival in advanced hcc patients receiving radiotherapy (RT). Oncotarget. 2018;9:28818–28829. doi:10.18632/oncotarget.25522
37. Kadalayil L, Benini R, Pallan L, et al. A simple prognostic scoring system for patients receiving transarterial embolisation for hepatocellular cancer. Ann Oncol. 2013;24:2565–2570. doi:10.1093/annonc/mdt247
38. Park Y, Kim SU, Kim BK, et al. Addition of tumor multiplicity improves the prognostic performance of the hepatoma arterial-embolization prognostic score. Liver Int. 2016;36:100–107. doi:10.1111/liv.12878
39. Cappelli A, Cucchetti A, Cabibbo G, et al. Refining prognosis after trans-arterial chemo-embolization for hepatocellular carcinoma. Liver Int. 2016;36:729–736. doi:10.1111/liv.13029
40. Op Den Winkel M, Nagel D, Op Den Winkel P, et al. The munich-transarterial chemoembolisation score holds superior prognostic capacities compared to TACE-tailored modifications of 9 established staging systems for hepatocellular carcinoma. Digestion;2018. 1–12. 10.1159/000493136
41. Op Den Winkel M, Nagel D, Op Den Winkel P, et al. Transarterial chemoembolization for hepatocellular carcinoma: development and external validation of the munich-TACE score. Eur J Gastroenterol Hepatol. 2018;30:44–53. doi:10.1097/MEG.0000000000001005
42. Arizumi T, Ueshima K, Iwanishi M, et al. Evaluation of ART scores for repeated transarterial chemoembolization in Japanese patients with hepatocellular carcinoma. Oncology. 2015;89(Suppl 2):4–10. doi:10.1159/000440625
43. Kloeckner R, Pitton MB, Dueber C, et al. Validation of clinical scoring systems ART and ABCR after transarterial chemoembolization of hepatocellular carcinoma. J Vasc Interv Radiol. 2017;28:94–102. doi:10.1016/j.jvir.2016.06.012
44. Mahringer-Kunz A, Kloeckner R, Pitton MB, et al. Validation of the risk prediction models STATE-score and START-strategy to guide TACE treatment in patients with hepatocellular carcinoma. Cardiovasc Intervent Radiol. 2017;40:1017–1025. doi:10.1007/s00270-017-1606-4
45. Adhoute X, Penaranda G, Naude S, et al. Retreatment with TACE: the ABCR SCORE, an aid to the decision-making process. J Hepatol. 2015;62:855–862. doi:10.1016/j.jhep.2014.11.014
46. Pinato DJ, Arizumi T, Allara E, et al. Validation of the hepatoma arterial embolization prognostic score in European and Asian populations and proposed modification. Clin Gastroenterol Hepatol. 2015;13:1204–8 e2. doi:10.1016/j.cgh.2014.11.037
47. Pinato DJ, Arizumi T, Jang JW, et al. Combined sequential use of HAP and ART scores to predict survival outcome and treatment failure following chemoembolization in hepatocellular carcinoma: a multi-center comparative study. Oncotarget. 2016;7:44705–44718. doi:10.18632/oncotarget.9604
48. Pipa-Muniz M, Castells L, Pascual S, et al. The ART-SCORE is not an effective tool for optimizing patient selection for DEB-TACE retreatment. A multicentre Spanish study. Gastroenterol Hepatol. 2017;40:515–524. doi:10.1016/j.gastrohep.2017.05.009
49. Terzi E, Terenzi L, Venerandi L, et al. The ART score is not effective to select patients for transarterial chemoembolization retreatment in an Italian series. Dig Dis. 2014;32:711–716. doi:10.1159/000368007
50. Hiraoka A, Kumada T, Kudo M, et al. Hepatic function during repeated TACE procedures and prognosis after introducing sorafenib in patients with unresectable hepatocellular carcinoma: multicenter analysis. Dig Dis. 2017;35:602–610. doi:10.1159/000480256
51. Kohla MAS, Abu Zeid MI, Al-Warraky M, Taha H, Gish RG. Predictors of hepatic decompensation after TACE for hepatocellular carcinoma. BMJ Open Gastroenterol. 2015;2:e000032. doi:10.1136/bmjgast-2015-000032
52. Lencioni R, de Baere T, Burrel M, et al. Transcatheter treatment of hepatocellular carcinoma with doxorubicin-loaded DC bead (DEBDOX): technical recommendations. Cardiovasc Intervent Radiol. 2011;35:980–985. doi:10.1007/s00270-011-0287-7
53. Facciorusso A, Di Maso M, Muscatiello N. Drug-eluting beads versus conventional chemoembolization for the treatment of unresectable hepatocellular carcinoma: A meta-analysis. Digestive Liver Dis. 2016;48:571–577. doi:10.1016/j.dld.2016.02.005
54. Facciorusso A. Drug-eluting beads transarterial chemoembolization for hepatocellular carcinoma: current state of the art. World J Gastroenterol. 2018;24:161–169. doi:10.3748/wjg.v24.i2.161
55. Sakr OS, Berndt S, Carpentier G, Cuendet M, Jordan O, Borchard G. Arming embolic beads with anti-VEGF antibodies and controlling their release using LbL technology. J Control Release. 2016;224:199–207. doi:10.1016/j.jconrel.2016.01.010
56. Lahti S, Ludwig JM, Xing M, et al. In vitro biologic efficacy of sunitinib drug-eluting beads on human colorectal and hepatocellular carcinoma-A pilot study. PLoS One. 2017;12:e0174539. doi:10.1371/journal.pone.0174539
57. Salem R, Lewandowski RJ, Kulik L, et al. Radioembolization results in longer time-to-progression and reduced toxicity compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2011;140:497–507.e2. doi:10.1053/j.gastro.2010.10.049
58. Salem R, Gordon AC, Mouli S, et al. Y90 radioembolization significantly prolongs time to progression compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology. 2016;151:1155–1163.e2. doi:10.1053/j.gastro.2016.08.029
59. Kim H-C. Radioembolization for the treatment of hepatocellular carcinoma. Clin Mol Hepatol. 2017;23:109–114. doi:10.3350/cmh.2017.0004
60. Yin L, Li H, Li A-J, et al. Partial hepatectomy vs. transcatheter arterial chemoembolization for resectable multiple hepatocellular carcinoma beyond milan criteria: A RCT. J Hepatol. 2014;61:82–88. doi:10.1016/j.jhep.2014.03.012
61. Hsu C-Y, Huang Y-H, Hsia C-Y, et al. A new prognostic model for hepatocellular carcinoma based on total tumor volume: the taipei integrated scoring system. J Hepatol. 2010;53:108–117. doi:10.1016/j.jhep.2010.01.038
62. Yao Q, Zhang H, Xiong B, et al. Combination of sorafenib and TACE inhibits portal vein invasion for intermediate stage HCC: a single center retrospective controlled study. Oncotarget. 2017;8:79012–79022. doi:10.18632/oncotarget.20745
63. Kamo N, Kaido T, Yagi S, Okajima H, Uemoto S. Liver transplantation for intermediate-stage hepatocellular carcinoma. Liver Cancer. 2018;7:179–189. doi:10.1159/000487058
64. D’Avola D, Iñarrairaegui M, Pardo F, et al. Prognosis of hepatocellular carcinoma in relation to treatment across BCLC stages. Ann Surg Oncol. 2011;18:1964–1971. doi:10.1245/s10434-011-1551-4
65. Morimoto M, Numata K, Kondou M, Nozaki A, Morita S, Tanaka K. Midterm outcomes in patients with intermediate-sized hepatocellular carcinoma: a randomized controlled trial for determining the efficacy of radiofrequency ablation combined with transcatheter arterial chemoembolization. Cancer. 2010;116:5452–5460. doi:10.1002/cncr.25314
66. Veltri A, Moretto P, Doriguzzi A, Pagano E, Carrara G, Gandini G. Radiofrequency thermal ablation (RFA) after transarterial chemoembolization (TACE) as a combined therapy for unresectable non-early hepatocellular carcinoma (HCC). Eur Radiol. 2006;16:661–669. doi:10.1007/s00330-005-0029-9
67. Cabibbo G, Tremosini S, Galati G, et al. Transarterial chemoembolization and sorafenib in hepatocellular carcinoma. Expert Rev Anticancer Ther. 2014;14:831–845. doi:10.1586/14737140.2014.920694
68. Chao Y, Chung Y-H, Han G, et al. The combination of transcatheter arterial chemoembolization and sorafenib is well tolerated and effective in Asian patients with hepatocellular carcinoma: final results of the START trial. Int J Cancer. 2015;136:1458–1467. doi:10.1002/ijc.29126
69. Li L, Zhao W, Wang M, et al. Transarterial chemoembolization plus sorafenib for the management of unresectable hepatocellular carcinoma: a systematic review and meta-analysis. BMC Gastroenterol. 2018;18:138. doi:10.1186/s12876-018-0863-2
70. Meyer T, Fox R, Ma YT, et al. Sorafenib in combination with transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma (TACE 2): a randomised placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol Hepatol. 2017;2:565–575. doi:10.1016/S2468-1253(17)30156-5
71. Pawlik TM, Reyes DK, Cosgrove D, et al. Phase II trial of sorafenib combined with concurrent transarterial chemoembolization with drug-eluting beads for hepatocellular carcinoma. J Clin Oncol. 2011;29:3960–3967. doi:10.1200/JCO.2011.37.1021
72. Li C, Zhang W, Zhang R, Zhang L, Wu P, Zhang F. Therapeutic effects and prognostic factors in high-intensity focused ultrasound combined with chemoembolisation for larger hepatocellular carcinoma. Eur J Cancer. 2010;46:2513–2521. doi:10.1016/j.ejca.2010.06.015
73. Dendy MS, Ludwig JM, Stein SM, Kim H. Locoregional therapy, immunotherapy and the combination in hepatocellular carcinoma: future directions. Liver Cancer. 2019;1–15. doi:10.1159/000494843
74. Slovak R, Ludwig JM, Gettinger SN, Herbst RS, Kim HS. Immuno-thermal ablations - boosting the anticancer immune response. J Immunother Cancer. 2017;5:78. doi:10.1186/s40425-017-0284-8
75. Duffy AG, Ulahannan SV, Makorova-Rusher O, et al. Tremelimumab in combination with ablation in patients with advanced hepatocellular carcinoma. J Hepatol. 2017;66:545–551. doi:10.1016/j.jhep.2016.10.029
76. Hasdemir DB, Davila LA, Schweitzer N, et al. Evaluation of CT vascularization patterns for survival prognosis in patients with hepatocellular carcinoma treated by conventional TACE. Diagn Interv Radiol. 2017;23:217–222. doi:10.5152/dir.2016.16006
77. Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–96. doi:10.1053/gast.2003.50016
78. Hayes CN, Zhang P, Zhang Y, Chayama K. Molecular mechanisms of hepatocarcinogenesis following sustained virological response in patients with chronic hepatitis C virus infection. Viruses. 2018;10:531. doi:10.3390/v10100531
79. Mabed M, Esmaeel M, El-Khodary T, Awad M, Amer T. A randomized controlled trial of transcatheter arterial chemoembolization with lipiodol, doxorubicin and cisplatin versus intravenous doxorubicin for patients with unresectable hepatocellular carcinoma. Eur J Cancer Care (Engl). 2009;18:492–499. doi:10.1111/j.1365-2354.2008.00984.x
80. Llovet JM, Real MI, Montana X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002;359:1734–1739. doi:10.1016/S0140-6736(02)08649-X
81. Meyer T, Kirkwood A, Roughton M, et al. A randomised phase II/III trial of 3-weekly cisplatin-based sequential transarterial chemoembolisation vs embolisation alone for hepatocellular carcinoma. Br J Cancer. 2013;108:1252–1259. doi:10.1038/bjc.2013.85
82. Yu SC, Hui JW, Hui EP, et al. Unresectable hepatocellular carcinoma: randomized controlled trial of transarterial ethanol ablation versus transcatheter arterial chemoembolization. Radiology. 2014;270:607–620. doi:10.1148/radiol.13130498
83. Kolligs FT, Bilbao JI, Jakobs T, et al. Pilot randomized trial of selective internal radiation therapy vs. chemoembolization in unresectable hepatocellular carcinoma. Liver Int. 2015;35:1715–1721. doi:10.1111/liv.12750
84. Golfieri R, Giampalma E, Renzulli M, et al. Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer. 2014;111:255–264. doi:10.1038/bjc.2014.199
85. Brown KT, Do RK, Gonen M, et al. Randomized Trial of hepatic artery embolization for hepatocellular carcinoma using doxorubicin-eluting microspheres compared with embolization with microspheres alone. J Clin Oncol. 2016;34:2046–2053. doi:10.1200/JCO.2015.64.0821
86. Kudo M, Han G, Finn RS, et al. Brivanib as adjuvant therapy to transarterial chemoembolization in patients with hepatocellular carcinoma: A randomized phase III trial. Hepatology. 2014;60:1697–1707. doi:10.1002/hep.27290
87. Wang H, Liu Y, Wang X, et al. Randomized clinical control study of locoregional therapy combined with arsenic trioxide for the treatment of hepatocellular carcinoma. Cancer. 2015;121:2917–2925. doi:10.1002/cncr.29456
88. Pinter M, Ulbrich G, Sieghart W, et al. Hepatocellular carcinoma: a phase II randomized controlled double-blind trial of transarterial chemoembolization in combination with biweekly intravenous administration of bevacizumab or a placebo. Radiology. 2015;277:903–912. doi:10.1148/radiol.2015142140
89. Lencioni R, Cioni D. RFA plus lyso-thermosensitive liposomal doxorubicin: in search of the optimal approach to cure intermediate-size hepatocellular carcinoma. Hepat Oncol. 2016;3:193–200. doi:10.2217/hep-2016-0005
90. Liu D, Li H, Li P, et al. Evaluation of TACE combined with RFA and PEI in treating advanced hepatic carcinoma. J Interventional Radiol. 2009;18:389–391.
91. Zhao M, Wang JP, Li W, et al. [Comparison of safety and efficacy for transcatheter arterial chemoembolization alone and plus radiofrequency ablation in the treatment of single branch portal vein tumor thrombus of hepatocellular carcinoma and their prognosis factors]. Zhonghua Yi Xue Za Zhi. 2011;91:1167–1172.
92. Huang D, Chen Y, Chen S, et al. TACE plus percutaneous chemotherapy-lipiodol treatment of unresectable pedunculated hepatocellular carcinoma. Medicine (Baltimore). 2017;96:e7650. doi:10.1097/MD.0000000000007650
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
