Back to Journals » International Journal of General Medicine » Volume 15
Interaction Effect Between Hemoglobin and Hypoxemia on COVID-19 Mortality: an observational study from Bogotá, Colombia
Authors Patiño-Aldana AF , Ruíz Sternberg M , Pinzón Rondón M , Molano-Gonzalez N , Rodriguez Lima DR
Received 25 April 2022
Accepted for publication 20 June 2022
Published 2 September 2022 Volume 2022:15 Pages 6965—6976
DOI https://doi.org/10.2147/IJGM.S371067
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Andrés Felipe Patiño-Aldana,1 Ángela María Ruíz Sternberg,1 Ángela María Pinzón Rondón,1 Nicolás Molano-Gonzalez,1 David Rene Rodriguez Lima1,2
1Grupo de Investigación Clínica, Escuela de Medicina y Ciencias de la Salud, Universidad del Rosario, Bogotá, Colombia; 2CIMED, Hospital Universitario Mayor - Méderi, Bogotá, Colombia
Correspondence: Andrés Felipe Patiño-Aldana, Email [email protected]
Purpose: We aimed to assess the effect of hemoglobin (Hb) concentration and oxygenation index on COVID-19 patients’ mortality risk.
Patients and Methods: We retrospectively reviewed sociodemographic and clinical characteristics, laboratory findings, and clinical outcomes from patients admitted to a tertiary care hospital in Bogotá, Colombia, from March to July 2020. We assessed exploratory associations between oxygenation index and Hb concentration at admission and clinical outcomes. We used a generalized additive model (GAM) to evaluate the observed nonlinear relations and the classification and regression trees (CART) algorithm to assess the interaction effects.
Results: We included 550 patients, of which 52% were male. The median age was 57 years old, and the most frequent comorbidity was hypertension (29%). The median value of SpO2/FiO2 was 424, and the median Hb concentration was 15 g/dL. The mortality was 15.1% (83 patients). Age, sex, and SpO2/FiO2, were independently associated with mortality. We described a nonlinear relationship between Hb concentration and neutrophil-to-lymphocyte ratio with mortality and an interaction effect between SpO2/FiO2 and Hb concentration. Patients with a similar oxygenation index had different mortality likelihoods based upon their Hb at admission. CART showed that patients with SpO2/FiO2 < 324, who were less than 81 years with an NLR > 9.9, and Hb > 15 g/dl had the highest mortality risk (91%). Additionally, patients with SpO2/FiO2 > 324 but Hb of < 12 g/dl and a history of hypertension had a higher mortality likelihood (59%). In contrast, patients with SpO2/FiO2 > 324 and Hb of > 12 g/dl had the lowest mortality risk (9%).
Conclusion: We found that a decreased SpO2/FiO2 increased mortality risk. Extreme values of Hb, either low or high, showed an increase in the likelihood of mortality. However, Hb concentration modified the SpO2/FiO2 effect on mortality; the probability of death in patients with low SpO2/FiO2 increased as Hb increased.
Keywords: hypoxia, erythrocytosis, acute respiratory infection, SARS-CoV-2, neutrophil-to-lymphocyte ratio, generalized additive model, classification and regression tree, inflammation, altitude, acute lung injury
Introduction
On December 31, 2019, SARS-CoV-2 emerged in China and rapidly spread worldwide, with more than 293 million infections and 5.4 million deaths.1 In Colombia, which is a developing country, as of January 5th, there have been more than 5.2 million cases, with more than 130,000 deaths in the national territory. In Bogota, the most affected city in the country, there have been more than 1.49 million people infected, and 27,846 people have died.2,3
The clinical spectrum of COVID-19 disease is diverse. The disease can be asymptomatic, can be present with flu-like symptoms that typically resolve in a few days, or can generate severe symptoms that require medical attention and could cause death.4,5
Several studies worldwide have associated factors with mortality in COVID-19 patients. Most studies have been consistent with risk factors for severe disease. Studies in Asia reported age, history of smoking, vital signs at admission, albumin, C-reactive protein, and proinflammatory cytokines as risk factors for disease progression.6,7 Studies in the USA described factors such as oxygenation (SpO2/FiO2) at admission, age, heart failure, sex, nursing home residency, respiratory rate, and body mass index (BMI) as the main predictors associated with COVID-19 critical illness.8,9 Arterial hypertension, bronchopathy, Charlson index > 3 and vitamin D deficiency have also been associated with severe disease.10,11 These factors might be linked to a hyperinflammatory syndrome, which favors an exaggerated immune response and organ failure when facing a viral infection.12,13
Some ecological studies have evaluated COVID-19 mortality in high-altitude places, but the results are contradictory. Some authors reported higher mortality in men younger than 65 years old living in the USA and Mexico at >2000 m elevation than those located <1500 m.14 Other studies developed in an Andean population (Colombia and Perú) showed a negative correlation between high altitude and COVID-19 mortality and lower mortality excess.15–17 People who permanently live in high-altitude places develop adaptative mechanisms against low atmospheric oxygen pressure exposure. In locations such as Bogotá, which has an altitude of more than 2500 meters, there is a decrease in mean SpO2 values among its population.18 People who live in high altitude locations develop ventilatory, cardiovascular, reproductive, and even cognitive changes.19,20
A recent publication of a cohort of more than 5000 patients in Bogotá showed that a SpO2/FiO2 ratio, less than 259, and lactate dehydrogenase (LDH) greater than 617 U/L at admission, were associated with a greater probability of death, similar to reports in cities at sea level.21
As part of the compensatory mechanisms, erythrocyte concentration in the blood increases, caused by a fast reduction in plasma volume. Hypoxia leads to an erythropoietic stimulus by activating hypoxia-inducible factor 1-alpha (HIF1-α), which binds hypoxia-inducible factor 1-beta (HIF1-β). Together, they act as a promoting factor for erythropoietin (EPO), stimulating red blood cell (RBC) production.22 High altitude also leads to hyperventilation driven by an increased tidal volume and respiratory rate. Living in a high-altitude place is related to alveolar and arterial hypoxemia. A person at sea level will have an alveolar oxygen pressure between 90- and 100-mm Hg, a resident at Bogotá, will reach a PaO2 between 60 and 70 mmHg, while someone at 5100 m elevation will have a PaO2 of 43 mmHg.23–25 The adaptative mechanisms allow for the survival of populations conditioned to these harsh environments. However, studies of people living at high altitudes have described increases in the O2 maximum consumption as they descend to sea level, highlighting the physiologically challenging condition imposed by low oxygen pressures for oxygen uptake and utilization.23
Numerous studies have proposed hemoglobin (Hb) as a biomarker of severe COVID-19.26 Anemia is a marker of chronic disease and a risk factor in critically ill patients. Limited oxygen-carrying capacity and delivery might play a crucial role in organ failure development. Thus, increasing the likelihood of severity and mortality.26,27 A recent meta-analysis found a lower mean Hb concentration between moderate and severe cases but did not find significant differences between survivors and nonsurvivors.26
Adaptative mechanisms to high altitude are related to oxygen intake, transport, and the availability for tissues. Patients with acute respiratory infections who live at high altitudes face a convergence between pathological and adaptive processes. Mechanisms that could be interrelated moderating the disease outcome. Our research aimed to assess the effect of Hb and oxygenation index on COVID-19 mortality.
Materials and Methods
Study Population
We performed an observational, retrospective study of the COVID-19 patients admitted between March and July 2020 to the Hospital Universitario Mayor Méderi (HUM) in Bogotá, Colombia. We included patients with confirmed infection of SARS-CoV-2 by RT–PCR or antigen. We excluded patients with a history of COPD, SAHOS, CKD, anemic, lymphoproliferative, or myelodysplastic syndromes. We also excluded patients with information of permanent residency under 2500 meters above sea level (MASL) and without complete blood count (CBC) measurement. The Ethics Committee of the Universidad del Rosario approved the research protocol (#DVO005 1568-CV1411). Qualified professionals carried out all activities and procedures following the principles outlined in the Declaration of Helsinki.
Variables and Main Outcomes
Data were collected from clinical records through a comprehensive review of hospital admission information. A CBC was taken only in patients with hospital admission criteria that required laboratory assessments and who received at least a few hours of in-hospital observation. The CBC was processed in HUM’s clinical laboratory using a Sysmex XN-1000 hematology analyzer. In cases of low-flow systems that could not deliver constant FiO2, we took clinically recorded FiO2. A nasal cannula increased FiO2 by approximately 0.4% per liter/min. A nonrebreather mask with a flow output higher than 10 L/min was taken as 100% FiO2.28 We used admission values as baseline predictors; thus, we did not have any high flow nasal cannula o mechanical non-invasive ventilation registries. We calculated SpO2/FiO2, mean arterial pressure (MAP), and neutrophil to lymphocyte ratio (NLR). We defined the discharge condition (alive or dead) as the primary outcome.
Statistical Analysis
We reported qualitative variables as frequencies and percentages and quantitative variables as the means and standard deviations or medians and interquartile ranges, depending on the normality of the distribution (tested by Shapiro–Wilk test). To assess possible associations with mortality, we performed an exploratory analysis using the independent samples t-test on continuous variables with a normal distribution, the Mann–Whitney test for continuous variables without a normal distribution, and the chi-square test for the qualitative variables. We made a purposeful selection of clinically and statistically significant covariates for the multivariate model, as described by Hosmer, Lemeshow, and Sturdivant.29 Variables were considered for multivariate analysis based on Hosmer-Lemeshow criteria (p < 0.2). We built a generalized additive model (GAM) to appraise nonlinear relations found, estimating linear and nonlinear effects. Instead of a single regression coefficient, GAM estimates a k number of base functions, which in sum describes the functional form of the relationship between dependent and independent variables.30 We tested for interaction effects using tensor products in the GAM model. Notably, the tensor smoothing function (Te) calculates different k base functions for each variable included in the interaction effect, and it is helpful for variables with different scales.29,30
In a second approach, we used the classification and regression tree (CART) algorithm to find the most relevant variables associated with the clinical outcome. As a strength, the tree-based method explained how the effect of an explanatory variable depended on the level of another variable. Thus it modeled interactions between variables in a nonlinear manner.31 We set the overall significance level at 5%. The sampling method was not probabilistic and consecutive. We defined the sample size by convenience. Thus, the analyses were exploratory. We used R version 4.0.2 software for statistical analyses.
Results
From March to July 2020, 1000 patients were diagnosed with SARS-CoV-2 infection at HUM, and 650 met the inclusion criteria with in-hospital admittance and CBC measurement. We excluded fifty-eight patients with a history of COPD, twenty-seven patients with CKD, six patients with SAHOS; four had a history of anemia, two hematologic malignancies, two patients with pancytopenia of unknown cause, and one permanent residency at low altitude (< 2500 MASL), yielding 550 patients included in this study. (Supplementary Figure 1)
The median (IQR) age was 57 years old (43–70), and 53% of patients were male. The more frequent comorbidities were hypertension (29%), diabetes (16%), cardiovascular disease (3.6%), and atrial fibrillation (2.2%). The median MAP and SpO2/FiO2 were 92 mmHg (84–102) and 424 (381–438). Regarding the CBC on admission, the median white blood cell count (WBC) was 7.0 (5.3–9.6) x 103 cells/µL, and the median concentration of Hb was 15 g/dL (13.7–16.0). Among the total sample, 83 patients (15.1%) died, and 467 (84.9%) survived.
Table 1 shows the demographic characteristics and comorbidities history by discharge condition with an exploratory hypothesis test result. We found a statistically significant difference in the proportion of males between survivors and nonsurvivors. Additionally, there was a statistically significant difference in age and the number of patients with a history of hypertension. Table 2 shows the vital signs and complete blood count by discharge condition. Concerning vital signs, we found statistically significant differences in the median respiratory rate, FiO2, SpO2, and SpO2/FiO2. Regarding CBC, there were differences between survivors and non-survivors in median WBC, absolute lymphocyte count (ALC), absolute neutrophil count (ANC), neutrophil, lymphocyte, and monocyte percentage, and NLR.
 |
Table 1 Demographic Characteristics, Comorbidity History by Discharge Condition in COVID-19 Patients |
 |
Table 2 Vital Signs and Complete Blood Count by Discharge Condition in COVID-19 Patients |
We carried out a purposeful selection of covariates for modeling based on statistically significant differences found.29 We found that age, sex, SpO2/FiO2, Hb, and NLR were independently associated with in-hospital mortality. The relationship between age and SpO2/FiO2 with mortality was linear. However, the association between Hb and NLR with mortality was nonlinear. Thus, we performed a GAM that included linear and smoothened terms. Moreover, we found a significant interaction term between SpO2/FiO2 and hemoglobin. Table 3 shows the effects of the linear and smoothed terms in GAM.
 |
Table 3 Linear and Smoothed Terms of the Generalized Additive Model |
Smoothed variables and interaction effects from the GAM model can be better understood visually. Figure 1 presents the functional form of the smoothed variable’s influence on mortality. Death probability had a positive correlation with NLR. Hemoglobin at admission had a U-shaped correlation with mortality. Patients with low or high hemoglobin concentrations were more prone to die during hospitalization. However, the significant interaction term showed us that the Hb and SpO2/FiO2 effects on mortality were modified by each other.
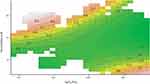
The contour plot in Figure 2 shows how Hb modifies the SpO2/FiO2 effect on mortality. Notice how patients with similar SpO2/FiO2 at admittance had a different likelihood of death according to their Hb value at admission. For instance, with SpO2/FiO2 values above 300, death probability remained constant (10%) with Hb > 10 g/dl but raised to 70% for anemic patients even with normal SpO2/FiO2 at admission. In contrast, notice how hypoxemia is worse with higher Hb values. Patients with SpO2/FiO2 of 300 and Hb of approximately 15 g/dL had a 20% likelihood of death. This probability increased proportionally as the Hb concentration rose. It increased to 70% of death likelihood for patients with SpO2/FiO2 of approximately 300 and Hb >20 g/dL and 90% for patients with SpO2/FiO2 <150 and a Hb of about 18 g/dL. We further explored this interaction effect with a second approach, explained below.
Figure 3 shows a CART model, which classified patients according to their likelihood of death using SpO2/FiO2, Hb, age, history of hypertension, and NLR as interacting variables. We found four clinical profiles with a higher probability of death. Patients older than 81 years old with SpO2/FiO2 < 324 had a death likelihood of 83%. Additionally, patients with SpO2/FiO2 < 324 with less than 81 years old but with an NLR > 9.9 had a death likelihood of 60%. Noteworthy, this probability increased to 91% with a Hb> 15 g/dl and lowered to 22% with a Hb < 15 g/dl. Besides, patients with SpO2/FiO2 ≥ 324 but anemic (Hb < 12 g/dl) and a history of hypertension had a death likelihood of 59%. In comparison, patients with the lowest probability of death (9%) were those who did have a SpO2/FiO2 >324 and a Hb >12 g/dL at admission. Interestingly, the CART method also showed that the hemoglobin concentration at admittance modified the SpO2/FiO2 effect on the probability of death.
Discussion
This original research described the nonlinear relations and, to our knowledge, an unrecognized interaction effect between Spo2/FiO2 and Hb on the mortality of patients with SARS-CoV-2 acute respiratory infection. Using novel multivariate statistical methods to assess nonlinear relations, we found that Spo2/FiO2, Hb, NLR, age, and male sex were independently associated with the probability of death. The Hb and NLR values had a nonlinear relationship with the outcome in GAM. Interestingly, low or high Hb concentrations showed a sharp quadratic increase in the likelihood of death (Figure 1). We found a significant interaction between SpO2/FiO2 and Hb effects on mortality (Figure 2). Atak Tel et al described an association between low Hb levels and the possibility of reconsultation in outpatients with COVID-19,32 however, the relationship of Hb with oxygenation has not been described. We explored this further using CART, which showed that patients older than 81 years and those less than 81 years old but with an NLR > 9.9 and Hb > 15 g/dl had the highest probability of death (83% and 91%, respectively). Interestingly, the likelihood of death descended to 22% for patients less than 81 years old, NLR > 9.9 but with Hb < 15 g/dl. Additionally, normoxic (SpO2/FiO2 >324) but anemic patients (<12 g/dl) with hypertension had a higher probability of death (59%). Normoxic nonanemic patients (>12 g/dl) had, as expected, the lowest likelihood of death (9%).
The proportion of death among hospitalized patients was 15.1%, and the cumulative death incidence between March and July was 74.5 per 500 patients admitted to HUM. The Centers for Disease Control and Prevention (CDC) reported in-hospital mortality ranging from 8.6% to 23.4% in approximately the same period.33 Regarding the oxygenation index, we found a significant difference in the median SpO2/FiO2 between survivors and nonsurvivors. Some authors have proposed the SpO2/FiO2 ratio as a continuous noninvasive monitoring tool for assessing oxygenation in acute respiratory failure or its use as a surrogate for estimating PaO2/FiO2 in sepsis.34,35 The SpO2/FiO2 ratio showed good performance with an AUC =0.801 (95% CI 0.746–0.855) for early mechanical ventilation requirements in patients with COVID-19, even with better performance than the ROX index. Its sequential assessment showed a sharp decline in nonsurvivors compared to an increasing shift in survivors.36 Catoire et al described an excellent performance AUC of 0.91 (95% CI 0.885–0.950) of SpO2/FiO2 to estimate PaO2/FiO2 values in COVID-19 patients.37
We found a significant association between SpO2/FiO2 and mortality. The CART model established a cut point of 324 to define higher-risk groups. Type I respiratory failure in acute respiratory distress syndrome (ARDS) is stratified by PaO2/FiO2 evaluation, although some authors have proposed a modified definition for scarce resource settings using SpO2/FiO2 assessment.38 Berlin’s definition has allowed stratifying patients based on oxygenation compromise. There is a correlation between disease severity measured by PaO2/FiO2 and mortality risk. However, it has a limited prognostic performance with an AUC of 0.57 (95% CI 0.561–0.593).39
For instance, patients with severe ARDS (PaO2/FiO2 values <100) have a differential prognosis according to distensibility and expiratory volume. Higher expiratory volume and lower distensibility distinguish a higher mortality risk group, even with similar PaO2/FiO2.39 Nevertheless, these measures require advanced monitoring, which is not frequently available in scarce resource settings. Numerous studies have explored other biomarkers to enhance prognostication in patients with ARDS.
Red bloodline characteristics have raised concern in the physiopathology of COVID-19 and ARDS. In our study, either high or low Hb values were associated with a higher likelihood of death in GAM, giving a nonlinear, U-shaped correlation between hemoglobin concentration and the probability of dying (Figure 1C). However, the oxygenation index measured by the SpO2/FiO2 ratio modified this effect. Patients with similar SpO2/FiO2 had different mortality probabilities according to Hb concentration (Figure 2).
Taneri et al conducted a meta-analysis including 139 observational studies. They reported a weighted mean difference (WMD) of −4.08 g/L (CI −5.12; −305) between moderate and severe cases in patients with COVID-19. However, among 27 studies, there were no significant differences in the pooled mean Hb concentrations between survivors and nonsurvivors, with a WMD of −0.26 g/L (95% CI −2.37; 1.85).26 In an in-silico analysis, Liu et al proposed a direct effect of SARS-CoV-2 proteins ORF1ab, ORF10, and ORF3a in the Hb beta chain competing against iron. This would lead to a functional loss of hemoglobin and hemolysis. However, given that these hypotheses proposed a non-described protein-protein hemoglobin degradation pathway, some authors criticized it for its flawed methods and unreliability.40,41 In the same way, De Martino et al did not find differences in the hemoglobin dissociation curves or hemolytic biomarkers between patients with COVID-19-related ARDS and patients with ARDS from other causes.42
Histopathological descriptions of the lung tissue of patients with ARDS describe the presence of RBCs. However, they are considered a marker for the increased permeability of the endothelial-alveolar barrier. Nevertheless, recently, the role of RBCs and cell-free Hb has been discussed as a central phenomenon in the progression of acute respiratory infection to sepsis, critical illness, and ARDS pathogenesis. The proinflammatory state steers lipid peroxidation, pump damage, changes in calcium influx, and 2,3-DPG concentrations. This leads to RBC membrane changes, facilitating their aggregation, inducing thrombotic events, and hemolysis with cell-free hemoglobin and iron unstable (Fe 4+) group liberation. These perpetuate an injury cycle with nitric oxide consumption, vasoconstriction, inflammation, and increased endothelial permeability.43 Oxidative and inflammatory damage, and thrombosis with cell aggregation in capillary beds, might explain the harmful effect of polycythemia that we observed in our sample.
Furthermore, other RBC biomarkers are related to ARDS prognosis. Some authors have studied red blood cell distribution width (RDW) and circulating nucleated red blood cells (NRBCs) as prognostic markers. An RDW >14.5 was independently associated with mortality at 30 and 90 days (OR 1.91, CI 95% 1.08–3.39 and 2.56, CI 95% 1.50–4.37, respectively).44,45 The NRBCs are biomarkers of increased erythropoietic activity. They are related to hypoxemia and inflammation. A study reported a significant difference in the proportion of deaths (50.8% versus 27.3% [p <0.001]) between patients with and without NRBCs. Additionally, patients with severe cases had more NRBCs, which were detectable for a longer time. Additionally, there was a negative correlation between the NRBC absolute count and survival time.46
Otherwise, we found that a higher NLR was related to worse outcomes. Previous studies have consistently proposed this relation as a biomarker of severe disease.47–49 It is used in validated evaluation scales such as COVID-GRAM for predicting critical illness risk.47 Kilercik et al evaluated the performance of CBC measures for predicting the risk of COVID-19 severity and mortality. They reported that an NLR >5.23 had a sensitivity and specificity for mortality of 85.6% and 56.8%, respectively. Khalid et al reported that, with a cutoff point of 2.98 in NLR, the AUC for prediction of severe disease is 0.83.50 Additionally, with a cutoff point of 4.4, NLR had a sensitivity of 78.5% and specificity of 68.2% for predicting severe disease.51
A lower ALC is related to the risk of COVID-19 progression, as previously reported.49,50 The CALL score uses the ALC as a variable for predicting pneumonia progression.52 Patients with COVID-19 who developed ARDS demonstrated sustained CD4+ and CD8+ lymphopenia compared to patients without COVID-19-related ARDS.53 Additionally, the absolute counts of B, T, and natural killer (NK) cells were significantly lower in patients with severe COVID-19 cases than in nonsevere COVID-19 cases.12 Immune activation by long-term antigen exposure throughout life is related to sterile and chronic low-grade inflammation associated with chronic diseases, cardiovascular risk, obesity, and cancer.54 This process leads to a senescent adaptive immune system with a predominance of an innate response, which could generate an exaggerated inflammatory response leading to sepsis. The NLR could be a biomarker of this predominance.53,54
We also found that male patients were more likely to die in the hospital than females. Analysis of other coronaviruses, such as SARS and MERS, also showed an excess of mortality in male patients.55,56 Interestingly, the erythroid response to chronic high-altitude hypoxia might be influenced by sex hormones. Chronic mountain sickness (CMS) is rare in Andean females of reproductive age, but its incidence presents a sharp increase with menopause. Additionally, CMS is more frequent in Andean male patients than female patients. Estrogens might confer protection against excessive erythrocytosis in CMS or Monge’s disease. At physiologic concentrations in vitro, estrogens were related to lower RBC counts than testosterone. Estrogens regulate EPO, HIF1A, GATA1, VEGF, genes related to erythropoiesis, and erythroid apoptosis mechanisms.57 These findings suggest that sex hormones moderate the erythropoietic response of chronic exposure to hypoxia and may contribute to the mortality excess in male patients with COVID-19.
This study has some limitations. First, we only considered admission values as baseline predictors of mortality. Patients with COVID-19 might have different behaviors with several intervention requirements and therapies that we did not observe, which could modify the prognosis. We did not consider certain variables such as folate, iron, transferrin, and vitamin B 12 to identify the anemia causes, nor some variables related to the Hb dissociation curve as PCO2 or acid-base status, which might be associated with residual confusion bias. However, our findings propose a u-shaped relation with a high likelihood of death for patients with polycythemia. It supports a previously proposed association between anemia and severe COVID-19 or mortality, indistinctly the cause.26 Moreover, we observed that Hb modified the effect of hypoxemia.
Furthermore, we did not consider the pharmacological history that could affect the baseline CBC. Patients with COPD and CKD were excluded, which may underestimate mortality, since this group of patients is at high risk for severe COVID-19 and death. Lastly, given the retrospective nature of our study, and since the data were gathered from clinical records, we could not guarantee a uniform measurement for each variable. It is necessary to note that no effect can be associated with high-altitude exposure, given the absence of a comparative group. The variables studied might also be modified in chronic conditions. However, we controlled several variables, such as COPD, SAHOS, and CKD, which might affect the Hb concentration. Additionally, tobacco use might also be related to Hb changes; however, it lacked significance in our model. This study allowed us to hypothesize that the adaptative mechanism for chronic hypoxia modifies the pathological process in respiratory diseases. Further studies are required to understand this biological interaction.
This study is useful in daily clinical practice because it allows us to identify patients at risk of developing severe COVID-19 with parameters easily available in emergency services and primary care (SpO2/FiO2 ratio and complete blood count). It also highlights the importance of the interaction of Hb and SpO2/FiO2 ratio, in the prognosis of patients with COVID-19 at high altitude, whether this interaction is significant in other pathologies and cities at sea level remains to be determined.
Conclusion
This study explored the role of the oxygenation index and CBC biomarkers taken at admission as predictors of in-hospital mortality. We found in GAM that Hb and NLR were independently associated with mortality following nonlinear trends. Both low and high Hb concentrations showed a higher likelihood of death. Decreases in SpO2/FiO2 were associated with an increase in the probability of death. However, we found that the effects of Hb and SpO2/FiO2 on mortality were modified by each other. For instance, patients with similar oxygen index values had different death probabilities based on their Hb at admission. The likelihood of death of patients with a low SpO2/FiO2 increased proportionally as Hb increased. The CART model showed that patients with a SpO2/FiO2 >324 and a Hb >12 g/dl had the lowest mortality risk (9%). In contrast, normoxic but anemic patients with Hb <12 g/dl and a history of hypertension had a higher probability of death (59%). Patients whose SpO2/FiO2 was lower than 324 and were older than 81 years had a death likelihood of 83%. Finally, patients with less than 81 years old but NLR > 9.9 and Hb > 15 had the highest probability of death (91%), but this probability hugely decreased to 22% with a Hb < 15 g/dl.
Abbreviations
AIC, Akaike information criteria; ALC, Absolute lymphocyte count; ANC, Absolute neutrophil count; ARDS, Acute respiratory distress syndrome; BMI, Body mass index; CART, Classification and regression tree; CBC, Complete blood count; CKD, Chronic kidney disease; CMS, Chronic mountain sickness; COPD, Chronic obstructive pulmonary disease; OSA, Obstructive sleep apnea; EPO, Erythropoietin; FiO2, Fraction inspired O2; GAM, Generalized additive model; Hb, Hemoglobin concentration (g/dL); HIF-1a, Hypoxia-inducible factor 1-α; HIV, Human immunodeficiency virus; HUM, Hospital Universitario Mayor; MAP, Mean arterial pressure; MASL, Meters above sea level; NK, Natural killer cells; NLR, Neutrophil to lymphocyte ratio; NRBCs, Nucleated red blood cells circulating; PCO2, Partial CO2 pressure; RBC, Red blood cells count; RDW, Red blood cell distribution width; SpO2, Peripheral O2 saturation; VEGF, Vascular-endothelial growth factor; WBC, White blood cell count; WMD, Weighted mean difference.
Acknowledgments
We thank Estefania Rodríguez Alvarino, Isabella Sanclemente Mariño, Mateo Díaz Quiroz and María José Niño for supporting the literature review, and Elizabeth Cruz Tapias for her work in image editing.
Disclosure
The authors declare that they have no competing interests.
References
1. WHO coronavirus (COVID-19) dashboard | WHO Coronavirus (COVID-19) dashboard with vaccination data. Available from: https://covid19.who.int/.
2. Colombia: WHO coronavirus disease (COVID-19) dashboard with vaccination data | WHO Coronavirus (COVID-19) dashboard with vaccination data. Available from: https://covid19.who.int/region/amro/country/co.
3. Instituto Nacional de Salud. Coronavirus Colombia; 2020. Available from: https://www.ins.gov.co/Noticias/Paginas/Coronavirus.aspx.
4. Aktas G. A comprehensive review on rational and effective treatment strategies against an invisible enemy; SARS Cov-2 infection. Exper Biomed Res. 2020;3(4):293–311. doi:10.30714/j-ebr.2020463629
5. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239. doi:10.1001/jama.2020.2648
6. Liu W, Tao ZW, Wang L, et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med J. 2020;133(9):1032–1038. doi:10.1097/CM9.0000000000000775
7. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
8. Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966.
9. Garibaldi BT, Fiksel J, Muschelli J, et al. Patient trajectories among persons hospitalized for COVID-19: a cohort study. Ann Intern Med. 2021;174(1):33–41. doi:10.7326/M20-3905
10. Sardiña-González C, López-Reboiro ML, Suárez-Fuentetaja R, et al. COVID 19 comprehensive management in a regional hospital of Northwestern Spain. GMM. 2020;156(4):4839. doi:10.24875/GMM.M20000398
11. López-Castro J. Coronavirus disease-19 pandemic and vitamin D: so Much for so little? Rev Investig Clin. 2021;73(6):6894. doi:10.24875/RIC.21000305
12. Tian D-S, Zhou L, Hu Z, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. 2020;71(15):762–768. doi:10.1093/cid/ciaa248
13. Yin Tan L, Vaani Komarasamy T, Rmt Balasubramaniam V. Hyperinflammatory immune response and COVID-19: a double edged sword. Front Immunol. 2021;3981. doi:10.3389/fimmu.2021.742941
14. Woolcott OO, Bergman RN. Mortality attributed to COVID-19 in high-altitude populations. High Alt Med Biol. 2020;21(4):409–416. doi:10.1089/ham.2020.0098
15. Cano-Pérez E, Torres-Pacheco J, Fragozo-Ramos MC, et al. Negative correlation between altitude and COVID-19 pandemic in Colombia: a preliminary report. Am J Trop Med Hyg. 2020;103(6):2347–2349. doi:10.4269/ajtmh.20-1027
16. Intimayta-Escalante C, Rojas-Bolivar D, Hancco I. Letter to the Editor: influence of Altitude on the prevalence and case fatality rate of COVID-19 in Peru. High Alt Med Biol. 2020;21:426–427. doi:10.1089/ham.2020.0133
17. Ortiz-Prado E, Fernandez Naranjo RP, Vasconez E, et al. Analysis of excess mortality data at different altitudes during the COVID-19 outbreak in Ecuador. High Alt Med Biol. 2021;22(4):406–416. doi:10.1089/ham.2021.0070
18. Trompetero González AC, Cristancho Mejía E, Benavides Pinzón WF, et al. Comportamiento de la concentración de hemoglobina, el hematocrito y la saturación de oxígeno en una población universitaria en Colombia a diferentes Alturas. Nutricion Hospitalaria. 2015;32(5):2309–2318. doi:10.3305/nh.2015.32.5.9711
19. Julian CG. High altitude during pregnancy. Clin Chest Med. 2011;32(1):21–31. doi:10.1016/j.ccm.2010.10.008
20. Pun M, Lima ÉDA, Carvalho DCM, et al. Effects on cognitive functioning of acute, subacute and repeated exposures to high altitude. Front Physiol. 2018;9:1–15. doi:10.3389/fphys.2018.00001
21. Rodriguez Lima DR, Pinzón Rondón ÁM, Rubio Ramos C, et al. Clinical characteristics and mortality associated with COVID-19 at high altitude: a cohort of 5161 patients in Bogotá, Colombia. Int J Emerg Med. 2022;15(1):22. doi:10.1186/s12245-022-00426-4
22. Windsor JS, Rodway GW. Heights and haematology: the story of haemoglobin at altitude. Postgrad Med J. 2007;83(977):148–151. doi:10.1136/pgmj.2006.049734
23. West JB. Are permanent residents of high altitude fully adapted to their hypoxic environment? High Alt Med Biol. 2017;18(2):135–139. doi:10.1089/ham.2016.0152
24. Acevedo LE, Solarte I. Gasimetria arterial en adultos jóvenes a nivel de Bogotá. Arterial blood gas in young adults in Bogotá. Acta Méd Colomb. 1984;9:7–14.
25. Johanna TR, Hurtado C, Salazar T, De La Peña M. Valores Normales de Gases Arteriales en Bogotá. Normal Values of Arterial Blood Gases in Bogotá. Umbral Científico. 2007;3:94–102.
26. Taneri PE, Gómez-Ochoa SA, Llanaj E, et al. Anemia and iron metabolism in COVID-19: a systematic review and meta-analysis. Eur J Epidemiol. 2020;35(8):763–773. doi:10.1007/s10654-020-00678-5
27. Hayden SJ, Albert TJ, Watkins TR, Swenson ER. Anemia in critical illness: insights into etiology, consequences, and management. Am J Respir Crit Care Med. 2012;185(10):1049. doi:10.1164/rccm.201110-1915CI
28. Fuentes S, Chowdhury YS. Fraction of Inspired Oxygen. StatPearls; 2021.
29. Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. Biometrics. Wiley; Vol. 47, 1991.
30. Wood SN. Generalized Additive Models. Statistical Science. Vol. 1. CRC Press; 1986.
31. Breiman. L, Friedman. J, Olshen RA, Charles J. Classification and Regressión Trees. Vol. 1. Chapman & Hall; 1984.
32. Atak Tel B, Kahveci G, Bilgin S, et al. Haemoglobin and red cell distribution width levels in internal medicine patients indicate recurrent hospital admission during COVID-19. fmpcr. 2022;24(1):32–36. doi:10.5114/fmpcr.2022.113011
33. COVID-19 Hospital Data - In-hospital mortality among confirmed COVID-19 encounters by week. Available from: https://www.cdc.gov/nchs/covid19/nhcs/hospital-mortality-by-week.htm.
34. Rice TW, Wheeler AP, Bernard GR, et al. Comparison of the SpO2/FIO2 ratio and the PaO 2/FIO2 ratio in patients with acute lung injury or ARDS. Chest. 2007;132(2):410–417. doi:10.1378/chest.07-0617
35. Pandharipande PP, Shintani AK., Hagerman HE, et al. Derivation and validation of SpO2 /FiO2 ratio to impute for PaO2/FiO2 ratio in the respiratory component of the Sequential Organ Failure Assessment (SOFA) Score. Crit Care Med. 2009;23:1–7.
36. Lu X, Jiang L, Chen T, et al. Continuously available ratio of SpO2/FiO2serves as a noninvasive prognostic marker for intensive care patients with COVID-19. Respir Res. 2020;21(1):1–4. doi:10.1186/s12931-020-01455-4
37. Catoire P, Tellier E, de la Rivière C, et al. Assessment of the SpO2/FiO2 ratio as a tool for hypoxemia screening in the emergency department. Am J Emerg Med. 2021;44:116-120. doi:10.1016/j.ajem.2021.01.092
38. Riviello ED, Kiviri W, Twagirumugabe T, et al. Hospital incidence and outcomes of the acute respiratory distress syndrome using the Kigali modification of the Berlin definition. Am J Respir Crit Care Med. 2016;193(1):52–59. doi:10.1164/rccm.201503-0584OC
39. Ranieri VM, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi:10.1001/jama.2012.5669
40. Wenzhong L, Hualan L. COVID-19: attacks the 1-beta chain of hemoglobin and captures the porphyrin to inhibit human heme metabolism. ChemRxiv. 2020;105. doi:10.26434/chemrxiv.11938173.
41. Read R. Flawed methods in “COVID-19: attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism”; 2020. doi:10.26434/CHEMRXIV.12120912.V1
42. DeMartino AW, Rose JJ, Amdahl MB, et al. No evidence of hemoglobin damage by SARS-CoV-2 infection. Haematologica. 2020;105(12):2769–2773. doi:10.3324/haematol.2020.264267
43. Janz DR, Ware LB. The role of red blood cells and cell-free hemoglobin in the pathogenesis of ARDS. J Intensive Care. 2015;3(1):20. doi:10.1186/s40560-015-0086-3
44. Yu XS, ZQ Chen, YF Hu, et al. Red blood cell distribution width is associated with mortality risk in patients with acute respiratory distress syndrome based on the Berlin definition: a propensity score matched cohort study. Heart Lung. 2020;49(5):641–645. doi:10.1016/j.hrtlng.2020.04.008
45. Wang B, Gong Y, Ying B, Cheng B. Relation between RED CELL distribution width and mortality in critically ill patients with acute respiratory distress syndrome. Biomed Res Int. 2019;2019:1–5.
46. Menk M, Giebelhäuser L, Vorderwülbecke G, et al. Nucleated red blood cells as predictors of mortality in patients with acute respiratory distress syndrome (ARDS): an observational study. Ann Intensive Care. 2018;8(1):42. doi:10.1186/s13613-018-0387-5
47. Liang W, Liang H, Ou L, et al. Development and validation of a clinical risk score to predict the occurrence of critical illness in hospitalized patients with COVID-19. JAMA Intern Med. 2020;180(8):1081–1089. doi:10.1001/jamainternmed.2020.2033
48. Kuri-Cervantes L, Pampena MB, Meng W, et al. Comprehensive mapping of immune perturbations associated with severe COVID-19. Sci Immunol. 2020;5(49). doi:10.1126/sciimmunol.abd7114.
49. Aktas G. Hematological predictors of novel Coronavirus infection. Rev Assoc Med Bras. 2021;67(suppl 1):1–2. doi:10.1590/1806-9282.67.suppl1.20200678
50. Khalid A, Ali Jaffar M, Khan T, et al. Hematological and biochemical parameters as diagnostic and prognostic markers in SARS-COV-2 infected patients of Pakistan: a retrospective comparative analysis. Hematology. 2021;26(1):529–542. doi:10.1080/16078454.2021.1950898
51. Kilercik M, Demirelce Ö, Serdar MA, Mikailova P, Serteser M. A new haematocytometric index: predicting severity and mortality risk value in COVID-19 patients. PLoS One. 2021;16(8):1–19. doi:10.1371/journal.pone.0254073
52. Ji D, Zhang D, Xu J, et al. Prediction for progression risk in patients with COVID-19 pneumonia: the CALL score. Clin Infect Dis. 2020;71(6):1393–1399. doi:10.1093/cid/ciaa414
53. Hue S, Beldi-Ferchiou A, Bendib I, et al. Uncontrolled innate and impaired adaptive immune responses in patients with COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med. 2017;202(11):1509–1519. doi:10.1164/rccm.202005-1885OC
54. Fulop T, Larbi A, Dupuis G, et al. Immunosenescence and inflamm-aging as two sides of the same coin: friends or Foes? Front Immunol. 2018;8. doi:10.3389/fimmu.2017.01960
55. Karlberg J, Chong DSY, Lai WYY. Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol. 2004;159(3):229–231. doi:10.1093/aje/kwh056
56. Alghamdi IG, Hussain I, Alghamdi M, et al. The pattern of Middle East respiratory syndrome coronavirus in Saudi Arabia: a descriptive epidemiological analysis of data from the Saudi Ministry of Health. Int J Gen Med. 2014;7:417–423. doi:10.2147/IJGM.S67061
57. Azad P, Villafuerte FC, Bermudez D, Patel G, Haddad GG. Protective role of estrogen against excessive erythrocytosis in Monge’s disease. Exp Mol Med. 2021;53(1):125–135. doi:10.1038/s12276-020-00550-2
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.