Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Integrating Tobacco Dependence Treatment into Hospital Practice Using the Rochester Model
Authors Grable JC , Lin JK , Peltzer K, Schultz R, Bugbee D, Pilipenko M, Levy SC, Hawkins S
Received 22 December 2022
Accepted for publication 23 March 2023
Published 4 April 2023 Volume 2023:16 Pages 905—911
DOI https://doi.org/10.2147/JMDH.S400615
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
John C Grable,1,* Jonathan K Lin,2,* Kenneth Peltzer,1,* Rebecca Schultz,1,* Doris Bugbee,3,* Mikhail Pilipenko,3,* Scott C Levy,1,* Shayne Hawkins3,*
1Department of Medicine, University of Rochester School of Medicine, Rochester, NY, USA; 2Department of Medicine, UT Southwestern Medical Center, Dallas, TX, USA; 3Department of Nursing, University of Rochester School of Medicine, Rochester, NY, USA
*These authors contributed equally to this work
Correspondence: John C Grable, University of Rochester School of Medicine, 601 Elmwood Avenue, Rochester, NY, 14642, USA, Tel +1 585-275-7424, Fax +1 585-276-2820, Email [email protected]
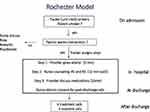
Purpose: Delivering evidence-based tobacco dependence treatments to hospital patients in real-world settings continues to be a challenge. To achieve long-term abstinence, a program should provide both bedside counseling and post-discharge contacts. These program features are necessary but difficult to implement due to lack of training, time and low administrative support. The Rochester Model is a tobacco treatment program using existing staff and medical students to reduce the barriers for treating hospitalized smokers.
Patients and Methods: Any smoking patient admitted to a participating hospital unit can participate. Staff nurses, mid-level providers and physicians deliver the counseling steps during the admission. Nurses hold two bedside counseling sessions, while providers give quitting advice and encourage pharmacotherapy. Nurses also contribute as unit champions and post-discharge call counselors. New York State quit line counselors combined with a University of Rochester call team fulfill the post-discharge calls. The latter call team is composed of staff nurses, respiratory therapists and medical students.
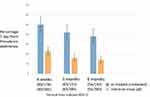
Results: The number of smoking patients screened was 2610 while 385 enrolled after a proof-of-concept period. The 7-day point prevalence quit rates using the as treated (patients contacted) analysis is 50% at 4 weeks, 42% at 3 months and 38% at 6 months. The 7-day point prevalence quit rates using the intent-to-treat (all patients) analysis is 23% at 4 weeks, 16% at 3 months and 14% at 6 months.
Conclusion: Preliminary data on the Rochester Model is showing an effective yet affordable tobacco treatment program using hospital staff and medical students. Nurses serve as bedside counselors, unit champions and post-discharge call counselors. Hospitals, even with limited resources, can implement tobacco treatment programs using existing staff.
Keywords: tobacco dependence treatment, nurse counseling, quit-line counseling, respiratory therapists, medical students
Plain Language Summary
Hospitalization is a window of opportunity to help smokers quit. Successful programs require both bedside counseling and post-discharge contacts beyond a month. The barriers for hospital smoking programs are numerous but cost is the major issue. The Rochester Model is a tobacco treatment program that uses hospital staff and medical students to counsel patients at the bedside and give phone counseling to patients after discharge. Nurses have the largest contribution to the program. The program is showing high quit rates at a low cost.
Introduction
A hospital admission is a “window of opportunity” to assist smoking patients in a quit attempt.1,2 The Joint Commission issued an optional measure set for screening and treatment of hospitalized smokers in 2012.3 Many hospital systems do not offer these programs despite evidence that in-patient tobacco treatments increase cessation rates,4 decrease readmission rates5 and reduce costs.6 Challenges for a hospital staff to treat in-patient smokers include the lack of training, daily time constraints and low administrative support.7 Administrative costs and the perceived return on the investment are the major barriers.4,6 Securing funding for comprehensive hospital tobacco programs is a significant issue for US hospital systems.4
Sustaining long-term abstinence requires counseling in the hospital, followed by least one month of supportive contacts after discharge.1 A review of academic center programs4 shows that tobacco treatment specialists (TTS) or specialist Respiratory Therapists (RT) can function as bedside counselors. Because of the nominal reimbursements available from US health care, these programs require major institutional support (>$140,000 per year)4,6 One emerging strategy is the use of hospital staff nurses to deliver bedside interventions.8 A Tobacco Tactics Program, using staff nurses as counselors, showed significant quit rate improvements in several hospital systems.8,9 The independently created Rochester Model (RM) program trains nurses in a 30-minute session, then provides continuing education using an on-line module and brief refreshers by a nurse champion.
After hospital discharge, contacts beyond a month are necessary to maintain abstinence. Post-discharge calls are difficult for hospitals to implement due to the lack of personnel, time and support.7 State Quit lines are available, but many states, including New York, offer just two calls.10 Interactive Voice Response (IVR) systems are adopted for post-discharge support but the cost is considerable ($55,000 per year).4,6 At low cost, the RM program uses New York state quit line counselors combined with a University of Rochester (UR) call team for the post-discharge calls.
The purpose of this report is to demonstrate the efficacy and low cost of the RM program. This unique program uses hospital staff and medical students to deliver both bedside counseling and stage-based, post-discharge calls.
Materials and Methods
Design, Setting and Population
After review of existing tobacco treatment programs11–13 and resource evaluation, the RM program was designed. The program received approval from the hospital chief medical officer, the nursing administration and each unit nurse manager. The design is an evidence-based service program and IRB approval is not required. Strong Memorial Hospital (SMH) has 886 beds with 39,000 annual admissions in Rochester NY. After a pilot from Jan. 2013 to Feb. 2014 on unit 612, the program expanded to hospital units 712, 714 and 736. Units 614 and 634 joined in 2018, followed by units 516 and 536 in 2021 (Figure 1). These represent four medicine, two cardiac, and two neurology units, with ten units remaining. An active smoker of any amount admitted to a participating unit can join.
Screening and Enrollment
The unit clerk, designated as the tracker, screens new admissions for smoking (Figure 2). The tracker inquires if the patient wishes to participate. For patients who decline, the patient’s nurse provides a handout of community programs.
Training of Unit Nurses for the Bedside Counseling and the Nurse Champion
Nurses train for the bedside counseling during a 30-minute session. Five successive days were required to train an average of 35 nurses on a unit using handouts and segments from “Clearing the Air” manual.14 The sessions include patient motivation, nicotine addiction, triggers, coping skills and social supports. In 2016, an on-line module was prepared and nurses were assigned this continuing education every 6 months. Each unit established a nurse champion to review the counseling steps at regular intervals with nurses. Mid-level providers and physicians received program training at conferences and unit sign-out rounds.
Recruitment and Training of UR Post-Discharge Call Counselors
Emails and screen server advertisements invite nurses, respiratory therapists (RT) and UR medical students (MS) to become post-discharge call counselors. First through fourth year, MS seeking volunteer activities became call counselors. An on-line module followed by a 45-minute didactic session trained nurses, RT staff and MS. The module and didactic session presented scenarios that call counselors might encounter and how to reinforce the quit plan developed in the hospital.
The UR Post-Discharge Call Team and Reimbursements
From 2013 to 2015, the call team consisted of four unpaid volunteer RT staff. From 2016 to 2020, 2–4 RT staff and 2–4 nurses were paid $15.64/hour for call counseling. From 2017 to 2019, 3–7 MS (volunteers) participated. To maintain a steady number of counselors, a nurse call counselor (NCC) program was developed in 2020. After this, the hourly payments to nurses and RT staff stopped.
Nurse Call Counselor Program
The number of nurses, RT staff or medical students available for post-discharge counseling varied each year due to interest and availability. A nurse call counselor (NCC) program was developed in order to obtain a steady number of counselors each year. The program received approval from the UR nursing administration. The program, which began Sept. 2020, advances the nurse pay grade from level two to level three. The program requires staff nurses call 15 patients, recording the calling strategies and outcomes. The nurse then presents his/her findings to a nursing promotion panel for approval. Three nurses who completed this NCC program continue to call post-discharge patients.
Low Program Costs
The Department of Medicine awarded $8200 (total program cost) from Jan. 2013 to Sept. 2020. The RT and nurse phone counseling time was reimbursed with this support from 2016 to 2020. In comparison, a Tobacco Treatment Service using a TTS counselor with an IVR system reported yearly costs of $143,000.6
Program Process Changes
Figure 1 shows the timeline of program changes. The collection of outcome data to 6 months started Feb. 2016. Starting Oct. 2018, the demographic/smoking data (Table 1) was recorded when adequate staff was available. Starting Sept. 2020, the NCC program for nurses began. Unit clerks established as trackers improved the program flow. On-line modules were prepared to train unit nurses and to motivate patients to participate. The final program (Figure 2) developed from Jan. 2013 to Feb. 2016 using the Plan-Do-Study-Act cycles of quality improvement.15
 |
Table 1 Demographic and Smoking Data Collection Started October 2018 on 100 Patients and Averaged |
Inpatient Intervention
Smoking patients are invited to watch a video describing the program that gives testimonials from ex-smokers. The unit clerk-tracker (Figure 2) assigns staff and tracks Steps 1–3 in a unit log. Typically within hospital day 1–2, the tracker notifies the provider to give Step 1 advice. When the patient’s condition dictates, the patient’s nurse gives Nurse counseling #1, using “Clearing the Air” segments to discuss motivation, secondhand smoke and nicotine addiction. A following nurse gives Nurse counseling #2 session, discussing triggers, coping behaviors and completes a summary worksheet. Each nurse counseling session lasted about 15 minutes. Starting pharmacotherapy is the standard of care for inpatient smokers,3 so the provider team discusses nicotine replacement, Bupropion or Chantix options in Step 3. The patient fills out a consent form updating contact information and giving permission to receive post-discharge calls. On discharge, the provider team provides medication prescriptions that patient and provider have agreed upon. If a patient is discharged before completing the steps they are not followed further but are given a handout of outpatient cessation resources.
Treatment, Outcome Calls and Evaluation Methods
A prior study showed four post-discharge treatment calls are effective,16 so the RM program provides this. Patients are E-referred to the NYS quit line and receive two treatment calls within two weeks after discharge. Then, the UR team places two treatment calls (3-and 6 weeks) and three outcome calls (4 weeks, 3-and 6 months) after discharge. The outcome calls (self-report) only ask if patients have smoked even a puff in the last seven days. This defines 7-day point prevalence.17 Five treatment or outcome calls are attempted at each time point. A designation of “not reached” includes patients without contact at two successive time points (total 10 attempts). A designation of “smoker” includes patients who decline calls or request to stop the program. During a post-discharge call, the demographic and smoking data are collected. Quit confidence is a self-reported measure: 5 is most confident, 1 is least confident to quit smoking at discharge (Table 1).
Data Analysis
Self-reported 7-day point prevalence abstinence at 4 weeks, 3-and 6 months determined the quit rates. Quit rates are calculated using the as treated (AT) analysis and the intention-to-treat (ITT) analysis. The AT analysis accounts for patients who were contacted by phone. The AT analysis is calculated as follows: number of patients quit/number of patients contacted (quit + smokers). The ITT analysis accounts for all the patients whether they were contacted or lost to follow-up. The ITT analysis is calculated as follows: number of patients quit/number of all patients (quit+ smokers + not reached) at a time point. The confidence intervals were calculated by R package DescTools, R version 4.2.1.
Results
Screening and Enrollment Data
During the proof-of-concept period (Jan. 2013-Feb. 2016), 871 patients were screened and 316 patients enrolled. After this, 2610 patients were screened while 385 patients enrolled from Feb. 2016-Mar. 2021 (Table 2). The interval increase in the patients screened from 1/19–3/21 is likely due to the addition of two program units on Oct. 2018 (Figure 1).
 |
Table 2 Screening and Enrollment Data from Feb 2016 to March 2021 |
Demographic and Smoking Data
The demographic and smoking data collected on 100 patients starting Oct. 2018 (Table 1) after program staff were available (Figure 1). This patient group had 47% cardiac diagnoses, the average quit confidence was 80% and 58% received post-discharge pharmacotherapy.
Smoking Cessation Outcome Data
From Jan. 2013-Jan. 2016 including the pilot and proof-of-concept period, 316 patients enrolled showing a 7-day point prevalence quit rate of 52% at 4 weeks using the AT analysis. From Feb. 2016 to Mar. 2021, data collection occurred at 4 weeks, 3- and 6 months on 385 patients. Using the AT analysis (patients contacted) the 7-day point prevalence quit rates at 4 weeks, 3-and 6 months are 50% (89/178), 42% (63/151) and 38% (54/143), respectively (Figure 3). Using the ITT analysis (all patients) the 7-day point prevalence quit rates at 4 weeks, 3-and 6 months are 23% (89/385), 16% (63/385) and 14% (54/385), respectively. The 95% CI for all time points for both the AT and ITT patients are displayed. A small sample (20 patients) who declined the program showed a quit rate of 20% at 4 weeks using the AT analysis.
Discussion
Smoking outcomes were collected at 4 weeks, 3- and 6 months on 385 patients, after the proof-of-concept period. The AT (patients contacted) group show a robust 6-month quit rate of 38%, exceeding a benchmark self-report AT quit rate of 25% for hospital programs.18 The program cost is much lower than programs using a TTS6 or a study-nurse bedside counselor.18
The Rochester Model has novel features. The program promotes tobacco treatments in daily hospital patient care and gives staff continuing cessation education. Hospital nurses are the major program contributors, serving as bedside counselors, unit champions and post-discharge call counselors. Nurse bedside counseling is logical as they are the largest number of health-care workers spending considerable time with patients.19,20 The RM program offers a new role for nurses as post-discharge call counselors. A call counselor program promotes both career and pay incentives to attract and retain nurses in this role. The RM program shows that a team including nurses, RT’s and medical students can accomplish the post-discharge call counseling.
Limitations
The program now needs evaluation using implementation processes.21 Evaluations of nurse, provider acceptance, adherence, program feasibility and costs are necessary. Limitations of this initial report include the incomplete demographic/smoking data and the lack of biochemical verification.
Conclusions
The Rochester Model program shows robust quit rates at low cost while fulfilling the Joint Commission guidelines for treatment of inpatient smokers.3 A hospital system with limited resources can implement an effective tobacco dependence program using existing staff. This program should appeal to health-care systems, particularly those with limited budgets seeking an effective method to treat hospitalized smokers.
Abbreviations
RM, Rochester Model; TTS, Tobacco Treatment Specialist; RT, Respiratory Therapist; MS, Medical student; UR, University of Rochester; IVR, interactive voice response; NCC, nurse call counselor, AT, as treated, ITT, intent-to-treat.
Acknowledgments
The authors would like to thank Dr. Kimberly P. Richter PhD, MPH from the University of Kansas for her helpful comments.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Rigotti NA, Clair C, Munafo MR, Stead LF. Interventions for smoking cessation in Hospitalized patients. Cochrane Database Syst Rev. 2012;5:CD001837. doi:10.1002/14651858.CD001837.pub3
2. Rigotti NA, Stoney C. CHARTing the future course of tobacco-cessation interventions for hospitalized smokers. Am J Prev Med. 2016;51(4):549–550. doi:10.1016/j.amepre.2016.07.012
3. Fiore MC, Goplerud E, Schroeder SA. The joint commission’s new tobacco-cessation measures-will hospitals do the right thing? NEJM. 2012;366:1172–1174. doi:10.1056/NEJMp1115176
4. Palmer AM, Rojewski AM, Chen LS, et al. Tobacco treatment program model in US hospitals and outpatient centers on behalf of the SRNT treatment network. Chest. 2020;159:1652–1663. doi:10.1016/j.chest2020.11.025
5. Cartmell KB, Dooley M, Muller M, et al. Effect of an evidence-based inpatient tobacco dependence treatment service on 30-,90-and 180 day hospital readmission rates. Med Care. 2018;56(4):358–363. doi:10.1097/MLR.0000000000000884
6. Cartmell KB, Dismuke CE, Dooley M, et al. Effect of an evidence-based inpatient tobacco dependence treatment service on 1-year postdischarge health care costs. Med Care. 2018;56(10):883–889. doi:10.1097/MLR.0000000000000979
7. Sharpe T, Alsahlanee A, Ward K, Doyle F. Systematic review of clinician-reported barriers to provision of smoking cessation interventions in hospital inpatient settings. J Smok Cessat. 2018;13(4):233–243. doi:10.1017/jsc.2017.25
8. Duffy SA, Ronis DL, Karvonen-Gutierrez CA, et al. Effectiveness of the tobacco tactics program in the department of veterans affairs. Ann Beh Med. 2014;48:265–274. doi:10.1007/s12160-014-9605-z
9. Duffy SA, Ronis DL, Karvonen-Gutierrez CA, et al. Effectiveness of the tobacco tactics program in the Trinity health system. Am J Prev Med. 2016;51(4):551–565. doi:10.1016/j.amepre.2016.03.012
10. North American Quitline Consortium. Quitline profiles 2020. Available from: http://map.naquitline.org/.
11. Miller NH, Smith PM, DeBusk RF, Sobel DS, Taylor CB. Smoking cessation in hospitalized patients. results of a randomized trial. Arch Intern Med. 1997;157:409–415. doi:10.1001/archinte.1997.00440250059007
12. Reid RD, Mullen KA, Slovine ME. Smoking cesation for hospitalized smokers: an evaluation of the “Ottawa Model”. Nicotine Tob Res. 2010;12(1):11–18. doi:10.1093/ntr/ntp165
13. Rigotti NA, Regan S, Levy D, et al. Sustained care intervention and postdischarge smoking cessation among hospitalized adults. A randomized clinical trial. JAMA. 2014;312(7):719–728. doi:10.1001/jama.2014.9237
14. National Cancer Institute. Clearing the Air. NIH Publication No. 08-1647. National Cancer Institute; 2008.
15. Crowl A, Sharma A, Sorge L, Sorenson T. Accelerating quality improvement within your organization: applying the model for improvement. J Am Pharm Assoc. 2003. doi:10.1331/JAphA.2015.15533
16. Taylor CB, Miller NH, Cameron R, Fagans EW, Das S. Dissemination of an effective inpatient tobacco use cessation program. Nicotine Tobacco Res. 2005;7(1):129–137. doi:10.1080/14622200412331328420
17. Cheung KL, De Ruijter D, Hiligsmann M, et al. Exploring consensus on how to measure smoking cessation. A Delphi study. BMC Public Health. 2017;17:890. doi:10.1186/s12889-017-4902-7
18. Smith P, Reilly K, Miller NH, DeBusk RF, Taylor CB. Application of a nurse-managed inpatient smoking cessation program. Nicotine Tobacco Res. 2002;4:211–222. doi:10.1080/14622200210123590
19. Kazemzadeh Z, Manzari ZS, Pouresmail Z. Nursing interventions for smoking cessation in hospitalized patients: a systematic review. Int Nurs Rev. 2016;64:263–275. doi:10.1111/inr.12320
20. Rice VH, Heath L, Livingstone-Banks J, Hartman-Boyce J; the Cochrane Tobacco Addiction Group. Nurse practitioner interventions for smokers with chronic hepatitis C. Cochrane Database Syst Rev. 2017;2017(12):CDO01188.
21. Pearson N, Naylor PJ, Ashe M, Fernandez M, Yoong SL, Wolfenden L. Guidance for conduction, feasibility and pilot studies for implementation trials. BMC. 2020;6:167.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.