Back to Journals » International Journal of General Medicine » Volume 8
Integrating complementary/alternative medicine into primary care: evaluating the evidence and appropriate implementation
Authors Wainapel S, Rand S, Fishman L, Halstead-Kenny J
Received 30 April 2015
Accepted for publication 1 July 2015
Published 7 December 2015 Volume 2015:8 Pages 361—372
DOI https://doi.org/10.2147/IJGM.S66290
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser

Stanley F Wainapel,1 Stephanie Rand,1 Loren M Fishman,2 Jennifer Halstead-Kenny1
1The Arthur S Abramson Department of Physical Medicine and Rehabilitation, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, 2Department of Rehabilitation and Regenerative Medicine, College of Physicians and Surgeons, Columbia University, New York, NY, USA
Abstract: The frequency with which patients utilize treatments encompassed by the term complementary/alternative medicine (CAM) is well documented. A number of these therapies are beginning to be integrated into contemporary medical practice. This article examines three of them: osteopathic manipulation, yoga, and acupuncture, with a focus on their physiological effects, efficacy in treating medical conditions commonly encountered by practitioners, precautions or contraindications, and ways in which they can be incorporated into clinical practice. Physicians should routinely obtain information about use of CAM as part of their patient history and should consider their role based on physiological effects and clinical research results.
Keywords: integrative medicine, osteopathic manipulation, yoga, acupuncture therapy
Corrigendum for this paper has been published.
Introduction
Although alternative methods for treating disease have existed for hundreds, and even thousands of years, it is only within the past few decades that they have begun to be evaluated by clinical research and to be integrated into medical management. Dr Andrew Weil’s concept of “Integrative Medicine”1 is based on the incorporation of so-called “complementary/alternative medicine (CAM)” into the allopathic medical paradigm. Eisenberg et al2 have documented that CAM therapies are utilized by more than one-third of the population and that their use is often not communicated to the patient’s primary physician. Given this high prevalence, it is particularly important for medical practitioners to acquire greater knowledge about the potential benefits and hazards associated with them. This article examines three frequently encountered CAM therapies, the physiological basis for their effects, common clinical applications, precautions or contraindications, and opportunities for continuing education or training.
CAM encompasses a wide range of treatments, and a comprehensive review of all of them is beyond the scope of this article. A 400-page textbook edited by one of the authors3 examined only ten of them. However, using the conceptual framework posited in that book, CAM can be broadly classified into six categories:
- Manipulative therapies involve a relatively passive patient with an active therapist who manipulates soft tissue, muscles, tendons, joints, and/or bones, usually using the hands. Examples include osteopathic manipulative treatment (OMT), chiropractic, massage therapy, reflexology, acupressure, and therapies developed by Rolfe, Prudden, and others.
- Movement therapies involve an active patient supervised by the therapist. Movements or postures encourage mobility, strength, balance, coordination, and/or mental clarity. Examples include yoga, tai chi, Pilates-therapy, and Alexander technique.
- Physical modalities involve agents such as heat, cold, light, water, oxygen, and electricity, which are applied for medicinal effects. Examples include hydrotherapy, electrotherapy, acupuncture (including electroacupuncture), hyperbaric oxygen, and light therapy.
- Mind–body therapies can be considered manipulative and/or movement therapies with the mind as prime mover. Examples include prayer, mindfulness meditation, Transcendental Meditation, hypnotherapy, biofeedback, and guided imagery.
- Medicinal therapies involve ingestion of food, nutritional supplements, herbal formulae, or homeopathic preparations to treat symptoms of disease and improve health. Examples include botanical (herbal) medicine, nutritional therapy, and homeopathy.
- Mixtures is a category in which the previous five approaches are combined as part of comprehensive non-allopathic-based systems of care, including traditional Chinese medicine (TCM), Ayurvedic Medicine (AM), or naturopathic medicine.
The treatments discussed in the following sections of this article are representative of the first three of these categories: OMT (manipulation), yoga (movement), and acupuncture (modalities). It should be stressed that mind–body and medicinal therapies are equally worthy of detailed study and have many applications relevant to medical care but would warrant a separate article of at least equal length to this one. Also, the clinical applications for which these three therapies have been recommended reflect the patient population seen by the authors, all of whom are specialists in physical medicine and rehabilitation rather than internal medicine or primary care. For example, while acupuncture has been used for treating symptoms of irritable bowel syndrome, asthma, sinusitis, and gynecologic problems, these conditions are not typically referred to physical medicine practitioners.
Osteopathic manipulative treatment
The principles and philosophy of osteopathic medicine were formulated in the late 19th century by Dr Andrew Taylor Still, a traditionally trained American physician.4 Contemporaneously, Daniel David Palmer founded the field of chiropractic, whose main principle is that vertebral malalignment can cause pressure on nerves, affecting visceral function and leading to disease.5 Both osteopathic and chiropractic practitioners manipulate soft tissues, vertebrae, and joints, but vertebral manipulation remains the hallmark of chiropractic; OMT utilizes a wider range of techniques.4,6 The families of Physiotherapist Edgar Cyriax and Physician James Mennell were instrumental in teaching manipulative medicine to European physiotherapists during the early 20th century. Their publications, including Cyriax’s classic Textbook of Orthopedic Medicine, are contemporary with those of the early osteopathic physicians.5 Cyriax or Mennell’s techniques have many parallels in OMT.
The main tenets of osteopathic medicine are as follows:
- The body is a unit.
- Structure and function are interrelated.
- The body possesses self-regulatory mechanisms.
- The body has the inherent capacity to defend and repair itself.
- When normal adaptability is disrupted, or when environmental changes overcome the body’s capacity for self-maintenance, disease may ensue.
- Rational treatment is based on the previous principles.4
Techniques and physiological correlates
OMT practitioners manipulate bones, muscles, ligaments, and/or fascia to relieve pain, improve function, and return the body to its natural state, reinforcing its inherent self-healing capabilities. Somatic dysfunction is defined as the impaired or altered function of components of the somatic system: skeletal, arthrodial, and myofascial structures, and their related vascular, lymphatic, and neural elements.4 The effectiveness of OMT has been documented in the treatment of a number of conditions, including spine pain, fibromyalgia, influenza, and pulmonary disease.6–15 It has also been associated with decreased length of stay for hospitalized patients in various studies.7,16 However, OMT research has inherent difficulties. Efficacy studies do not easily fit the scientific model because it is difficult to have a blinded protocol or to perform a sham manipulation.17
Commonly used OMT techniques include myofascial release encompassing counterstrain, balanced ligamentous tension, and cranial osteopathy; muscle energy (ME); and high-velocity low-amplitude thrusting (Figure 1). Myofascial release stretches and releases muscle and/or fascial restrictions. ME utilizes muscle contractions (usually isometric) and stretching for muscle spasms contributing to structural imbalances. High-velocity low-amplitude thrusting involves positioning a joint with limited motion against its restrictive barrier and then applying a short (low amplitude) quick (high velocity) thrust to move it past the barrier.4,18 These techniques utilize different neurophysiologic principles. Counterstrain shortens the muscle spindle, resetting hyperactive gamma motor neurons associated with spasm. ME may trigger the Golgi tendon organ (GTO, stretch receptors in the skeletal muscle) reflex, reciprocal innervation reflex, or elastic stretch reflex.4 Lymphatic pump techniques directly increase lymph flow and leukocyte concentration within lymphatic fluid, as well as increase antibody response to pathogens.19
Many OMT techniques are safe enough to use in pregnant women, acutely ill individuals, or elderly patients. Contraindications include high-velocity low-amplitude thrusting in patients with rheumatoid arthritis, osteoporosis, or Down syndrome, which could produce catastrophic spinal cord damage; and ME in intensive care units or following recent surgery, where active muscle exertion can compromise healing. The use of OMT in patients with cancer remains controversial.4,18
Clinical applications
Spine disorders and fibromyalgia
Back pain is the most common reason patients seek osteopathic care and is also OMT’s most studied use. Other treated musculoskeletal conditions include neck pain, sprains, tension headaches, post-orthopedic surgery, and fibromyalgia.17 In one study of patients with fibromyalgia, Gamber et al found that OMT plus medication was more likely to improve pain and relieve tenderpoints, as well as improve independence in self-care and associated psychological symptoms.9 Studies have shown improvement in low back pain (LBP) in patients treated with OMT compared with placebo, active treatment, or no treatment.11–13,17 A meta-analysis by Licciardone et al showed that pain reduction from OMT is greater than expected from placebo effects alone, while further studies show that pain relief continues for at least 3 months and up to 1 year posttreatment.11,13 OMT can decrease the use of pain medications as well as physical therapy.14,15 In addition to improving short-term physical outcomes, OMT can have longer term beneficial effects, avoiding the development of disability and chronic pain states.12,14
Influenza and respiratory disease
Studies related to the 1918 influenza pandemic documented dramatically lower mortality rates among patients receiving osteopathic treatment.10 Although contemporary osteopathic physicians advocate influenza vaccination, antivirals, and chemoprophylaxis, they also continue to use OMT, such as lymphatic pump techniques, when treating patients with influenza.20 Lymphatic pump techniques directly or indirectly manipulate the lymphatic system by milking lymphatic glands, releasing fascial strain around lymphatic glands, and applying gentle manual vibrations to the spleen, liver, thorax, or feet (using the legs as levers to rock the body, Figure 2).4,21 Similar techniques are also used as an adjunct in treating asthma, postoperative atelectasis, and pneumonia.4,8,17 Adding OMT to conventional care in multicenter studies of patients with pneumonia reduced length of stay and need for antibiotics by 1–2 days.8,17
  | Figure 2 Pedal pump technique. |
Obstetrical and pediatric applications
OMT has a potential role in reducing pregnancy-related back pain as well as labor pain.22,23 Back pain in pregnancy is extremely common, particularly during the second trimester.24 In pediatrics, OMT has been documented to be effective in decreasing episodes of acute otitis media and the need for surgery in recurrent otitis media, as well as improving sleep and decreasing time spent crying in newborns with infantile colic.17
Education and training
The Osteopathic International Alliance differentiates between osteopathic physicians and osteopaths. Both must have “achieved the nationally recognized academic and professional standards within his or her country to independently practice diagnosis and provide treatment based upon the principles of osteopathic philosophy”, but the osteopathic physician additionally has unlimited medical practice privileges.25 In the United States, osteopathic medical colleges accredit physicians to practice medicine and surgery through a 4-year academic curriculum similar to allopathic medical schools, granting the degree Doctor of Osteopathy (DO). There are currently 30 osteopathic medical schools in the United States, whose graduates learn OMT through an additional mandatory 150–200 hours of study during training.17,26 According to an informal 2013 survey by the Osteopathic International Alliance, there were over 82,000 practicing American osteopathic physicians, while Russia, France, and Germany had the most DOs outside of the United States, numbering approximately 1,300, 1,600 and 2,300, respectively. In France and Germany, osteopaths greatly outnumber osteopathic physicians.25
Continuing Medical Education courses are available for physicians or physiotherapists to learn OMT. Harvard Medical School’s Department of Continuing Education holds an intensive 3-day “Introduction to Osteopathic Manipulative Medicine” as does the University of New England College of Osteopathic Medicine for interested MDs or practicing DOs who need a refresher course.27 Michigan State University College of Osteopathic Medicine holds a yearlong series of courses in OMT available to DOs, MDs, or physiotherapists, and the London College of Osteopathic Medicine holds a 2 days per week 18-month-long course in Osteopathy for physicians.27–29
Yoga
Originally developed in India, yoga is one of the oldest forms of Integrative Medicine. This discussion will focus on using asanas, the poses associated with hatha yoga, to treat specific medical conditions. Asanas are postures in standing, sitting, supine, prone, or inverted positions, combining flexibility, balance, strength, and mental focus. BKS Iyengar’s Light on Yoga30 should be used as reference for precise illustration of each asana. Treatment recommendations reflect a yoga-based office practice involving more than 20,000 patients over 35 years.
Yoga physiology
Yoga poses are held for prolonged periods, initially stimulating and subsequently inhibiting myotatic reflexes. During muscle stretch, intrafusal (IF) muscle fibers are facilitory and the GTO inhibitory. IF fibers initially stimulate brisk muscle contraction (Figure 3), as in the patellar reflex, a reaction initially stronger than the GTO’s inhibition, but after 60–120 seconds, the IF adjusts signal intensity, and the GTO’s inhibitory response predominates, favoring increased stretch and relaxation. The agonist–antagonist relationship invoked by yoga practitioners is harder to observe. Quadriceps contraction induces hamstring relaxation (reciprocal relaxation), while yoga promotes quadriceps tightening in this situation for a better hamstring stretch. A third mechanism explains yoga’s beneficial effect on heart rate and blood pressure. Meditation, breathing exercises, and “extreme” postures stimulate visceral afferents of the vagus nerve, inclining the autonomic nervous system from sympathetic “fight-or-flight” toward parasympathetic “rest-and-digest” responses.31,32
Orthopedic/musculoskeletal applications
Back pain/sciatica
Treatment depends on specific diagnosis. Lumbar herniations are treated with extension-based postures (Salabhasana, Setu Bandhasana, and Ustrasana), functioning like McKenzie extension exercises in physiotherapy;33 conversely, spinal stenosis requires forward bending postures (Janu Sirsasana, Adho Mukha Svanasana, and Paschimottanasana).34 Piriformis syndrome, while not originating in the lower back but presenting with sciatica, is best alleviated with twisting postures (Matsyendrasana, Parivrtta Trikonasana, and Parivrtta Parsvakonasana). In sacroiliac joint derangement, adduction as in Gomukhasana and Garudasana is effective.35 In axial back pain, quadratus lumborum spasm is best relieved by forward bends. Facet syndrome from arthritis or spasm of short intravertebral muscles respond to bilateral asymmetrical stretch (Parighasana and Supta Padangusthasana II) and twists (Matsyendrasana and Marichyasana). Other postural anomalies (hyperlordosis and “flat-back syndrome”) respond to relatively gentle postures such as Janusirsasana, Balasana, and Parsvottanasana.35
Rotator cuff tear
A 1-minute headstand or less-demanding equivalent activates the subscapularis, which substitutes for the torn supraspinatus in 90% of these injuries. One study records doubling to tripling of painless abduction and flexion in 96% of 50 patients with magnetic resonance imaging (MRI)-confirmed supraspinatus tears.36 After doing the pose, electromyography demonstrates greater subscapularis activity between 80° and 110° abduction, the range in which the supraspinatus is most active (Figure 4). Yoga is instrumental in retraining the shoulder muscles, and patients operantly condition themselves to the new painless movement pattern. Individuals with highly trained shoulders such as baseball pitchers or violinists may take longer to improve. Slightly more arthritis in the affected shoulder has been noted on serial imaging, but patients retain painless functional range of motion after more than a decade of follow-up.
  | Figure 4 Electromyography of patient who had right shoulder rotator cuff repair, and used yoga for subsequent complete left cuff tear. |
Scoliosis/kyphosis
From 6 months to 8 months of daily practice of a minor variation of Vasisthasana, the side-plank posture improved the lower lumbar curve in adolescent idiopathic scoliosis by 49% and degenerative scoliosis an average of 38%.37 “S” and inverted “S” and triple curves require other postures such as Ardha Chandrasana and often require individual evaluation. Less dramatic reductions in thoracic curves possibly support the theory that higher curves are often compensatory. Even well-established kyphosis improves, albeit not as much as kyphosis in younger people. Poses such as Utkatasana, Salabhasana, and modified versions of Ustrasana are recommended.38
Plantar fasciitis and bunion
Muscular imbalance contributes to both these conditions; asanas such as Parsvottanasana, Trianga Mukhaikapada Paschimottanasan, Virasana, and Janusirsasana, performed serially, can effectively quiet the overactive extensors in plantar fasciitis and improve the tension of the abductor hallucis in cases of bunion if treatment is started early.35
Osteoporosis
A training DVD of yoga exercises was provided to nearly 800 patients over 7 years in an office setting. DEXA scan changes preceding study entry were compared with changes 2 and 4 years subsequently. Strong reversal of bone loss was seen in spine and hip in the pilot study (Figure 5).39 None of the patients have developed osteoporotic fractures in long-term follow-up. Yoga thus offers an alternative to pharmacological treatments, avoiding medication side effects, while producing better range of motion, posture, balance, and strength, all of which reduce the risk of falls and fractures.
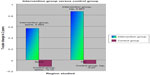  | Figure 5 A small pilot study showing dramatic gains in hip and spine in patients practicing yoga versus controls. |
Neurological and psychological applications
Multiple sclerosis
Yoga has been useful in the symptomatic treatment of multiple sclerosis40 through its effects on spasticity, balance, and coordination. The previously described physiological changes in myotatic and agonist–antagonist reflexes, as well as vagal stimulation, are the most compelling explanations for its efficacy. Additionally, there is good evidence that yoga alleviates the ubiquitous problem of fatigue in these patients.41
Post-traumatic stress disorder
A number of Veterans Administration facilities in the United States are using yoga to treat this service-related condition, with promising preliminary results.42 Combativeness, anxiety, and sadness are reduced by meditation and asana.43 Here, too, yoga’s action is partly mediated by the vagus nerve.44
Depression
Depression has been effectively treated through meditation, breathing, and asana. Weintraub45 has worked effectively with this approach, and Philbil46 has integrated yoga into psychotherapy for grief with beneficial results.
Insomnia
A combination of meditation and asana is most effective for promoting sleep. A three-part series of Supta Padangusthasana, the breathing exercise Viloma, and ten Tantric conceptual meditation have been utilized to help many individuals sleep without side effects.35 We suspect vagal afferents from the lungs aid the GTO, subduing hypothalamic, periventricular gray, and subcortical arousal centers.
Cardiovascular/pulmonary applications
Hypertension
Yeung et al47 and Chainani-Wu et al48 document significant drops in systolic and diastolic blood pressure with non-sectarian meditation. Other authors give evidence that yoga generates a similar parasympathetic emphasis in the autonomic nervous system, which slows the heart, dilates certain blood vessels, and promotes “rest and digest” as opposed to “fight or flight” predominance.32 Similar physiological changes may explain the beneficial effects of yoga on atrial fibrillation and other arrhythmias.49
The efficacy of yoga in asthma is debated. Papers favoring its utility outnumber those reporting no improvement,50 but no definitive conclusion can be reached at this time. The studies use different combinations of asana and breathing techniques, which may explain these disparities.
Endocrine applications
Diabetes mellitis
Innes and other researchers in India and Singapore have shown yoga to be salutary in controlling serum glucose levels. While any vigorous exercise will be valuable, yoga may be one of the least physically demanding, making it especially applicable in patients with medical or functional limitations. Done with vigor, yoga increases the muscular outflow of PGC1-alpha, a powerful endogenous anti-inflammatory known to decrease the incidence of diabetes type II.51–53
Precautions and contraindications
A recent survey of 33,000 yoga teachers/therapists54 found yoga injuries to be uncommon, generally self-correcting, and due more to the zealousness or perfectionism of the student than to poor alignment or inadequate teaching, the second and third most common causes. Some important contraindications to individual postures have been documented: inversion in headstand and handstand double intraocular pressure within 15–30 seconds of onset and twisting poses toward the side of a herniated disc may extend the herniation.35 Careful investigation is required in every application mentioned earlier, and it is recommended that yoga therapy be administered only with verified diagnosis and medical clearance.
Some types of yoga involve vigorous aerobic exercise or are performed in a room with high ambient temperatures. It may be inadvisable for patients with significant cardiovascular/pulmonary limitations or multiple sclerosis to participate in them. However, less strenuous yoga-based exercises have been safely used with frail elderly homebound patients or residents of long-term care facilities. Schaff55 has focused on such specialties as chair and aquatic yoga, which is effective and well-tolerated in the disabled population. Prinster56 has also developed programs for patients with cancer before, during, and after treatment.
Acupuncture
A growing body of research supports the validity of acupuncture as a therapeutic modality.57 Acupuncture is based on the principle of the movement of energy, traditionally referred to as “Qi”. Qi (energetics) is conceptualized as the movement of electrons. The acupuncture needle, a stainless steel shaft with a second alloy wrapping its handle, has the qualities of a weak electrode, which allows for several phenomena producing movement of electrons down the shaft to the needle tip when inserted into an acupoint.58 Having two metals in close proximity reinforces electron flow from one to another. A thermoelectric phenomenon is present when a temperature gradient forms between the inserted needle tip and the handle exposed to air, resulting in the tip becoming positive. Needle manipulation, adding heat, or electrical stimulation reverses polarity, causing the tip to become negative, theoretically driving electrons through a specific meridian.59,60
For over 3,000 years, acupuncture has been practiced based on a TCM paradigm. Qi is believed to circulate through a series of 14 principle channels (meridians), and disease symptoms result from alterations in circulation. Needle insertion into selected acupoints helps restore the normal balance of Qi (homeostasis). TCM practitioners examine the radial pulse and tongue and take a detailed history and systems review to identify these imbalances.59 Recent research has clarified the anatomical and neurochemical basis for the beneficial effects of this treatment.
Anatomy and physiology
Many acupuncture points are located in surface depressions along cleavage points of muscles, at bifurcations of large peripheral nerves or at sites of nerves passing through bony foramina.61,62 High correlations exist between muscle motor points, trigger points, and acupuncture points.63,64 Although acupoints do not contain specific structures, they seem to be organized in a distinctive fashion: vertical columns of loose connective tissue with a lymphatic trunk in the center coupled with a large arteriole and satellite vein. Morphologic studies demonstrate a net-like structure of unmyelinated cholinergic nerve fibers surrounding these vessels, and electron microscopy reveals high concentrations of microvesicles at sympathetic nerve terminations in 80% of acupoints.59
Stimulation of acupuncture points produces peripheral and central nervous system changes. Needle insertion causes local release of acetylcholine, resulting in vasodilatation in spastic or ischemic muscles, a rationale for the effectiveness of dry trigger point needling for myofascial pain.65 Substance P is also released into the microenvironment at the needle tip, peripherally influencing capillaries, mast cells, and sympathetic ganglia.66 Acupuncture needles mainly stimulate small myelinated (A-delta) afferent and muscle fibers that synapse in laminae I and V of the dorsal horn.67 The typical “De Qi” sensation (a dull ache elicited by needle placement) is attributed to the activation of small myelinated group III muscle afferents.68 The gate control theory (by which the small myelinated fibers stimulated by the acupuncture needle block the nociceptive impulses carried by the slower unmyelinated C fibers) and diffuse noxious inhibitory control contribute to acupuncture’s analgesic effects.69 Electroacupuncture influences different central nervous system levels depending on its frequency. Low frequency (2–4 Hz) stimulation is endorphin-dependent, activating spinal cord interneurons, the medulla’s raphe magnus nucleus, and the midbrain and hypothalamic peri-aqueductal gray (mesolimbic loop of analgesia).70 High frequency (>70 Hz) stimulation directly activates serotonergic and norepinephrinergic fibers in the midbrain’s dorsolateral fasciculus.71,72 Functional MRI has also been used to explore the specificity of individual acupuncture points.73,74
Clinical applications
Acupuncture is useful for treating chronic pain. A recent meta-analysis involving nearly 18,000 patients found it superior to both non-acupuncture control and sham acupuncture for chronic back and neck pain, osteoarthritis, headache, and shoulder pain.75 It has been separately studied in LBP.76,77 Most studies used individualized TCM rather than standardized acupoints. Lack of uniformity creates difficulties when designing research protocols. One research group applied electrical frequencies to needles placed segmentally along paraspinal musculature or peripheral nerves, a technique called percutaneous electrical nerve stimulation (PENS).78 They found significant short-term relief of chronic LBP superior to transcutaneous electrical nerve stimulation and exercise groups. In lumbar radiculopathy, PENS was more effective than transcutaneous electrical nerve stimulation for improving sleep and physical activity and reducing opioid use.79 Another study proposed 14 standardized points for chronic LBP. This single-center trial comparing the effectiveness of individualized versus standardized acupuncture treatments found them equally effective in reducing pain scores.80 The creation and validation of such pain “protocols” could help acupuncture become more of a standard of care in pain management.
Pericardium 6 (P6), an acupoint proximal to the volar wrist crease between radius and ulna, has been very effective for treating motion sickness and nausea/vomiting, including symptoms associated with chemotherapy. Acupuncture combined with medication significantly reduced the incidence and degree of delayed chemotherapy-induced nausea and vomiting (CINV).81 A 2015 study compared needling of P6 to IV zofran in patients receiving moderately emetogenic chemotherapy. Acupuncture and medication treatment arms had comparable effectiveness in acute CINV, and acupuncture seemed more effective in preventing delayed CINV.82 A functional MRI study has identified specificity when needling this point, and at least, one study suggests downregulation of serotonin and dopamine as the underlying mechanism.83,84
Several Cochrane database reviews explore acupuncture’s effectiveness in preventing migraine and tension-type headaches. The most recent reviews concluded that acupuncture is at least as effective as prophylactic drug treatment and has fewer adverse effects when used for migraine prophylaxis, but evidence did not support superiority of true over “sham” acupuncture.85 The same researchers stated acupuncture could be a valuable non-pharmacologic modality for recurrent tension headache.86
Acupuncture for insomnia also has some growing support. In 2007, a systematic review of auriculoacupuncture concluded that it appears to be favored over control interventions for increasing sleeping hours, maintenance, and feeling refreshed upon awakening, although further well-designed trials were recommended.87 In auriculoacupuncture, needles are placed in specific locations on the external ears. Auriculoacupuncture does not require the patient to disrobe and can be carried out in group-style settings allowing for greater flexibility and efficiency.
Precautions and recommendations
The York acupuncture safety study reported no serious adverse events in over 34,000 treatments.88 Nine surveys involving nearly 250,000 patients found a very low incidence of serious complications, such as pneumothorax and needle fracture requiring surgical removal (0.001%).89 Minor events included local bleeding, discomfort at the needle sites, tiredness, syncope, and forgotten needles. Pooled data revealed ten cases with delayed physician contact and effective conventional therapy among patients being treated by TCM practitioners. Missed diagnosis or delayed treatment is less likely in countries that only allow licensed physicians to practice acupuncture, such as Austria or Germany, but in countries that certify both physician and TCM-trained practitioners, delayed conventional treatment is a potential concern.90
Physicians integrating acupuncture into medical care need to be aware of referral options. Licensed acupuncturists are extensively trained in oriental colleges and develop considerable expertise in the TCM paradigm of diagnosis and treatment along with TCM herbal therapy, but lack a physician’s anatomical, pathophysiological, or allopathic differential diagnostic expertise. Therefore, it is appropriate to become familiar with the varying credentials and treatment styles of acupuncture practitioners prior to referring patients to them. Nevertheless, considering its potential benefits and low risk, it is reasonable to offer acupuncture as a treatment modality.
Discussion
Understanding the physiological basis for OMT, yoga, and acupuncture helps to demystify them and reinforces the appropriateness of their integration into primary care. The autonomic nervous system, especially its parasympathetic portion, provides a rationale for the beneficial effects of yoga, as well as many of the mind–body therapies such as meditation, which have not been covered in this article. Benson’s “relaxation response”, mediated via the vagus nerve, has been recognized for >40 years.91 Another example of overlapping physiological effects is the role of the muscle spindle in OMT and in yoga. Reduction of painful muscle spasm through these techniques can potentially eliminate the need for muscle relaxant medications with their attendant side effects. The impressive results of yoga in patients with osteoporosis, scoliosis, or rotator cuff tears offer an option that may substitute for pharmacological management in the former and for surgical treatment in the latter two conditions.
While published studies documenting objective physiological changes produced by the three CAM therapies examined in this article are quite compelling, the studies of their clinical efficacy are less so. As discussed by Earley and Luce17 with regard to OMT, it is difficult to utilize scientifically rigorous methods. Double-blind trials such as those used to evaluate a medication versus a placebo would be feasible in the case of herbal or nutritional supplements, but there are methodological difficulties associated with doing sham versions of OMT, yoga, or acupuncture. Also, most CAM treatments are tailored to the individual patient rather than adhering to any standardized protocols. Correlating the neurochemical changes produced by these techniques with their clinical outcomes may be a fruitful avenue for future research.
One reflection of the current lack of acceptance of these therapies, at least in the United States, is the fact that most of them (OMT is one prominent exception) are not covered by medical insurance. While the costs of acupuncture are not excessive compared with other interventions, they may exceed the financial resources of lower income individuals or families. Yoga has the advantage of frequently being done in group settings where the cost per individual is quite modest, and subsequent practice at home can utilize cassette, compact disk, or digital video. Similarly, various forms of meditation can be taught in group settings and continued at home without incurring undue expense.
Conclusion
It is unreasonable to expect all physicians to develop sufficient expertise in one or more of the manipulative, movement, or modality-based therapies to directly incorporate them into their daily medical practice, though opportunities for continuing education and training are certainly available. But it is entirely appropriate for them to be aware of the resources within their communities in which such treatments can be provided. Osteopathic, yoga, and acupuncture practitioners should be viewed as consultants who can provide valuable patient care services, and the primary care physician should cultivate these professional relationships. As with any other consultant, effective interpersonal communication and mutual respect will optimize patient care and outcome. Integrative Medicine combines the best aspects of modern Western Medicine (scientific rigor, pathophysiologic specificity, effectiveness in the treatment of acute disease) with those of CAM (focus on functional, mental, and spiritual well-being and effectiveness in chronic conditions, where conventional treatments have been less successful), enhancing the efficacy and outcome of both systems.
Acknowledgment
Special thanks to Kyle Silva, DO and Brian Lee, DO for consenting to and allowing us to use their photographic images in Figures 1 and 2.
Disclosure
The authors report no conflicts of interest in this work.
References
Weil A, Rees L. Integrative medicine imbues orthodox medicine with the values of complementary medicine. BMJ. 2001;322:119–120. | |
Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States: prevalence, costs, and patterns of use. N Engl J Med. 1993;328:246–252. | |
Wainapel SF, Fast A. Alternative Medicine in Rehabilitation: A Guide for Practitioners. New York: Demos Publishing; 2001. | |
DiGiovanna EL, Schiowitz S, Dowling DJ. An Osteopathic Approach to Diagnosis and Treatment. Philadelphia: Lippincott Williams and Wilkins; 2005. | |
Pettman EA. History of manipulative therapy. J Man Manip Ther. 2007;15(3):165–174. | |
Kaptchuk TJ, Eisenberg DM. Chiropractic: origins, controversies, and contributions. Arch Intern Med. 1998;158(20):2215–2224. | |
Snider KT, Snider EJ, DeGooyer BR, Bukowski AM, Fleming RK, Johnson JC. Retrospective medical record review of an osteopathic manipulative medicine hospital consultation service. J Am Osteopath Assoc. 2013;113(10):754–767. | |
Noll DR, Degenhardt BF, Morley TF, et al. Efficacy of osteopathic manipulation as an adjunctive treatment for hospitalized patients with pneumonia: a randomized controlled trial. Osteopath Med Prim Care. 2010;4:2. | |
Gamber RG, Shores JH, Russo DP, Jimenez C, Rubin BR. Osteopathic manipulative treatment in conjunction with medication relieves pain associated with fibromyalgia syndrome: results of a randomized clinical pilot project. J Am Osteopath Assoc. 2002;102(6):321–325. | |
Smith RK. One hundred thousand cases of influenza with a death rate of one-fortieth of that officially reported under conventional medical treatment [reprint of J Am Osteopath Assoc. 1920;20:172–175]. J Am Osteopath Assoc. 2000;100(5):320–323. | |
Licciardone JC, Brimhall AK, King LN. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskelet Disord. 2005;6:43. | |
Williams NH, Wilkinson C, Russell I, et al. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Pract. 2003;20:662–669. | |
Clinical Guideline Subcommittee on Low Back Pain. American Osteopathic Association guidelines for osteopathic manipulative treatment (OMT) for patients with low back pain. J Am Osteopath Assoc. 2010; 110(11):653–666. | |
Andersson GB, Lucente T, Davis AM, Kappler RE, Lipton JA, Leurgans S. A comparison of osteopathic spinal manipulation with standard care for patients with low back pain. N Engl J Med. 1999;341:1426–1431. | |
Prinsen JK, Hensel KL, Snow RJ. OMT associated with reduced analgesic prescribing and fewer missed work days in patients with low back pain: an observational study. J Am Osteopath Assoc. 2014; 114(2):90–98. | |
Wieting JM, Beal C, Roth GL, et al. The effect of osteopathic manipulative treatment on postoperative medical and functional recovery of coronary artery bypass graft patients. J Am Osteopath Assoc. 2013; 113(5):384–393. | |
Earley BE, Luce H. An introduction to clinical research in osteopathic medicine. Prim Care. 2010;37(1):49–64. | |
Savarese RG, Capobianco JD, Cox JJ. OMT Review: A Comprehensive Review in Osteopathic Medicine. 3rd ed. Spain: OMT; 2003. | |
Hodge LM. Osteopathic lymphatic pump techniques to enhance immunity and treat pneumonia. Int J Osteopath Med. 2012;15(1):13–21. | |
Mueller DM. The 2012–2013 influenza epidemic and the role of osteopathic manipulative medicine. J Am Osteopath Assoc. 2013; 113(9):703–707. | |
Chikly BJ. Manual techniques addressing the lymphatic system: origins and development. J Am Osteopath Assoc. 2005;105:457–464. | |
Licciardone JC, Buchanan S, Hensel KL, King HH, Fulda KG, Stoll ST. Osteopathic manipulative treatment of back pain and related symptoms during pregnancy: a randomized controlled trial. Am J Obstet Gynecol. 2010;202(1):43. e1–43. e8. | |
King HH, Tettambel MA, Lockwood MD, Johnson KH, Arsenault DA, Quist R. Osteopathic manipulative treatment in prenatal care: a retrospective case control design study. J Am Osteopath Assoc. 2003;103:577–582. | |
Fast A, Shapiro D, Ducommun E, Friedmann LW, Bouklas T, Floman Y. Low-back pain in pregnancy. Spine. 1987;12(4):368–371. | |
Osteopathic International Alliance. Osteopathic Medicine and Osteopathy. [Webpage] wp.oialliance.org/about-us/osteopathic-medicine-and-osteopathy/. Accessed February 4, 2015. | |
Frequently Asked Questions. American Osteopathic Association Website. Available from: http://www.osteopathic.org/osteopathic-health/about-dos/about-osteopathic-medicine/Pages/frequently-asked-questions.aspx. Accessed January 28, 2015. | |
Schierhorn C. Helping Hands? DOs Make Case for Teaching MDs OMT Basics. TheDO Website; 2013. Available from: http://thedo.osteopathic.org/2013/06/helping-hands-dos-make-case-for-teaching-mds-omt-basics/. Accessed February 4, 2015. | |
Greenman PE. Manual Medicine CME Series. Michigan State University College of Osteopathic Medicine website. Available from: http://com.msu.edu/CME/History.htm. Accessed February 4, 2015. | |
Postgraduate Course for Qualified Doctors. London College of Osteopathic Medicine Website. Available from: http://www.lcom.org.uk/course.html. Accessed February 4, 2015. | |
Iyengar BKS. Light on Yoga. New York: Schocken Books; 1966. | |
Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses. 2012;78:571–579. | |
Streeter CC, Whitfield TH, Owen L, et al. Effects of yoga versus walking on mood, anxiety, and brain GABA levels: a randomized controlled MRS study. J Altern Complement Med. 2010;16:1145–1152. | |
McKenzie R, Kubey C. 7 Steps to a Pain-Free Life. USA: Penguin; 2011. | |
Fishman LM, Wilkins AN. Functional Electrodiagnosis: Provocative Maneuvers in Electromyography. New York: Springer Publishing Company; 2010. | |
Fishman LM. Healing Yoga: Proven Postures to Treat Twenty Common Ailments – From Back Pain to Bone Loss, Shoulder Pain to Bunions. New York: WW Norton; 2015. | |
Fishman LM, Wilkins AN, Konnoth C, Schmidhofer S, Ovadia O, Rosner B. Yoga-based maneuver effectively treats rotator cuff syndrome. Top Geriatr Rehabil. 2011;27(2):151–161. | |
Fishman LM, Sherman KJ, Groessl EJ. Serial case reporting yoga for idiopathic and degenerative scoliosis. Global Adv Health Med. 2014;3(5):16–21. | |
Greendale GA, Huang MH, Karlamangla AS, Seeger L, Crawford S. Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc. 2009;57(9):1569–1579. | |
Fishman LM. Yoga for osteoporosis: a pilot study. Top Geriatr Rehabil. 2009;25(3):244–250. | |
Fishman LM, Small E. Yoga in the Treatment of Multiple Sclerosis. New York: Demos Medical Publishing; 2007. | |
Ahmadi A, Arastoo AA, Nikbakht M, Zahednejad S, Rajabpour M. Comparison of the effect of 8 weeks aerobic and yoga training on ambulatory function, fatigue and mood status in MS patients. Iran Red Crescent Med J. 2013;15(6):449–454. | |
Staples JK, Hamilton MF, Udda M. A yoga program for the symptoms of post-traumatic stress disorder in veterans. Mil Med. 2013; 178(8):854–860. | |
Libby DJ, Reddy F, Pilver CE, Desai R. The use of yoga in specialized VA PTSD treatment programs. Int J Yoga Therap. 2012;22:79–87. | |
Telles S, Singh N, Balkrisna A. Post traumatic stress symptoms and heart rate variability in Bihar flood survivors following yoga: a randomized controlled study. BMC Psychiatry. 2010;10:18. | |
Weintraub A. Yoga Skills for Therapists: Effective Practices for Mood Management. New York: WW Norton; 2012. | |
Philbil K. Yoga in grief management. Top Geriatr Rehabil. 2009; 25(3):244–250. | |
Yeung A, Slipp LE, Niles H, et al. Effectiveness of the relaxation response-based group intervention for treating depressed Chinese American immigrants: a pilot study. Int J Environ Res Public Health. 2014;11(9):186–201. | |
Chainani-Wu N, Weidner G, Purnell DM, et al. Changes in emerging cardiac biomarkers after an intensive lifestyle intervention. Am J Cardiol. 2011;108(4):498–507. | |
Cohen DL, Bloedon LT, Rothman RL, et al. Iyengar yoga versus enhanced usual care on blood pressure in patients with prehypertension to stage I hypertension: a randomized controlled trial. Evid Based Complement Alternat Med. 2011;2011:546428. | |
Cramer H, Posadzki P, Dobos G, Langhorst J. Yoga for asthma: a systematic review and meta-analysis. Ann Allergy Asthma Immunol. 2014;112(6):503. e–510. e. | |
de G R Hansen E, Innes KE. The benefits of yoga for adults with type 2 diabetes: a review of the evidence and call for a collaborative, integrated research initiative. Int J Yoga Therap. 2013;23:71–83. | |
Cramer H, Lauche R, Dobos G. Characteristics of randomized controlled trials of yoga: a bibliometric analysis. BMC Complement Altern Med. 2014;14:328. | |
Handschin C, Spiegelman BM. The role of exercise and PGC1alpha in inflammation and chronic disease. Nature. 2008;454(7203):463–469. | |
Fishman LM, Saltonstall E, Genis S. Understanding and preventing yoga injuries. J Int Assoc Yoga Ther. 2009;19(1):47–53. | |
Schaff T. Senior yoga: in and out of chairs. Top Geriatr Rehabil. 2012;28(3):223–237. | |
Prinster T. Yoga for Cancer: A Guide to Managing Side Effects, Boosting Immunity and Improving Recovery for Cancer Survivors. Rochester, VT: Healing Arts Press; 2014. | |
Cheng KJ. Neurobiological mechanisms of acupuncture for some common illnesses: a clinician’s perspective. J Acupunct Meridian Stud. 2014;7(3):105–114. | |
Menzel D. Fundamental Formulas of Physics. New York: Dover Books; 1960. | |
Helms JM. Acupuncture Energetics. New York: Thieme Publishers; 1995. | |
Pomeranz B. Acupuncture analgesia basic research. In: Stux G, Hammerschlag R, editors. Clinical Acupuncture, Scientific Basis. Berlin: Springer; 2001:1–28. | |
Dung HC. Anatomical features contributing to the formation of acupuncture points. Am J Acupunct. 1984;12:139–143. | |
Heine H. The morphological basis of the acupuncture points. Acupuncture. 1990;1:1–6. | |
Liu YK. The correspondence between some motor points and acupuncture loci. Am J Chin Med. 1975;3:347–358. | |
Melzak R. Trigger points and acupuncture points for pain. Correlations and implications. Pain. 1977;3:3–23. | |
Kuwazawa J. Experimental research on acupuncture effect on local muscle pain: VI. Effect of vasodilators and neuropeptide on recovery from the reduced twitch after tetanic stimulation. J Showa Med Assoc. 1987;47:15–22. | |
Daddona MM, Haldar J. Opioid modulation of oxytocin release from spinal cord synaptosomes. Neuroreport. 1994;5(14):1833–1835. | |
Vibes J. A-Delta fibers: the essential support of the acupunctural phenomenon? Acupuncture. 1990;1.5:100–102. | |
Chiang CY. Peripheral afferent pathway for acupuncture analgesia. Sci Sin B. 1973;16:210–217. | |
Le Bars D. Diffuse noxious inhibitory controls (DNIC) in animals and in man. Acupunct Med. 1991;9(2):47–56. | |
Chen XH, Han JS. Analgesia induced by electroacupuncture of different frequencies is mediated by different types of opioid receptors: another cross-tolerance study. Behav Brain Res. 1992;47(2):143–149. | |
Han JS. The role of central 5-hydroxytryptamine in acupuncture analgesia. Sci Sin B. 1979;22:91–104. | |
Cheng RS, Pomeranz B. Electroacupuncture analgesia could be mediated by at least two pain relieving mechanisms: endorphin and non-endorphin systems. Life Sci. 1979;25:1957–1962. | |
Liu H, Xu JY, Li L, et al. FMRI evidence of acupoints specificity in two adjacent acupoints. Evid Based Complement Alternat Med. 2013; 2013:5. | |
Claunch JD, Chan ST, Nixon EE, et al. Commonality and specificity of acupuncture action at three acupoints as evidenced by fMRI. Am J Chin Med. 2012;40(4):695–712. | |
Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012; 172(19):1444–1453. | |
Berman BM, Langevin HH, Witt CM, et al. Acupuncture for chronic low back pain. N Engl J Med. 2010;363(5):454–461. | |
Yuan JP, Purepong NM, Kerr DP, et al. Effectiveness of acupuncture for low back pain: a systematic review. Spine. 2008;33(23): E887–E900. | |
Ghoname EA, Craig WF, White PF, et al. Percutaneous electrical nerve stimulation for low back pain: a randomized crossover study. J Am Med Assoc. 1999;281(9):818–823. | |
Ghoname EA, White PF, Ahmed HE, Hamza MA, Craig WF, Noe CE. Percutaneous electrical nerve stimulation: an alternative to TENS in the management of sciatica. Pain. 1999;83:193–199. | |
Pach D, Yang-Strobel Y. Standardized versus individualized acupuncture for chronic low back pain: a randomized controlled trial. Evid Based Complement and Alternat Med. 2013;2013:125937. [Article ID 125937]. | |
Chien TJ, Liu CY, Hsu CH. Integrating acupuncture into cancer care. J Tradit Complement Med. 2013;3(4):234–239. | |
Rithirangsriroj K, Manchana T, Akkayagorn L. Efficacy of acupuncture in prevention of delayed chemotherapy induced nausea and vomiting in gynecologic cancer patients. Gynecol Oncol. 2015;136:82–86. | |
Bai L, Yan H, Li L, et al. Neural specificity of acupuncture stimulation at pericardium 6: evidence from an fMRI study. J Magn Reson Imaging. 2010;31:71–77. | |
Zhang X, Jin HF, Fan Y. Effects and mechanisms of transcutaneous electroacupuncture on chemotherapy-induced nausea and vomiting. Evid Based Complement Alternat Med. 2014;2014:6. | |
Linde K, Allais G, Brinkhaus B, Manheimer E, Vickers A, White AR. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;1:CD001218. | |
Linde K, Allais G, Brinkhaus B, et al. Acupuncture for tension-type headache. Cochrane Database Syst Rev. 2009;1:CD007587. | |
Chen HY, Shi Y, Ng CS, Chan SM, Yung KK, Zhang QL. Auricular acupuncture treatment for insomnia: a systematic review. J Altern Complement Med. 2007;13(6):669–676. | |
MacPherson H, Thomas K, Walters S, Fitter M. The York acupuncture safety study: prospective survey of 34,000 treatments by traditional acupuncturists. BMJ. 2001;323:486–487. | |
Ernst E, White AR. Prospective studies of the safety of acupuncture: a systematic review. Am J Med. 2001;110:481–485. | |
Tsuchigane S. European Acupuncture Licensing and Education. Tristate College of Acupuncture Website. Available from: http://www.tsca.edu/site/alumni-services/articles/european-acupuncture-licensing-and-education. Accessed March 1, 2015. | |
Benson H, Klipper MZ. The Relaxation Response. USA: Harper Collins; 1975. | |
Fishman, LM. Headstand in the treatment of rotator cuff syndrome – Sirsasana or surgery. J Int Assoc Yoga Ther. 2006;(16):137–145. | |
Fishman L, Saltonstall E. Yoga for Osteoporosis. New York: WW Norton & Company; 2010. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.