Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Integrated Disease Surveillance Response Practice and Associated Factors Among Health Professionals Working in Public Hospitals in West Hararghe Zone, Eastern Oromia, Ethiopia: Multi-Center Cross-Sectional Study
Authors Yusuf A , Oljira L , Mehadi A , Ayele BH
Received 21 March 2023
Accepted for publication 14 April 2023
Published 26 April 2023 Volume 2023:16 Pages 1111—1126
DOI https://doi.org/10.2147/JMDH.S411191
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Ahmednajash Yusuf,1 Lemessa Oljira,1 Ame Mehadi,2 Behailu Hawulte Ayele1
1School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia; 2School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Correspondence: Ame Mehadi, School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia, Tel +251919118839, Fax +251256668081, Email [email protected]
Background: Health workforces across all levels of the healthcare system are the main modulators in the effective implementation of disease surveillance system. However, their level of integrated disease surveillance response (IDSR) practice and determinant factors was hardly investigated in Ethiopia. This study determined the level of IDSR practice and associated factors among health professionals in the west Hararghe zone, eastern Oromia, Ethiopia.
Methodology: A multicenter facility-based cross-sectional study design was conducted between December 20, 2021, and January 10, 2022, among 297 systematically selected health professionals. Trained data collectors collected data using structured pretested self-administered questionnaires. The level of IDSR practice was assessed using six questions where each acceptable practice was given “ 1” and unacceptable “ 0”, with a total score of 0 to 6. Hence, a score above or equal to the median was categorized as good practice. Epi-data and STATA were used for data entry and analysis. A binary logistic regression analysis model with an adjusted odds ratio was used to determine the effects of independent variables on the outcome variable.
Results: The magnitude of good practice of IDSR was 50.17% (95% CI: 45.17, 55.17). Being married (AOR = 1.76; 95% CI: 1.01, 3.06), perceived organizational support (AOR = 2.14, 95% CI: 1.16, 3.94), good knowledge (AOR = 2.77, 95% CI: 1.61, 4.78), positive attitude (AOR = 3.30, 95% CI: 1.82, 5.98) and working in an emergency (AOR = 0.37, 95% CI: 0.14, 0.98) were significantly associated with the level of practice.
Conclusion: Only half of the health professionals had a good level of practice in integrated disease surveillance response. Marital status, working department, perceived organizational support, knowledge level, and attitude toward integrated disease surveillance were significantly associated with health professionals’ practice of disease surveillance. Thus, organizational and provider-targeted interventions should be considered to improve the knowledge and attitude of health professionals that improve integrated disease surveillance response practice.
Keywords: Integrated disease surveillance, response, practice, health professionals, public hospitals, Ethiopia
A Letter to the Editor has been published for this article.
Introduction
Surveillance, including early warning and epidemic intelligence, is an essential element to detect public health significance diseases and initiate management interventions rapidly.1 It is a base for the control and prevention of disease and the principal component delineated in the International Health Regulations (IHR) core capacity monitoring framework.1
Integrated Disease Surveillance and Response (IDSR) system is renowned, as a part of a health information system that organizes data to information for action, comprises health professionals, material, and database, and has been acknowledged as an effective strategy in the efforts to prevent and control diseases, especially epidemic‑liable diseases.2–4
The need for timeliness in reporting and response that requires effective linkages to those with authorized responsibility for disease control imposes additional requirements on health information systems.2,3 Delays in every step of reporting epidemic outbreaks and other diseases of public health priority concerns have been linked to poor implementation of the IDSR system.5 Many less developed and developing countries have been suffering to implement effective IDSR systems.5
Globally there is increasing growth of threat epidemics pose to health security and a significant disaster to the livelihood of people.6 Thus, there is a persistent need for a strategic solution for every public health system, particularly in African and other poor-income settings where infectious and epidemic-liable diseases are national priority diseases.3 In sub-Saharan Africa, due to the increasing number of infectious disease threats from time to time, effective ways of predicting outbreaks and planning for responses become critically important.7 Such activities need the functioning system of IDSR that involves the continuous scrutiny of disease on an individual, local, national, and international level and depends on health professionals practicing in the health-care sector.8
Health workforces are the main modulators in achieving effective IDSR system implementation and improvement across all levels of the healthcare system.9 This needs consistent availability of reliable, competent, and motivated professionals that monitor and designate the incidence and spread of diseases and events of public health significance as reportable, including individual reports whose signs demonstrate unknown, acute problems as well as clinical and laboratory diagnoses that meet standard case definitions for the diseases under surveillance.9–12
Despite being at risk of health security threats, the developing world like the African region is still facing challenges of insufficient numbers of trained personnel and high turnover.6,9–11 In African countries, particularly sub-Saharan, emerging and re-emerging infectious disease with pandemic potential continues to frustrate fragile health-care systems and challenged the continent.6 The IDSR strategy assisted countries in better monitoring and tracking planned time-bound targets as part of the improvement to the health-care system. However, after a decade of implementation, the level of IDSR practice among health professionals still needs improvement.1
In Jordan, the level of notifiable disease surveillance practice was 39.5% among physicians,13 while in Egypt, the mean score of IDSR practice of health professionals was 68.6%.14 However, in Nigeria, the level of IDSR practice was reported as 18.8%,15 while only 23.6% of health professionals knew half of the listed priority diseases under surveillance, and 40.3% of study participants did not know reporting procedure.16 In Zanzibar (Tanzania), only 30% of district surveillance staff and 17% of the staff of public primary health facilities were able to describe the IDSR strategy.17 In Zambia, good knowledge of disease surveillance was 45.5%,5 while in Kenya, only 27% of health professionals knew the IDSR strategy, and 92.9% were not aware of the number of priority diseases under surveillance.18
Available shreds of evidence show several organizational and individual-related factors associated with a poor level of IDSR practice. Lack of organizational support, poor knowledge, lack of time or workload, procedure complexity, inadequate resources, transport and communication challenges, perceptions, lack of regular data analysis and interpretation, absence of feedback, poor staff motivation, lack of staff, lack of training and weak supervision were factors linked to poor IDSR practice and reported to affect the overall implementation of the IDSR system.5,8,19–24 Like other resource-restricted countries, in Ethiopia, recurrent and unexpected disease outbreaks are continually confronting the public health system. The management of health consequences of natural and human-made disasters, emergencies, crises, wars, and conflicts is challenging the detection and response to outbreaks and continues to disrupt the already fragile healthcare system in the country. Due to these problems, the detection and response to outbreaks are becoming complicated.19,20,25
Currently, the surveillance system is operated in health facilities under the guidance of the Ethiopian public health institute through a dedicated structure from the facility to a higher level in all regions.25 Despite the achieved improvement through IDSR evidenced in Ethiopia, the overall implementation status of the system is not satisfactory.19,20,25 In Dawuro zone, Southwestern Ethiopia, 64.3% of health centers had a reporting system, of which 35.7% reported sending in surveillance reports by hand delivery,25 while the overall quality of IDSR service provision was good in 13% of health facilities in Tigray region, Northern Ethiopia.19
To find a possible solution for challenged surveillance in complex situations where resources are limited, studies are needed. However, to the best of the Authors’ knowledge, no study addressed the level of and factors affecting the practice of disease surveillance among health professionals in Ethiopia, particularly in eastern part. Yet there is a gap in the scientific evidence on the level of practice of disease surveillance and affecting factors among health professionals. Therefore, the purpose of this study was to determine the level of IDSR practice and associated factors among health-care professionals in the West Hararghe zone, eastern Oromia, Ethiopia.
Methods and Materials
Study Area and Period
The study was conducted in public hospitals of West Hararghe Zone. West Hararghe Zone is one of the 20 Zones in the Oromia Regional State. Chiro town, the capital of the zone, is located, 321 kilometers from Addis Ababa, the capital city of the country, in the eastern direction. By 2020, the Zone has a total population of 2,728,836. The zone has 15 districts and 2 city administrations. There are a total of seven public hospitals, 84 public health centers, and 482 health posts in the zone.26 There are two general hospitals; Chiro and Gelamso General Hospital, and five primary hospitals: Asebot, Hirna, Burka Dhintu, Badessa, and Daro Labu. Since the last three primary hospitals, Burka Dhintu, Badessa, and Daro Labu, did not have functional disease reporting systems until the development of the proposal, the study was conducted in Chiro and Gelamso General Hospitals and Asebot and Hirna Primary Hospitals from December 20, 2021, to January 10, 2022.
Study Design and Population
The study employed a multi-facility-based cross-sectional study design using an interviewer-administered questionnaire. All health professionals including Doctors, Nurses, Midwives, Laboratory technicians, Health officers, Integrated emergency surgical officers, Psychiatry professionals, Anesthetists, and Optometrists who met the inclusion criteria and gave consent were studied. All health professionals who were working in public hospitals, who were available during the data collection period, and who gave consent were included in the study, whereas, health professionals who were on annual leave during data collection time, not volunteers, not staff of the stated hospital, and less than six months after recruitment were not included in the study.
Sample Size Determination and Sampling Procedures
The sample size required for this study was calculated using the double population proportion formula:  with the assumptions of 63.5% prevalence of a good level of IDSR practice from the study in Nigeria27 and 74.8% of health professionals reported different factors associated with the DSR system,21 power of 80%, a design effect of 2 and 10% non-response rate. This resulted in a sample size of 257. When multiplied by a design effect of 2 yields 514. Since our total population (586) was less than 10,000, the sample size was adjusted using the correction formula and resulted in a sample size of 275. After adding a 10% non-response rate, the sample size was 303. Finally, 303 was the final sample size used for this study. However, data were collected from 297 health professionals who signed consent for this study.
with the assumptions of 63.5% prevalence of a good level of IDSR practice from the study in Nigeria27 and 74.8% of health professionals reported different factors associated with the DSR system,21 power of 80%, a design effect of 2 and 10% non-response rate. This resulted in a sample size of 257. When multiplied by a design effect of 2 yields 514. Since our total population (586) was less than 10,000, the sample size was adjusted using the correction formula and resulted in a sample size of 275. After adding a 10% non-response rate, the sample size was 303. Finally, 303 was the final sample size used for this study. However, data were collected from 297 health professionals who signed consent for this study.
Proportional allocation to size (PPS) was used for selecting study participants from each public hospital in West Hararghe. Accordingly, from the four functional hospitals in the zone, sample sizes were proportionally allocated to each hospital based on the number of health professionals in each hospital then the respondents were selected from each hospital by using simple random sampling. Accordingly, 101/195, 91/176, 53/103, and 58/112 health professionals were selected from Chiro General Hospital, Gelamso General Hospital, Asebot Primary Hospital, and Hirna Primary Hospital, respectively.
Data Collection Methods and Procedures
Four clinical nurses collected the data using a self-administered questionnaire that was adapted, standardized, and used in different studies.5,13,14,28 The questionnaire had five parts. The first part was the socio-demographic characteristics of health professionals, the second part was perceived organizational support factors, the third part was behavioral factors (knowledge and attitude of health professionals on IDSR), the fourth part was technical competency, technical complexity factors and perceived IDSR data quality factors, and the last part was IDSR practice of health-care professionals. The data collection was done at the workplace of study participants in each hospital simultaneously from December 20, 2021, to January 10, 2022.
Variables
The main outcome variable of this study was the level of integrated disease surveillance reporting practice, whereas, socio-demographic characteristics (sex, age, educational status, profession, working department, year of experience), perceived organizational factors (training, availability of report form, supervision, motivation, work overload, responsibility, accountability, the culture of data use), behavioral factors (knowledge, beliefs, and attitude of IDSR), perceived quality of IDSR data and perceived technical competency (design of data collection, use of technology, format friendly, complexity of report procedure) were independent variables.
Operational Definitions and Measurements
Attitude: It is a health professional’s beliefs, opinions, and agreement regarding IDSR whether positive or negative opinions. A scoring system was used in which the respondent’s correct and incorrect answers provided for the questions were allocated “1” or “0” points, respectively, and a score above or equal to the median was categorized as a positive attitude, whereas a score below the median as negative attitude towards IDSR.4,14 Knowledge of IDSR: this study defined knowledge of disease under surveillance, condition, and even notified, knowledge of reporting procedure and period and measured by six questions. Each correct answer was assigned “1” and an incorrect was “0” and summed up to give a total knowledge score ranging from 0 to 6 and used to classify the knowledge into two categories: good knowledge (if above or equal to the median) and poor knowledge (if below the median).4,5,14 Practice of IDSR: is the act of identification of cases, investigation, registration, notification, and reporting of priority disease data to relevant bodies. It was measured using six questions, where each acceptable or correct practice was given a score of “1” and unacceptable was assigned a score of “0”, hence the total score of IDSR practice ranged from 0 to 6. Since data were not normally distributed, the median was used for the classification of practice that scored above or equal to the median categorized as good practice whereas a score below the median was the poor practice of IDSR.4,13,14 Perceived organizational support: is defined as any factor associated with organizational support related to surveillance activity of health-care professionals and assessed by 7 computed questions with a total score range of 0 to 7. Based on the respondent’s correct or incorrect answer to each question, a score of “1” was allotted for each acceptable support and “0” for unacceptable support. Then, the total score above or equal to the median was categorized as good organizational support, whereas a score below the median as poor organizational support. Perceived quality of IDSR data: in this study defined in terms of data accuracy, completeness, and timeliness of the report and measured using five-point Likert scale questions scored out of 25. A total score of 20 and above was taken as good, and a score less than 20 was considered poor.19 Perceived technical competency of IDSR: is defined in terms of data collection design, use of technology for data entry, analysis, and format friendly and measured by Five Point Likert scale questionnaire. A total of six questions were computed to construct the technical competency factor and scored out of 30, a score of 24 and above was reported as good technical competency, and a score less than 24 was reported as poor technical competency.4
Data Quality Management
Data were collected using a standardized self-administered questionnaire after adequate training was given to the data collectors and supervisors on data collection tools and procedures. The standard questionnaire was prepared in English. The tool was pre-tested on 5% of the sample size in Haramaya Hospital and appropriate amendments were done before the actual data collection. A content validity test was applied by checking the coverage of the content listed conceptual framework. Data collectors were clinical nurses and supervisors were professional nurses and/or public health officers. Both data collectors and supervisors were selected from other health institutions not under study. Two days of training were given to the data collectors on the data collection tool and the data collection procedures. Supervisors and the principal investigator closely supervised the data collection process at each hospital. The collected data were checked for completeness of each questionnaire at the end of each day. Two data clerks did double data entry and crosschecked the consistency of the entered data by comparing the two separately entered data into Epidata and then exporting to STATA for analysis.
Data Processing and Analysis
After data collection, each questionnaire was checked for completeness and coded before entry into the software, then entered into Epidata version 3.1 and exported to STATA version 16.0, cleaning and analysis were done accordingly. Frequency, percentage, and descriptive summaries were computed for univariate variables. Binary logistic regression was carried out to identify factors associated with IDSR practice. The goodness of model fitness was checked by the Hosmer-Lemeshow test. Multi-collinearity tests were carried out to see the correlation between independent variables and checked by using the standard error and collinearity statistics (variance inflation factors >10 and standard error >2 were considered as suggestive of the existence of multi co-linearity). Variables with a p-value less than 0.25 in the bivariate binary logistic regression analysis were considered for further multivariate binary logistic regression analysis to control for possible confounding factors. In the multivariate binary logistic regression, the Odds ratio along with 95% CI was used to present the association, and statistical significance was declared at a p-value <0.05. The finding was described and presented using tables, charts, and graphs.
Results
Socio-Demographic Characteristics of the Study Participants
Out of 303 health professionals recruited for this study, 297 participated with a response rate of 98.01%. The median age of respondents was 28 (IQR: 5) years while 30.64% of respondents were between the age of 25–28 years. The majority of the study participants, 61.95%, were males. More than half, 52.53% were nurses in the profession and 35.69% were working in the inpatient department. About a third, 32.00%, of the respondents, reported experience in an administrative position/role and 42.09% had worked for more than five years (Table 1).
 |
Table 1 Socio-Demographic Characteristics of the Respondents in West Hararghe Zone, Oromia, Eastern Ethiopia, 2022 (n = 297) |
Perceived Organizational Support
In this study, perceived organizational support related to IDSR practice was also assessed. Accordingly, the presence of training on IDSR within 12 months preceding data collection time, availability of adequate IDSR reporting formats, presence of a system of recognition or reward system for good performance, accountability for reporting system or a penalty for not reporting and receiving feedback for the practice of IDSR from the zonal or regional health bureau was reported by 39.06%, 71.72%, 54.21%, 64.31%, and 65.66% of the study participants, respectively. The computed overall good perceived organizational support for IDSR practice was reported by 62.96% of the study participants (Figure 1).
 |
Figure 1 Perceived organizational support for IDSR practice among health professionals in public hospitals in West Hararghe zone, Oromia, Eastern Ethiopia, 2022. |
Knowledge of IDSR
Out of 297 study participants, 69 (23.23%) knew the exact figure of reportable disease. More than two-fifth of the participants, 43.43% knew reporting timeliness of the disease/conditions both immediately and weekly. The overall good level of IDSR knowledge of health professionals was 52.52% (Figure 2).
 |
Figure 2 Level of IDSR knowledge among health professionals working in public hospitals in West Hararghe zone, Oromia, Eastern Ethiopia, 2022. |
Attitude of Health Professionals on IDSR
Out of the study participants, 94.28% agreed with the use of surveillance to detect epidemics, whereas 86.53% agreed with the importance of surveillance. The convenience of the surveillance system was reported by 68.01% of study participants. More than three-fifths (61.95%) of health professionals agreed with the responsibility of reporting by service providers, while 29.63% of participants agreed on the importance of reporting the case despite the difficulty in confirming it. More than four-fifths, 80.13%, of the study participants answered that reporting notifiable diseases was mandatory, irrespective of other work. Overall, 68.01% of health professionals had a positive attitude toward IDSR (Table 2).
 |
Table 2 Health Professionals’ Attitude on IDSR in West Hararghe Zone, Oromia, Eastern Ethiopia, 2022 |
Perceived Technical Competency, Technical Complexity, and Quality of IDSR Data
Out of 297 study participants, 50.17%, 59.25%, 63.97% and 55.90% of respondents reported the presence of well-designed surveillance data collection and reporting formats, the ability of trained staff to fill out IDSR formats, the presence of skilled human resources to collect health data, and the presence of a friendly format that is easy for reporting results and to visualize, respectively.
The presence of IDSR reporting formats, tally sheets, and registers common tools for data collection and reporting was reported by 69.36% of health professionals, while the presence and usage of appropriate technology for IDSR data analysis, transfer, and presentation was reported by 47.48% of study participants. In this study, the computed perceived technical competency of IDSR was good among 27.27% of health professionals.
Perceived similarity of reported data from their facility and the data in facility registers was reported by 192 (64.65%) of study participants, while 58.92% of respondents reported perceived similarity of immediate and weekly reported data and the monthly report of the same cases. Completeness of report and data and timeliness of reporting in their working facilities were perceived by 69.02%, 62.96%, and 65.31% of the respondents, respectively. Moreover, overall perceived good quality of IDSR data was reported by 45.45% of health professionals (Table 3).
 |
Table 3 Perceived Technical Competency, Technical Complexity and Quality of IDSR Data Among Health Professionals in West Hararghe Zone Public Hospitals, Oromia, Eastern Ethiopia, 2022 |
Level of IDSR Practice with Its Components
Out of 297 health professionals who participated in this study, 50.17% (95% CI: 45.17–55.17) have good practice of IDSR (Figure 3). The computed overall good perceived organizational support for IDSR practice was reported by 62.96% of the study participants. The overall good level of IDSR knowledge of health professionals was 52.52% and 68.01% of health professionals had a positive attitude toward IDSR. Moreover, overall perceived good quality of IDSR data was reported by 45.45% of health professionals, whereas only 27.27% of health professionals reported good perceived technical competency on IDSR (Figure 4).
 |
Figure 3 Magnitude of good level of IDSR practice among health professionals in public hospitals of West Hararghe zone, Oromia, Eastern Ethiopia, 2022. |
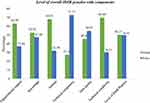 |
Figure 4 Level of overall IDSR practice with components among health professionals in public hospitals in West Hararghe zone, Oromia, Eastern Ethiopia 2022. |
Factors Associated with IDSR Practice
After running the Chi-square test, marital status (X2=8.04, p = 0.01), profession (X2=19.78, p = 0.01), salary (X2=23.64, p = 0.00), perceived organizational support (X2= 17.05, p = 0.000), level of IDSR knowledge (X2=23.22, p = 0.000), the attitude of providers on IDSR (X2=26.42, p = 0.000), perceived technical competency (X2=8.76, p = 0.003), perceived technical complexity (X2=18.75, p = 0.000), and surveillance data quality (X2=18.13, p = 0.000) were significantly associated with providers practice of IDSR.
For this study, binary logistic regression was fitted. During bivariable analysis, eight variables (including marital status, working department, organizational support factors, level of IDSR knowledge, attitude toward IDSR, technical competency, perceived surveillance data quality, and technical complexity) with a p-value <0.25 were included in multi variable analysis (Table 4).
 |
Table 4 Bivariable Binary Logistic Analysis of Factors Associated with IDSR Practice Among Health Professionals Working at Public Hospitals in West Hararghe Zone, Oromia, Eastern Ethiopia, 2022 |
During multivariate analysis, only five variables including, marital status, working department, perceived organizational support, knowledge of IDSR, and attitude of health professionals on IDSR showed significant association with IDSR practice at p-value <0.05.
Accordingly, the odds of good practice of IDSR was 1.76 (AOR = 1.76, 95% CI: 1.01, 3.06) times higher among married study participants compared to those not married. Similarly, those who had perceived good organizational support were 2.14 (AOR = 2.14, 95% CI: 1.16, 3.94) times more likely to practice IDSR compared with their counterparts. Likewise, those who have good knowledge of IDSR were 2.77 (AOR = 2.77, 95% CI: 1.61, 4.78) times more likely to better practice IDSR compared with those who had poor IDSR knowledge. Health professionals who had a positive attitude were 3.30 (AOR: 3.30, 95% CI: 1.82, 5.98) times more likely to better practice IDSR compared to those who had a negative attitude. However, those who worked in the Emergency department were 63% (AOR: 0.37, 95% CI: 0.14, 0.98) less likely to practice IDSR compared with those who worked in the outpatient department (Table 5).
 |
Table 5 Multivariable Binary Logistic Analysis of Factor Associated with IDSR Practice Among Health Professionals Working in Public Hospitals in West Hararghe, Oromia, Eastern Ethiopia, 2022 |
Discussion
This study was done to identify the level of IDSR practice and associated factors among health professionals. Accordingly, half of the health professionals had a good level of IDSR practice. This finding is higher than the study done in Jordan13 and the Eastern part of Nigeria21 in which only 39.50% and 25.20% of health-care providers had a good level of IDSR practice, respectively. On the contrary, the result of this study showed a lower level of IDRS practice compared to the study conducted in Egypt,14 Nigeria,27 Kingdom of Bahrain8 and in the Tigray region of Ethiopia,19 which revealed 68.70%, 63.50%, 80.01%, and 80.40% good level of IDSR practice, respectively. The reason for this discrepancy might be knowledge differences, low organizational support, the country’s educational curriculum, and the complexity of reporting systems and study areas.8,14
Health professionals who had good perceived organizational support were more than two times (AOR: 2.14) more likely to have good IDSR practice compared to those who had poor organizational support. This was in line with a Nigerian study, in which health-care workers who had received training on disease surveillance and those who received regular feedback for their reporting practice were three (AOR: 3.41) and four (AOR: 4.12) times more likely to report neglected tropical diseases and had good IDSR practice compared to their counterparts, respectively.27 This might be because organizational support like training was one supportive package of IDSR implementation indicating that effective training closes the knowledge gap and therefore improves the attitude and practice of health-care workers in disease surveillance and reporting.25 However, a contrasting study finding was reported from South Africa29 revealing no significant association between training on disease surveillance and notification (DSN) (OR: 1.16) and IDSR practice.
Regarding the level of IDSR knowledge, health-care professionals who had good knowledge were about three times (AOR: 2.77) more likely to have good IDSR practice compared with those who had poor knowledge. This is consistent with studies conducted in Nigeria16,21 and Egypt,14 in which knowledge of the reportable disease, the reporting formats, the reporting period and frequency, and the purpose of surveillance tended to affect the level of IDSR practice. This indicates knowledge of the disease reporting system is essential for IDSR practice, which plays a crucial role in the prevention and control of infectious diseases.30
Moreover, health professionals who had a positive attitude were 3.30 times (AOR: 3.30) more likely to practice IDSR. This finding is in agreement with the study conducted in Egypt.14 This indicates positive attitudes toward the IDSR system signifies willingness to participate in disease surveillance, helps maintain a good level of practice, and is an enabling factor for disease surveillance and reporting practice.14 However, the current study is in contrast with the study conducted in South Africa29 and Jordan.13 The discrepancy might be due to differences in methodology, training, and level of awareness.14
Finally, the odds of having a good level of IDSR practice was 63% (AOR: 0.37) less likely among health professionals working in the emergency department compared with those who were working in the outpatient department. This finding is in agreement with a study conducted in Egypt.14 This might be due to the high flow of patients and workload in the emergency department. However, our finding is in contrast to the study finding in South Africa.29 The possible reason might be attributed to the difference in the method of study, time, and population difference.31
The current study was the first of its kind in Ethiopia, particularly in the eastern part to assess health professionals’ level of IDSR practice. The study focused on a little-investigated but very important theme and provides future direction for national studies. It presented a wide scope since all relevant health-care workers that might be engaged in IDSR implementation at any time when the need arise were included. Further, the study based on primary data examined the level of IDSR practice using a standardized tool and implemented a good measurement process. Exposures of multiple variables measured at a time were also tested with outcome variables.
Despite all these merits, the study finding should be interpreted with the following limitations; the absence of local and national studies limited a comparison, the cross-sectional nature of the study design, and the study is the self-reported information that is prone to social desirability bias that might lead to an over-estimation of the level of IDSR practice among health-care workers.
Conclusions
In this study, only half of the health professionals reported a good level of IDSR practice. Among many factors expected to predict the level of IDSR practice marital status, working department, well-perceived organizational support, knowledge, and attitude of IDSR were significant factors associated with the level of IDSR practice among health-care professionals.
Awareness, information, education, and communication programs concerning the surveillance system and its importance for health-care providers should be provided on a regular basis to build capacity for IDSR practice. Health professionals should comply with the national standard instruction manual, principles, and guidelines on integrated disease surveillance developed for health facilities. Organizational support like training, supportive supervision, and feedback to all individuals working in the health institution on integrated disease surveillance and response should be strengthened at the health facility level. The MOH strongly advised developing ongoing evaluation mechanisms of IDSR practice since practices are unlikely to remain static. Furthermore, the MOH should also ensure and secure resource needs for the provision of regular IDSR training targeting all health-care workers. Finally, another study with mixed method or qualitative or comparative should be conducted.
Abbreviations
AOR, Adjusted Odd Ratio; CHMS, College of Health and Medical Science; COR, Crude Odd Ratio; DSN, Disease Surveillance and Notification; EPHI, Ethiopian Public Health Institute; MOH, Ministry of Health; IDSR, Integrated Disease Surveillance and Response; WHO, World Health Organization.
Data Sharing Statement
All datasets pertinent to the work are included within the article. Detailed raw data analyzed for the work reported can be available from the corresponding author upon reasonable request.
Ethical Consideration
This study was conducted according to the Helsinki Declaration. Ethical clearance was obtained from the Institutional Health Research and Ethics Review Committee (IHRERC) of Haramaya University, College of Health and Medical Science with ethics number: HUSM_2022_857. Before data collection, an official support letter obtained from Haramaya University College of Health and Medical Sciences was submitted to the West Hararghe zone health bureau and each hospital under study. Permission to conduct the study was secured from the head of each hospital. Each study participant provided a written voluntarily signed consent after the purpose, risk, and benefit of the study were explained. All COVID-19 standard safety principles were implemented strictly throughout the data collection process.
Acknowledgments
The authors expressed their heartfelt gratitude and humble appreciation to Haramaya University for giving ethical approval. All study respondents, data collectors, and supervisors who made this study feasible were also grateful. Finally, all cooperative staffs of each hospital as well as all individuals who contributed directly or indirectly to the accomplishment of the study were thankful.
Author Contributions
All authors made substantial intellectual contributions to the work reported, whether in the conception, study design, execution and acquisition of data, analysis, and interpretation or all of these parts; participated in drafting the manuscript, critical review or revision of the article; have read and approved the final version; selected and settled the journal to which the article submitted; and approved accountability in all aspects of the work reported.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Integrated Disease Surveillance and Response Technical Guidelines: Booklet Three: Sections 4, 5, 6, and 7. World Health Organization. Regional Office for Africa; 2019.
2. World Health Organization. Framework Standards for Country Health Information Systems.
3. Kasolo F, Yoti Z, Bakyaita N, et al. IDSR as a platform for implementing IHR in African countries. Biosecur Bioterror. 2013;11(3):163–169. doi:10.1089/bsp.2013.0032
4. Chime OH, Ogugua IJ, Obionu IM, et al. Assessment of knowledge and practice of disease surveillance and notification among health workers in private hospitals in Enugu State, Nigeria. Nigerian J Med. 2021;30(6):693–700. doi:10.4103/NJM.NJM_132_21
5. Haakonde T, Lingenda G, Munsanje F, Chishimba K. Assessment of factors affecting the implementation of the integrated disease surveillance and response in public health care facilities – the case of Rufunsa District, Zambia. Divers Equal Health Care. 2018;15(1):15–22.
6. World Health Organization. WHO Health emergencies programme in the African Region: annual report 2016; 2017.
7. Mremi I, George J, Rumisha SF, Sindato C, Mboera LE, Kimera SI. Twenty years of integrated disease surveillance and response in sub-saharan Africa: challenges and opportunities for effective management of infectious disease epidemics. One Health Outlook. 2020;2. doi:10.1186/s42522-020-00017-4
8. Al-Hashimi DA, Al-Roomi K, Al-Sayyad AS. Reasons for under-reporting of notifiable communicable diseases in the Kingdom of Bahrain: health-centers based survey. J Bahrain Med Soc. 2014;25(2):75–79. doi:10.26715/jbms.25_2_3
9. Ng’etich AK, Voyi K, Kirinyet RC, Mutero CM, Zhang H-L. A systematic review on improving implementation of the revitalised integrated disease surveillance and response system in the African region: a health workers’ perspective. PLoS One. 2021;16(3):e0248998. doi:10.1371/journal.pone.0248998
10. Fall IS, Rajatonirina S, Yahaya AA, et al. Integrated disease surveillance and response (IDSR) strategy: current status, challenges and perspectives for the future in Africa. BMJ Global Health. 2019;4(4):e001427. doi:10.1136/bmjgh-2019-001427
11. Wolfe CM, Hamblion EL, Dzotsi EK, et al. Systematic review of Integrated Disease Surveillance and Response (IDSR) implementation in the African region. PLoS One. 2021;16(2):e0245457. doi:10.1371/journal.pone.0245457
12. Adokiya MN, Awoonor-Williams JK, Beiersmann C, Müller O. Evaluation of the reporting completeness and timeliness of the integrated disease surveillance and response system in northern Ghana. Ghana Med J. 2016;50(1):3–8. doi:10.4314/gmj.v50i1.1
13. Abdulrahim N, Alasasfeh I, Khader YS, Iblan I. Knowledge, awareness, and compliance of disease surveillance and notification among Jordanian Physicians in residency programs. INQUIRY. 2019;56:0046958019856508. doi:10.1177/0046958019856508
14. Faten M, Rabie SSA, Amany H. Awareness and practice of health care providers towards communicable disease surveillance in Assuit University Hospitals - Egypt. Egyptian J Commun Med. 2020;38(1):22–32.
15. Awunor N. Awareness, perception and preferences of resident doctors toward disease surveillance and notification in a tertiary health facility in Edo State, Nigeria. Therap Adv Drug Safety. 2019;2019:120.
16. Aniwada EC, Obionu CN. Disease surveillance and notification, knowledge and practice among private and public primary health care workers in Enugu State, Nigeria: a comparative study. J Adv Med Med Res. 2016;13:1–10.
17. Saleh F, Kitau J, Konradsen F, Mboera LE, Schiøler KL. Assessment of the core and support functions of the integrated disease surveillance and response system in Zanzibar, Tanzania. BMC Public Health. 2021;21(1):1–12. doi:10.1186/s12889-021-10758-0
18. Francis FM, Muchiri EM, Kamari KM. Knowledge, attitudes and implementation of integrated disease surveillance and response programme by health workers: a survey of selected health facilities in Meru County of Kenya. Xenobiotica. 2019;49(12):1396–1402. doi:10.1080/00498254.2019.1581301
19. Ajemu KF, Desta AA, Bezabih NM, Araya AA, Hilawi EH. Level and predicators of quality of integrated disease surveillance and response for infectious disease in Tigray, Northern Ethiopia: cross-Sectional Study; 2020.
20. Alemu T, Gutema H, Legesse S, Nigussie T, Yenew Y, Gashe K. Evaluation of public health surveillance system performance in Dangila district, Northwest Ethiopia: a concurrent embedded mixed quantitative/qualitative facility-based cross-sectional study. BMC Public Health. 2019;19(1):1–9. doi:10.1186/s12889-019-7724-y
21. Iwu AC, Diwe KC, Merenu IA, Duru CB, Uwakwe KA. Assessment of disease reporting among health care workers in a South Eastern State, Nigeria. Int J Commun Med Public Health. 2016;3(10):2766–2774. doi:10.18203/2394-6040.ijcmph20163359
22. Lafond KE, Dalhatu I, Shinde V, et al. Notifiable disease reporting among public sector physicians in Nigeria: a cross-sectional survey to evaluate possible barriers and identify best sources of information. BMC Health Serv Res. 2014;14(1):1–9. doi:10.1186/s12913-014-0568-3
23. Mairosi N, Tshuma C, Juru T, Gombe N, Shambira G, Tshimanga M. Evaluation of notifiable disease surveillance system in Centenary District, Zimbabwe, 2016. Open J Epidemiol. 2017;7(3):251–261. doi:10.4236/ojepi.2017.73019
24. Phalkey RK, Kroll M, Dutta S, et al. Knowledge, attitude, and practices with respect to disease surveillance among urban private practitioners in Pune, India. Glob Health Action. 2015;8(1):28413. doi:10.3402/gha.v8.28413
25. Begashaw B, Tesfaye T. Assessment of integrated disease surveillance and response implementation in special health facilities of Dawuro Zone. J Anesthesiol. 2016;4(3):11–15. doi:10.11648/j.ja.20160403.11
26. Central statistical Authority of Ethiopia. Ethiopian Population and Housing Census Survey. Addis Abeba, Ethiopia: Central statistical Authority of Ethiopia; 2016.
27. Emeto DC, Salawu AT, Salawu MM, Fawole OI. Recognition and reporting of neglected tropical diseases by primary health care workers in Ibadan, Nigeria. Pan Afr Med J. 2021;38:224.
28. World Health Organization. Protocol for the Assessment of National Communicable Disease Surveillance and Response Systems: Guidelines for Assessment Teams. World Health Organization; 2001.
29. Benson FG, Levin J, Rispel LC, Gibney K. Health care provider compliance with the notifiable diseases surveillance system in South Africa. PLoS One. 2018;13(4):e0195194. doi:10.1371/journal.pone.0195194
30. Osagiede EF, Isah EC, Ozomata EA, et al. Assessment of knowledge and materials availability in the implementation of integrated diseases surveillance and responses in public facilities in South-south Nigeria. Nigerian J Med. 2020;29(1):11–19. doi:10.4103/1115-2613.284870
31. Matsoso MP, Strachan B. Human resources for health for South Africa: HRH strategy for the health sector 2012/13-2016/17. South Afr Health Rev. 2011;2011(1):49–58.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
