Back to Journals » International Journal of Women's Health » Volume 10
Initiation and continuation of breastfeeding among Jordanian first-time mothers: a prospective cohort study
Authors Al dasoqi K, Safadi R , Badran E , Basha AS , Jordan S, Ahmad M
Received 30 May 2018
Accepted for publication 20 August 2018
Published 5 October 2018 Volume 2018:10 Pages 571—577
DOI https://doi.org/10.2147/IJWH.S175850
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Khadeejeh Al dasoqi,1 Reema Safadi,1 Eman Badran,2 Asma Sa’d Basha,3 Sue Jordan,4 Muayyad Ahmad5
1Department of Maternal and Child Health Nursing, School of Nursing, University of Jordan, Amman, Jordan; 2Department of pediatrics, School of Medicine, University of Jordan, Amman, Jordan; 3Department of Obstetrics and Gynecology, School of Medicine, University of Jordan, Amman, Jordan; 4Department of Nursing, Swansea University, Swansea, UK; 5Clinical Nursing Department, School of Nursing, University of Jordan, Amman, Jordan
Objective: This study aimed to examine the rates of initiation and continuation of breastfeeding (BF) and their relationship with mothers’ sociodemographic, obstetric, neonatal, and medical interventions.
Methods: Data were collected from 199 first-time Jordanian mothers using medical records, face-to-face interviews within 24 hours of birth, and two telephone interviews at 6 weeks and 6 months after birth.
Results: The rate of BF initiation within the first 4 hours after birth was only 13%. The rate of exclusive BF at 6 weeks was 25.5%, and this rate dropped to 2.1% at 6 months. Mothers who initiated BF before discharge were older, were employed, had normal vaginal birth, and had undergone antenatal or after-birth BF education. Infants’ birth weight or gender was not interrelated with BF initiation. There was no relationship between initiation and continuation of BF and use of medications for labor pain or for induction/augmentation. The only significant relationship was found between the dose of ergometrine and BF failure and painful BF at 6 weeks.
Conclusion: There is a need for increasing health care providers and public awareness about the role of intrapartum medications and procedures on the initiation and continuation of BF at 6 weeks and 6 months after birth.
Keywords: exclusive breastfeeding, ergometrine, obstetric procedures, intrapartum medication, Jordan
Introduction
Breastfeeding (BF) is crucial for both infant and maternal health.1–3 Early initiation of BF and exclusive BF (EBF) for the first 6 months postpartum are strongly recommended.1 Rate of BF initiation is suboptimal worldwide and in Jordan.2–4 A higher rate of EBF has been documented in developing countries.2,5 Decisions to initiate and continue BF are complex and affected by several factors.5 These include sociodemographic characteristics of mothers,3,5–11 obstetric and neonatal factors,12–16 as well as intrapartum interventions.17–24 Sociodemographic characteristics of mothers influence initiation of BF and optimal EBF. These include mothers’ age,6 education,7 income,8,9 and employment.10,11 Successful BF is also influenced by mode of birth.7,12 For instance,7 uncomplicated spontaneous vaginal birth – where there is immediate skin-to-skin contact with infant – improves the chances of BF initiation and continuation,7 whereas emergency and elective cesarean section births are documented to negatively affect the success of BF.12 Evidence from observational studies suggests that BF may be affected by medications administered during birth, including analgesics (opioids such as pethidine and epidural fentanyl),17–21 oxytocin for induction or augmentation of vaginal birth,22–24 and uterotonics for the prophylactic management of the third stage of labor (ergometrine).23,24
The aims of this paper are to examine the relationship between BF initiation and continuation of EBF until 6 weeks and 6 months postpartum on the one hand and the following factors on the other: 1) sociodemographic variables (age, education, income, and employment); 2) obstetric and neonatal variables (mode of birth, newborn gender, and newborn weight); and 3) dose of medications given during birth (pethidine, fentanyl in epidural anesthesia, oxytocin, and active management of third stage of labor). Identifying the predictors of successful BF may facilitate health care professionals in setting policies and planning practices and educational programs that enhance BF.
Methods
Design and setting
A longitudinal prospective cohort design was used. Data were collected between September 2013 and April 2015 from the postpartum units at two major hospitals in Amman, Jordan. These two hospitals are: Jordan University teaching hospital and the Islamic private hospital. These two hospitals provide maternal and child healthcare services for a large population from various socio-demographic backgrounds.
Participants
First-time healthy mothers of healthy full-term singleton infants, selected from labor records with the help of the liaison nurse/midwife, were invited to enroll in the study. The inclusion criteria were that all participants be healthy first-time postnatal mothers who gave birth with a term pregnancy (37–42 weeks) and had received initial postnatal care in the first 24–48 hours after birth. The excluded participants were mothers with chronic illnesses (eg, diabetes, asthma), mothers with multiple pregnancies, or mothers of infants with congenital anomalies or malformations (eg, cleft lip, cleft palate and neural tube defect). The exclusion of these mothers was because maternal illnesses, multiple pregnancies, and infants’ health status may influence the initiation and continuation of BF.25
Recruitment
Recruitment of mothers was facilitated by a liaison nurse/midwife at the postnatal ward, who confirmed to the research assistant that eligible mothers are fully conscious, are oriented, and in stable physical status to communicate with the research assistant. The research assistant approached a mother and invited her to participate. This process continued until the desired number for the sample size (203) was reached.
Sample size
Power analysis demonstrated that a sample size of at least 118 mothers is required. This would be sufficient to provide 80% power. These numbers provide an overall significance level of 0.05, based on two pairwise tests, each at the 0.05 significance level.26
Data collection procedures and tools
Four structured tools for data collection were developed, tested, and validated. These included the following: 1) medical records information sheet; 2) structured questionnaire for the face-to-face interview within 24 hours of birth; and structured questionnaire for the telephone interviews at 3) 6 weeks; and 4) 6 months after birth. The medical records tool included demographic information (age, education, income, and employment), obstetric and neonatal information (ie, mode of birth, medications and doses of medications, infant gender, infant weight, and Apgar score). One of the coauthors is an obstetrics–gynecology consultant, who verified the documentation of doses of medications administered intrapartum. The second tool, a structured questionnaire, was used in face-to-face interviews by trained research assistants, who were trained on how to collect the data using this tool. This interview was conducted within 24 hours of birth and included questions related to demographics (education level of the mother and the husband, employment status during pregnancy, the intention to breastfeed, and the length of maternity leave), and BF practices (timing of initiation of BF in hours within the first 24 hours after birth). Tools 3 and 4 were used for the 6-week and 6-month telephone interviews. These questionnaires included 40 open- and closed-ended questions with multiple responses, to assess BF continuation and feeding practices. Examples of these questions are as follows: “during the past 6 weeks, mention any BF problems you faced)”, and “how do you describe the pattern of BF you provide to your baby (full, partial, or bottle feeding?)” (options were given). Data collection tools were piloted with a group of 15 first-time mothers as a field test at the teaching hospital in Amman, and no changes were needed.
Ethical considerations
Ethical approvals were obtained from the Research Committees at the School of Nursing and The University of Jordan and the two targeted hospitals (namely, University of Jordan hospital and the Islamic hospital). Permissions to collect data from medical records were obtained from the hospital administration and participants. All mothers were informed about the purpose, benefits, and risks of participation, and they gave written informed consent in the Arabic language. They were told that participation was voluntary, and declining engagement did not negatively influence the health care provision. Confidentiality and anonymity were assured. Data from medical records, contact numbers, personal information, and completed questionnaires were saved in a locked cabinet, and only the primary investigator had access to these data files.
Statistical analyses
Statistical analyses of the data were conducted using SPSS version 21.27 Data were explored with univariate and bivariate techniques, chi-squared test, and Spearman rho correlation. The variables studied for correlation were examined with the appropriate correlation statistics based on their level of measurement.
Results
Data on 225 first-time mothers were obtained from admission records. Face-to-face first interviews were conducted with 199 mothers who met the inclusion criteria (26 mothers were excluded because they gave birth to preterm infants with <37 weeks’ gestation). Because this study followed a longitudinal design, a few participants dropped out over time. The number of mothers who were retained in the 6-week and 6-month interviews after birth was 196 and 194 mothers, respectively, yielding an attrition rate of 0.9% during the period from 6 weeks to 6 months.
The mean ± SD (range) of the age of the mothers at childbirth was 26±5.05 (18–43) years. About 59% of the mothers and their spouses had >12 years of education. Sixty percent of the mothers were employed during pregnancy, of whom 91.5% had a full-time job. Almost half of the mothers were in professional jobs, with a maternity leave that ranged between 7 and 150 days (average of 80 days). Within the first 24 hours of birth, almost all mothers (195, 98%) had no postpartum complications. The participants’ characteristics are presented in Table 1.
  | Table 1 Sociodemographic characteristics of the mothers (N=199) |
Rates of BF
Vigilant data about infant feeding were obtained from mothers before discharge, as well as at 6 weeks and 6 months after birth. The rate of BF initiation was only 13.1% during the first 4 hours after birth, was 57.8% between 4 and 12 hours of birth, and reached up to 90.0% within the first 24 hours after birth. At 6 weeks after birth, the rates of EBF, partial BF, and bottle feeding were 25.1%, 54.6%, and 19.9%, respectively. At 6 months after birth, rates of EBF, partial BF, and bottle feeding were 2.0%, 64.4%, and 33.5%, respectively (Table 2).
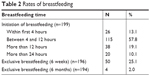  | Table 2 Rates of breastfeeding |
Relationship of BF with sociodemographic factors and birth interventions
Using Spearman rho correlation, mothers who initiated BF before discharge were significantly older (r=0.19, P<0.01) and employed (r=0.14, P<0.05). Significant relationship was found between mode of birth and the following: initiation of breastfeeding (r=0.38, P<0.01), information about BF during pregnancy (r=0.18), and information about BF during the postpartum period (r=0.16, P<0.05). No significant relationship was found between initiation of BF and the following: type of work, education status, and infant’s gender and birth weight (Table 3).
  | Table 3 Relationship between maternal and infant-related factors and breastfeeding |
Mode of birth (vaginal birth vs cesarean birth) and pain relief during childbirth (epidural or intramuscular pethidine) were examined. Thus, 130 mothers had vaginal births (65.3%). The remaining 69 (34.7%) had cesarean births. In the case of 121 mothers, pethidine was used during birth (60.8%), and 49 mothers received epidural analgesia containing fentanyl (24.6%). The remaining mothers (33, 16.2%) had no pharmacological analgesia other than intravenous paracetamol. No significant relationship was found between intramuscular and epidural pain management approaches and BF initiation and continuation.
The relationship between success of BF initiation and continuation of EBF at 6 weeks and 6 months on the one hand and active management of the third stage on the other was examined. Mothers in this study group had 100% episiotomies, and about 94% of them received active management by oxytocin and ergometrine during the third stage of birth. A significant relationship was found between the dose of ergometrine and EBF failure at 6 weeks (r=0.17, P<0.05), while no significant relationship was found between BF and the use of oxytocin in active management. The only significant relationship found was between the dose of ergometrine (a higher dose) administered in active management and BF failure (Table 4). Additionally, mothers’ reports indicated that they were more likely to stop BF because of pain during feeding related to cracked nipples or mastitis at 6 weeks after birth (r=0.17, P<0.05) (Table 5).
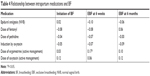  | Table 4 Relationship between intrapartum medications and BF |
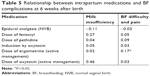  | Table 5 Relationship between intrapartum medications and BF complications at 6 weeks after birth |
Maternal factors for BF cessation were as follows: 1) inadequate milk (58.2%); 2) being tired of BF (29.5%); and 3) returning to work (26.4%). Infant-related factors included the following: 1) infant’s refusal of BF (16.1%); 2) infant’s weight gain was subnormal (8.25%); 3) infant’s health problems (5.7%); 4) nipple biting (5.7%); and 5) infant’s allergic response to breast milk (2.1%).
Discussion
This study yielded several salient findings that reflect the situation of intrapartum care in the two selected hospitals. To some extent, it can be assumed that there are many similarities of these situations in other maternity and neonatal wards across the country, and probably in countries where maternity care is still struggling to improve its maternal and neonatal statistical figures. To be more specific, intrapartum interventions are highly practiced, and BF policies are not officially regulated in spite of the relentless efforts of BF campaigns and education carried out by official bodies, such as the Ministry of Health and the United Nations Children’s Fund (UNICEF), to enforce policies that ban formula feeds and encourage BF.
This study showed low rates of initiation of BF within the first 4 hours of birth (13%). This suboptimal rate of BF initiation is congruent with findings drawn from many developing and developed countries.2,3,5 The result of low BF initiation is lower than that described in the statistics for Jordan (19%),4 Ethiopia (52%),2 and Bangladesh (36%).28 The nonendorsement of BF initiation policies, such as rooming-in or formula restriction enforcement regulations, has fostered the practice of a large proportion of mothers leaving their newborns in nursery units where they are formula fed. This low rate of initiation during the first 4 hours of birth is an indication of the lack of policies that encourage skin-to-skin contact and baby latches in birthing rooms. This may also represent the lack of knowledge of mothers about their rights to embrace their infants as soon as they are born. In another explanation that we may construe in these data, we find high rates of medicalization and interventions in childbirth. This includes the expansive use of pain medications, episiotomy, and active management of the third stage of birth.
In another dimension, this study revealed a significant relationship between BF initiation and three demographic variables. These include mothers’ age, employment status, and BF education during pregnancy and after birth. Most significantly, employed mothers were enthusiastic about initiating BF, knowing that they will be unable to continue BF upon returning to work after a maternity leave of a maximum of 90 days. Although employed mothers had higher initiation rates of BF than the nonemployed, they did not continue to breastfeed until 6 weeks and later. BF education during pregnancy and postpartum were significantly associated with BF initiation, and this is consistent with the literature (3, 6–8). This result is promising because, although BF education remains informally structured in maternity units, this has shown some positive results in initiating BF. Further plans and policies toward establishing structured BF education is recommended.
Regarding obstetric and neonatal factors, this study demonstrated that mothers who had cesarean births were less likely to initiate BF than mothers who had vaginal birth, but this did not show a significant relationship at 6 weeks or 6 months. This result is congruent with the plethoric literature that supports the notion that mode of birth is significantly associated with BF initiation and later success of BF.3,5,7,8,11,12 For instance, uncomplicated spontaneous vaginal birth, where there is immediate skin-to-skin contact with the infant, improves the chances of BF initiation and continuation.12,23 On the other hand, emergency and elective cesarean births are documented to negatively affect the success of BF.3,12,23
Contrary to studies in the region (Egypt [an Arab Muslim culture] and cultures with traditional beliefs [India, a traditional culture]),14,15 this study did not show a relationship between BF and infant’s gender and weight. Gender bias toward male children can be understood in the social context of preference for male children in the Middle East and the pressure exerted on a woman to get pregnant as soon she as gives birth to a female infant.16 In this situation, a woman is not encouraged to use contraceptives or to breastfeed as this may hinder an immediate pregnancy with another child.14,15 In this study, this was not the case because mothers were first-time mothers and were thrilled to have their first-born child; moreover, data were collected within 6 months of birth, not permitting us enough time to gauge their next pregnancy plans. It is worth examining in a later study how many mothers become pregnant within 6 months of birth.
In exploring the effect of pain medications, induction or augmentation of birth, and active labor management, the results showed no significant relationship between BF initiation and all intrapartum medications (pain management, induction and augmentation, and active management of birth). There was one only significant relationship, between EBF at 6 weeks and the dose of ergometrine, an active management drug, given during the third stage of birth to control postpartum bleeding. The dose of ergometrine was also significantly associated with BF difficulty and pain at 6 weeks after birth.
Our result of the lack of relationship between pain medication and induction of birth on the one hand and BF initiation and continuation on the other is contradictory to our understanding of the probable role of certain medications, such as pethidine and fentanyl, on the ability of infants to latch and suckle.23 These medications (opioids), which are widely administered during the first stage of birth for pain relief, pass to the neonate through the placenta and breast milk; moreover, lipophilic compounds, such as fentanyl and fentanyl derivatives, reach the neonate more quickly, and this association is dose related. These sedatives may interfere with the neonates’ coordination and ability to suckle.17–21 Prior research has demonstrated that this intervention is associated with a decrease in BF rates by hindering the initiation and continuation of BF,21,23 as well as increasing the perception of breast milk insufficiency.23 It is documented that mothers who had epidural analgesia were less likely to provide their infants with EBF at 12 weeks postpartum than mothers who had not had epidural analgesia.21 An association between doses of fentanyl and successful initiation and continuation of BF was established.17,19 However, no studies investigated the relationship between the use of fentanyl and its dose on BF among Jordanian mothers. This can be serious because of the substantial use of this drug by practitioners in birth settings in Jordan.
The finding of no significant relationship between BF initiation and these medications can be explained in relation to women’s enthusiasm as first-time mothers to breastfeed. It is a religious recommendation in Islam that mothers breastfeed their infants for 2 years, and thus most mothers are conditioned that BF is religiously rewarded. However, and later, as a mother starts encountering social challenges, such as the absence of assigned public areas for BF mothers, health problems such as painful BF and discomfort, and the absence of professional support, it is more likely that mothers relinquish BF entirely and look for easier alternatives to feed their babies. In the current study, mothers who stopped BF entirely at 6 weeks and 6 months reported multiple maternal and infant-related factors, examples of which include milk inadequacy, tiredness, infants’ health problems, lack of baby weight gain, allergy to milk, and refusal of BF.
In this study, almost all first-time mothers received an intramuscular injection of either oxytocin or Syntometrine® (oxytocin plus ergometrine) during the third stage (94%). Administration of the uterotonic agent (ergometrine) during the third stage did not interfere with BF initiation. However, it was associated with shortened BF duration later. Mothers were less likely to breastfeed by 6 weeks postpartum if they had received a higher dose of ergometrine in the third stage of birth. In developing countries, where about one-quarter of maternal deaths are related to hemorrhage, receiving active management during the third stage of birth (expulsion of placenta)23 is a common practice. This intervention seems to decrease duration of EBF, as indicated by a randomized controlled trial (n=132)24 that showed a statistically significant correlation between active management and BF cessation by 1 and 4 weeks after birth. In a large British survey23 (n=48,366), there was a reduction of 6%–8% in BF with the administration of oxytocin alone or in combination with ergometrine for prevention of postpartum hemorrhage. One possible explanation for this finding can be obtained by our understanding of the physiology of lactation. At birth, increased production of prolactin and oxytocin is important for successful BF. Ergometrine, which is a dopamine agonist, interferes with this process if given intramuscularly or intravenously. It is documented that the administration of ergometrine intravenously reduces the duration of BF by disturbing the normal physiology of lactation.23
In this study, mothers who had received higher doses of ergometrine were also more likely to report stopping BF at 6 weeks because they had more difficulty and pain. This is consistent with the study by Brown and Jordan,23 where mothers who received this medication reported difficulty with infant latch and had perceived milk insufficiency. Pain and discomfort during BF might affect proper latching and proper position. These two factors (good latch and proper positioning) are vital for the establishment of adequate milk supply and lactogenesis. Release of prolactin and oxytocin can be disturbed with weak suckle and incompletely emptied breasts, which subsequently results in infant’s weight loss, thus supporting the maternal perception of insufficient breast milk.13,23 This perception is documented as one of the most predictable factors of early discontinuation of BF in Jordan and other countries.7,9,13,23 In relation to the success of BF, this study and other evidence merit the need for greater support of mothers who receive active management. These mothers require help to overcome pain and difficulty associated with BF and milk insufficiency in the early postpartum days.
Implications of this study
Findings from this study enhance our confidence in the important role of counseling and educational programs before and after birth to prepare mothers to breastfeed their infants. The establishment of administrative structured environment toward baby-friendly units that actively apply the Ten Steps to Successful Breastfeeding can greatly enhance the rates of EBF.1 The establishment of written policies, structured educational programs, and the involvement of lactation consultants to consult and encourage BF before and after birth are essential in the enhancement of BF initiation and continuation plans.
Conclusion
This study expands our evidence-based understanding that intrapartum medications and procedures, as well as sociodemographic characteristics, may influence BF initiation and continuation of BF. Evidence about the negative role of ergometrine in the third stage of birth agrees with previous arguments regarding its interference with normal lactation process and physiology and, hence, BF difficulties and insufficient supply of breast milk.
Disclosure
The authors report no conflicts of interest in this work.
References
World Health Organization [homepage on the Internet]: World breastfeeding week; 2016. Available from: http://www.who.int/mediacentre/events/2016/world-breastfeeding-week/en/. Accessed May13, 2017. | ||
Salasibew MM, Filteau S, Marchant T. Measurement of breastfeeding initiation: Ethiopian mothers’ perception about survey questions assessing early initiation of breastfeeding. Int Breastfeed J. 2014;9(13):13. | ||
Al-Akour N, Khassawneh M, Khader Y, Ababneh A, Haddad A. Factors affecting intention to breastfeed among Syrian and Jordanian mothers: a comparative cross-sectional study. Int Breastfeed J. 2014;5(6R). | ||
Jordan Population and family health survey; 2012. Available from: https://dhsprogram.com/pubs/pdf/FR282/FR282.pdf. Accessed December 15, 2016. | ||
Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Matern Child Nutr. 2015;11(4):433–451. | ||
Jara-Palacios MÁ, Cornejo AC, Peláez GA, Verdesoto J, Galvis AA. Prevalence and determinants of exclusive breastfeeding among adolescent mothers from Quito, Ecuador: a cross-sectional study. Int Breastfeed J. 2015;10:33. | ||
Khasawneh W, Khasawneh AA. Predictors and barriers to breastfeeding in north of Jordan: could we do better? Int Breastfeed J. 2017;12(49):49. | ||
Cox K, Binns CW, Giglia R. Predictors of breastfeeding duration for rural women in a high-income country: evidence from a cohort study. Acta Paediatr. 2015;104(8):e350–e359. | ||
Oniwon O, Tender JA, He J, Voorhees E, Moon RY. Reasons for Infant Feeding Decisions in Low-Income Families in Washington, DC. J Hum Lact. 2016;32(4):704–710. | ||
Sulaiman Z, Liamputtong P, Amir LH. The enablers and barriers to continue breast milk feeding in women returning to work. J Adv Nurs. 2016;72(4):825–835. | ||
Li L, Zhang M, Scott JA, Binns CW. Factors associated with the initiation and duration of breastfeeding by Chinese mothers in Perth, Western Australia. J Hum Lact. 2004;20(2):188–195. | ||
Hobbs AJ, Mannion CA, Mcdonald SW, Brockway M, Tough SC. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth. 2016;16:90. | ||
Panigrahi A, das SC. Undernutrition and its correlates among children of 3–9 years of age residing in slum areas of Bhubaneswar, India. Scientific World Journal. 2014;2014(9):1–9. | ||
Jayachandran S, Kuziemko I. Why do mothers breastfeed girls less than boys? Evidence and implications for child health in India. Q J Econ. 2011;126(3):1485–1538. | ||
Chakravarty A: Gender-biased breastfeeding in Egypt. Examining the fertility preference hypotheses of Jayachandran and Kuziemko. Journal of Applied Economics. 2015;30(5):848–855. | ||
Safadi R. Jordanian women: perceptions and practices of first-time pregnancy. Int J Nurs Pract. 2005;11(6):269–276. | ||
Jordan S, Emery S, Bradshaw C, Watkins A, Friswell W. The impact of intrapartum analgesia on infant feeding. BJOG. 2005;112(7):927–934. | ||
Jordan S. Infant feeding and analgesia in labour: the evidence is accumulating. Int Breastfeed J. 2006;1(25):25. | ||
Torvaldsen S, Roberts CL, Simpson JM, Thompson JF, Ellwood DA. Intrapartum epidural analgesia and breastfeeding: a prospective cohort study. Int Breastfeed J. 2006;1(1(24):24. | ||
Radzyminski S. The effect of ultra low dose epidural analgesia on newborn breastfeeding behaviors. J Obstet Gynecol Neonatal Nurs. 2003;32(3):322–331. | ||
Volmanen P, Valanne J, Alahuhta S. Breast-feeding problems after epidural analgesia for labour: a retrospective cohort study of pain, obstetrical procedures and breast-feeding practices. Int J Obstet Anesth. 2004;13(1):25–29. | ||
Odent MR. Synthetic oxytocin and breastfeeding: reasons for testing an hypothesis. Med Hypotheses. 2013;81(5):889–891. | ||
Brown A, Jordan S. Active management of the third stage of labor may reduce breastfeeding duration due to pain and physical complications. Breastfeed Med. 2014;9(10):494–502. | ||
Begley CM. A comparison of ‘active’ and ‘physiological’ management of the third stage of labour. Midwifery. 1990;6(1):3–17. | ||
Sutherland T, Pierce CB, Blomquist JL, Handa VL. Breastfeeding practices among first-time mothers and across multiple pregnancies. Matern Child Health J. 2012;16(8):1665–1671. | ||
Bartlett J, Kotrlik J, Higgins C. Organizational research: Determining appropriate sample size for survey research. Information Technology, Learning, and Performance Journal. 2001;19(1):43–50. | ||
Statistics V21.0.0 documentation [homepage on the Internet]: IBM SPSS; 2012. Available from: https://www.ibm.com/support/knowledgecenter/en/SSLVMB_21.0.0/com.ibm.spss.statistics_21.kc.doc/pv_welcome.html. Accessed August 20, 2016. | ||
Joshi PC, Angdembe MR, das SK, Ahmed S, Faruque ASG, Ahmed T. Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: a cross-sectional study. Int Breastfeed J. 2014;9:7. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
