Back to Journals » Patient Preference and Adherence » Volume 17
Influencing Factor Analysis of First-Choice Medical Institutions for Aging People in China
Received 20 June 2023
Accepted for publication 23 September 2023
Published 5 October 2023 Volume 2023:17 Pages 2475—2485
DOI https://doi.org/10.2147/PPA.S426915
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Xianyu Xie,1,* Zijun Zhao,2,* Qinde Wu3,*
1Department of Medical Administration, Fujian Medical University Union Hospital, Fuzhou, Fujian, People’s Republic of China; 2School of Public Administration & Law, Fujian Agriculture and Forestry University, Fuzhou, Fujian, People’s Republic of China; 3Department of Education Administration, Fujian Medical University Union Hospital, Fuzhou, Fujian, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qinde Wu, Department of Education Administration, Fujian Medical University Union Hospital, No. 29 Xinquan Road, Fuzhou, Fujian Province, 350001, People’s Republic of China, Tel +0086-13365917369, Fax +0086-0591-83325046, Email [email protected]
Purpose: This study aimed to analyze first-choice medical institutions for middle-aged and older adults in Fujian Province to promote the development of hierarchical diagnosis and treatment for them.
Patients and Methods: Single factor analysis, disordered multi-classification logistic regression, and multiple correspondence classification were used to analyze the influencing factors of first-choice medical institutions for middle-aged and older adults. A total of 486 valid questionnaires were obtained. The questionnaire was based on Health Service Integration Theory and the behavioral model of Andersen.
Results: Age, education level, living area, monthly income, nearest medical institution to home, and integrated health service system understanding significantly influenced respondents’ preference of first medical institution. Middle-aged and older adults were more inclined to visit county and municipal hospitals first. The treatment center’s proximity was also an important determinant of their first-choice selection of medical care.
Conclusion: To realize high-quality hierarchical diagnosis and treatment and integrated health service system construction, it is important to improve the service capacity of primary medical institutions, increase the training of family doctors, implement the contract coverage of family doctors, optimize the allocation and geographical layout of primary medical institutions, ensure adequate income levels, and promote township hospital staff.
Keywords: hierarchical diagnosis, middle-aged adult, older adult, first medical institution, influencing factors
Introduction
In the 1990s, the United States created the integrated health service system (IDSs), which refers to the coordination and integration of the functions of different levels and types of health institutions and the activities of medical staff in the form of alliances to provide patients with safe, efficient, and high-quality comprehensive health services.1 Since then, health service integration has gradually become the focus of health system reforms in various countries.2 It has been proposed that the integration of health services involves investing and raising capital, as well as service provision, management, organization, and integration with clinical services. Establishing collaboration between different departments and within departments to improve services is also needed. According to extant research, the medical and health service system is changing from the diagnosis and treatment of individual patients to the health benefits service of the whole population.3–6
In China’s aging population, chronic non-communicable diseases are becoming increasingly severe. Further, the structure of health resources is unreasonable, and the medical and health service system is fragmented. One prominent problem is that it is “difficult and expensive to see a doctor”. Therefore, the Central Committee of the Communist Party of China and the State Council promulgated “Guidance on Promoting the Construction of the Hierarchical Diagnosis and Treatment (HDT)” to build IDSs. Fujian Province is one of the first provinces in China to pilot a comprehensive medical reform program. It took the lead in launching the construction of HDT. By the end of 2020, Fujian Province had IDSs in every county.7
The World Health Organization proposed that people aged 45–59 years are middle-aged and people aged 60 and above are older adults. Middle-aged and older adults over 45 years old are a unique group. Studies have shown that middle-aged and older adults are more likely to get sick than other age groups.8–10 The results of the seventh national census in China showed that the population aged 60 and above in China is 264.02 million, accounting for 18.70% of the total. Middle-aged people aged 45–59 are indispensable to the labor force needed for China’s economic development.
Chinese residents have always been able to choose medical treatment freely. This situation differs from developed countries such as the United Kingdom, the United States, and Germany, where residents are limited to medical treatments available at specific institutions. Few studies have examined the medical institution choice of older adult patients in China. Andersen’s model considers environmental factors, population characteristics, health behaviors, and health outcomes are the influencing factors of health choosing behavior.11 This study uses a questionnaire survey based on the Health Service Integration Theory and Andersen’s behavioral model to explore the situation and influencing factors of medical institution choice for middle-aged and older adult patients for HDT in Fujian Province. We also identify middle-aged and older adults’ vulnerabilities and put forward corresponding countermeasures to promote the further construction of HDT and improve their satisfaction and health level.
Methods
Data Source
Questionnaires were designed based on the Health Service Integration Theory and Andersen’s behavioral model. The main questionnaire contents included basic information (gender, age, education level, permanent residential area, type of medical insurance, monthly income, type of nearby medical institution, etc.), their understanding of the integrated health service system, and first-choice medical institutions.
Residents over 45 years old in integrated health service systems in nine cities of Fujian Province were selected as participants. Questionnaires were distributed based on the population of the integrated health service system using multistage random stratified sampling method from May to October 2022. Exclusion criteria were: unable to communicate or understand the questionnaire and unwilling to participate in the investigation.
A total of 500 questionnaires were distributed and 491 were returned, for a response rate of 98.20%. Among them, 486 questionnaires were valid, yielding an effective response rate of 98.98%.
Research Methods and Quality Control
Before conducting the questionnaire, the investigators were strictly trained and the recovered questionnaires were repeatedly reviewed item by item. The questionnaires were numbered and unqualified responses were eliminated. SPSS 22.0 was used for statistical analysis. Frequency description was used for basic information description. Univariate analysis (χ2 test) was used to study the difference of categorical variables and α=0.05 was used as the significant test level. Multiple correspondence analysis was used to explore the tendency of first-visit medical institutions in different middle-aged and older adult patients.
The reliability and validity of the questionnaire were analyzed, the reliability of the questionnaire being evaluated by Cronbach’s alpha. The coefficient was 0.871, indicating a good reliability level. The validity of the questionnaire was analyzed by the KMO test and Bartlett spherical test. The results showed that the KMO value was 0.904, Bartlett’s sphericity test chi-square value was 45,531.601, and the p-value was <0.01, indicating that the validity level was good. The reliability and validity of the questionnaire were tested and suitable for questionnaire analysis.
Results
Basic Information
The basic information of the 486 respondents is shown in Table 1.
 |
Table 1 Descriptive Statistics of the Participants |
First-Choice Medical Institution
The questionnaire in the form of single-choice questions was used to investigate respondents’ choice for the first visit to a medical institution. The results are shown in Figure 1. The choices for the first visit to a medical institution are ranked in the order of preference. The first choice included county-level hospitals at 45.27%, followed by municipal hospitals at 26.34%, community or township hospitals at 21.81%, and provincial hospitals at 6.58%.
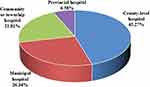 |
Figure 1 Preference of Respondents of Medical Institution. |
A survey was conducted on the most important factors considered by the respondents about first-choice medical institutions in the form of multiple-choice questions. The survey results are shown in Figure 2. The most important factors considered were ranked in the order of medical service level, service attitude, distance to visit, economic burden, hospital professional reputation, equipment completeness, drug completeness, and department completeness. Among them, 388 respondents selected the medical service level as the most important factor considered, accounting for 79.84%.
 |
Figure 2 Most Important Factors of First-Choice of Medical Institutions. |
Single Factor Analysis of Factors Influencing the Preference for Medical Institutions
The influencing factors of respondents’ preference for the first-visit medical institution were analyzed by single-factor analysis. The results are shown in Table 2. There was no significant difference in the effect of sex on the preference of the first medical institution (P>0.05). Factors such as age, education level, medical insurance type, permanent residential area, monthly income, nearby medical institution type and understanding of the integrated health service system had significant differences in the preference for the first choice in medical institutions (P<0.05).
 |
Table 2 Single-Factor Analysis of First-Choice Medical Institutions (N (%)) |
Multivariate Analysis of Influencing Factors of First-Choice Medical Institutions
Age, education level, medical insurance type, permanent residential area, monthly income, nearby medical institution type, and understanding of integrated health service system were selected for the univariate analysis. We used an unordered multi-class logistic regression model to further analyze these seven factors. The results are shown in Table 3. Age, education level, permanent residential area, monthly income, nearby medical institution type, and understanding of integrated health service system were the main factors influencing the first-choice medical institution.
 |
Table 3 Multi-Factor Analysis of First-Choice Medical Institutions |
Multiple Correspondence Analysis of Preference and Influencing Factors of First-Choice Medical Institutions
Multiple correspondence analysis was used to further analyze the influence of age, education level, permanent residential area, monthly income, type of nearby medical institution, and understanding of integrated health service system on the first-choice medical institutions of middle-aged and older adult patients. The results are shown in Figure 3. Correspondence analysis is a visual data analysis method that uses graphs to represent the relationships between categories of categorical variables in a low-dimensional space. Multiple correspondence analysis can study the relationships between multiple categorical variables and explore the correspondence between different variables by analyzing the interactive summary of qualitative variables.12 The results showed that middle-aged and older adult patients over 65 years old, living nearby a community or township hospital, having attended junior high school and below, and who have not heard of the integrated health service system preferred to first visit a community or township hospital; respondents in rural areas, with high school education, a home nearby county-level hospitals, an understanding of integrated health service systems, aged 46–55 years old, and with a monthly income of 3000–5000 preferred to visit county-level hospitals first. Middle-aged and older adult patients 56–65 years old living near a municipal hospital preferred to visit the municipal hospital first, while those living near provincial hospitals and high-income individuals preferred to visit provincial hospitals first.
 |
Figure 3 Corresponding Analysis of the Influencing Factors of First-Choice Medical Institutions for Middle-Aged and Older Adult Patients. |
Discussion
Middle-Aged and Older Adult Patients Prefer County-Level Hospitals
According to the “Fujian Health Statistical Yearbook”, in 2020, the number of visits to tertiary hospitals (mainly municipal and provincial hospitals) in Fujian Province accounted for 23.34% of the total number of visits, while the number of visits to primary health care institutions (mainly community or township hospitals) accounted for 56.26% of the total number of visits. According to the survey results, 45.27% of middle-aged and older adult patients preferred to visit county-level hospitals first and 26.34% preferred to go to municipal hospitals for the first diagnosis. When combined, the percentage exceeded 70%, which was much larger than that for the sum of community or township hospitals and provincial hospitals. Moreover, 79.84% of the middle-aged and older adult patients surveyed regarded the medical service level as the most important factor when considering the first choice in medical institutions, ranking first among the eight types. The proportion of primary medical institutions ranked as the first choice was low. The main reason is that middle-aged and older adults have multiple chronic diseases and their conditions are relatively complex. Extant studies have shown that due to long-term fatigue, bad habits, social pressure, and other factors, the probability of chronic diseases and geriatric syndromes in older adults is significantly higher than that in young adults.13 However, in recent years, with the vigorous implementation of the policy of HDT and integrated health service systems, the medical service level of primary medical institutions has improved. However, their attraction to high-quality medical staff is insufficient and their ability to diagnose and treat the relatively complex conditions of middle-aged and older adults is lacking. The trust of middle-aged and older adults in primary medical institutions is not high as well, which leads to an insufficient willingness to first visit primary medical institutions. The low proportion of first visits to provincial hospitals is mainly due to the inconvenience of the location and the economic burden of medical treatment. Provincial hospitals are mostly in the center of the provincial capital city. For most middle-aged and older adults, the long distance to reach medical treatment and the relative inconvenience of travel greatly reduce the convenience of medical treatment. Provincial hospitals have relatively higher medical expenses and lower medical insurance reimbursement rates, and most middle-aged and older adults have relatively low economic incomes. Therefore, the economic burden of medical treatment may lead them to choose medical institutions with lower medical costs. A county-level hospital is between primary medical institutions and provincial hospitals and treats moderate-difficulty diseases, which is more in line with the medical needs of middle-aged and older adults. From the perspective of middle-aged and older adults, the current implementation of the HDT policy in Fujian Province is not effective. We thus recommend improving the service capacity of primary medical institutions for middle-aged and older adults’ diseases, increasing the training of family doctors, implementing the contract coverage of family doctors, releasing the medical responsibilities of county and municipal hospitals to primary medical institutions, increasing the proportion of primary medical institution selected as a first choice, and realizing high-quality HDT and integrated health service system construction.
Visiting Distance is an Important Influencing Factor for the First Choice of Medical Institutions
For every 1% increase in the distance between residence and medical institutions, the demand for health services decreases by 0.36%.14 Our results show that the proximity of a medical institution to the home is an important influencing factor for middle-aged and older adult patients. A nearby medical institution is the first choice for most middle-aged and older adult patients. The proportion of such patients who lived near the provincial hospitals that they ranked as their first choice was as high as 75.00%, while that of middle-aged and older adult patients who were near the municipal hospitals that they ranked as their first choice was as high as 85.05%. Further, the proportion of the participants who lived near the county hospitals that they ranked as first choice was as high as 85.43% and that of middle-aged and older adult patients who lived near the communities or township hospitals that they ranked as their first choice was 50.00%. The visit distance of medical treatment reflects the latter’s convenience and cost. Due to the relative inconvenience of movement, middle-aged and older adult patients will pay more attention to visit distance and convenience of medical treatment. According to the survey, 281 middle-aged and older adult patients ranked visit distance as the most important factor, accounting for 57.82%, ranking third among the eight factors. Therefore, government departments at all levels should optimize the allocation and geographical layout of primary medical institutions to provide medical resources and improve the effect of HDT in the future. Additionally, they should aim to shorten the travel time for care at primary medical institutions, invest more medical resources, provide convenient basic medical services for middle-aged and older adult patients, improve the proportion of primary first diagnosis for these patients, and improve their health level. They should also increase the input from medical patients, medical equipment, and drugs in primary medical institutions.
Regional Differences
The questionnaire results showed a significant difference (P<0.05) in the first-choice medical institutions among residential areas. Specifically, middle-aged and older adult patients in urban areas tended to first visit primary medical institutions and 34.78% of them first visited community or township hospitals. Middle-aged and older adult patients in rural areas tended to visit county-level hospitals first and 56.62% of them visited county-level hospitals first. One reason may be that, compared with rural areas, the configuration and layout of primary medical institutions in urban areas are more reasonable and primary medical institutions for middle-aged and older adult patients in urban areas are more convenient. Second, compared with rural areas, urban areas have a higher level of economic and social development, meaning it is easier to cultivate the medical habits of the patients’ first visit to primary medical institutions. Studies on the medical behavior of rural residents in India and Ethiopia showed a significant positive impact on the demand for medical services.15,16 Another study showed that the higher the household monthly expenditure is, the more likely family members are to use medical services, and that the price elasticity of demand is between −0.19 and 0.11.17 Third, compared with rural areas, primary institutions in urban areas have more complete hardware and software facilities, more adequate medical staff, and higher medical service levels, which makes them more attractive to middle-aged and older adult patients, while patients from rural areas prefer county-level hospitals that provide a better initial medical experience. Relatively, the HDT policy in the urban areas of Fujian Province was more consistently implemented and achieved good initial results. Therefore, in the process of carrying out HDT and the construction of integrated health service systems, more attention should be paid to the construction of primary medical institutions in rural areas, focusing on the construction of the medical service capacity of township hospitals, increasing investment, ensuring the income level and promotion channels for township hospital staff, attracting high-quality medical staff to join, improving the proportion of first visit primary medical institutions in rural areas, improving the health level of middle-aged and older adults in rural areas, and achieving high-level HDT.
Educational Level Influences First-Choice Medical Institutions
Education can improve individual health awareness and relay the necessary information for the use of medical services. It also affects the choice of medical institutions and the number of medical services when individuals seek medical treatment.18 An extant study used the China Health and Nutrition Survey to analyze the relationship between individual social interaction and health service utilization, showing that active participation in social activities of the individual make possibility of using medical service greater.19 According to the results, there was a significant difference in the influence of education level on the preference for the first visit to medical institutions (P<0.05). The results showed that middle-aged and older adult patients with a junior high school level education and below were more likely to prefer to visit the primary medical institution first, while those with a high school education or above were more likely to prefer to visit county hospitals and higher-level hospitals first. In other words, the higher the education level of middle-aged and older adult patients, the more they prefer to visit higher-level medical institutions first. Extant studies have also shown that the high-education level people have better health literacy and information search capabilities.20 In the case of a minor illness, they usually use their own medical knowledge and the Internet to inform their medical treatment rather than visiting medical institutions. Moreover, their demands are focused or targeted to obtain better medical services, and they are consequently more likely to choose a high-level medical institution.21 Therefore, government departments should continue to pay attention to the medical issues of middle-aged and older adults with different educational levels, increase efforts to carry out publicity and education on HDT for individuals with a higher education level, and guide their first visit to a primary medical institution. By using new media and self-media to publicize the advantages and characteristics of primary medical institutions, each regional government should adapt primary medical institutions to the medical habits and needs of local middle-aged and older adults, improve the medical environment of primary medical institutions, create targeted medical service characteristics and highlights, and enhance the experience and satisfaction of primary medical institutions. They should also promote preventive health care and health promotion projects such as health counseling, psychological counseling, and rehabilitation health care; attract primary medical treatment seekers from the middle-aged and older adult population with a higher education level; promote HDT; and decrease medical costs.22
Conclusions
The results showed that age, education level, permanent residential area, monthly income, nearby medical institution type, and understanding of integrated health service system were the main factors influencing the first-choice medical institution. To realize high-quality HDT and build an integrated health service system, it is important to improve the service capacity of primary medical institutions, increase the training of family doctors, implement the contract coverage of family doctors, optimize the allocation and geographical layout of primary medical institutions, ensure adequate income levels, and provide promotion paths for township hospital staff.
Ethics Approval and Consent to Participate
All methods were carried out in accordance with relevant guidelines and regulations. Ethical clearance (2022KY205) was granted by the ethics committee of Fujian Medical University Union Hospital. Informed consent was obtained from individual participants. The study complies with the Declaration of Helsinki.
Acknowledgments
We would like to express our gratitude to all who have helped us throughout the research and writing of this paper. We also want to thank all professors and warm-hearted teachers who have greatly helped us in our studies and lives. Finally, our gratitude also extends to our friends and families, who have provided invaluable encouragement and financial support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by Fujian Province Social Science Foundation Project in 2023 (FJ2023BF030), the Fujian Provincial Innovation Strategy Research Project (grant number 2021R0052), Fujian Provincial Innovation Strategy Research Project (grant number 2022R0038), Fujian Provincial Health Technology Project (grant number 2020RK008), and Startup Fund for Scientific Research, Fujian Medical University (grant number 2019QH1063).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Enthoven AC, Tollen LA. Competition in Health Care: it Takes Systems to Pursue Quality and Efficiency. Health Aff. 2005;24(1):240–433. doi:10.1377/hlthaff.24.1.240
2. Schmitt M. Do Hospital Mergers Reduce Costs? J Health Econ. 2017;52(3):74–94. doi:10.1016/j.jhealeco.2017.01.007
3. Kodner DL. Integrated care: meaning, logic, applications, and implications - A discussion paper. Int J Integr Care. 2002;2:e12. doi:10.5334/ijic.67
4. Simoens S, Scott A. Integrated primary care organizations: to what extent is integration occurring and why? Health Serv Manage Res. 2005;18(1):25–40. doi:10.1258/0951484053051951
5. Krieger JW, Bourcier E, Lara M, et al. Integrating asthma prevention and control: the roles of the coalition. Health Promot Pract. 2006;7(2 Suppl):127S–138S. doi:10.1177/1524839906287059
6. Shahzad M, Upshur R, Donnelly P, et al. A population based approach to integrated healthcare delivery: a scoping review of clinical care and public health collaboration. BMC Public Health. 2019;19:708. doi:10.1186/s12889-019-7002-z
7. Wu Q, Li Y, Xie X, Pan B, Chen Y, Wang L. The impact of basic medical insurance system on medical economic burden of the rural older adult residents in Fujian. Chin Rural Health Serv Admin. 2018;38:705–709. doi:10.3969/j.issn.1005-5916.2018.06.001
8. Jiao N, Guo Y. The identification and governance of rural elderly poverty in China from the perspective of multidimensional deprivation. Chin J Pop Sci. 2021;3:82–97.
9. Liu E, Zhang Q, Feng Y. Elderly poverty risk due to chronic diseases: theoretical mechanism and empirical analysis. Ins Stud. 2020;11:6378.
10. Liu Z, Zheng W, Jia R, Jing P. Health insurance, health heterogeneity, and targeted poverty reduction: a vulnerability to poverty approach. J Financ Res. 2019;5:56–75.
11. Andersen RA. Behavioral Model of Families’ Use of Health Services. Chicago: Center for Health Administration Studies, University of Chicago; 1968. doi:10.13497/j.cnki.is.2020.11.005
12. Khangar NV, Kamalja KK. Multiple correspondence analysis and its applications. Electr J Appl Statist Anal. 2017;10(2):432–462.
13. Yin QI, He Y, Sun C, et al. Application of multidimensional comprehensive diagnosis and treatment program in the treatment of chronic diseases in the older adult. Chin J Gerontol. 2021;41:1031–1033. doi:10.3969/j.issn.1005-9202.2021.05.040.016
14. Dzator J, Asafu-Adjaye J. A study of malaria care provider choice in Ghana. Health Policy (New York). 2004;69(3):389–401. doi:10.1016/j.healthpol.2004.01.005
15. Asfaw A, Von Braun J, Klasen S. How big is the crowding-out effect of user fees in the rural areas of Ethiopia? Implication for equity and resources mobilization. J World Dev. 2004;32(12):2065–2081. doi:10.1016/j.worlddev.2004.07.004
16. Sarma S. Demand for outpatient healthcare: empirical findings from rural India. Appl Health Econ Health Policy. 2009;7(4):265–277. doi:10.1007/BF03256160
17. Srivastava D, McGuire A. Patient access to health care and medicines across low-income countries. Soc Sci Med. 2015;133:21–27. doi:10.1016/j.socscimed.2015.03.021
18. Dou Y. Review of foreign medical behavior research. Rural Econ Sci-Technol. 2017;28:
19. Dong GN. Social capital as correlate, antecedent, and consequence of health service demand in China. China Econ Rev. 2016;37:85–96. doi:10.1016/j.chieco.2015.12.001
20. Shan L, Wu L. A study on the cognition and intention of medical cluster among residents in Nanjing. Chin Hosp. 2021;25:9–10. doi:10.19660/j.issn.1671-0592.2021.2.03
21. Wang Y, Mou M, Zhao S, Guo D, Wang L. Research on influencing factors of residents’ willingness of first-visit at grass roots medical institution under the background of hierarchical medical system in Shandong Province. Med Soc. 2021;34:77–81. doi:10.13723/j.yxysh.2021.02
22. Zhao S, Tong X, Zhang A, Wu Q, Zhang Y, Wang Y. Study on the influence of patients’ trust mode and level on the willingness of primary first visit. Chin J Health Policy. 2021;14:16–20. doi:10.3969/j.issn.1674-2982.2021.08.003
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
