Back to Journals » Clinical Ophthalmology » Volume 17
Influence of Trabeculectomy with Mitomycin C on Longitudinal Changes in the Visual Field in Glaucoma Patients with High Myopia
Authors Yamagata Y, Suda K , Akagi T, Ikeda HO, Kameda T, Hasegawa T, Miyake M, Tsujikawa A
Received 17 April 2023
Accepted for publication 17 July 2023
Published 17 August 2023 Volume 2023:17 Pages 2413—2422
DOI https://doi.org/10.2147/OPTH.S415654
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Yutaro Yamagata,1 Kenji Suda,1 Tadamichi Akagi,1,2 Hanako Ohashi Ikeda,1 Takanori Kameda,1 Tomoko Hasegawa,1 Masahiro Miyake,1 Akitaka Tsujikawa1
1Department of Ophthalmology and Visual Sciences, Kyoto University Graduate School of Medicine, Kyoto, Japan; 2Division of Ophthalmology and Visual Science, Niigata Graduate School of Medical and Dental Sciences, Niigata, Japan
Correspondence: Kenji Suda, Department of Ophthalmology and Visual Sciences, Kyoto University Graduate School of Medicine, 54 Shougoin Kawahara-cho, Sakyo-ku, Kyoto, Japan, Tel +81-75-751-3248, Fax +81-75-752-0933, Email [email protected]
Purpose: To evaluate the effect of trabeculectomy (Trab MMC) on visual field (VF) progression in eyes with glaucoma and high myopia.
Patients and Methods: Patients diagnosed with primary open-angle glaucoma or exfoliation glaucoma who underwent Trab MMC as the first glaucoma surgery along with ≥ 3 VF tests preoperatively and postoperatively were enrolled. High myopia was defined as an axial length ≥ 26.5 mm. Postoperative reductions in intraocular pressure (IOP) were assessed by survival analysis using IOP measurements obtained preoperatively. The longitudinal trends of the outcome measures were evaluated using linear mixed models.
Results: Thirty-five eyes of 32 patients were included in this study, including 22 eyes of 20 patients in non-highly myopic group and 13 eyes of 12 patients in highly myopic group. IOP decreased after Trab MMC, and the survival rate did not differ significantly in relation to axial length. Linear mixed-model analyses suggested that the inhibitory effects of Trab MMC on the rate of mean deviation (MD) changes were significant in the non-highly myopic group (− 0.53 ± 0.15 dB/year preoperatively to − 0.16 ± 0.13 dB/year postoperatively; P = 0.004), but not in the highly myopic group (− 0.66 ± 0.19 dB/year preoperatively to − 0.48 ± 0.18 dB/year postoperatively; P = 0.32).
Conclusion: Trab MMC reduced IOP in both highly myopic and non-highly myopic eyes, and IOP reduction was very similar in both groups. The VF deterioration rate decreased in both groups, but the change was weaker and nonsignificant in the highly myopic group.
Keywords: glaucoma, myopia, trabeculectomy, glaucoma progression
Introduction
Over the past few decades, a considerable number of studies have evaluated the relationship between glaucoma and myopia, and myopia is known to be a risk factor for the development of glaucoma.1–3 A meta-analysis of 11 population-based studies by Marcus et al reported that the pooled odds ratio between low myopia and glaucoma was 1.65 and that between high myopia and glaucoma was 2.46.4 However, the influence of myopia on glaucoma progression remains debatable; some recent studies have shown that myopia is a protective factor against glaucoma progression,5–7 whereas others concluded that the opposite is true.8–10 A few studies also indicated that the effect of myopia was not significant on either direction.11
In addition to showing visual field (VF) deterioration, glaucoma with myopia has been also reported to be associated with a higher risk of cecocentral VF loss in early stages.12,13 VF defects in the central VF directly affect the quality of vision, and thus can be a driving force alongside the VF deterioration rate for the initiation of early surgical treatments, such as trabeculectomy with mitomycin C (Trab MMC), in treating glaucoma with myopia.
Trab MMC is a primary surgical option for glaucoma in adults that can lower intraocular pressure (IOP) and protect VF progression. Although the effect of Trab MMC has been shown repeatedly,10,14,15 only a few attempts have been made to investigate the effect of this glaucoma treatment for patients with high myopia. A previous study by Tanaka et al showed that the IOP-lowering effect of Trab MMC was similar in highly myopic and non-highly myopic eyes with glaucoma, but they did not analyze the influence of these effects on VF progression.16 Since eyes with high myopia tend to show a unique progression of VF, as described above, and characteristic structural findings such as tilted disc or peripapillary atrophy (PPA) are observed,17 similar IOP-lowering effects may not directly imply similar abilities to protect against VF loss. Therefore, in this study, we evaluated the effects of Trab MMC on the VF deterioration rate and compared the results between highly myopic and non-highly myopic eyes.
Methods
Patients
This retrospective study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board and Ethics Committee of Kyoto University Graduate School of Medicine (approval number: R2652). Written informed consent was waived because of the retrospective design of this study, instead we have publicly disclosed this retrospective research on the treatment outcomes of glaucoma on our faculty’s website, also providing the subjects an opportunity for opt-out. Under this condition, the Institutional Review Board and Ethics Committee of Kyoto University Graduate School of Medicine approved the waiver of informed consent. Patient data were stored and handled safely and securely to ensure patient confidentiality in this study. We retrospectively enrolled patients who met the following inclusion criteria: diagnosed with primary open-angle glaucoma or exfoliation glaucoma by gonioscopy, underwent Trab MMC as the first glaucoma surgery between January 2009 and February 2018 at Kyoto University Hospital, and had undergone 3 or more VF tests with reliable results using a Humphrey Visual Field Analyzer (HFA; Carl Zeiss-Meditec, Dublin, CA, USA) using the 24–2 or 30–2 SITA standard testing protocol each preoperatively and postoperatively in our hospital. Eyes with prior or ongoing uveitis, history of ocular trauma, neovascularization of the iris, macular diseases that can influence visual acuity (eg, retinal vein occlusion, diabetic retinopathy), previous refractive surgery or intraocular surgery other than cataract surgery, aphakia, neurologic diseases that can influence visual acuity (eg, pituitary tumor) were excluded.
Primary open-angle glaucoma was diagnosed if the following 3 findings were present: (1) Glaucomatous cupping of optic disc such as notch formation or retinal nerve layer defects detected by fundus photography or optical coherence tomography (OCT); (2) Glaucomatous VF defects, defined according to Anderson and Patella’s criteria (a cluster of 3 or more points in the pattern deviation plot within a single hemifield [superior or inferior] with a P value < 5%, one of which must have a P value < 1%);18 and (3) An open angle observed on gonioscopy.
Data Collection
Data on the age at operation, sex, diagnosis, axial length, and presence of combined cataract surgery were collected from clinical records. IOP measurements were obtained just before surgery and at 1 month, 3, 6, and 12 month(s) after surgery.
Baseline examinations included evaluations of best-corrected visual acuity (BCVA; decimal visual acuity measured by Landolt C), refraction (ARK-530A; Nidek, Gamagori, Japan), IOP measurements using Goldmann applanation tonometry, central corneal thickness (SP-3000; Tomey, Tokyo, Japan), gonioscopy including anterior chamber angle, axial length measurements using ocular biometry (IOL Master; Carl Zeiss Meditec), slit-lamp biomicroscopy, stereoscopic optic disc photography (3-Dx simultaneous stereo disc camera; Nidek, Gamagori, Japan), Spectralis HRA+OCT (Heidelberg Engineering, Heidelberg, Germany), and VF tests using HFA. For both 24–2 and 30–2 examinations of HFA, the mean of the total deviation (TD) of the test point corresponding to 24–2 was treated as the mean deviation (MD) of the 24–2 examination. Only reliable results (less than 20% fixation losses, 15% false-positive responses, and 15% false-negative responses) were included. High myopia was defined as an axial length ≥26.5 mm,19,20 and the patients were divided into 2 groups (highly myopic and non-highly myopic groups).
Trabeculectomy
Trab MMC was performed by 4 surgeons (TA, TK, HN, or MH). As previously described (Supplement Figure 1);16 after topical anesthesia, a fornix-based flap of the conjunctiva and Tenon capsule was created by limbal peritomy at the superonasal or superotemporal quadrant. Sub-Tenon anesthesia was administered at the counter quadrant. Bipolar diathermy was used for hemostasis when needed. A 4×4 mm partial thickness rectangular scleral flap was created, and MMC (0.4 mg/mL, 0.04%) was applied to the scleral flap and sub-Tenon capsule space with surgical sponges for 3 to 4 min. The area was then irrigated with 200 mL of balanced salt solution. Phacoemulsification with intraocular lens (IOL) implantation was performed after the irrigation if combined with Trab MMC. A second 3 × 4-mm deep rectangular scleral flap was constructed, which was removed with the trabecular block followed by a peripheral iridectomy. The first scleral flap was sutured using 10–0 nylon. The number, position, and tension of the sutures were individualized for each case to provide adequate leakage of the aqueous fluid. The fornix-based flap of the conjunctiva and Tenon capsule was closed with 10–0 nylon and anchored at the limbus.
All patients received topical antibiotics and topical steroids for 1 to 3 months after the surgery. The 10–0 nylon sutures anchoring the conjunctiva and Tenon capsule to the limbus were removed approximately 1 month after the surgery. Postoperative interventions, such as digital ocular massage, laser suture lysis, and anterior chamber reformation, were done based on the IOP, conjunctival bleb shape, anterior chamber depth, and presence/absence of complications. If a postoperative IOP elevation was due to insufficient filtration, laser suture lysis was applied after a lack of response to digital massage. If the high IOP persisted, needling was performed in the operating room. MMC was used in some cases according to surgeon’s discretion. If the high IOP could not be reduced by these procedures, bleb revision surgery was performed in the operating room. Topical antiglaucoma medications were restarted according to decision of the consulting doctor.
Definition of Success
We conducted a survival analysis for IOP according to the consensus for the definition of success and the guidelines on the design and reporting of glaucoma surgical trials.
Postoperative IOP was assessed on the basis of the probability of success in the Kaplan–Meier survival-curve analysis. We defined 3 success criteria (1, 2, and 3) according to the guidelines of the World Glaucoma Association and considered cases meeting all 3 criteria as successful: criterion 1, absence of reoperation (additional glaucoma surgery); criterion 2, postoperative IOP < 18, 15, or 12 mmHg (3 alternative limits); criterion 3, ≥20% reduction from baseline. For criteria 2 and 3, exceeding the limits on 2 consecutive visits was treated as failure. If the IOP was controlled under limit, needling and additional medication(s) were not defined as failure.
Statistical Analysis
A generalized estimating equation (GEE) was used to compare the means between the groups with and without high myopia. Each eye is considered to be dependent on an individual in the GEE framework. Differences in categorical parameters between the 2 groups were evaluated using Fisher’s exact test. Comparisons of success rates between the groups and identification of the relative risk of surgical failure were performed using Kaplan–Meier survival analysis and a mixed-effects Cox regression model using the “survival” and “coxme” packages in R (R Foundation for Statistical Computing, Vienna, Austria). In the mixed-effects Cox regression model, eyes were nested within patients as a random effect.
The longitudinal time trends of the outcome measures were evaluated using linear mixed models (LMMs) fitted with random intercepts and coefficients at both subject and eye levels. The following equation describes the corrections applied to the data.
Model A: Yijt = β0 + β1 × TIME + ζ0j + ζ1j×TIME + ζ0i|j + ζ1i|j×TIME + ɛijt,
where Yijt is the individual measurement at visit t; β0 and β1 are the fixed-effects coefficients; ζ0j and ζ1j are the random patient effects associated with the intercept and time slope, respectively; and ζ0i|j and ζ1i|j are the random effects associated with the inclusion of both eyes of a single subject. Model A was applied to the data before and after the surgery in each group.
To compare the rate of MD change between the groups or between the preoperative and postoperative periods, we applied the following equation to all VF results in this study.
Model B: Yijt =β0 + β1 × TIME + β2 × group (high myopia or not) + β3 × surgery (before surgery = 0, after surgery =1) + β4 × group × surgery + β5 × TIME × group + β6 × TIME × surgery + β7 × TIME × group × surgery + ζ0j + ζ1j × TIME + ζi|j + ζ1i|j × TIME + ɛijt
Model B allowed evaluation of the extent of perioperative MD exacerbation (β3), the difference in perioperative MD exacerbation between the groups (β4), and the difference in the rate of MD change before and after surgery between each group using the results of β1, β5, β6, and β7.
All P-values presented are two-sided values. Statistical significance was defined as P < 0.05. All analyses were performed using R ver. 4.04 and SAS ver. 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
Thirty-five eyes from 32 patients were included in this study. During the period from 2008 to 2018, 97 eyes underwent Trab MMC as the first surgery for glaucoma at Kyoto University Hospital, of which 35 also underwent sufficient VF tests. The axial length of 22 eyes of 20 patients was shorter than 26.5 mm (non-highly myopic group), and that of 13 eyes of 12 patients was longer than 26.5 mm (highly myopic group). The observation period was 9.23 ± 3.07 years in the non-highly myopic group and 9.63 ± 2.84 years in the highly myopic group, 9.38 ± 2.88 years overall.
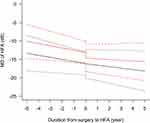
Table 1 shows the demographic and ophthalmic characteristics of the patients. The average patient age was 64.5 ± 10.6 years in the non-highly myopic group and 58.9 ± 10.3 years in the highly myopic group. Only the number of eyes of patients with dyslipidemia differed significantly between the two groups (p=0.02). The findings of survival analyses of postoperative IOP are illustrated in Figure 1. Mixed-effects Cox regression showed no significant intergroup differences at all three limits for defining success (18, 15, and 12 mmHg).
 |
Table 1 Demographics of the Subjects in the Current Study |
The results of the LMM analysis (Model A: simplified model with no comparison between groups or periods) are presented in Table 2. In the non-highly myopic group, the rate of MD change was −0.78 ± 0.30 dB/year preoperatively and −0.08 ± 0.10 dB/year postoperatively. In the highly myopic group, the corresponding values were −0.78 ± 0.18 dB/year and −0.67 ± 0.20 dB/year, respectively. Intercept refers to the estimated HFA MD at the operation. The intercept soon before or soon after the operation was estimated from each LMM before or after the operation. A gap was observed between the 2 intercepts, not only in both groups, but also before and after surgery, indicating the existence of perioperative exacerbation.
 |
Table 2 Results of Linear Mixed Model A Estimating Rates of Mean Deviation Changes in Visual Field Testing Before and After Trabeculectomy |
To compare the significant differences in the rates of MD changes or perioperative MD exacerbations, we conducted another LMM analysis (Model B; a complex model enabling comparison between groups or between preoperative and postoperative periods) (Table 3 and Figure 2). The perioperative exacerbation was 0.91 ± 0.26 dB. The extent of exacerbation differed but not significantly between the groups (non-highly myopic group: 1.22 ± 0.31 dB [95% confidential interval (CI): 0.60 to 1.84 dB]; highly myopic group: 0.19 ± 0.46 dB [95% CI: −0.72 to 1.10 dB]; P = 0.07). The inhibitory effect of Trab MMC on VF deterioration (rate of MD change) was significant in the non-highly myopic group (−0.53 ± 0.15 dB/year preoperatively to −0.16 ± 0.13 dB/year postoperatively; P = 0.004), but not in the highly myopic group (−0.66 ± 0.19 dB/year preoperatively to −0.48 ± 0.18 dB/year postoperatively; P = 0.32). These differences in the inhibitory effects of Trab MMC on the deteriorating rates of changes between the groups were not significant (0.19 ± 0.22 dB/year [95% CI: −0.25 to 0.63 dB/year]; P = 0.39; Table 3).
 |
Table 3 Results of Linear Mixed Model B Estimating Rates of Mean Deviation Changes in Visual Field Testing Before and After Trabeculectomy |
Discussion
This study evaluated the effect of Trab MMC on VF progression in eyes with glaucoma and high myopia, and the results indicated a notable reduction in IOP after Trab MMC, and that the extent of IOP reduction did not differ significantly between the two groups divided by axial length. This result is consistent with that of a previous report by Tanaka et al14 which indicated that the IOP-lowering effect did not differ in relation to the presence of high myopia or that the effect was slightly higher in the highly myopic group. However, some reports have suggested that the IOP-lowering effect is significantly weaker in the eyes of younger patients.16,21 In our study, the average age in the highly myopic group was comparatively lower; therefore, the higher IOP-lowering effect in high myopia may have been counteracted by the influence of younger patient age.22 In terms of IOP-lowering effects, Trab MMC can be regarded as an effective treatment for glaucoma in highly myopic eyes.
The simple calculation of the rate of MD change in the patients in this study indicated that Trab MMC resulted in a significant improvement in the longitudinal MD change. The extent of this effect was reasonable in comparison with the findings reported previously. Bertrand et al reported the rate of change in the VF between before and after Trab MMC by using a similar method as in this study; in their study, IOP reduction from 18 mmHg to 11 mmHg had an inhibitory effect on VF deterioration (−0.36 dB/year preoperatively to −0.16 dB/year postoperatively).14 Shigeeda et al also revealed a slowdown in the MD slope after Trab MMC in normal-tension glaucoma (NTG) patients (−1.05 dB/year preoperatively to −0.44 dB/year postoperatively).15 Although most of the patients in these previous reports had NTG with IOPs within the normal limits before surgery, the inhibitory effect of Trab MMC on VF deterioration was confirmed to be reproducible in all patients, including those with high myopia.
The analyses using the mixed-effects Model A revealed a gap between the 2 intercept MDs estimated from Model A before and after surgery in each group. We hypothesized that perioperative exacerbations would occur in Trab MMC, which has already been reported in several studies.23,24 Naito et al analyzed the perioperative MD change in Japanese NTG patients, reporting that the MD obtained using the HFA changed from −18.86 ± 4.16 dB preoperatively to −20.11 ± 4.25 dB postoperatively. The deterioration of −1 dB in the perioperative period in their study was similar to the results of our study. However, in their study, the perioperative gap was larger in the highly myopic group, in contrast to our results. Considering the causes of MD changes before and after surgery, they speculated that the changes in ocular rigidity represented by hypotony maculopathy resulted in a reduction in visual acuity, which can explain the greater perioperative deterioration of MD in highly myopic eyes since highly myopic eyes are generally considered to have weak stiffness. However, while their findings were obtained in NTG patients, many of the eyes in our study had high preoperative IOP above the normal limit. Since preoperative elevation and perioperative fluctuation of IOP may be the primary causes of perioperative MD deterioration in our study, the results for the perioperative MD gap may be different between the previous and current studies.
Although the MD slope improved in both the highly myopic and non-highly myopic groups in the present study, the inhibitory effect of VF deterioration was small and not significant in the highly myopic group. Because IOP decreased well in both groups as shown in Figure 1, this mild effect in highly myopic eyes may be attributable to factors unrelated to IOP. The factors may be the features in highly myopic eyes that accelerate VF progression independent of IOP. Some distinguishing characteristics of glaucoma with high myopia in comparison with glaucoma without high myopia have been reported previously and can be roughly categorized as structural and vascular factors.
Among the structural factors, tilted discs and peripapillary atrophy (PPA) have been identified as characteristic findings in myopic eyes. Park et al reported an association between optic disc torsion and VF defects in myopic NTG,25 and multiple studies have described abnormalities of the optic nerve head (ONH) in myopic glaucoma.26,27 Han et al reported the findings for deep ONH parameters, which indicated that the obliqueness of optic nerve insertion into the eyeball was related with the presence of myopic NTG.28,29 These reports suggest that myopic NTG involves mechanisms of optic neuropathy other than IOP elevation. Recent advances in the evaluation of microcirculation in and around the optic disc using OCT angiography have suggested that abnormal blood flow in the ONH is involved in the pathogenesis of myopic NTG. Hong et al revealed that deep vessel density or its fluctuations are associated not only with PPA but also with central VF defect.30 Kiyota et al reported that microcirculation deep within the PPA is associated with central retinal structure and visual function in myopic NTG.31 Indeed, Seol et al reported that IOP reduction could suppress progression in NTG with myopic disc and that such progression was associated with disc hemorrhage in the same article.32 We hypothesize that these non-pressure-dependent factors drive the progression of VF deterioration even after achievement of IOP reduction.
This study has several limitations that should be considered when interpreting the findings. To exclude the effects of other surgeries, such as trabeculotomy, we only included eyes that underwent Trab MMC as the primary surgery, which limited the sample size. Moreover, the selection criteria for the number of VF tests further reduced the eligible sample size. In addition, due to statistical limitations, we could not include cases in which Trab MMC was performed immediately after referral and those in which the HFA testing protocol was changed from 24–2 to 10–2 postoperatively because of VF loss outside 10° or the need for detailed evaluation of paracentral scotoma. Furthermore, owing to the limited sample size we could not exclude cases that underwent cataract surgery before, after, or combined with Trab MMC. Thus, it is fair to consider that the results are biased to some degree.
In conclusion, Trab MMC reduced IOP in both highly myopic and non-highly myopic eyes, and IOP reduction was very similar in both groups. The VF deterioration rate decreased in both groups, and the change was significant in the non-highly myopic group, but weaker and not significant in the highly myopic group. Since Trab MMC appears to show IOP-reducing and some VF-protecting effects in highly myopic eyes, we believe it can be recommended for eyes showing high IOP and VF progression regardless of axial length; however, further verification of the VF-protecting effects in highly myopic eyes is required in the future.
Abbreviations
BCVA, best-corrected visual acuity; CI, confidential interval; GEE, generalized estimating equation; HFA, Humphrey Visual Field Analyzer; IOL, intraocular lens; IOP, intraocular pressure; LMM, linear mixed models; MD, mean deviation; NTG, normal-tension glaucoma; OCT, optical coherence tomography; ONH, optic nerve head; PPA, peripapillary atrophy; TD, total deviation; Trab MMC, trabeculectomy with mitomycin C; VF, visual field.
Acknowledgment
The authors thank Dr. Masanori Hangai and Dr. Hideo Nakanishi for their support as glaucoma surgeons in charge of the patients in the current study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999;106(10):2010–2015. doi:10.1016/S0161-6420(99)90416-5
2. Xu L, Wang Y, Wang S, Wang Y, Jonas JB. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology. 2007;114(2):216–220. doi:10.1016/j.ophtha.2006.06.050
3. Suzuki Y, Iwase A, Araie M, et al. Risk factors for open-angle glaucoma in a Japanese population: the Tajimi Study. Ophthalmology. 2006;113(9):1613–1617. doi:10.1016/j.ophtha.2006.03.059
4. Marcus MW, De Vries MM, Junoy Montolio FG, Jansonius NM. Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology. 2011;118(10):1989–1994.e2. doi:10.1016/J.OPHTHA.2011.03.012
5. Sakata R, Aihara M, Murata H, et al. Contributing factors for progression of visual field loss in normal-tension glaucoma patients with medical treatment. J Glaucoma. 2013;22(3):250–254. doi:10.1097/IJG.0b013e31823298fb
6. Qiu C, Qian S, Sun X, Zhou C, Meng F. Axial myopia is associated with visual field prognosis of primary open-angle glaucoma. PLoS One. 2015;10(7):e0133189. doi:10.1371/JOURNAL.PONE.0133189
7. Lee JY, Sung KR, Han S, Na JH. Effect of myopia on the progression of primary open angle glaucoma. Invest Ophthalmol Vis Sci. 2015;56(3):1775–1781. doi:10.1167/iovs.14-16002
8. Perdicchi A, Iester M, Scuderi G, Amodeo S, Medori EM, Recupero SM. Visual field damage and progression in glaucomatous myopic eyes. Eur J Ophthalmol. 2007;17(4):534–537. doi:10.1177/112067210701700409
9. Lee YA, Shih YF, Lin LLK, Huang JY, Wang TH. Association between high myopia and progression of visual field loss in primary open-angle glaucoma. J Formos Med Assoc. 2008;107(12):952–957. doi:10.1016/S0929-6646(09)60019-X
10. Gaasterland DE, Ederer F, Beck A, et al. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–440. doi:10.1016/S0002-9394(00)00538-9
11. Sohn SW, Song JS, Kee C. Influence of the extent of myopia on the progression of normal-tension glaucoma. Am J Ophthalmol. 2010;149(5):831–838. doi:10.1016/j.ajo.2009.12.033
12. Araie M. Visual field damage in myopic glaucoma. In: Myopia and Glaucoma. Springer Nature; 2015:65–73.
13. Mayama C, Suzuki Y, Araie M, et al. Myopia and advanced-stage open-angle glaucoma. Ophthalmology. 2002;109(11):2072–2077. doi:10.1016/S0161-6420(02)01175-2
14. Bertrand V, Fieuws S, Stalmans I, Zeyen T. Rates of visual field loss before and after trabeculectomy. Acta Ophthalmol. 2014;92(2):116–120. doi:10.1111/aos.12073
15. Shigeeda T, Tomidokoro A, Araie M, Koseki N, Yamamoto S. Long-term follow-up of visual field progression after trabeculectomy in progressive normal-tension glaucoma. Ophthalmology. 2002;109(4):766–770. doi:10.1016/S0161-6420(01)01009-0
16. Tanaka D, Nakanishi H, Hangai M, et al. Influence of high myopia on outcomes of trabeculectomy with mitomycin C in patients with primary open-angle glaucoma. Jpn J Ophthalmol. 2016;60(6):446–453. doi:10.1007/s10384-016-0468-7
17. Akagi T, Nakanishi H, Yoshimura N. Morphological changes after trabeculectomy in highly myopic eyes with high intraocular pressure by using swept-source optical coherence tomography. Am J Ophthalmol Case Rep. 2016;3:54–60. doi:10.1016/j.ajoc.2016.06.006
18. Anderson DR. Automated Static Perimetry.
19. Jonas JB, Panda-Jonas S, Wang YX. Glaucoma neurodegeneration and myopia. Prog Brain Res. 2020;257:1–17. doi:10.1016/BS.PBR.2020.06.014
20. Shin JW, Song MK, Sung KR. Longitudinal macular ganglion cell-inner plexiform layer measurements to detect glaucoma progression in high myopia. Am J Ophthalmol. 2021;223:9–20. doi:10.1016/J.AJO.2020.09.039
21. Dally LG, Ederer F, Gaasterland D, et al. The Advanced Glaucoma Intervention Study (AGIS): 11. Risk factors for failure of trabeculectomy and argon laser trabeculoplasty. Am J Ophthalmol. 2002;134(4):481–498. doi:10.1016/S0002-9394(02)01658-6
22. Landers J, Martin K, Sarkies N, Bourne R, Watson P. A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology. 2012;119(4):694–702. doi:10.1016/J.OPHTHA.2011.09.043
23. Park HYL, Yi R, Jung Y, Park CK. Effect of glaucoma surgery on the progression rate and pattern in glaucoma patients with myopia. Invest Ophthalmol Vis Sci. 2016;57(10):4170–4179. doi:10.1167/iovs.16-19564
24. Naito T, Fujiwara M, Miki T, et al. Effect of trabeculectomy on visual field progression in Japanese progressive normal-tension glaucoma with intraocular pressure < 15 mmHg. PLoS One. 2017;12(8):1–12. doi:10.1371/journal.pone.0184096
25. Park HY, Lee K, Park CK. Optic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopia. Ophthalmology. 2012;119(9):1844–1851. doi:10.1016/j.ophtha.2012.03.006
26. Lan YW, Chang SY, Sun FJ, Hsieh JW. Different disc characteristics associated with high myopia and the location of glaucomatous damage in primary open-angle glaucoma and normal-tension glaucoma. J Glaucoma. 2019;28(6):519–528. doi:10.1097/IJG.0000000000001217
27. Park HYL, Shin DY, Jeon SJ, et al. Predicting the development of normal tension glaucoma and related risk factors in normal tension glaucoma suspects. Sci Rep. 2021;11(1). doi:10.1038/S41598-021-95984-7
28. Han JC, Lee EJ, Kim SB, Kee C. The characteristics of deep optic nerve head morphology in myopic normal tension glaucoma. Invest Ophthalmol Vis Sci. 2017;58(5):2695–2704. doi:10.1167/IOVS.17-21791
29. Clark RA, Suh SY, Caprioli J, et al. Adduction-induced strain on the optic nerve in primary open angle glaucoma at normal intraocular pressure. Curr Eye Res. 2021;46(4):568–578. doi:10.1080/02713683.2020.1817491
30. Hong KE, Kim SA, Shin DY, Park CK, Lopilly Park HY. Ocular and hemodynamic factors contributing to the central visual function in glaucoma patients with myopia. Invest Ophthalmol Vis Sci. 2022;63(5). doi:10.1167/IOVS.63.5.26
31. Kiyota N, Kunikata H, Takahashi S, Shiga Y, Omodaka K, Nakazawa T. Factors associated with deep circulation in the peripapillary chorioretinal atrophy zone in normal-tension glaucoma with myopic disc. Acta Ophthalmol. 2018;96(3):e290–e297. doi:10.1111/aos.13621
32. Seol BR, Kim S, Kim DM, Park KH, Jeoung JW, Kim SH. Influence of intraocular pressure reduction on progression of normal-tension glaucoma with myopic tilted disc and associated risk factors. Jpn J Ophthalmol. 2017;61(3):230–236. doi:10.1007/S10384-017-0508-Y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.