Back to Journals » Patient Preference and Adherence » Volume 17
Influence of Reminder on Enhancing Compliance in Patients with Fixed Orthodontic Appliance Treatment (a Randomized Controlled Clinical Trial)
Received 11 May 2023
Accepted for publication 5 July 2023
Published 20 July 2023 Volume 2023:17 Pages 1759—1769
DOI https://doi.org/10.2147/PPA.S418109
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Shara Hussein, Hadi Ismail
Department of Pedodontics, Orthodontics and Preventive Dentistry, College of Dentistry, University of Sulaimani, Sulaimanyah, Iraq
Correspondence: Hadi Ismail, House 11, Street 47, County 215 Majeedbag, Sulaimanyah, 46001, Iraq, Tel +9647702106211, Email [email protected]
Purpose: Patient compliance during orthodontic treatment has a significant effect on the aims, outcome, and duration of the treatment. The aim of this study is to evaluate the influence of reminders on enhancing orthodontic patient compliance.
Patients and Methods: Twenty-six subjects undergoing orthodontic treatment with fixed appliances were randomly assigned into two groups: control (Ct) and intervention (In) groups. The oral hygiene parameters of plaque index (PI), bleeding index (BI), and white spot lesion (WSL) with appointment adherence and bracket fracture were recorded at base line (T0), 2 months (T1), 4 months (T2), and 6 months (T3). In group participants received weekly reminders and subjects’ compliances were classified into poor, fair, and excellent compliance.
Results: Statistically significant differences were found in PI level at T2 between Ct and In groups (p-value = 0.006), whereas a non-significant difference was found for BI (p-value> 0. 05). There was a statistically significant increase in WSL for the Ct group across the study time points (p-value = 0.03), while no significant change in WSL was detected for the In group (p-value> 0.05). The compliance levels of In and Ct groups were excellent and fair, respectively.
Conclusion: The study suggests that weekly reminders can enhance the oral hygiene status in patients with orthodontic appliances (POA) and elevate the level of compliance to excellent.
Registration number: ClinicalTrials.gov NCT05331820.
Keywords: orthodontic patient compliance, oral hygiene, reminder systems, white spot lesions
Introduction
The effectiveness of orthodontic treatment is reliant on four main components: the orthodontist’s therapeutic and diagnostic skills, the patient’s desirable biological features (bone turnover, craniofacial anatomy, growth stage, etc.), patient compliance, and the use of efficient and appropriate orthodontic appliances. Patient compliance has been reported to have a major impact on the treatment’s goals, outcomes, and duration. However, patient compliance remains the weakest link in the chain because it is the least predictable aspect of orthodontic treatment planning.1 Patient compliance is defined as patients’ cooperation with the orthodontist to enhance the quality of treatment, including adherence to appointment attendance, following instructions provided by the orthodontist, complying with oral hygiene measures as recommended, and caring about the orthodontic appliance.2–4
The level of dental plaque in patients with orthodontic appliances (POA) is two to three times higher than in those who do not wear appliances.5 In addition to making routine oral hygiene measures more challenging, fixed orthodontic appliances lead to an increase in the number of plaque retention sites on tooth surfaces that are typically less vulnerable to caries formation.6 Therefore, the most common consequences of dental biofilm development amongst POA are enamel demineralization and gingivitis in 50–70% of POA.7 A few POA may experience extensive or severe demineralization, however, the majority of them will experience at least one mild white spot lesion (WSL).8
Attendance at orthodontic appointments impacts the results of orthodontic treatment, length of treatment, and associated side effects and is also considered as an indicator of compliance. Bracket fracture, which is a frequent occurrence during orthodontic treatment, is a setback. It not only increases the treatment duration but destroys the enamel due to repeated acid etching, interrupts the treatment, causes discomfort, and adds extra cost for the patients.9
Several studies constructed classifications to describe levels of patient compliance.10–14 Each one of these studies uses a different method of classification. In the current research, a method of classification was established (Index of Orthodontic Patient Compliance [IOPC]) to classify the participants and the group.
Life in the 21st century is symbolized by the slide and swipe culture. Digital platforms have been integrated into the dentistry world and used by dentists and orthodontists to improve patient experience, satisfaction, safety, and clinical decision-making. Behavioral management by positive reinforcement via reminders and motivating instructions might be a practical approach to managing and achieving optimal compliance in patients undergoing orthodontic treatment. To the best of our knowledge, this approach has not previously been examined. Therefore, this study aimed to assess the influence of weekly reminders via social applications on compliance of POA.
Patients and Methods
Study Design
This controlled clinical trial was a double center, randomized, two parallel group, 6 months follow up study. Prior to the start of the study, the Ethics Committee of the College of Dentistry, University of Sulaimani approved the research protocol and consent form (modified from the World Health Organization WHO template) with approval number: 54/21. This study corresponds to the ethical standards governing medical research with human subjects as stated in the World Medical Association’s Helsinki Declaration. The study was registered at ClinicalTrials.gov with the identifier NCT05331820. The trial was carried out and reported in conformity with the guidelines of the Consolidated Standards of Reporting Trials (CONSORT).
A total of 26 participants seeking orthodontic treatment were recruited in two centers: University of Sulaimani Dental Clinic and Suli-orthodontics Center between November 2021 and September 2022. The participants or their parents (in the case of being aged under 18) first signed the consent form and filled out a prepared questionnaire before the placement of the fixed appliance, and patient characteristics, starting date, clinical examination of oral hygiene of Plaque Index (PI), Bleeding Index (BI), and WSL were then recorded.
Using a simple randomization technique, the study subjects were divided between two groups: control (Ct) and Intervention (In), with 13 subjects in Ct and 13 subjects in In group. The participants assigned to the In group received weekly reminders through Viber or WhatsApp, whichever was available, and individual messages were sent to protect their privacy. The reminders related to oral hygiene measures, appliance care, and importance of adherence to scheduled appointments in the form of text, photo, video. Text message related to importance of adherence to appointments and types of food that causes fracture of appliance. Photos were showing consequences of poor oral hygiene and instructional videos to improve oral hygiene. This motivation and instructional reminders continued for 6 months. The measures that were recorded at baseline (T0) were repeated at 2 months after first record (T1), 4 months after first record (T2), and six months after first record (T3) in the record form, as well as any information on appliance fracture or scheduled appointments that were missed or canceled. The T0 records was taken before placement of orthodontic appliance and the same records of PI, BI, and WSL were repeated at T1, T2, T3.
Study Population
The targeted population was patients seeking orthodontic treatment. The inclusion criteria were patients that were starting fixed orthodontic appliance treatment for both jaws and for the first time, both genders, aged 15–30 years old, with good gingival health, and having access to smartphone and Internet connection. The included malocclusion levels of the patients undergoing treatment, according to the Index of Orthodontic Treatment Need (IOTN), were grades 1, 2 and 3, without severe crowding. Different operators bonded the fixed appliance in direct method. Patients with a removable appliance, cleft lip and palate, severe hypo mineralization visible on anterior teeth, susceptibility to periodontal disease, diabetes, disabled patients, and those with severe malocclusion above IOTN grade 3, and ceramic brackets were excluded.
Randomization and Intervention
The study subjects were randomly divided between two groups: In and Ct, by simple randomization using an online computer generator program with allocation ratio of 1:1. At the beginning of the study, every participant, regardless of type of study group received detailed audiovisual instructions on how to brush their teeth, floss, and take care of the appliance to prevent fracture. Orthodontic models were used to show the brushing techniques with flossing. Oral hygiene instruction and motivation lasted 10–15 minutes, including a demonstration on dental models of how to clean teeth with braces by brushing after each meal, use of floss and interdental brush. Every participant received a standard orthodontic brush kit which contained tooth brush, travel tooth brush, interdental brush, floss, dental mirror, Hourglass timer, dental floss threaders, orthodontic wax, orthodontic mouth wash and toothpaste (Kin laboratories, Orthokin, Barcelona, Spain). In addition, instruction on how to avoid fracture of the bracket, which type of food to avoid, and importance of avoiding direct bite on food.
The importance of attending scheduled appointments was provided. Attendance at scheduled appointments was listed as a factor in the success of the expected duration of orthodontic treatment. Weekly reminders were sent to In group participants that contained written instructions, photos and video about oral hygiene, and information on appliance care, and appointment adherence. The participants in the Ct group did not receive the reminders.
Reliability
To ensure the reliability of the clinical measurements, the clinical examiner received appropriate training. Every patient at every record time was examined by the same clinical examiner to ensure there was no difference in examination procedure and scoring of indexes.
Sample Size Calculation
The sample size was based on previous studies of BI change difference between two groups by using G power version 3.1.9.6 (Franz Faul University, Kiel, Germany) to achieve 80% power and considering an alpha error of 0.05. This resulted in a sample size of 13 participants per group.15
Primary and Secondary Outcomes: Clinical Assessment and Method
First, the clinical parameters of PI16 and BI17 of buccal surfaces of all teeth were recorded. Visual clinical examination was carried out to check for WSL after drying the tooth surface for 5 seconds and taking a picture with a Canon EOS 850D (Rebel T8i) DSLR Camera fitted with a Canon EF 100 mm f/2.8 L Macro IS USM Lens. The upper and lower anterior teeth were examined and divided into four parts (upper mesial, upper distal, lower mesial, and lower distal).
The second component of the record form was appliance care. The number of bracket fractures and cause of the fracture were recorded between the time points T0 and T3. The third component was adherence to scheduled appointments, and the number of appointments missed was recorded as one mark if the patient had been informed of the schedule within the past month. The numbers of brackets that had debonded and appointments missed were recorded as a cumulative record from the initial time point until the end of the trial.
Classification of Compliance
For a clear and understandable classification of patient compliance, we developed an index named Index of Orthodontic Patient Compliance (IOPC), shown in Table 1, which includes all aspects of patient compliance (oral hygiene, appointment adherence, appliance care) and grades patients as poor, fair, or excellent. These grades depend on scores that are given to patients based on the compliance table and ranging from 5 to 15. Scores below 7 are regarded as poor, from 7–11 as fair compliance and above 11 as excellent compliances.
 |
Table 1 Index of Orthodontic Patient Compliance (IOPC) |
Statistics
The collected data were analyzed using the Statistical Package for Social Sciences version 23 (SPSS Inc., Chicago, IL, USA). Shapiro–Wilk test was used for testing the normality of the data. The effects of patient characteristics including age, gender, occupation, treatment center, and motivation to start treatment on their level of compliance (PI, BI, WSL, bracket fracture, and appointment adherence) were analyzed using the Spearman correlation test. P-value was obtained for the continuous variable using nonparametric test 2-Independent Samples Test (Mann–Whitney U, Friedman test) and Kruskal–Wallis H was used for comparing the median and interquartile range. The Wilcoxon signed-rank test was used to evaluate whether the median difference between the paired variables was statistically significant. For categorical variables the odds ratio was used with a 95% confidence interval to determine significant associations between categorical dependent and independent variables, with P-value considered significant if it was less than 0.05.
Result
A total of 25 patients successfully completed the study. A CONSORT diagram showing the flow of participants through the study is presented in Figure 1. Frequency and distribution of participants in each group and in total are shown in Table 2. Matching samples from the two groups showed significant difference in age p-value = 0.04, and education level p-value = 0.01. Results of comparing the In and Ct groups for PI and BI across the study time points are shown in Table 3. As seen in Figure 2, both the In and Ct groups experienced changes in their PI over time. Examining BI changes in the two groups revealed that BI in the In group decreased from 0.075 to 0.05, while in Ct group it increased from 0.32 to 0.35 (Figure 3).
 |
Table 2 Distribution of Participants in the Study |
 |
Table 3 Median and Interquartile Range of PI and BI in Both Groups |
 |
Figure 1 CONSORT flow diagram. |
 |
Figure 2 Plaque Index change over time. Median (interquartile range). |
 |
Figure 3 Bleeding Index changes over time. Median (interquartile range). |
The results of 2-tailed T-test revealed that the linear correlation of BI in Ct group between T1 and T2 and in In group between T0 and T2 was statistically significant (p-value = 0.039) (p-value = 0.002). Results from Wilcoxon signed-rank test for investigation in between follow ups in the groups is shown in Table 4. There was a significant increase in WSL of Ct group from the beginning of the trial to the last follow up (p-value = 0.03), whereas no significant change in the In group was observed (p-value>0.05). Furthermore, there were no significant differences between the Ct and In group in terms of the times of missed appointments, times of cancelled appointments, and bracket fractures (p-value>0.05).
 |
Table 4 Significant Differences Within Follow-Up Time Points |
The results of the current study regarding relationships between personal characteristics and the other research variables indicated that only the following significantly related:
- Education level and mean PI at T1 (p-value = 0.042),
- Education level and mean BI at T1 and T2 (p-value = 0.001),
- Occupation with PI at T0 (p-value = 0.005),
- Age group with mean PI at T0 (p-value = 0.008),
- Residency with bracket fracture (p-value = 0.042).
The groups’ total PI, BI, WSL, number of bracket fractures, and number of appointments missed were calculated and scored based on the IOPC table as shown in Table 5.
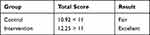 |
Table 5 Total Group Scores Based on the IOPC Table |
Discussion
In the current study, all elements of patient compliance were considered to assess the effect of reminders on orthodontic patient compliance. According to the findings based on the Index of orthodontic patient compliance IOPC (Table 5), the In group had excellent compliance compared to the Ct group (fair compliance). This enhancement can be attributed to the role of reminders regarding the components of compliance that were investigated, since the participants in the In group gained excellent scores in more than half of the components of compliance. For a patient with excellent compliance, the treatment can be performed exactly as planned, with no difficulties arising due to poor oral hygiene, appliance breakage, or missed appointments.
The inclusion criteria for this study were designed from the start to avoid any cofounding factors that could influence the results. Patients with upper and lower fixed appliances were included because fixed appliance attachments create the most difficulties in oral hygiene maintenance.6 In contrast, removable appliances have a shorter treatment duration and greater simplicity of maintaining dental hygiene. Regardless of this fact, surprisingly, some studies did not specifically include removable appliance treatment as an exclusion criterion,18 which may have affected their results.
The current study differed from earlier studies showing positive benefits of text messaging in that the reminders were delivered to the patients rather than the parents. The participants of this study were above 15 years old, had mobile devices with Internet connection, on which they were able to receive direct reminders. When their children are already in treatment, parents are frequently more motivated than their children,19 so sending a reminder through parents has an indirect influence.
In the research by Cozzani et al20 and the present research, patients were included from the beginning and before the placement of the fixed appliance in order to prevent participants having varying experience with the fixing of the appliance. A few studies21,22 included patients who were already receiving treatment, which may have influenced the results. Also this is the main reason type of wires are not part of inclusion criteria for the research as participants were in progress of wire beginning from niti and some of them have reached stainless steel wire.
Comparable studies have also utilized the PI for assessing patient compliance,20,22,23 since it is a significant measure for evaluating a patient’s motivation and level of self-care while undergoing treatment, in addition to oral hygiene.24 Also, due to its excellent sensitivity and specificity in assessing periodontal health, the BI is a reliable predictor of oral hygiene compliance.25
Similar to the results of the current study, in a study by Eppright et al,15 it was reported that an initial decline in oral hygiene following the placement of fixed appliances was followed by an improvement in oral hygiene compliance at the fifth month of treatment. But the results in this study differ in that the enhancement was recorded at the second follow up, which was 4 months after bracket placement. A short decline after initial bonding was seen clearly in the current study because the records began at the start of placement and the decline in oral hygiene was obvious at the first follow up.
Both groups’ participants had increased plaque at T1, although the In group had a lower level of plaque than the Ct group, but at T2, both groups recorded a significant drop in PI values. With the exception of the intervention during the follow-up check, oral hygiene reinforcement was carried out irrespective of the participants’ group. The fact that patients were aware they were a part of a study may have contributed to this trend of change by encouraging better oral hygiene practices among patients in the Ct group. Patients in the Ct group also received oral hygiene instruction and encouragement during follow-up visits, and the records helped them recall that they were participating in research. Results may have been affected as a result of oral hygiene instructions being given to both groups at the start of the trial and repeated at each appointment. Effective oral hygiene requires a combination of frequency and proper technique. Previous studies showed that repeated oral hygiene instruction and motivation with a hygienist significantly improved plaque scores in orthodontic patients.26
Based on the data achieved from the present study, the BI was increased in the Ct group and decreased in the In group. The changes in BI were not significant among the groups. In contrast with the results of our study, Hadzic et al27 and Soheilifar et al28 reported that an increment in the mean value of the BI was observed at each check-up after the placement of a fixed orthodontic appliance. Evaluation of BI measurements among research groups using Pearson correlation coefficient, Spearman Rank Correlation and 2-tailed T-test revealed different results. So, providing reminder programs could be effective in improving BI in patients with fixed orthodontic appliance treatment. Meanwhile, in those patients who were not involved in reminding programs, the BI values did not show a clear trend.
In a similar studies, Baherimoghadam et al29 evaluated the effect of reminders on oral hygiene of POA and reported significant improvement in BI, PI, and gingival index in the reminder group with improvement in the group without message reminder. Moreover, Yashwant et al30 stated that the patients in the reminder group demonstrated statistically significant results over the Ct group. According to the findings of their study, a text message reminder increases the amount of plaque removed at a particular period of time. Another study, by Abdaljawwad et al,31 reported that the reduction in compliance of the patients in the Ct group may be attributed to the fact that they did not receive reminders. Bowen et al32 also obtained similar results. Salil et al33 concluded that sending a once weekly text message is a useful way to improve oral hygiene compliance over a period of 4 months. They finally stated that reminders can efficiently promote oral hygiene in patients undergoing removable orthodontic treatment.
Our data revealed that in all participants, WSLs that were observed in initial records increased in their final records. Srivastava et al34 reported that demineralization is an inevitable side-effect associated with fixed orthodontic treatment, especially when associated with poor oral hygiene. Development of WSL in POA has been reported to range from 19.44%35 to 68.4%.36 In our study 64% of the participants had WSL by the end of study follow ups. Based on the findings of the present study there was no significant change in the initial and final records of WSL in the In group over time, while these changes in the Ct group were significant over time. Based on these findings, providing reminder facilities to the patients improves their compliance with provided treatment and decreases their WSL. In line with the data presented in this study, Weyland et al37 reported that occurrence of WSLs during fixed orthodontic appliance treatment can be prevented through reminder programs.
Common characteristics of non-compliant patients include a fractured appliance and a debonded bracket.38 The current study participants had a mean of 1.7 bracket fractures and no significant difference was found between the groups.
Regular reminders would be an excellent tool for preventing patients forgetting appointments.9 Furthermore, the reminders provide the patient with the option of canceling the appointment if required. In this study, patients were reminded of the importance of appointment adherence rather than the schedule of their appointments. As a result, there were no significant differences between the groups in terms of numbers of missed and canceled appointments. Consequently, providing or not providing this type of reminders may not significantly affect appointment adherence among patients.
Several studies constructed classifications for describing levels of patient compliance.10–14 Participants in the research by Cucalon10 were divided into three groups based on their level of compliance: good, fair, or poor. The following factors were utilized to determine compliance: 1) oral hygiene; 2) appliance upkeep and care; 3) rubber band and/or headgear wear; and 4) missing and/or arriving late for orthodontic appointments. A different study applied the same criteria to determine compliance at the completion of active orthodontic treatment and the patients were split into two groups: good compliance and poor compliance.11
Another study applied a different scoring method and variables to assess patients for total compliance, based on 10 scored variables, with scores ranging from 1 (very poor) to 5 (excellent). Performance in terms of wearing headgear, wearing elastics, oral hygiene, keeping appointments, willingness to adhere to instructions, preventing broken appliances, cooperating during appliance placement and adjustment, general attitude, and parental attitude were among the compliance factors that were scored.12 The classification of fully, fairly, and poor compliant was employed again in a further study, with scores ranging from 1–5, excellent to poor.13 More information about the scoring was given in a retrospective study,14 with the clinician recording incidences of poor oral hygiene, inadequate elastic wear, and unsuccessful or troublesome visits and collating these entries for classification. As a result, based on this classification, excellent compliers significantly assisted treatment, poor compliers significantly hampered treatment, and in medium compliers ordinary orthodontic treatment proceeded in a typical manner.
An IOPC was established in this study to score the components of patient compliance. According to the findings on this study’s participants, the In group had excellent compliance and the Ct group had fair compliance. This variation in compliance can be related to the effect of reminders on participants. As opposed to classifications used in earlier research, this method brings together all the components of patient compliance to designate the participants as having excellent, fair, or poor compliance. This classification method would have been better with larger sample size and a limitation of the IOPC index is that it does not include elastics, headgear, removable appliances, or aligners. This can be related to the inclusion criteria regarding participants’ age and fixed orthodontic appliance, also the fact that recording started at the beginning of the treatment, whereas treatment with elastics usually starts later.
Conclusion
The result of this study suggests that text reminders can enhance compliance of orthodontic patients and oral hygiene status. This article is notable for its investigation and evaluation of the all main key factors contributing to patient compliance and also is distinguished by its creation of a unique and profound index for the classification of compliance. Its recommended for future trials to use the index on larger sample size when comparing groups of different intervention. Orthodontists should incorporate an active reminder system regarding the importance of oral hygiene compliance into their standard treatment protocol and when reminders are added to protocol it should remind the patient exact date of appointment and not a generalized reminder. Reminders may therefore provide a useful adjunct to adherence-enhancing strategies.
Abbreviations
PI, Plaque Index; BI, Bleeding Index; WSL, white spot lesion; IOPC, Index of Orthodontic Patient Compliance; POA, patients with orthodontic appliance.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Consent form, questionnaire form, and record form will be available when requested.
For request please contact correspondence author Hadi Ismail at Email: [email protected]
Acknowledgments
The authors of this research want to thank the participants of the clinical trial, the colleagues, and the private clinic staff.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chow J, Cioffi I. Pain and orthodontic patient compliance: a clinical perspective. Semin Orthod. 2018;24(2):242–247. doi:10.1053/j.sodo.2018.04.006
2. Bukhari OM, Sohrabi K, Tavares M. Factors Affecting Patients’ Adherence to Orthodontic Appointments. Vol. 149. Mosby Inc.;2016:319–324. doi:10.1016/j.ajodo.2015.07.040
3. Barbosa IV, Ladewig V de M, Almeida-Pedrin RR, Cardoso MA, Santiago Junior JF, Conti AC. The association between patient’s compliance and age with the bonding failure of orthodontic brackets: a cross-sectional study. Prog Orthod. 2018;19(1):1–5. doi:10.1186/s40510-018-0209-1
4. Anuwongnukroh N, Dechkunakorn S, Kanpiputana R. Oral hygiene behavior during fixed orthodontic treatment. Dentistry. 2017;7(10). doi:10.4172/2161-1122.1000457
5. Klukowska M, Bader A, Erbe C, et al. Plaque levels of patients with fixed orthodontic appliances measured by digital plaque image analysis. Am J Orthod Dentofac Orthop. 2011;139(5). doi:10.1016/j.ajodo.2010.05.019
6. Øgaard B. White Spot Lesions During Orthodontic Treatment: mechanisms and Fluoride Preventive Aspects. Semin Orthod. 2008;14(3):183–193. doi:10.1053/J.SODO.2008.03.003
7. Palomares NB, Celeste RK, Oliveira BH, Miguel JAM. How does orthodontic treatment affect young adults’ oral health-related quality of life? Am J Orthod Dentofac Orthop. 2012;141(6):751–758. doi:10.1016/j.ajodo.2012.01.015
8. Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ. Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod. 2011;81(2):206–210. doi:10.2319/051710-262.1
9. Li X, Xu ZR, Tang N, et al. Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clin Oral Investig. 2016;20(8):1849–1859. doi:10.1007/s00784-015-1662-6
10. Cucalon A 3rd, Smith RJ. Relationship between compliance by adolescent orthodontic patients and performance on psychological tests. Angle Orthod. 1990;60(2):107–114.
11. Lee S-J, Ahn S-J, Kim T-W. Patient compliance and locus of control in orthodontic treatment: a prospective study. Am J Orthod Dentofac Orthop off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2008;133(3):354–358. doi:10.1016/j.ajodo.2006.03.040
12. Southard KA, Tolley EA, Arheart KL, Hackett-Renner CA, Southard TE. Application of the Millon Adolescent Personality Inventory in evaluating orthodontic compliance. Am J Orthod Dentofac Orthop off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 1991;100(6):553–561. doi:10.1016/0889-5406(91)70097-G
13. Pinskaya YB, Hsieh TJ, Roberts WE, Hartsfield JK. Comprehensive clinical evaluation as an outcome assessment for a graduate orthodontics program. Am J Orthod Dentofac Orthop. 2004;126(5):533–543. doi:10.1016/j.ajodo.2004.05.017
14. Skidmore KJ, Brook KJ, Thomson WM, Harding WJ. Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofac Orthop. 2006;129(2). doi:10.1016/j.ajodo.2005.10.003
15. Eppright M, Shroff B, Best AM, et al. Influence of active reminders on oral hygiene compliance in orthodontic patients. Angle Orthod. 2014;84(2):208–213. doi:10.2319/062813-481.1
16. World Health Organization. Oral Health Surveys - Basic Methods.
17. Saxton CA, van der Ouderaa FJ. The effect of a dentifrice containing zinc citrate and Triclosan on developing gingivitis. J Periodontal Res. 1989;24(1):75–80. doi:10.1111/j.1600-0765.1989.tb00860.x
18. Jones G, Goldsmith R, O’donnell K. Reminder systems during orthodontic treatment. Evid Based Dent. 2018;19(4):109–110. doi:10.1038/SJ.EBD.6401342
19. Daniels AS, Seacat JD, Inglehart MR. Orthodontic treatment motivation and cooperation: a cross-sectional analysis of adolescent patients’ and parents’ responses. Am J Orthod Dentofac Orthop off Publ Am Assoc Orthod Its Const Soc Am Board Orthod. 2009;136(6):780–787. doi:10.1016/j.ajodo.2007.11.031
20. Cozzani M, Ragazzini G, Delucchi A, et al. Oral hygiene compliance in orthodontic patients: a randomized controlled study on the effects of a post-treatment communication. Prog Orthod. 2016;17(1). doi:10.1186/s40510-016-0154-9
21. Sujay Kumar G, Kashyap A, Raghav S, Bhardwaj R, Singh A, Guram G. Role of text message reminder on oral hygiene maintenance of orthodontic patients. J Contemp Dent Pract. 2018;19(1):98–101. doi:10.5005/JP-JOURNALS-10024-2219
22. Alkadhi OH, Zahid MN, Almanea RS, Althaqeb HK, Alharbi TH, Ajwa NM. The effect of using mobile applications for improving oral hygiene in patients with orthodontic fixed appliances: a randomised controlled trial. J Orthod. 2017;44(3):157–163. doi:10.1080/14653125.2017.1346746
23. Zotti F, Dalessandri D, Salgarello S, et al. Usefulness of an app in improving oral hygiene compliance in adolescent orthodontic patients. Angle Orthod. 2016;86(1):101–107. doi:10.2319/010915-19.1
24. Lima IFP, De Andrade Vieira W, De Macedo Bernardino I, et al. Influence of reminder therapy for controlling bacterial plaque in patients undergoing orthodontic treatment: a systematic review and meta-analysis. Angle Orthod. 2018;88(4):483–493. doi:10.2319/111117-770.1
25. de Souza PHR, De toledo BEC, Rapp GE, Zuza EP, Neto CB, Mendes AJD. Reliability of bleeding and non-bleeding on probing to gingival histological features. J Int Acad Periodontol. 2003;5(3):71–76.
26. Marini I, Bortolotti F, Parenti SI, Gatto MR, Bonetti GA. Combined effects of repeated oral hygiene motivation and type of toothbrush on orthodontic patients: a blind randomized clinical trial. Angle Orthod. 2014;84(5):896–901. doi:10.2319/112113-856.1
27. Hadzic S, Gojkov-Vukelic M, Pasic E, et al. Evaluation of Periodontal Changes in Patients Before, During, and After a Fixed Orthodontic Therapy. Mater Sociomed. 2022;34(2):121–125. doi:10.5455/msm.2022.34.121-125
28. Soheilifar S, Soheilifar S, Javanshir B, Malekshoar M, Mohamadi Z. Recovery of Clinical Periodontal Parameters After Orthodontic Appliance Removal: a Prospective Study. Iran J Orthod. 2019. doi:10.5812/ijo.55047
29. Baherimoghadam T, Naseri N, Hamedani S, Nikmehr S, Mokhtar M. Influence of Multimedia Reminders on Oral Hygiene Status During Removable Orthodontic Treatment: a Randomized Controlled Trial. J Orthod Sci. 2022;11:27. doi:10.4103/jos.jos_193_21
30. Yashwant A, Sankar H, Alexander L, Ammayappan P, Ismail N, Jayavarma A. Influence of Reminders on Oral Hygiene Status in Patients Undergoing Fixed Orthodontic Treatment: a Double-blinded, Clinical Randomized Controlled Trial. SBV J Basic, Clin Appl Heal Sci. 2021;4(3):59–62. doi:10.5005/jp-journals-10082-03125
31. Abdaljawwad A. The Influence of Text Message Reminders on Oral Hygiene Compliance in Orthodontic Patients. Iraqi Dent J. 2016;38:58. doi:10.26477/idj.v38i1.74
32. Bowen TB, Rinchuse DJ, Zullo T, DeMaria ME. The influence of text messaging on oral hygiene effectiveness. Angle Orthod. 2015;85(4):543–548. doi:10.2319/071514-495.1
33. Salil Nene HJ. Does Text Messaging Reminder Help in the Orthodontic Compliance of Patients to Maintain their Oral Hygiene. J Oral Hyg Heal. 2014;02(05):2–5. doi:10.4172/2332-0702.1000152
34. Srivastava K, Tikku T, Khanna R, Sachan K. Risk factors and management of white spot lesions in orthodontics. J Orthod Sci. 2013;2(2):43–49. doi:10.4103/2278-0203.115081
35. Ali A, Ismail H, Amin K. Effect of nanosilver mouthwash on prevention of white spot lesions in patients undergoing fixed orthodontic treatment - a randomized double-blind clinical trial. J Dent Sci. 2022;17(1):249–255. doi:10.1016/j.jds.2021.03.016
36. Sundararaj D, Venkatachalapathy S, Tandon A, Pereira A. Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: a meta-analysis. J Int Soc Prev Community Dent. 2015;5(6):433. doi:10.4103/2231-0762.167719
37. Weyland MI, Jost-Brinkmann P-G, Bartzela T. Management of white spot lesions induced during orthodontic treatment with multibracket appliance: a national-based survey. Clin Oral Investig. 2022;26(7):4871–4883. doi:10.1007/s00784-022-04454-5
38. Tervonen MM, Pirttiniemi P, Lahti S. Development of a measure for orthodontists to evaluate patient compliance. Am J Orthod Dentofac Orthop. 2011;139(6):791–796. doi:10.1016/j.ajodo.2009.10.045
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
