Back to Journals » Clinical Ophthalmology » Volume 17
Influence of Preoperative Parameters on the Ratio of Keratometric Change per Diopter of Attempted Spherical Equivalent (∆K/∆SEQ) for Myopic Correction Within LASIK, PRK, and SMILE
Authors Moshirfar M , Theis JS, Cha DS, Porter KB, Payne CJ , Hoopes PC
Received 15 June 2023
Accepted for publication 21 August 2023
Published 29 August 2023 Volume 2023:17 Pages 2563—2573
DOI https://doi.org/10.2147/OPTH.S423087
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Majid Moshirfar,1– 3 Joshua S Theis,4 David S Cha,5 Kaiden B Porter,4 Carter J Payne,1,6 Phillip C Hoopes1
1Hoopes Vision Research Center, Hoopes Vision, Draper, UT, USA; 2John A. Moran Eye Center, University of Utah School of Medicine, Salt Lake City, UT, USA; 3Utah Lions Eye Bank, Murray, UT, USA; 4University of Arizona College of Medicine Phoenix, Phoenix, AZ, USA; 5Saint Louis University School of Medicine, Saint Louis, MO, USA; 6Department of Ophthalmology, George Washington University School of Medicine and Health Sciences, Washington, DC, USA
Correspondence: Majid Moshirfar, Hoopes Vision Research Center, 11820 S. State St. #200, Draper, UT, 84020, USA, Tel +1 801 568 – 0200, Fax +1 415-476-0336, Email [email protected]
Purpose: To compare 3 of the most common corneal refractive procedures; PRK, LASIK, and SMILE assessing ΔK/ΔSEQ ratio and its correlation with preoperative demographics including age, keratometry, pachymetry, cylinder value, and attempted myopic correction. The goal was to analyze the relative strength of each preoperative parameter in accounting for changes in ∆K/∆SEQ.
Patients and Methods: A total of 370 eyes from 102 male and 97 female patients (173 eyes PRK, 153 LASIK, and 44 SMILE) with ages ranging from 20 to 51 underwent refractive surgery for myopia between − 0.25 and − 7.71 D manifest refraction spherical equivalent (MRSE). All surgeries were performed at a single surgery center in Draper, Utah. The Pentacam was used for all optical measurements and data were gathered pre-operatively and then again 1-year post-operatively. Only patients who achieved emmetropia at a visual acuity of 20/25 or better were included.
Results: The mean ΔK/ΔSEQ ratio for LASIK (0.839 ± 0.020) was significantly greater than that of PRK (0.775 ± 0.022) and SMILE (0.709 ± 0.046). Age was found to negatively correlate with ΔK/ΔSEQ for both LASIK (r = − 0.177) and SMILE (r = − 0.451) procedures. Pre-op keratometry was found to negatively correlate with ΔK/ΔSEQ for LASIK (r = − 0.202) but not for PRK or SMILE. Pre-op pachymetry was not correlated with ΔK/ΔSEQ for any of the procedures. Attempted myopic spherical equivalent (SEQ) correction was positively correlated with ΔK/ΔSEQ for LASIK (r = 0.236), PRK (r = 0.459), and SMILE (r = 0.304). Lastly, pre-op cylinder value was found to be correlated to ΔK/ΔSEQ in SMILE (r = − 0.367), but not in LASIK or PRK.
Conclusion: The ΔK/ΔSEQ ratio not only differs depending on the procedure being done but also by pre-operative factors such as age, keratometry, attempted correction, and cylinder value. Multiple linear regression analysis revealed that the attempted correction had the greatest effect on ∆K/∆SEQ out of all parameters in LASIK and PRK. For SMILE, age had the greatest predictive value of the change in ∆K/∆SEQ. While the exact effect of these parameters will vary by surgeon, all of these should be factored into a refractive surgeon’s nomograms in order to achieve optimal visual outcomes for their patients.
Keywords: cornea, refractive surgery, spherical equivalent, nomogram, keratometry, pachymetry, age, cylinder
A Letter to the Editor has been published for this article.
A Response to Letter by Dr Motwani has been published for this article.
Introduction
Refractive surgery has emerged as a safe and reliable treatment for correcting myopia and astigmatism. As the field continues to develop, clinicians continue to find new methods to optimize visual outcomes for their patients. One such method is accounting for the change in keratometry relative to the change in spherical equivalent from preoperatively to postoperatively. This value (ΔK/ΔSEQ ratio) has a known value of 0.7–0.8 and has been shown to be larger in smaller refractive error corrections and vice versa. This indicates as the amount of refractive change increases, the change in simulated keratometry necessary to achieve that correction decreases.1,2 For instance, to achieve a change in spherical equivalent of 3 diopters, the simulated keratometry value may have to change by 2.7 diopters due to a ∆K/∆SEQ of ~0.9, whereas a change in spherical equivalent of 5 diopters may only necessitate a change in simulated keratometry of 3.75 diopters due to a ∆K/∆SEQ of ~0.75. This allows clinicians to better estimate the amount of correction to be performed for a desired outcome.
Since the inception of refractive surgery, nomograms have been essential in helping surgeons calculate the amount of corneal tissue to remove. By accounting for various preoperative factors, such as age, sex, and preoperative refraction, nomograms are able to increase the accuracy of refractive correction.3,4 Many variables affect refractive surgery outcomes, and failure to account for these in pre-operative planning without the use of nomograms could result in over or under correction, where patients may require additional enhancement or resume dependence on glasses.
One study demonstrated that wavefront-guided LASIK to have a larger ∆K/∆SEQ than wavefront-optimized LASIK, suggesting that surgical technique may influence this ratio.5 Similarly, we hypothesized that ∆K/∆SEQ ratio would change between LASIK, PRK, and SMILE as well as various preoperative characteristics for a given patient. Specifically, the preserved biomechanical corneal strength in SMILE may result in a less malleable ∆K/∆SEQ ratio compared to PRK or LASIK. Accordingly, this study aimed to evaluate the relationship between the change in keratometry and the change in spherical equivalent (SEQ) from pre-operatively to one year post-operatively in laser in situ keratomileusis (LASIK), photorefractive keratectomy (PRK) and small incision lenticule extraction (SMILE). Furthermore, we investigated the correlation of this ratio (∆K/∆SEQ) with various preoperative parameters, including age, keratometry, minimum corneal thickness, attempted corrective change (SEQ), and cylinder value. Ultimately, the goal of this study was to find parameters that influence ∆K/∆SEQ within each refractive surgery and compare the relative strengths of those parameters.
Materials and Methods
This non-randomized, retrospective study was completed at a single tertiary surgery center in Utah, USA. All procedures were completed by a single surgeon, MM. Patients signed an informed consent for all procedures and the use of de-identified data for research. The study and consent procedure were approved by the Hoopes Vision Ethics Committee. The Biomedical Research Alliance of New York (BRANY) Institutional Review Board (#A20-12-547-823) approved this study. This study adhered to the tenets of the Declaration of Helsinki.
This retrospective study included 370 eyes from 102 male and 97 female patients. LASIK was performed on 153 eyes from 83 patients, PRK on 173 eyes from 93 patients, and SMILE on 44 eyes from 22 patients. Patients included in the study were those who underwent myopic corrections of −0.25 to −7.71 D (MRSE) via LASIK, PRK, or SMILE in one or both eyes from the period of June 2020 to March 2022. Only those patients who had a preoperative and one-year postoperative Pentacam (HR; Oculus, Wetzlar, Germany) assessment with a measurement status of “OK” were included. Patients who were unable to undergo LASIK or SMILE due to thin corneas underwent PRK surgery. Only patients with a residual stromal bed of 300 microns or greater and less than 40% percentage tissue altered for LASIK and SMILE were included. For PRK, only patients with at least 400 micron thickness of residual stromal bed were included. Patients with a history of glaucoma, cataracts, corneal diseases (keratoconus, corneal dystrophies), systemic diseases (uncontrolled diabetes, herpes simplex keratoconjunctivitis, etc.), and systemic medication use (long-term corticosteroids, hydroxychloroquine, etc.) were excluded from the study. Additionally, patients who required enhancements and patients with monovision were excluded. All patients achieve emmetropia and had a visual acuity of 20/25 or better.
The keratometry values refer to the anterior simulated keratometry readings, referred to as Sim Ks, provided by the Pentacam. Specifically, the mean Sim K (Km) was examined, calculated as the arithmetic average of the flat (K1) and steep (K2) Sim K’s, which are each measured on a ring in intervals of 15 degrees around the corneal vertex.
Surgical Methods
For LASIK, the FS200 (Alcon Laboratories, Inc., Fort Worth, TX, USA) femtosecond laser was utilized to create a 100µm flap. Corneal ablation for LASIK and PRK was done with the WaveLight EX500 laser system (Alcon Laboratories, Inc., Fort Worth, TX, USA). For LASIK and PRK, a 6.5 mm central zone with a transition zone extending up to 9.0mm was created. For SMILE, the VisuMax 500 kHz femtosecond laser (Carl Zeiss Meditec, Jena, Germany) was utilized to extract the 6.0–6.5mm diameter lenticule using a 120µm corneal cap. Further details of the surgical techniques and post-operative treatment can be found in references for LASIK, PRK, and SMILE.6–8
Statistical Analysis
Statistical analysis of this study was conducted using the applications Microsoft Excel 2016 (Redmond, WA) and IBM SPSS Statistical Software (Armonk, NY). Graphs and tables were created using the same applications. Statistical significance was determined using multiple statistical tests. In order to use both eyes of each patient to increase our overall sample size, generalized estimating equations (GEE) were used to account for the correlation between eyes of the same patient. Shapiro–Wilk test was used to assess normality of data distribution. Demographic data between groups were analyzed using One Way ANOVA to compare means and chi-square analysis to compare proportions. Pearson correlations were performed between preoperative parameters and ∆K/∆SEQ. Multivariate linear regression was then run on correlations found to be significant. For a medium effect size of d = 0.5, a minimum sample size of 42 eyes was calculated for an α-value of 0.05 and power (1- β) of 0.95 using G*Power (version 3.1, Franz Faul, Unversität Kiel, Germany).
Results
Demographic data are summarized in Table 1, which demonstrates that age, male:female ratio, and mean asphericity were not significantly different between LASIK, PRK, and SMILE. However, the SMILE group on average has more myopic sphere (−5.18D) than LASIK (−2.99D, p<0.001) and PRK (−3.33D, p<0.001). Additionally, SMILE has decreased absolute mean cylinder (−0.44D) compared to both than LASIK (−1.02D, p<0.001) and PRK (−0.44D, p<0.001). PRK also has lower minimal corneal thickness (522.66µm) than LASIK (548.90µm, p<0.001) and SMILE (551.86µm, p<0.001). Mean keratometry of PRK (44.18D) was also significantly greater than LASIK (43.81D, p = 0.001) (Table 2).
 |
Table 1 Summary of Patient Demographics |
 |
Table 2 Post-Hoc Analyses for Patient Demographics |
The primary outcome was the ratio of change in Km to the change in SEQ (∆K/∆SEQ). For PRK, this ratio was found to be 0.775± 0.022. For LASIK, the ratio was 0.839 ± 0.020, and SMILE was 0.709 ± 0.046. Each of these findings were statistically different from one another (Figure 1).
Age was found to have a negative correlation with ∆K/∆SEQ for both LASIK (r = −0.177, p = 0.029) and SMILE (r = −0.451, p = 0.002) (Table 3). This suggests that as age increases, the ratio of ∆K/∆SEQ will decrease for LASIK and SMILE patients. While both procedures showed a significant correlation with age on their own, the correlations were not statistically different from one another (p = 0.893). There was no significant correlation found between age and ∆K/∆SEQ in PRK and therefore it was not compared to the other correlations. These findings can be seen in Figure 2.
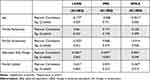 |
Table 3 Correlations Between ∆K/∆SEQ with Independent Variables Across LASIK, SMILE, and PRK |
Pre-op pachymetry values were also assessed for correlation with ∆K/∆SEQ. None of the procedures produced a significant correlation between pre-op pachymetry and resulting ∆K/∆SEQ (Table 3, Figure 3).
Pre-op keratometry (Km) was found to be negatively correlated (r = −0.202) with ∆K/∆SEQ in the LASIK group (p = 0.012), but not the PRK or SMILE cohorts. This indicates that steeper corneas have a lower ratio of ∆K/∆SEQ when undergoing LASIK (Table 3, Figure 4).
Attempted change in SEQ was also tested for correlation with ∆K/∆SEQ across the three procedures. A significant correlation was found among each of the three procedures. PRK showed a positive correlation (r = 0.459, p<0.001) between attempted SEQ change ∆K/∆SEQ. This means that for larger myopes, the ∆K/∆SEQ ratio becomes smaller. This same trend is shared for LASIK (r = 0.236, p = 0.003) and SMILE (r = 0.304, p = 0.045). There was no statistical difference between the correlations of SMILE and LASIK or PRK and LASIK, but a significant difference was observed between PRK’s correlation and SMILE’s (p = 0.031) (Table 3, Figure 5).
Pre-op cylinder was negatively correlated with ∆K/∆SEQ within the SMILE (r = −0.367, p = 0.014) cohort, but not with LASIK or PRK. This suggests that a lower degree of astigmatism relates to a lower ∆K/∆SEQ ratio for patients undergoing SMILE (Table 3, Figure 6).
Stepdown multivariate analyses were run within LASIK, PRK, and SMILE, using the preoperative variables found in Table 1 and examining their effect on ∆K/∆SEQ. In LASIK, both attempted SEQ change and pre-op keratometry independently contributed to the model of predictive value for ∆K/∆SEQ, with attempted SEQ change being a stronger predictor than keratometry. Age, pre-op pachymetry, and pre-op cylinder were excluded from the model due to their lack of significant independent effect on ∆K/∆SEQ once attempted SEQ and pre-op keratometry were taken into account (Adjusted R2: 0.089 Durbin-Watson 1.743). In PRK, only attempted SEQ change independently contributed to the model with all other variables excluded (Adjusted R2: 0.206, Durbin-Watson = 1.356). In SMILE, only age independently contributed to the model with all other variables excluded (Adjusted R2: 0.184, Durbin-Watson = 2.015) (Table 4).
 |
Table 4 Multivariate Regression Analysis of ∆K/∆SEQ Across Three Surgery Groups |
Discussion
This study looked at three populations of refractive surgery patients that were similar in age, male-to-female distribution, and mean asphericity. SMILE patients were obviously more myopic and had less diopters of cylinder than the other two groups. The nature of the procedure can only correct up to 3 diopters of cylinder and has been shown to be more effective in those with greater degrees of myopia. PRK patients naturally had thinner corneas preoperatively than both other groups and steeper corneas than LASIK patients. PRK is more suitable to those with thinner corneas, who tend to have central steepening. Although these patients are not normalized, meaningful conclusions can still be drawn both within and between groups regarding their effect on ∆K/∆SEQ.
The change in keratometry value (Km) compared to the change in SEQ in the different corneal refractive surgeries was the primary outcome measure. While this value is well known to be around 0.7–0.8,1 few studies have delved into how this ratio changes with regard to different procedures or different pre-operative characteristics.
In this study, each of the three procedures (PRK, LASIK, and SMILE) were found to have a different ∆K/∆SEQ. The value for LASIK (0.839±0.020) was significantly greater than PRK (0.775 ± 0.022) and SMILE (0.709 ± 0.046). Although SMILE had a lower ∆K/∆SEQ than PRK, the difference was not statistically significant. SMILE is postulated to have the lowest ∆K/∆SEQ due to the nature of the procedure.9 Both PRK and LASIK disturb the corneal epithelium and Bowman’s layer, with PRK removing the epithelium and LASIK creating a flap that disrupts the integrity of the anterior surface. SMILE, on the other hand, involves a small excision of a lenticule that leaves the corneal epithelium and Bowman’s layer intact; the relatively lower disturbance of the anterior surface could explain the lower change in Km per diopter of SEQ change. The lower ∆K/∆SEQ of PRK relative to LASIK may be explained by differences in both epithelial and stromal remodeling. PRK produces significantly greater stromal tissue deposition and increased epithelial thickening relative to LASIK at 1 year post-operatively.10 Pronounced epithelial hyperplasia and stromal thickening that occur in PRK may make the anterior surface more resistant to change in Km per diopter of correction relative to LASIK. These differences may make it important to include a correction factor for ∆K/∆SEQ, allowing for a better prediction of postoperative keratometry based on attempted correction. By knowing more accurately the value of postoperative keratometry in refractive surgery patients, clinicians would be better equipped to choose correct lens power when these patients eventually require cataract surgery.
Preoperative keratometry shows a correlation with ∆K/∆SEQ for LASIK patients. Specifically, a flatter cornea is associated with a greater ∆K/∆SEQ. If this higher-than-expected ∆K/∆SEQ is not accounted for, an undercorrection of the myopia will result. For example, if a patient has a −5D SEQ and is being corrected to 0D, their Km would need to be altered by 4.20D based on the 0.839 ∆K/∆SEQ average that was found for LASIK. If this ratio is higher-than-expected in a flatter cornea, assuming 0.90 ∆K/∆SEQ compared to 0.839, the patient would have actually needed a 4.50D change in Km to achieve the same 5D change in SEQ. These findings are corroborated by Mohamed, who show that flatter corneas tend to cause undercorrection of myopia.11 If clinicians want to account for this change in correction, they could utilize the regression we have included in Figure 4, where every diopter increase in keratometric power would decrease the expected ∆K/∆SEQ by 0.036.
A correlation between age and ∆K/∆SEQ was identified for both the LASIK and SMILE groups. As people age, it was found that the ∆K/∆SEQ decreases, meaning less ablation/tissue removal is needed to achieve a desired correction. For example using the regression in Figure 2, a 20-year-old patient would be expected to have a ∆K/∆SEQ of 0.92 whereas a 40-year-old patient would be expected to have a ∆K/∆SEQ of 0.79. This means to achieve a change of 5D in SE for both patients, the 20-year-old would need a change of 4.6D in Km whereas the 40-year-old would need only a change of 3.95D in Km. This correlation may be explained by age-related changes of the anterior cornea. Some studies have shown that younger patients require more tissue ablation relative to older patients for a desired correction, due to not only the more aggressive healing response in younger patients but also the greater maximum accommodation amplitude.12 Interestingly, no correlation was found between age and ∆K/∆SEQ for PRK. Some studies have shown that PRK compromises corneal biomechanics the least when compared to SMILE and LASIK with the least reduction of corneal stiffness.13 The stiffness may persist with age and could potentially render the cornea less likely to experience a reduction in ∆K/∆SEQ.
Our findings that pre-op pachymetry showed no correlation with ∆K/∆SEQ for any of the three procedures reflect similar findings in the published literature. A study by Zhang et al found that among 158 eyes from 80 patients, there was no correlation found between central corneal thickness and the degree of myopia in that eye.14 This finding implies that for any SEQ that a patient has, any pachymetry value is equally likely. Similarly, in two other studies by Almazrou et al (1005 eyes) and Valdez-Garcia et al (186 eyes), no correlation between central corneal thickness and keratometry value was found.15,16 This would also imply that for any given pachymetry value, any associated Km is equally likely. Given that ∆K/∆SEQ has been shown to change given the degree of refractive error in a patient, and that central corneal thickness is not associated with the degree of refractive error, it makes sense that ∆K/∆SEQ does not correlate with preoperative pachymetry. The lack of correlation between pachymetry and ∆K/∆SEQ in any surgery may be a result of surgical safety bias. We only performed certain procedures for patients with appropriate preoperative characteristics, including preoperative pachymetry. By ensuring a sufficient postoperative residual stromal bed, we may have indirectly accounted for pachymetry, resulting in a lack of correlation with ∆K/∆SEQ.
Pre-op cylinder value was found to correlate with ∆K/∆SEQ for SMILE patients but not for LASIK or PRK. Chow found that SMILE historically has undercorrected astigmatism.17 Specifically, Ivarsen et al found a 13% under correction in low astigmatism and a 16% under correction in high astigmatism in SMILE patients.18 This undercorrection was not found in LASIK or PRK. Therefore, there have been suggestions to increase the SMILE nomograms by 10% for astigmatic corrections. This under-correction matches the results that were found in this study; that the more severe the astigmatism, the larger the ∆K/∆SEQ. As stated previously, a ∆K/∆SEQ larger than expected is consistent with under-correction.
Finally, the attempted SEQ change showed a positive correlation with ∆K/∆SEQ for all three procedures. This implies that patients with higher degrees of myopia require less ablation per diopter of correction. A significant difference was found between PRK’s correlation and that of SMILE. This implies that the ∆K/∆SEQ changes at different rates between these two procedures and different correction factors must be added into the nomograms of these procedures depending on the degree of myopia being corrected. Specifically, PRK had a larger slope (Figure 5), implying that the correction factor will be larger than the corresponding SMILE correction factor. Although the correlation in LASIK was not statistically different than that of PRK and SMILE, the difference in slope may still be useful as a preoperative correction factor. The idea that different levels of correction are required for different levels of myopia emphasizes the importance of nomograms in optimizing patient outcomes.
Multivariate regression analyses demonstrated independent effects of both pre-op keratometry and attempted SEQ change in predicting the ∆K/∆SEQ value in LASIK patients. Of the two, attempted SEQ change was the most significant predictor. Attempted SEQ change was also the most significant predictor in PRK patients, but the results showed a degree of positive autocorrelation. In SMILE patients, the greatest predictor of ∆K/∆SEQ was the age of the patient. The multivariate regression analyses allowed us to construct equations to help predict ∆K/∆SEQ for given preoperative parameters. For LASIK, ∆K/∆SEQ = 2.723 + [0.029 × (attempted SEQ change)] – [0.039 × (pre-op keratometry)]. For PRK, ∆K/∆SEQ = 1.133 + [0.045 × (attempted SEQ change)]. For SMILE, ∆K/∆SEQ = 1.047 – [0.006 × (Age)] (Table 4).
One of the limitations of our study is that some of the correlation results are difficult to explain. Some of our parameters have correlations with ∆K/∆SEQ for certain surgical procedures and not others. For instance, pre-op cylinder only correlated with ∆K/∆SEQ in SMILE. Explaining these unique correlations requires an in-depth discussion on corneal biomechanics within each surgical subgroup that we feel ill-equipped to answer given the data we have presented. Furthermore, as a non-randomized study, there is potential for bias within the sample groups–particularly natural sampling bias as clinicians and patients discuss the best procedure for their specific case. Historically, SMILE has been reserved for patients who require high myopic correction with minimal astigmatism, as the procedure can only correct up to 3 diopters of astigmatism. In our population, this was true, as patients in the SMILE group had higher sphere/spherical equivalent values and lower cylinder value, on average. The greater degree of myopia in SMILE patients would necessitate greater attempted SEQ change, and interestingly SMILE was the only procedure in multiple regression analysis to not have attempted SEQ change as a partial regression coefficient in predicting the ∆K/∆SEQ. Perhaps in greater degrees of myopia, the attempted SEQ change becomes less important as a predictive factor of ∆K/∆SEQ.
In addition, PRK is more often used for patients with thinner corneas, which can be associated with an increased K-value. This sampling bias can be seen in the demographics of the subjects. Some might argue that the patients should have been normalized on the level of every preoperative characteristic. Although randomizing treatments could alter some of the strength of the correlations found in this study, patients with unique characteristics are typically better candidates for some procedures over others.
Conclusion
The ΔK/ΔSEQ ratio is an important clinical parameter, as it helps refractive surgeons to determine what ablation/correction needs to be programmed into the LASER. This ratio is not only different between refractive procedures but it differs with different preoperative parameters that should be considered. Age, pre-op keratometry, pre-op cylinder, and attempted SEQ correction were found to be correlated with ∆K/∆SEQ, while pre-op pachymetry value was not. Multivariate analysis revealed that the degree of attempted correction had the greatest influence on subsequent ∆K/∆SEQ ratio in LASIK and PRK, whereas age was the greatest factor in SMILE. Although not as great of an affect as attempted correction, pre-op keratometry also contributed significantly to predicting the change in ∆K/∆SEQ ratio in LASIK. These factors should be given the most weight when considering preoperative characteristics to adjust nomograms for achieving the desired attempted correction.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Calculation for LASIK ablation – eyeWiki; n.d. Available from: https://eyewiki.aao.org/Calculation_for_LASIK_Ablation.
2. Moshirfar M, Christiansen SM, Kim G. Comparison of the ratio of keratometric change to refractive change induced by myopic ablation. J Refract Surg. 2012;28(10):675–682. PMID: 23061996. doi:10.3928/1081597X-20120921-01
3. Yang SH, Van Gelder RN, Pepose JS. Neural network computer program to determine photorefractive keratectomy nomograms. J Cataract Refract Surg. 1998;24(7):917–924. doi:10.1016/S0886-3350(98)80043-6
4. Arba Mosquera S, de Ortueta D, Verma S. The art of nomograms. Eye Vis. 2018;5(1):1–13. doi:10.1186/S40662-018-0096-Z/TABLES/3
5. Lee WS, Manche EE. Comparison of simulated keratometric changes following wavefront-guided and wavefront-optimized myopic laser-assisted in situ keratomileusis. Clin Ophthalmol. 2018;12:613–619. PMID: 29636597; PMCID: PMC5880184. doi:10.2147/OPTH.S161387
6. Moshirfar M, Brown TW, Heiland MB, Rosen DB, Ronquillo YC, Hoopes PC. Comparative analysis of LASIK flap diameter and its centration using two different femtosecond lasers. Med Hypothesis Discov Innov Ophthalmol. 2019;8(3):241–249.
7. Mifflin MD, Betts BS, Frederick PA, et al. Efficacy and safety of a 3-month loteprednol etabonate 0.5% gel taper for routine prophylaxis after photorefractive keratectomy compared to a 3-month prednisolone acetate 1% and fluorometholone 0.1% taper. Clin Ophthalmol. 2017;11:1113–1118. doi:10.2147/OPTH.S138272
8. Payne CJ, Webster CR, Moshirfar M, Handlon JJ, Ronquillo YC, Hoopes PC. One-year visual outcomes and corneal higher-order aberration assessment of small-incision lenticule extraction for the treatment of myopia and myopic astigmatism. J Clin Med. 2022;11(21):6294. doi:10.3390/jcm11216294
9. Guo H, Hosseini-Moghaddam SM, Hodge W. Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis. BMC Ophthalmol. 2019;19(1). doi:10.1186/S12886-019-1165-3
10. Ivarsen A, Fledelius W, Hjortdal JØ. Three-year changes in epithelial and stromal thickness after PRK or LASIK for high myopia. Invest Ophthalmol Vis Sci. 2009;50(5):2061–2066. PMID: 19151379. doi:10.1167/iovs.08-2853
11. Mohamed Mostafa E. Effect of flat cornea on visual outcome after LASIK. J Ophthalmol. 2015;2015:1–7. doi:10.1155/2015/794854
12. Ghanem RC, de la Cruz J, Tobaigy FM, Ang LPK, Azar DT. LASIK in the presbyopic age group: safety, efficacy, and predictability in 40- to 69-year-old patients. Ophthalmology. 2007;114(7):1303–1310. doi:10.1016/J.OPHTHA.2006.10.026
13. Xin Y, Lopes BT, Wang J, et al. Biomechanical Effects of tPRK, FS-LASIK, and SMILE on the Cornea. Front Bioeng Biotechnol. 2022;10:834270. PMID: 35433653; PMCID: PMC9009506. doi:10.3389/fbioe.2022.834270
14. Zhang H, Xu L, Chen C, et al. Central corneal thickness in adult Chinese. Association with ocular and general parameters. The Beijing Eye Study. Graefes Arch Clin Exp Ophthalmol. 2008;246:587–592. doi:10.1007/s00417-007-0760-9
15. Almazrou AA, Abualnaja WA, Abualnaja AA, Alkhars AZ. Central corneal thickness of a Saudi population in relation to age, gender, refractive errors, and corneal curvature. Cureus. 2022;14(10). doi:10.7759/CUREUS.30441
16. Valdez-García JE, Hernandez-Camarena JC, Lozano-Ramírez JF, Zavala J, Loya-García D, Merayo-Lloves J. Correlation of age, corneal curvature and spherical equivalent with central corneal thickness. Rev Mex de Oftalmol. 2017;91(4):172–176. doi:10.1016/J.MEXOFT.2016.05.005
17. Chow SSW, Chow LLW, Lee CZ, Chan TCY. Astigmatism correction using SMILE. Asia Pac J Ophthalmol. 2019;8(5):391–396. doi:10.1097/01.APO.0000580140.74826.F5
18. Ivarsen A, Hjortdal J. Correction of myopic astigmatism with small incision lenticule extraction. J Refract Surg. 2014;30(4):240–247. doi:10.3928/1081597X-20140320-02
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.