Back to Journals » Clinical Ophthalmology » Volume 14
Influence of Perfluorocarbon Liquids on Peripapillary Retinal Nerve Fiber–Layer Thickness Following Pars Plana Vitrectomy with Silicone Oil–Based Endotamponade
Authors Maqsood S , Abdou Hannon A , Elalfy M, Elborgy ES, Hegazy SM
Received 13 July 2020
Accepted for publication 8 September 2020
Published 28 October 2020 Volume 2020:14 Pages 3541—3549
DOI https://doi.org/10.2147/OPTH.S271941
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sundas Maqsood,1 Ahmed Abdou Hannon,2 Mohamed Elalfy,1,3,4 Ebrahim Salah Elborgy,5 Sherif Momtaz Hegazy5
1Corneo Plastic Unit, Queen Victoria Hospital, East Grinstead, Sussex, UK; 2Paediatric Ophthalmology Unit, Research Institute of Ophthalmology, Cairo, Egypt; 3Cornea Unit, Research Institute of Ophthalmology, Cairo, Egypt; 4Eye Unit, Maidstone and Turnbridge Wells Hospitals, Maidstone, Kent, UK; 5Retinal Surgical Unit, Research Institute of Ophthalmology, Cairo, Egypt
Correspondence: Mohamed Elalfy
Research Institute of Ophthalmology, 2 El Ahram Street, Giza, Cairo 12557, Egypt
Tel +20 2-3571-8304
Email [email protected]
Background: Inner retina–layer modifications after pars plana vitrectomy (PPV) can be objectively assessed through spectral domain optical coherence tomography (SD-OCT).
Methods: This study explored prospectively changes in retinal nerve-fiber layer (RNFL) thickness with SD-OCT in eyes undergoing PPV with silicone oil–based tamponade with and without use of perfluorocarbon liquids (PFCLs) during the early postoperative phase (up to 3 months) at the Research Institute of Ophthalmology, Egypt.
Results: Thirty patients were recruited who underwent PPV and silicone oil–based tamponade for either retinal detachment or diabetic retinopathy between April 2019 and September 2019. Mean RNFL thickness showed no significant change during follow-up at the first week (102.90± 30.68 mm), 1 month (107.30± 32.27), or three months (105.90± 36.68; p=0.46, 0.68). There were significant correlations noticed between RNFL thinning and axial length of eyes, intraocular pressure, and use of PFCLs during the follow-up period.
Conclusion: The RNFL tends to change postvitrectomy, but not significantly. Careful examination and consistent follow-up is required for postvitrectomy patients with larger axial length and intraoperative PFCL use.
Keywords: pars plana vitrectomy, PPV, ganglion-cell complex, GCC, retinal nerve–fibre layer, RNFL, perfluorocarbon liquids, PFCL spectral domain optical coherence tomography, SD-OCT
Introduction
Pars plana vitrectomy (PPV) was introduced in 1971 by Machemer et al and essentially encompasses vitreous body removal as one of the essential steps in the surgical management of various retinal disorders.1 Despite technological advances, transconjunctival sutureless vitrectomy is not without complications, with reports of retinal tears,2,3 hypotony,4,5 and endophthalmitis6,7 in the early postoperative period and cataracts,8,9 retinal detachment,3,5 and recurrent macular edema8 as late-onset problems. The ganglion-cell complex has been defined as a region encompassing the retinal nerve–fiber layer (RNFL), ganglion-cell layer, and inner plexiform layer. The RNFL develops from retinal ganglion-cells axon converging on the disk to form bundles. Thickness of RNFL bundles is greater at the disc and becomes less so peripherally.10
Inner retina–layer changes after PPV have been a frequent topic of discussion in recent years.11 Some studies have reported RNFL thickening after vitrectomy, either as a result of direct mechanical traction on the papillomacular bundle, resulting in tenting and elevation of nerve fibers,12 or edema of the inner-retinal layers in the first postoperative week.13 Others have reported thinning, with possible mechanisms including NFL dehydration during fluid–air exchange,14 dye-related toxicity, mechanical injury, or increased intraocular pressure (IOP).15 There are several technologies that have been used for measuring the RNFL, these include scanning laser polarimetry, confocal scanning laser ophthalmoscopy, and ocular coherence tomography (OCT).16 The development of spectral domain (SD) OCT has made morphological study of different retinal layers with a high level of detail possible.13
Perfluorocarbon liquids (PFCLs) were first used in 1982 by Zimmerman and Faris to relocate a detached retina.17 Following reports on the efficacy and safety of intraoperative PFCL application in in vivo and in vitro studies, Chang et al utilized them in vitrectomies for retinal detachment with severe proliferative vitreoretinopathy.18 Their physical properties of low viscosity, high specific gravity (range 1.76–2.30), high surface tension, and transparency make them an ideal intraoperative tool.19 Short-term use of up to 48 hours has been declared safe in animal models, with no evidence of retinal toxicity at the microscopic level.20,21 This study investigated the effect of PFCL use on RNFL thickness using SD-OCT in eyes undergoing PPV with silicone-oil endotamponade with follow-up of 3 months.
Methods
This prospective noninterventional observational study of 30 eyes of 30 patients was conducted at the Research Institute of Ophthalmology, Egypt between April 2019 and September 2019. All patients underwent RNFL assessment after PPV with silicone oil–based endotamponade by SD-OCT. The study was approved as a prospective audit by the institutional review board at the Institute, and adhered to the Declaration of Helsinki. All patients provided informed consent for enrolment in the study.
All patients aged 18–70 years undergoing PPV with silicone oil–based endotamponade were enrolled during the study period. Patients with previous ocular trauma, ocular surgery, history of ocular vascular disease, uveitis, glaucoma, and high refractive errors were excluded from the study. All included patients underwent detailed ocular and systemic history, assessment of best-corrected visual acuity, IOP measurement, and peripapillary NFL-average measurement with SD-OCT using a Heidelberg OCT II (Heidelberg Engineering, Heidelberg, Germany) at 1 week, 1 month, and 3 months.
Surgical Technique
Three-port 23-gauge PPVs were performed using the Alcon Constellation vision system. All patients underwent triamcinolone-assisted posterior vitreous detachment using a cutter with vacuum set to 450 mmHg. Core vitrectomy was then performed with parameters set to 4,000 cuts/second with linear vacuum set to 300 mmHg, followed by peripheral shaving with cut rate increased to 7,000 cuts/second with vacuum maintained to the same value. As per discretion of the surgeon, parameters were modified based on specific case circumstances. Infusion pressure was maintained at 30mmHg throughout surgery and increased to 45 mmHg during fluid–air exchange. PFL was used in cases with peripheral breaks to avoid the need for drainage retinotomies. Trypan blue–assisted internal limiting membrane (ILM) peeling was performed if considered necessary by the surgeon. Sclerostomies were assessed at the end of surgery and sutured only if considered necessary by the surgeon.
RNFL-Analysis Protocol
Peripapillary RNFL thickness–analysis parameters used were resolution mode high speed, circle diameter 3.5 mm, size X 768 pixels (10.9 mm), size Z 496 pixels (1.9 mm); scaling X 14.17 m/pixel, and scaling Z 3.87 m/pixel. RNFL-thickness parameters in the peripapillary area were automatically calculated by the SD-OCT device and categorized into regions: temporal quadrant thickness (90°), temporal superior quadrant thickness (45°), nasal superior quadrant thickness (45°), nasal quadrant thickness (90°), nasal inferior quadrant thickness (45°), temporal inferior quadrant thickness (45°), and average global thickness (360°).
Recorded data were analyzed using SPSS version 20.0. Quantitative data are expressed as means ± SD. Qualitative data are expressed as frequency and percentage. Independent-sample t-tests of significance were used when comparing between two means. Paired-sample t-tests were used when comparing between related samples. One-way ANOVA was used when comparing more than two means. Pearson’s correlation coefficient (r) testing was used to assess the degree of association between two sets of variables. The confidence interval was set to 95% and the margin of error accepted was 5%. p<0.05 was considered significant.
Results
Thirty patients (21 men and nine women) underwent uneventful PPV with silicone oil–based endotamponade for multiple etiologies (17 retinal detachments, 13 proliferative diabetic retinopathy) at the Research Institute of Ophthalmology, Egypt between April 2019 to September 2019. Mean patient age was 53.00 ± 12.21 (30–70) years. Mean axial length of vitrectomized eyes was 25.07±1.72 (22–28) mm. Nineteen eyes underwent vitrectomy combined with cataract surgery. Ten cases underwent trypan stain–assisted ILM peeling, and PFCLs were used in ten cases. Endolaser, silicone endotamponade, and triamcinolone acetonide were used for all cases. Thirteen patients had no systemic disease, while eight were diabetic and nine suffered from both diabetes and hypertension (Table 1).
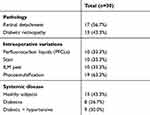 |
Table 1 Pathology, Intraoperative Variations, and Systemic Disease Distribution |
Changes in RNFL Thickness after Vitrectomy
Mean RNFL thickness showed no significant change during follow-up at the first week (102.90±30.68 mm), 1 month (107.30±32.27), or three months (105.90±36.68; p=0.46, 0.68).
Table 2 shows mean differences in RNFL thickness compared to preoperative states, with paired t -test results in nasal, superior nasal, inferior nasal, temporal, superior temporal, and inferior temporal quadrants. Regional RNFL thickness in the superior nasal, superior temporal, inferior nasal, inferior temporal, temporal, and nasal quadrants did not differ significantly among 1-week, 1-month, and 3-month follow-up.
 |
Table 2 Peripapillary Nerve Fiber–layer Analysis at Various Quadrants and Comparison at 1 Week, 1 Month, and 3 Months Postoperatively |
Correlation Between Changes in RNFL Thickness and Visual Acuity and IOP
Changes in RNFL thickness were highly significantly correlated with visual acuity and IOP (Table 3 and Figure 1)
 |
Table 3 Pre- and Post-Operative Comparison of Visual Acuity and Intraocular Pressure During Follow-up |
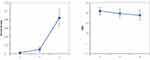 |
Figure 1 Visual acuity and intraocular pressure changes during follow-up. |
Changes in Retinal Nerve Fiber–Layer Thickness According to Eye and Patient Status
RNFL thickness in each quadrant was not significantly different by patient sex or age-group (paired t-test, p>0.05), pathology group (Table 4), or between healthy, diabetic and diabetic + hypertensive patient groups (ANOVA, p>0.05)
Changes in Retinal Nerve Fiber–Layer Thickness According to Operative Associations
RNFL thickness in each quadrant was not significantly different by use of stain-assisted ILM peeling or combining phacoemulsification with vitrectomy (paired t-test, p>0.05). RNFL thickness in average, nasal, temporal, superior temporal, inferior nasal, and inferior temporal quadrants was changed significantly by use of PFCs, as shown in Table 5.
 |
Table 4 Relationship of Axial Length and Etiology in Retinal Detachment (RD), and Diabetic Retinopathy (DR), and n RNFL Thickness at PostOperative Follow-up |
 |
Table 5 Effect of Perfluorocarbon Liquids (PFCLs) on Retinal Nerve Fiber–Layer Analysis. Clinically Significant Values (p>0.05) Depicted in Bold Font |
Discussion
RNFL thickness measured by SD-OCT objectively and qualitatively is important, as RNFL damage often occurs before both visual field defects and optic nerve–head damage can be detected. Kerrigan-Baumrind reported that at least 25%–35% retinal ganglion–cell loss is associated with statistical abnormalities in automated visual field testing.22 The pathophysiology of visual field defects after vitrectomy is a matter of debate. A postoperative increase in IOP, retinal toxicity of intravitreal gas tamponade, phototoxicity from endoillumination, mechanical retinal damage during posterior vitreous–detachment induction, damage to the NFL in ERM or external limiting–membrane peeling, dehydration of the RNFL caused by fluid–air exchange, and chemical retinal damage caused by indocyanine green (ICG) staining are possible explanations given in the literature.11,23–25 The present study included 30 patients who underwent PPV combined by silicon endotamponade. Our results showed that RNFL parameters did not change significantly throughout the 3-month follow-up in any quadrant. This finding correlates well with studies reported by Lee and Kim et al.25,26
We observed that visual acuity improved significantly, which statistically correlated with changes in the RNFL. IOP was found to be significantly decreased during period of follow-up. Early postoperative IOP elevation is explained by the inflammatory response that occurs postoperatively or due to the patient being a steroid responder. The subsequent decrease of IOP is assumed to be related to inflammatory recovery or steroid cessation. The spike in IOP was not alarming and was short-lived, and thus its effect on RNFL change is considered minimal if at all significant. PFCLs are useful and safe surgical tools in vitreoretinal surgery. Currently, retinal detachments associated with proliferative vitreoretinopathy, giant retinal tears, and penetrating trauma are the primary indications for their use. With growing evidence and advancements in surgical techniques, newer applications for PFCLs have been explored, including management of dislocated crystalline or intraocular lenses, retinopathy of prematurity, retinoschisis, retinal detachment associated with proliferative diabetic vitreoretinopathy, and management of suprachoroidal and submacular hemorrhage.28 The use of PFCLs as a temporary tamponade has been controversial, due to corneal toxicity, retinal infiltration, and inflammatory reaction in experimental studies. Although most clinical studies have not been able to establish any proof of retinal toxicity, such as progressive visual acuity loss, electroretinography or retinal histological analysis haas not been reported extensively.29
SD-OCT is a relatively new technology, which explains why there is a significant paucity of literature on the effect of PFCLs on RNFL thickness. This study confirmed a positive correlation of RFNL thinning with use of PFCLs in ten patients. This was significant at the 1-week (global, nasal, superior temporal, and inferior temporal) and 3-month(inferior nasal and inferior temporal) follow-up. We expected that there might be a significant correlation of thickening of the RNFL due to rebound edema caused by compression by heavy liquids like PFCLs, but report thinning of the RNFL in this study could be attributed to the mechanical compression effect of the liquid on the RNFL. Although silicone oils have been used for years and are relatively safe, there have been reports of RNFL thinning after the use of silicone oil,27,30 while others reported paradoxical thickening.31 In our study, we found that there were no statistically significant changes in RNFLs due to use of silicon endotamponade, in agreement with a study by Caramoy et al.32
Wolf et al reported that substantial damage to Müller-cell end feet is caused by ILM peeling, even in the untouched retina directly adjacent to the peeled area. This suggests that the basal lamina can transmit mechanical forces to the inner retinal layers, causing cellular damage in these layers.33 Kim et al and Yamashita et al assessed the RNFL after ICG-assisted vitrectomy and found that the RNFL was significantly reduced postoperatively.23,25 This can be explained by the mechanical damage due to retinal manipulation or by toxic effects of the dye. Although ICG is considered safe and widely used successfully, trypan blue has been demonstrated to have a larger safety margin.34 In the present study, we observed no statistically significant differences in changes in RNFL thickness in correlation with trypan-assisted ILM peeling. Our findings matched those of Toba et al, who reported no significant correlation between the degree of change in RNFL thickness and the type of vital stain (triamcinolone acetonide, brilliant blue, trypan blue, and ICG) used during surgery.35
It has been reported that, diabetic eyes that have been treated with panretinal photocoagulation have thinner RNFLs than nondiabetic eyes.36 Eren et al reported initial thickening of RFNL in the first 3 months postprocedure due to ensuing axonal edema, followed by thinning at the sixth month, attributed to axonal loss secondary to the laser treatment.37 All the cases in this study underwent panretinal photocoagulation, which was found to have no significant correlation with changes in RNFL thickness.38 This study found that changes in the RNFL did not differ significantly with patient age, sex, pathology group, presence/absence of systemic diseases, or combined phacovitrectomy procedure, in agreement with the literature.25,27,39,40 Limitations of this study include the short follow-up and multiple pathologies possibly being confounding factors in interpretation of the results. However, the study results show realistic scenarios faced in clinical practice.
Conclusion
The RNFLi tends to change postvitrectomy, but not significantly. Careful examination and consistent follow-up is required for postvitrectomy patients with larger axial length and intraoperative PFCL use. SD-OCT is a useful objective tool for evaluating RNFL thickness after vitrectomy, and large and long-term prospective studies are needed to evaluate changes in the RNFL with SD-OCT after vitrectomy.
Ethical Approval and Informed Consent
This study was approved as a prospective audit by the institutional review board at the Research Institute of Ophthalmology, Giza, Egypt and adhered to the Declaration of Helsinki. All participants provided informed consent for participation in the study.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, took part in drafting the article or revising it critically for important intellectual content, agreed to submit to the current journal, gave final approval to the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
No financial or nonfinancial conflicting interests exist for any author.
References
1. Machemer R, Buettner H, Norton EW, Parel JM. Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol. 1971;75:813–820.
2. Scartozzi R, Bessa AS, Gupta OP, Regillo CD. Intraoperative sclerotomy-related retinal breaks for macular surgery, 20- vs 25-gauge vitrectomy systems. Am J Ophthalmol. 2007;143:155–156. doi:10.1016/j.ajo.2006.07.038
3. Gupta OP, Ho AC, Kaiser PK, et al. Short-term outcomes of 23-gauge pars plana vitrectomy. Am J Ophthalmol. 2008;146(2):193–197. doi:10.1016/j.ajo.2008.04.010
4. O’ Reilly P, Beatty S. Transconjunctival sutureless vitrec- tomy: initial experience and surgical tips. Eye (Lond). 2007;21:518–521. doi:10.1038/sj.eye.6702255
5. Hikichi T, Matsumoto N, Ohtsuka H, et al. Comparison of one- year outcomes between 23- and 20-gauge vitrectomy for preretinal membrane. Am J Ophthalmol. 2009;147:639–643.e1. doi:10.1016/j.ajo.2008.10.009
6. Scott IU, Flynn HW
7. Kunimoto DY, Kaiser RS. Incidence of endophthalmitis after 20- and 25-gauge vitrectomy. Ophthalmology. 2007;114:2133–2137. doi:10.1016/j.ophtha.2007.08.009
8. Patelli F, Radice P, Zumbo G, et al. 25-gauge macular surgery: results and complications. Retina. 2007;27:750–754. doi:10.1097/IAE.0b013e31802c5125
9. Tewari A, Shah GK, Fang A. Visual outcomes with 23- gauge transconjunctival sutureless vitrectomy. Retina. 2008;28:258–562. doi:10.1097/IAE.0b013e318159ec5a
10. Quigley HA, Dunkelberger GR, Green WR. Retinal ganglion cell atrophy correlated with automated perimetry in human eyes with glaucoma. Am J Ophthalmol. 1989;107(5):453–464. doi:10.1016/0002-9394(89)90488-1
11. Pichi F, Lembo A, Morara M. Early and late inner retinal changes after inner limiting membrane peeling. Int Ophthalmol. 2014;34:437–446. doi:10.1007/s10792-013-9831-6
12. Reddy RK, Lalezary M, Kim SJ, et al. Prospective retinal and optic nerve vitrectomy evaluation (PROVE) study: findings at 3 months. Clin Ophthalmol. 2013;7:1761–1769.
13. Capelanes NC, Diniz AV, Magalhães ÉP, et al. Comparison of retinal nerve fiber layer thickness changes after macular hole surgery. Arq Bras Oftalmol. 2018;81(1):37–41. doi:10.5935/0004-2749.20180009
14. Welch JC. Dehydration injury as a possible cause of visual field defect after pars plana vitrectomy for macular hole. Am J Ophthalmol. 1997;124(5):698–699. doi:10.1016/S0002-9394(14)70915-8
15. Arora S, Goel N, Arora T, et al. Comparative evaluation of retinal nerve fiber layer thickness after conventional brilliant blue assisted internal limiting membrane peeling versus brilliant blue selective staining using whole blood in macular hole surgery. Ophthalmic Surg Lasers Imaging Retina. 2016;47(5):436–442. doi:10.3928/23258160-20160419-06
16. Jones-Odeh E, Hammond CJ. How strong is the relationship between glaucoma, the retinal nerve fibre layer, and neurodegenerative diseases such as alzheimer’s disease and multiple sclerosis? Eye (Lond). 2015;29(10):1270–1284.
17. Zimmerman NJ, Faris D. The use of N-perfluorocarbon amines in complicated retinal detachments. Invest Oph Thalmol Visual Sci. 1984;25(supplement):258.
18. Chang S, Ozmert E, Zimmerman NJ. Intraoperative perfluorocarbon liquids in the management of proliferative vitreoretinopathy. Am J Ophthalmol. 1988;106(6):668–674. doi:10.1016/0002-9394(88)90698-8
19. Sargent JW, Seffl RJ. Properties of perfluorinated liq- uids. Fed Proc. 1970;29(5):1699–1703.
20. Mackiewicz J, Maaijwee K, Luke C, et al. Effect of gravity in long-term vitreous tamponade: in vivo investigation using perfluorocarbon liquids and semi-fluorinated alkanes. Graefe’s Arch Clin Exp Ophthalmol. 2007;245(5):665–675.
21. Chang S, Sparrow JR, Iwamoto T, Gershbein A, Ross R, Ortiz R. Experimental studies of tolerance to intravitreal perfluoro-n-octane liquid. Retina. 1991;11(4):367–374.
22. Kerrigan-Baumrind LA, Quigley HA, Pease ME. Number of ganglion cells in glaucoma eyes compared with threshold visual field tests in the same persons. Invest Ophthalmol Vis Sci. 2000;41:741–748.
23. Yamashita T, Uemura A, Kita H, Sakamoto T. Analysis of the retinal nerve fiber layer after indocyanine green-assisted vitrectomy for idiopathic macular holes. Ophthalmology. 2006;113(2):280–284. doi:10.1016/j.ophtha.2005.10.046
24. Haritoglou C, Gass CA, Schaumberger M. Macular changes after peeling of the internal limiting membrane in macular hole surgery. Am J Ophthalmol. 2001;132:363–368. doi:10.1016/S0002-9394(01)01093-5
25. Kim KY, Yu SY, Kim MS, Kim ES, Kwak HW. Changes of parafoveal retinal nerve fiber layer thickness analyzed by spectral-domain optical coherence tomography after pars plana vitrectomy. Retina. 2013;33(4):776–784.
26. Lee SB, Shin YI, Jo YJ, Kim JY. Longitudinal changes in retinal nerve fiber layer thickness after vitrectomy for epiretinal membrane. Invest Ophthalmol Vis Sci. 2014;55:6607–6611. doi:10.1167/iovs.14-14196
27. Takkar B, Azad R, Kamble N, Azad S. Retinal nerve fiber layer changes following primary retinal detachment repair with silicone oil tamponade and subsequent oil removal. J Ophthalmic Vis Res. 2018;13:124–129.
28. Georgalas I, Ladas I, Tservakis I, et al. Perfluorocarbon liquids in vitreoretinal surgery: a review of applications and toxicity. Cutan Ocul Toxicol. 2011;30(4):251–262.
29. Figueroa MS, Casas DR. Inflammation induced by perfluorocarbon liquid: intra-and postoperative use. Biomed Res Int. 2014;2014.
30. Christensen UC, la Cour M. Visual loss after use of intraocular silicone oil associated with thinning of inner retinal layers. Acta Ophthalmol. 2012;90(8):733–737. doi:10.1111/j.1755-3768.2011.02248.x
31. Darija J, Mia ZG, Ivan Ć, Dobrila KU. Retinal layers measurements following silicone oil tamponade for retinal detachment surgery. Semin Ophthalmol. 2017.
32. Caramoy A, Droege KM, Kirchhof B, Fauser S. Retinal layers measurements in healthy eyes and in eyes receiving silicone oil‐ based endotamponade. Acta Ophthalmol. 2014;92(4):e292–7. doi:10.1111/aos.12307
33. Wolf S, Schnurbusch U, Wiedemann P, Grosche J, Reichenbach A, Wolburg H. Peeling of the basal membrane in the human retina: ultrastructural effects. Ophthalmology. 2004;111:238–243. doi:10.1016/j.ophtha.2003.05.022
34. Jackson TL, Hillenkamp J, Knight BC, et al. Safety testing of indocyanine green and trypan blue using retinal pigment epithelium and glial cell cultures. Invest Ophthalmol Vis Sci. 2004;45(8):2778–2785. doi:10.1167/iovs.04-0320
35. Toba Y, Machida S, Kurosaka D. Comparisons of retinal nerve fiber layer thickness after indocyanine green, brilliant blue g, or triamcinolone acetonide-assisted macular hole surgery. J Ophthalmol. 2014;187308.
36. Lim MC, Tanimoto SA, Furlani BA, et al. Effect of diabetic retinopathy and panretinal photocoagulation on retinal nerve fiber layer and optic nerve appearance. Arch Ophthalmol. 2009;127(7):857–862. doi:10.1001/archophthalmol.2009.135
37. Eren S, Ozturk T, Yaman A, Oner H, Osman SA. Retinal nerve fiber layer alterations after photocoagulation: a prospective spectral-domain OCT study. Open Ophthalmol J. 2014;8:82. doi:10.2174/1874364101408010082
38. Kim JE, Shah SN, Choi DL, Han DP, Connor TB. Transconjunctival 20-gauge pars plana vitrectomy using a single entry cannulated sutureless system. Retina. 2009;29(9):1294–1298. doi:10.1097/IAE.0b013e3181aa8e3b
39. Minami M, Oku H, Okuno T, Fukuhara M, Ikeda T. High infusion pressure in conjunction with vitreous surgery alters the morphology and function of the retina of rabbits. Acta Ophthalmol Scand. 2007;85(6):633–639. doi:10.1111/j.1600-0420.2007.00919.x
40. Gharbiya M, La Cava M, Tortorella P. Peripapillary RNFL thickness changes evaluated with spectral domain optical coherence tomography after uncomplicated macular surgery for epiretinal membrane. Semin Ophthalmol. 2016;1–7.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
