Back to Journals » Clinical Ophthalmology » Volume 13
Influence of eyelid pigmentation on the diagnosis of meibomian gland dysfunction
Authors Blumberg MJ, Millen AE , Patel SP
Received 9 July 2019
Accepted for publication 1 September 2019
Published 19 September 2019 Volume 2019:13 Pages 1815—1821
DOI https://doi.org/10.2147/OPTH.S222451
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Max J Blumberg,1 Amy E Millen,2 Sangita P Patel1,3
1Department of Ophthalmology, Ross Eye Institute, Jacobs School of Medicine and Biomedical Sciences, State University of New York at Buffalo, Buffalo, NY, USA; 2Department of Epidemiology and Environmental Sciences, School of Public Health and Health Professions, University at Buffalo, Buffalo, NY, USA; 3Research and Ophthalmology Services, Veterans Administration of Western New York Healthcare System, Buffalo, NY, USA
Correspondence: Sangita P Patel
Ross Eye Institute, 1176 Main Street, Buffalo, NY 14209, USA
Tel +1 716 862 6577
Fax +1 716 881 4349
Email [email protected]
Purpose: To determine whether reliance on eyelid margin vascularization as a diagnostic criterion for meibomian gland dysfunction (MGD) results in underdiagnosis of MGD in individuals with dark skin pigmentation.
Patients and Methods: This cross-sectional study enrolled consecutive cornea clinic patients in Buffalo, New York. Eyelid margin vascularization was graded qualitatively from slit-lamp photos. Skin pigmentation was quantified from digital photos using red/green/blue (RGB) pixel analysis and dichotomized using the RGB median. MGD was defined as abnormal quantity or quality of meibum or increased pressure required to express meibum. Additional testing included infrared meibography, Schirmer’s testing, and a dry eye questionnaire. Sensitivity of MGD diagnosis by visualization of vascularization, compared to diagnosis by expression of meibum, was estimated with and without stratification by skin pigmentation.
Results: Among 47 participants, 15–79 years old, meibomian gland truncation/dropout, abnormal tear production, and dry eye symptoms affected individuals of all skin pigmentations. Eyelid margin vascularization was less common in subjects with dark (n=21%) compared to light pigmentation (65%; p=0.002), although the prevalence of MGD assessed via clinical evaluation did not vary significantly between those groups. Use of eyelid margin vascularization alone was not sensitive (33%) for MGD diagnosis. The sensitivity was 17% when limited to those with dark pigmentation.
Conclusion: Our findings highlight the importance of gland expression and suggest limiting reliance on eyelid margin vascularization for MGD diagnosis, especially in those with dark eyelid skin pigmentation.
Keywords: meibomian glands, dry eye syndromes, skin pigmentation
Plain language summary
Dry eye disease is a common problem that affects people around the world. Meibomian gland dysfunction, or MGD, is a common contributor to dry eye disease. Some people who suffer from MGD have more small blood vessels along the edge of the eyelid than those who do not have MGD. This feature of the disease has been used by eye doctors to help in diagnosing and treating MGD. In this study, we looked for these blood vessels and other exam findings that can be seen with MGD, in people with a wide spectrum of skin tones. We found that in individuals with dark skin, we did not see these blood vessels, even if they had MGD. If eye doctors rely on observing the presence of these blood vessels, they may miss the diagnosis of MGD. Therefore, we argue that eye doctors should not rely on the presence (or absence) of blood vessels along the eyelid margin in their diagnosis of MGD, especially in people with dark skin.
Introduction
Dry eye disease is a worldwide problem with a multifactorial etiology, resulting in decreased quality of life and ocular morbidity.1 Meibomian gland dysfunction (MGD) is a common contributor to dry eye disease in all racial populations studied thus far.2 MGD is defined by an abnormal quantity and/or quality of meibomian gland secretions, known as meibum.3 Clinical diagnosis requires manual expression of the eyelid meibomian glands with evaluation of the meibum by slit-lamp biomicroscopy. Despite the high prevalence of MGD, ophthalmologists do not routinely express the meibomian glands for evaluation of MGD, but rely instead on evaluation of the lid margin appearance.4
In addition to requiring evaluation of meibum, the consensus reports on MGD diagnosis, grading, and treatment also include evaluation of anatomic abnormalities of the eyelid margin. These include changes such as irregularity/notching of the margin, displacement of meibomian gland orifices, and eyelid margin vascularization.3,5,6 Eyelid margin vascularization may not be as apparent in darker skinned individuals. For example, facial erythema and telangiectasia in rosacea are difficult to appreciate in individuals with dark skin.7,8 For research purposes of standardizing MGD grading scales for diverse populations, eyelid margin vascularization may not be a suitable generally applicable criterion. In addition, for those ophthalmologists inappropriately relying on anatomic eyelid abnormalities such as lid margin vascularization (without gland expression), many cases of obstructive MGD may be missed.9
In our multiracial clinic, we have observed severe obstructive MGD without eyelid margin vascularization in patients with dark skin pigmentation. We designed a cross-sectional clinical study to test the impact of eyelid skin pigmentation on the sensitivity of using eyelid margin vascularization in the diagnosis of MGD. We hypothesized that the sensitivity of eyelid margin vascularization in the diagnosis of MGD would be lower in individuals with dark compared to light eyelid skin pigmentation, and thus inappropriately relying on eyelid margin vascularization as a diagnostic criterion would result in underdiagnosis of MGD in a clinical population inclusive of individuals with dark skin pigmentation.
Materials and Methods
Study Participants
Consecutive patients, with and without dry eye disease/MGD, presenting to a cornea subspecialty clinic (SPP) were invited to participate in this study. Subjects were included if they were >14 years old and able to reliably complete study questionnaires and examination procedures. Exclusion criteria were use of eye make-up on the day of the exam, use of eye drops <3 hrs prior to exam, contact lens wear in the prior month, and conditions other than dry eye or MGD causing scarring of the eyelid margin or conjunctiva (e.g., chemical burns and cicatricial conjunctivitis). If only one eye met exclusion criteria, then the other eye alone was included.
Institutional Review Board approval was obtained from the University at Buffalo, and the described research adhered to the tenets of the Declaration of Helsinki. Following written informed consent of the participant, and parent or legal guardian for any participant under the age of 18 years, each participant completed the following testing.
Clinic Exam
Meibomian Glands
Meibum was expressed using the Korb Meibomian Gland Evaluator (Tear Science, Morrisville, North Carolina), a spring-loaded diagnostic instrument. With partial compression of the spring, the Korb delivers uniform pressure to the meibomian glands (pressure grade 0). If no meibum was expressed with partial compression of the spring in the Korb, we observed further for meibum expression with complete compression of the spring (pressure grade 1, obstructed meibomian glands).
Quality and quantity of meibum from the middle one-third of the lower eyelid was graded visually.10 Quality was graded as 0= clear, 1= cloudy, 2= granular, 3= toothpaste, or 4= none. Quantity was graded as 0= none, 1= normal or 2= increased. Since the definition of MGD includes abnormal meibum quality without consideration for grade, for statistical tests, a dichotomous variable was created with meibum quality =0 for clear, and meibum quality =1 for values of cloudy, granular, toothpaste, or none.
Definition of MGD
In our study, a patient was considered to have normal meibomian gland function if his/her meibum quality was 0= clear, quantity was 1= normal, and Korb was 0= no increased pressure needed. MGD was diagnosed if any of these components were graded otherwise, indicating abnormal quality and/or quantity of meibum.
Meibography and Dry Eye Assessments
Infrared images of the meibomian glands were taken using infrared imaging (Heidelberg Spectralis HRA with anterior segment module, Heidelberg, Germany). These images were used to grade gland truncation/dropout of the central 5 lower eyelid glands (Figure 1). Each gland was graded as 0= dropout, 1= truncated, or 2= normal and the sum of the 5 glands was averaged for two eyes for a score out of 10. Tear production was measured as the average for two eyes of millimeters of wetting of a 35-mm Schirmer’s test strip in 5 mins without topical anesthesia. Subjects completed the two-question Symptom Assessment iN Dry Eye (SANDE) questionnaire to screen for dry eye symptom frequency and severity. Answers to the two questions were measured in millimeters on a 10-cm visual analogue scale and averaged.11
 |
Figure 1 Infrared meibography for meibomian gland imaging. Arrows point to the glands of the lower eyelid when normal and truncated. The eyelid is everted with a Korb meibomian gland evaluator. |
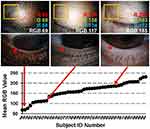
Eyelid Pigmentation Assessment
Photographs of the upper eyelid skin and lower eyelid margin were taken using a digital camera (Nikon, Tokyo, Japan) on a slit-lamp biomicroscope with uniform exposure settings for all subjects. Eyelid pigmentation was graded using the color histogram tool in ImageJ software (National Institutes of Health). A 1200×1200 pixel square was drawn uniformly for all photographs over the upper eyelid off-center in order to avoid the central light reflex (Figure 2). The mean red, green, and blue (RGB) values for the region were averaged and then the two eyes were averaged for the final RGB score.
Eyelid Margin Vascularization
Presence or absence of eyelid margin vascularization was qualitatively graded from the slit-lamp biomicroscopy photos and confirmed by two masked individuals with 100% agreement. The bottom-right image in Figure 2 is an example of a subject in which eyelid margin vascularization was present. If there was vascularization present in only one eye, we counted it as present overall.
Statistical Analysis
In cases where values for both eyes were obtained, there were no subjects where the two eyes were different on the pressure applied, the quality of meibum, or the presence of MGD. Using the median for RGB of 170, two pigmentation groups were created: dark (RGB <170) and light (RGB ≥170). Differences in mean meibography score, Schirmer’s tear production, and SANDE score were compared by level of RGB (light/dark) using independent t-tests. Chi-square tests were used to compare the percentage of subjects with vascularization, different meibum qualities, and diagnosis of MGD by RGB level (light/dark). P-values of <0.05 were considered statistically significant and two-sided tests were conducted. Last, we calculated the sensitivity and specificity of eyelid margin vascularization to diagnose MGD compared to our clinical diagnosis of MGD as defined above.
Results
We enrolled 47 subjects (n=27 female, 57%) with a mean age of 48 years. For six subjects, only one eye was included since the other eye met exclusion criteria. For all other subjects, both eyes were included. Subjects had a wide range of skin pigmentation (68 to 231 with a mean of 160 and a median of 170; Figure 2). The meibography scores for our subjects showed severe gland dropout (low scores) to normal glands (10; Figure 3A). Schirmer’s tear production test and SANDE symptom questionnaire values encompassed nearly the entire range of the test (Figure 3B and C). The least-square means (LSM) for meibography score were lower, and the LSM for the Schirmer’s test and the SANDE symptom score were slightly higher among those with dark compared to light pigmentation, although the mean differences were not statistically different by pigmentation level.
Fifty-seven percent (n=27) of subjects had vascularization present and 43% (n=20) did not (Figure 3D). Among those with dark pigmentation, there were statistically significantly fewer subjects with vascularization (n=5 [21%]) than among those with light pigmentation (n=15 [65%]) (p for chi-square =0.002).
Overall, there were n=30 (64%) subjects with clear meibum quality, n=10 (21%) with cloudy, n=2 (4%) with granular, n=2 (4%) with toothpaste, and n=3 (6%) with absent (Figure 3E). Among persons with dark skin pigmentation, n=14 (58%) had clear meibum quality vs n=16 (70%) for those with lighter skin pigmentation (p for chi-square =0.423).
Overall, there were n=16 (34%) subjects who required increased pressure. Among these subjects, there were n=3 subjects who had no meibum expression even after applying increased pressure. The other n=13 subjects had plugging, which was relieved by the increased pressure. Although more persons with dark skin pigmentation (n=10, 43%) required increased pressure compared to those with lighter skin pigmentation (n=6, 30%), this was not statistically significant (p for chi-square=0.362).
We diagnosed n=21 (45%) subjects as having MGD based on clinical examination. The prevalence of MGD did not vary significantly between those with dark (50%) compared to light (39%) pigmentation (p for chi-square =0.454) (Figure 3F).
The sensitivity and specificity of using vascularization alone to diagnose MGD were 33% and 50%, respectively. The sensitivity dropped to 17% among subjects with darker pigmentation and the specificity increased to 73% (Table 1).
 |
Table 1 Sensitivity and specificity of using vascularization alone to diagnose MGD in all subjects, and split around the median pigmentation |
Discussion
Findings from this cross-sectional clinical study showed that eyelid margin vascularization was less common in subjects with dark compared to light pigmentation, although the prevalence of MGD assessed via clinical evaluation did not vary significantly by skin pigmentation. The sensitivity of using eyelid margin vascularization alone to diagnose MGD does not appear valid, and may be less so in those with dark skin pigmentation.
Findings from this study showed a lower percentage of individuals with eyelid margin vascularization in patients with darker compared to lighter skin pigmentation, but there were no statistically significant differences in diagnosis of MGD. The prevalence of different forms of MGD may vary in groups of individuals defined by skin pigmentation. There are two general categories for MGD distinguished based upon the volume of meibum: low delivery (hyposecretory) and high delivery (hypersecretory). Included in the hyposecretory category is obstructive MGD which is further subdivided into cicatricial and noncicatricial,12 or obvious (presence of other eyelid findings) and nonobvious (no obvious eyelid abnormalities).9 It appears, in our sample, that nonobvious obstructive MGD (i.e., those with MGD without vascularization) is more common in our subjects with darker compared to lighter skin pigmentation, otherwise we would expect to see a lower percentage of individuals with MGD in the darker skin pigmentation group in parallel with the observed lower percentage of eyelid margin vascularization seen in this group.
Prior studies have shown that vascularization varies by race with less prominence in black individuals compared to white.13 A strength of our study is that we intentionally did not compare racial groups, but rather directly quantified level of eyelid pigmentation, thus providing objectivity to our data. The pigmentation cutoff at which we did not see eyelid margin vascularization (RGB <145) corresponds to a light brown pigmentation that is seen in many racial groups, not limited to black. One limitation of our study is that our sample is not random. However, our sample included a broad range across all variables tested, and the prevalence of MGD in our sample (45%) is within the range of other published studies. The reported prevalence of MGD ranges from 3.6% to 68.0%.14 Different studies use different diagnostic criteria, and therefore the prevalence between studies cannot be directly compared. A future study including a larger multiracial population could differentiate if our findings are related to pigmentation or race.
Criteria used to diagnose and grade MGD, including guidance from consensus workshops and recent working groups, continue to include eyelid margin vascularization.3,5,6,14 These criteria typically group eyelid margin vascularization with other eyelid margin anatomic abnormalities, such as meibomian gland orifice displacement or irregularity of the margin/notching. Eyelid vascularization is a reproducible measure for MGD grading currently used for clinical study purposes, according to a validation study using Japanese subjects.15 Our data, however, suggest limiting reliance on that criterion due to the implications of underdiagnosing or undergrading MGD in dark-skinned individuals.
Appropriate diagnosis and grading of MGD have implications for research as well as clinical and surgical eye care. Although eyelid margin vascularization may be one of many components useful in the diagnosis and grading of MGD in light-skinned individuals, ideal criteria should be applicable to the global population, independent of skin pigmentation. As such, our data advocate for consensus criteria that do not emphasize eyelid margin vascularization.
Acknowledgments
Funding was provided by Jacobs School of Medicine and Biomedical Sciences, University at Buffalo Summer Research Fellowship (MJB); start-up funds from the Jacobs School of Medicine and Biomedical Sciences and Department of Ophthalmology, University at Buffalo (SPP).
This work was supported, in part, by facilities and resources provided by the VA Western New York Healthcare System. The contents of this work do not represent the views of the Department of Veterans Affairs or the United States government.
Disclosure
Dr Sangita P Patel reports personal fees from Novartis, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. McDonald M, Patel DA, Keith MS, Snedecor SJ. Economic and humanistic burden of dry eye disease in Europe, North America, and Asia: a systematic literature review. Ocul Surf. 2016;14.2:144–167. doi:10.1016/j.jtos.2015.11.002
2. Baudouin C, Messmer EM, Aragona P, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Ophthalmol. 2016;100(3):300–306. doi:10.1136/bjophthalmol-2015-307415
3. Tomlinson A, Bron AJ, Korb DR, et al. The international workshop on meibomian gland dysfunction: report of the diagnosis subcommittee. Invest Ophthalmol Vis Sci. 2011;52(4):2006–2049. doi:10.1167/iovs.10-6997f
4. Foulks GN, Nichols KK, Bron AJ, Holland EJ, McDonald MB, Nelson JD. Improving awareness, identification, and management of meibomian gland dysfunction. Ophthalmology. 2012;119(10 Suppl):S1–S12. doi:10.1016/j.ophtha.2012.06.064
5. Bron AJ, Benjamin L, Snibson GR. Meibomian gland disease. Classification and grading of lid changes. Eye (Lond). 1991;5(Pt 4):395–411. doi:10.1038/eye.1991.65
6. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15(3):539–574. doi:10.1016/j.jtos.2017.05.001
7. Al Balbeesi AO, Halawani MR. Unusual features of rosacea in saudi females with dark skin. Ochsner J. 2014;14(3):321–327.
8. Al-Dabagh A, Davis SA, McMichael AJ, Feldman SR. Rosacea in skin of color: not a rare diagnosis. Dermatol Online J. 2014;20:10.
9. Blackie CA, Korb DR, Knop E, Bedi R, Knop N, Holland EJ. Nonobvious obstructive meibomian gland dysfunction. Cornea. 2010;29(12):1333–1345. doi:10.1097/ICO.0b013e3181d4f366
10. Korb DR, Blackie CA. Meibomian gland diagnostic expressibility: correlation with dry eye symptoms and gland location. Cornea. 2008;27(10):1142–1147. doi:10.1097/ICO.0b013e3181814cff
11. Amparo F, Schaumberg DA, Dana R. Comparison of two questionnaires for dry eye symptom assessment: the ocular surface disease index and the symptom assessment in dry eye. Ophthalmology. 2015;122(7):1498–1503. doi:10.1016/j.ophtha.2015.02.037
12. Nelson JD, Shimazaki J, Benitez-del-Castillo JM, et al. The international workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2011;52(4):1930–1937. doi:10.1167/iovs.10-6997b
13. Alghamdi YA, Mercado C, McClellan AL, et al. Epidemiology of meibomian gland dysfunction in an elderly population. Cornea. 2016;35(6):731–735. doi:10.1097/ICO.0000000000000815
14. Amano S. Meibomian gland dysfunction: recent progress worldwide and in Japan. Invest Ophthalmol Vis Sci. 2018;59(14):DES87–DES93. doi:10.1167/iovs.17-23553
15. Arita R, Minoura I, Morishige N, et al. Development of definitive and reliable grading scales for meibomian gland dysfunction. Am J Ophthalmol. 2016;169:125–137. doi:10.1016/j.ajo.2016.06.025
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.