Back to Journals » Patient Preference and Adherence » Volume 17
Influence of Disease Acceptance on the Quality of Life of Patients with Ankylosing Spondylitis – Single Centre Study
Authors Wysocki G , Czapla M, Uchmanowicz B, Fehler P, Aleksandrowicz K, Rypicz, Wolska-Zogata I , Uchmanowicz I
Received 3 January 2023
Accepted for publication 21 March 2023
Published 18 April 2023 Volume 2023:17 Pages 1075—1092
DOI https://doi.org/10.2147/PPA.S403437
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Grzegorz Wysocki,1 Michał Czapla,2– 4 Bartosz Uchmanowicz,5 Piotr Fehler,4 Katarzyna Aleksandrowicz,4 Łukasz Rypicz,6 Irena Wolska-Zogata,7 Izabella Uchmanowicz4,5
1LUX MED Medical Center, Warsaw, Poland; 2Department of Emergency Medical Service, Wroclaw Medical University, Wroclaw, Poland; 3Group of Research in Care (GRUPAC), Faculty of Health Science, University of La Rioja, Logroño, Spain; 4Institute of Heart Diseases, University Hospital, Wroclaw, Poland; 5Department of Nursing and Obstetrics, Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland; 6Department of Population Health, Faculty of Health Sciences, Wroclaw Medical University, Wrocław, Poland; 7Department of Applied Sociology and Social Work, Institute of Sociology, University of Wroclaw, Wroclaw, Poland
Correspondence: Michał Czapla, Department of Emergency Medical Service, Wroclaw Medical University, ul. Parkowa 34, Wroclaw, 51-616, Poland, Email [email protected]
Introduction: Ankylosing spondylitis (AS) is a chronic, progressive disease, often with multiple complications, with periods of exacerbation and remission. The onset of the disease usually affects people under 30 years of age. The disease impairs physical, psychological, and social functioning, leading to disability. Therefore, patients with AS face the challenge of adapting to life with the condition and deteriorating quality of life (QoL).
Objective: This study aimed to assess the impact of disease acceptance on quality of life in patients with AS.
Material and Methods: The study was conducted in the Department of Rheumatology and Internal Diseases of the University Hospital in Wrocław among 110 patients (67 men and 43 women) with the diagnosis of AS, aged 20– 89 years (M=48.44 years, SD± 12.55). The study used the Acceptance of Illness Scale (AIS), the WHOQoL-BREF Quality of Life Scale, and a self-constructed questionnaire of clinical and sociodemographic data.
Results: Respondents rated the quality of life as good and moderate (M = 3.49 points, SD=± 0.84). The mean AIS score was 27.44 (SD=± 8.67). AIS scores are positively correlated with all QoL domains and perception of quality of life and health (p< 0.001). The strongest correlation was in the physical domain (r=0.71), while the weakest correlation was observed in the social domain (r=0.329). AIS and QoL measures showed significant relationships with selected sociodemographic data (eg, gender, age, education, and occupational activity) and correlated with selected disease data (eg, type of treatment used, duration of disease, or comorbidities).
Conclusion: AIS in patients with AS condition correlated positively with their QoL in all domains. Both disease acceptance and quality of life are influenced by specific sociodemographic and disease-related data. Prevention of complications and the type of treatment for AS (primarily biological treatment) can be essential in improving patients’ quality of life.
Keywords: ankylosing spondylitis, health-related quality of life, quality of life, acceptance of illness
Introduction
Ankylosing spondylitis (AS) is a chronic rheumatic inflammatory disease with a progressive course. The prevalence of AS is estimated in the general population to be between 0.55% and 6.1%. This condition is found more often in Caucasians (ie, white) and is diagnosed 2–3 times more often in men than in women.1 The development of this disease most often occurs in the second and third decade of life, and it appears quite rarely after 40 years of age. The first symptoms of the disease appear before the age of 30 in 80% of patients; in less than 5% of cases, the first symptoms appear after 45 years of age.2 It is estimated that there are approximately two hundred and fifty-thousand individuals in Poland with AS.3 Some studies have demonstrated increased mortality among people with AS compared to the general population. Shorter survival times generally follow from complications such as nephropathy, spine fractures, aortic valve regurgitation, respiratory failure, and upper gastrointestinal bleeding.4
The course of AS is progressive and chronic, and the symptoms vary in severity, with periodic exacerbations and remissions.5 The patient’s life is made more difficult by the progressive development of this disease and the complications that arise, and depressive disorders often appear.2 Pain, stiffness, sleep disturbances, and fatigue are the main symptoms in patients with AS. As the disease progresses, it leads to functional limitations, gradual loss of spine mobility, and deterioration of quality of life (QoL). AS increases the risk of depression, anxiety, and adaptation disorders due to life changes; the likelihood of unemployment also rises as a result of progressive disability. Living with and accepting this disease is particularly difficult as it mainly affects young people (in late adolescence or early adulthood), who are often in their period of greatest productivity, thus their life possibilities are limited, and their conventional adult social roles are weakened. This disease often forces patients to give up their life plans, thus they become socially isolated and their joy in life is limited. The chronicity, the incurable nature, and the unpredictable and progressive nature of this disease all pose a high risk that these patients often subordinate their lives to it.6,7
The QoL of patients with AS largely depends on the patient’s health status, including the progression of the disease and the degree of functional disability resulting from impairment of the locomotor system. Longer duration of the disease and the associated comorbidities also reduce QoL and increase the costs of providing effective health care. The QoL of patients with AS is also determined by sociodemographic factors, eg, marital status, social status, level of education or professional activity. It is generally accepted that AS worsens the QoL compared to the general population.8–10
AS is generally a significant challenge for those affected. It is a heavy burden for patients and their families as it often forces them to give up their current habits and pleasures and causes changes in their lifestyle. Factors such as treatment, medications, the bodily appearance changes caused by the disease, functional difficulties, and changes in relations with the environment may cause stress and depressive and anxiety disorders, and reduce life satisfaction.11,12
However, adjusting to the disease can improve the patient’s overall well-being. From a patient’s perspective, this adaptation may change their assessment of the effects of the disease, thus increasing life satisfaction, despite the resulting limitations. One factor that determines a change of attitude towards this disease is acceptance of it. The concept of disease acceptance is understood as accepting the fact that one is sick and recognizing the need to adapt to the disease and its consequences. Greater acceptance of a disease positively affects self-management of health and is associated with a better QoL for patients.13,14
In the holistic model, disease adaptation is determined by disease factors, socio-demographic and external factors (eg, social and institutional support), and personality factors, including acceptance of the disease.11,15 This study aimed to determine the impact of disease acceptance on the QoL of AS patients.
Method
Study Design and Setting
The study was conducted among adult patients at the Department of Rheumatology and Internal Diseases of the University Hospital in Wrocław (University centre, third-class hospital). The patients were selected through convenience sampling method. All patients were fully informed of the purposes of the study. Inclusion criteria included clinical diagnosis of AS, were in a stable state of disease, age 18 years and consent to an anonymous survey. People who did not consent to the study and were not able to complete the questionnaire on their own were excluded.
The study was conducted with the consent of the Bioethics Committee at the Medical University of Wrocław (No. KB-264/2020).
Research Tools
The study used the Acceptance of Illness Scale (AIS), the WHOQoL-BREF Quality-of-Life Scale, and self-constructed questionnaires to collect sociodemographic and clinical data.
Acceptance of Illness Scale (AIS)
The AIS scale, by Felton, Revenson and Hinrichsen,16 measures the degree of disease acceptance among adult patients. Acceptance of disease is expressed by the fact that negative emotions and reactions related to health are less intense. The greater the disease acceptance, the better the adaptation and the lower the severity of psychological discomfort. This scale contains eight statements that describe the negative consequences of this disease, acceptance of the limitations imposed by it, lack of self-sufficiency, feeling dependent on others, and reduced self-esteem. In each statement, the respondent determines the AIS scores by providing answers on a five-point scale, from 1 – “I strongly agree” to 5 – “I strongly disagree”. The range of all possible points ranges from 8 to 40, and the sum of the points obtained is a general measure of the degree of disease acceptance: the more points received, the higher the disease acceptance level.
WHOQoL-BREF Quality of Life Scale
The World Health Organization Quality of Life (WHOQoL-BREF)17 is an abbreviated version of the WHOQoL-100 questionnaire. It consists of 26 questions, of which 24 questions relate to four areas of life: physical, psychological, social, and environmental. Questions about the physical field diagnose the health and physical functioning of the respondent (7 questions). The psychological domain measures self-esteem, meaning in life, experiencing feelings, and self-acceptance (6 questions). The social domain relates to the respondent’s intimate life and relationship with the environment (3 questions). The environmental domain subscale captures the sense of security, pursuit of interests, the patient’s living conditions, and coping with everyday life (8 questions). An additional 2 questions analyse the subjective perception of QoL in terms of life satisfaction and perception of one’s own health condition. The questionnaire questions refer to the previous 2 weeks of life. Answers are given on a five-point scale, from 1 to 5, where a higher score indicates better QoL.17,18
Statistical Analysis
For the analysis of quantitative variables, the mean (M), standard deviation (SD), median (Me), quartiles (Q), minimum (min) and maximum (max) were calculated. The analysis of qualitative variables included the numbers and percentages. The comparison of results for groups was performed using the Mann–Whitney test; comparisons of values for three or more groups were performed using the Kruskal–Wallis test. In the case of significant differences, post-hoc analysis with Dunn’s test was performed.
The correlation analysis used the Spearman correlation coefficient (rho). In the statistical analysis, the significance threshold was assumed at the level of p = 0.05. Statistical calculations were performed in R software version 4.0.4.19
Results
One hundred and ten people took part in the study, including 67 men and 43 women. Patients’ ages ranged from 20 to 89 years, and the mean age was 48.44 years (SD = 12.55). The characteristics of the sample in terms of sociodemographic and clinical variables are presented in Table 1.
 |
Table 1 Characteristics of Sociodemographic and Clinical Variables. Quality of Life and Disease Acceptance (N = 110) |
The average assessment of the QoL of the respondents was 3.49 points (SD = 0.84), which suggested that their QoL is between good and average (neither good nor bad). The mean self-assessment of health was average: 3.11 points (SD = 0.86). The mean AIS score was 27.44 points; descriptive statistics for individual areas of QoL and disease acceptance are presented in Table 1.
The Relationship Between Disease Acceptance and QoL
Acceptance of the disease is positively correlated with all dimensions of QoL (p < 0.001), thus suggesting that increased acceptance of the disease was accompanied by a better QoL in all dimensions (Table 2).
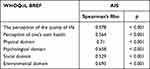 |
Table 2 Summary of Relations Between Disease Acceptance and Subscales of the WHOQoL-BREF Questionnaire |
Relationships Between Sociodemographic and Clinical Variables and QoL
Correlation analysis showed that there was a negative relationship between QoL in all subscales and age. Higher age correlated with lower overall QoL (rho = −0.33; p < 0.001), worse overall satisfaction with one’s health (rho = −0.22; p = 0.021), as well as poorer QoL in the physical (rho = −0.414; p < 0.001), psychological (rho = −0.393; p < 0.001), social (rho = −0.247; p = 0.009) and environmental domains (rho = −0.416; p < 0.001). Men obtained higher scores than women in the general quality-of-life subscale (p = 0.033), as well as in the physical (p = 0.01), psychological (p = 0.04) and environmental (p < 0.001) domains.
Among patients with higher education, compared to other categories of education, the general QoL (p = 0.003) and QoL measures in the physical (p = 0.006) and psychological (p = 0.01) domains were higher. On the other hand, QoL in the environmental field was higher in patients with secondary and higher education than in patients with primary and vocational education (p = 0.003).
The overall QoL measure and QoL in the social domain were higher in married than in single patients (p = 0.026 and p < 0.001, respectively). Patients living with relatives achieved higher scores than those living alone in the overall quality-of-life subscale (p < 0.001) and QoL measures in the psychological (p = 0.039) and social (p < 0.001) domains. Economically active people, compared to inactive people, reported higher overall QoL (p < 0.001), overall health satisfaction (p < 0.001), and QoL in all areas (p < 0.001).
People with disabilities, compared to those without a disability certificate, had lower overall QoL (p < 0.001), general satisfaction with health (p < 0.001) and QoL in terms of the physical (p < 0.001), psychological (p < 0.001) and environmental (p = 0.003) dimensions. These groups did not differ in QoL in the social field (p = 0.17).
Compared to those suffering for longer, people suffering from AS for 15 years or less showed better QoL scores on the overall QoL subscales (p = 0.019) and the physical (p = 0.002) and psychological (p = 0.008) subscales. Environmental QoL was significantly higher in patients aged 6–15 years than in patients aged over 15 (p = 0.002).
In the group of patients who only received biological treatment and the group of patients who received biological and pharmacological treatments, the QoL in the social field was higher than in patients who did not receive any treatment (p = 0.036).
Patients who had not been hospitalized in the last 12 months reported higher overall QoL (p = 0.024), overall health satisfaction (p = 0.01) and QoL in the physical (p = 0.039), psychological (p = 0.014) and social (p = 0.021) domains.
In the case of social support, the patients who received help from associations and support groups reported a lower overall QoL (p = 0.049); those who received institutional support reported even lower overall QoL (p = 0.007) and QoL in the physical (p < 0.001), psychological (p = 0.003) and environmental (p = 0.026) dimensions. People who declared no need for support assessed their overall QoL higher (p = 0.007) including the physical (p < 0.001) and psychological (p = 0.046) and the environmental (p = 0.009) QoL dimensions. Pet owners assessed their QoL as higher in the psychological (p = 0.037) and social (p = 0.03) domains compared to those without a pet.
People without vertebral fractures had higher QoL in the physical (p = 0.003), psychological (p = 0.004), social (p = 0.006) and environmental (p = 0.007) domains than those with such fractures. The group of people without cardiovascular system complications reported higher results in terms of overall QoL (p = 0.05) and QoL in the physical (p < 0.001) and psychological (p = 0.017) domains. People without digestive system complications had higher overall QoL (p = 0.002), better overall health satisfaction (p = 0.013), and better QoL in the physical (p < 0.001), psychological (p = 0.008) and environmental (p = 0.008) domains. Compared to those with these disorders, patients without mood disorders and depressive symptoms reported higher general satisfaction with their health (p = 0.003) and QoL in the psychological (p = 0.021), social (p 0.007), and environmental (p = 0.015) subscales. Detailed comparisons are presented in Table 3.
 |
Table 3 Relationships Between Sociodemographic and Clinical Variables and Quality of Life in patients with AS (N = 110) |
Relationships Between Sociodemographic and Clinical Variables and Disease Acceptance
The results of the Spearman correlation analysis showed a negative correlation between age and disease acceptance (rho = −0.47; p < 0.001). The disease acceptance level was higher in men than in women (p < 0.001). The level of acceptance of the disease increased with education: the highest level of acceptance was reported by people with higher education, whereas a significantly lower level of disease acceptance was reported by people with secondary/secondary vocational education, and the lowest degree was reported by people with primary/basic vocational education (p < 0.001).
The level of acceptance of the disease was higher 1) in the group of patients living with relatives compared to those living alone (p = 0.05); 2) in the group of economically active as compared to the economically inactive (p < 0.001); 3) in the group without a certificate of disability, compared to the disabled (p < 0.001); 4) in the group of patients suffering from disease for up to 15 years compared to patients suffering from disease for over 15 years (p = 0.01); 5) in the group of both biologically and pharmacologically treated patients than in the group of only pharmacologically treated patients (p = 0.011); 6) in the group of patients without vertebral fractures (p = 0.003) compared to patients without fractures; 7) in the group without gastrointestinal complications (p < 0.001) compared to patients with such complications; 8) in the group without mood/depressive disorders (p = 0.006) compared to those without these symptoms; 9) in people who had not been hospitalized in the last 12 months (p = 0.02) compared to those who had; 10) in the group not using institutional support (p < 0.001) compared to patients using this form of support; 11) in the group declaring no need for support (p = 0.005) compared to the group declaring the need for support. The exact results are shown in Table 4.
 |
Table 4 Relationships Between Sociodemographic and Clinical Variables and Disease Acceptance in patients with AS (N = 110) |
Discussion
AS is a chronic rheumatic inflammatory disease that significantly impacts the health and QoL of patients. The progressive inflammatory process ultimately leads to significant functional limitations and a deterioration in health-related QoL (HRQoL). Admittedly, the QoL of patients with AS is mainly determined by the activity of the disease and the level of disability.20–22
In this study, an attempt was made to assess the level of disease acceptance, QoL, and the impact of such acceptance on the QoL of patients with AS. Additionally, the relationships between selected sociodemographic or disease-related factors and disease acceptance or QoL were analysed.
In terms of sex, the largest group of respondents were men (60.91%), which may confirm the epidemiological data that show that the disease is more common in men. In a study by Nam et al, men constituted 76.3% of the respondents. Sixty percent of the patients in this study were aged between 20 and 50 years of age; this reflects the prevalence of AS in this age group. However, it should be noted that these were patients who had already been diagnosed with AS; as reported by Rosenbaum et al,23 the time from onset of this disease to diagnosis in a sample population of patients from the United States may be approx. 13 years.
In the present study, it was shown that the average AIS was 27.44, which means that the respondents neither accepted nor showed disapproval of their disease. Piekutin et al6 measured the comparable mean AIS in patients with AS, yielding an AIS score of 26.9. On the other hand, in studies of patients with systemic connective tissue diseases, Puto et al24 obtained an AIS score of 24.5 points.
The present study showed that the average perception of QoL (based on the WHOQoL-BREF) was 3.49 points (SD = 0.84), which means that the patients rated their QoL as good or average. On the other hand, the participants’ perception of their health was on average 3.11 points (SD = 0.86), thus indicating that their health assessment was neither satisfactory nor unsatisfactory. Taking into account individual quality-of-life areas, the respondents gave the best results in the social field (14.25 ± 2.77), and slightly worse results in the environmental (14.18 ± 2.12) and psychological (13.29 ± 2.41) areas. The QoL in the physical field was assessed as lowest (13.05 ± 2.32). According to Yang et al,25 health-related QoL in AS is lower than in type II diabetes and is comparable to rheumatoid arthritis.
In this study, a positive correlation was observed between disease acceptance and QoL in patients. In research on the QoL of patients with AS, several questionnaires are used, such as EASiQoL (Evaluation of Ankylosing Spondylitis Quality of Life), ASQoL (Ankylosing Spondylitis Quality of Life), SF-36 (Short-Form Health Survey-36), SF-6D, the 15D questionnaire and EQ-5D (EuroQoL-5 dimension-3). To some extent, such diversity of measures prevents direct comparisons with the obtained results of the WHOQoL-BREF. Nevertheless, the present results largely agree with the results of previously published studies.
Research conducted in the US by Rosenbaum et al23 showed a negative impact of AS on all areas of QoL and on various aspects of lifestyle, including sports and career choice. As in the present study, the greatest negative impact of AS was observed in the physical domain. In turn, in a study on the QoL of patients with AS (compared to the general population) in Sweden, Law et al26 found that patients had lower scores in QoL domains that reflect physical and mental health, and patients’ QoL in the physical domain was lower than in the psychological domain. In studies on patients diagnosed with AS in South Korea, Nam et al27 also found that respondents had low QoL, especially when the disease was progressing rapidly.
The present study showed that disease acceptance depended on gender and was significantly higher in men than in women. Puto et al24 similarly found that women have a lower level of disease acceptance and greater difficulties in adapting to living with this disease. A study by Rosenbaum et al23 indicated that women suffering from AS had greater disease activity than men and less frequently had children than the general population.
This study also found correlations between gender and QoL. Men had higher QoL in the physical, psychological and environmental domains, and higher subjective perception of QoL. Nam et al27 also found differences in QoL in AS in terms of sex: men had better QoL, and changes detected by radiographic measures were more pronounced in women. On the other hand, Law et al26 found that there may be some gender differences in individual HRQoL parameters, showing that there are no significant gender differences in the physical and psychological domains. The only significant difference that appeared was lower scores in the SF-36 physical domain in women.
Our analysis showed that disease acceptance decreased with increasing age. Similarly, age negatively correlated with overall QoL and poorer QoL in all WHOQoL domains. Higher education was associated with greater acceptance of the disease (p < 0.001). The economically active group was characterized by greater acceptance of the disease (29.61 ± 8.11) than the economically inactive group (21.34 ± 7.42). Similar results were obtained by Puto et al,24 who stated that acceptance of the disease decreased with age but increased with education level. Economically active people were shown to accept the condition better than the economically inactive, including pensioners, retirees, or other benefit recipients. It is presumed that higher acceptance of the disease in working people may result from lower disease activity than in non-working individuals.
In the context of the relationship between age and QoL in AS, in a study of a patient population in Scotland, Dean et al8 showed that women were more likely to have reduced QoL. At the same time, Law et al26 showed an inverse relationship between the physical component of QoL (SF-36) and the age of respondents. When examining Korean patients with AS, Nam et al27 noticed that disease activity and functional impairment are associated with low QoL and depression. These researchers identified several factors that reduce QoL: depression, poorer education, low income, lower self-efficacy, life without a partner, smoking, and a reduced sense of control over life and this disease.
In the present study, it was found that the duration of the disease correlated with acceptance of the disease (p = 0.01): people who had suffered for longer (>15 years) had a lower level of acceptance than those who had suffered for a shorter time. Piekutin et al6 also demonstrated that patients with longer AS duration (>20 years) displayed reduced acceptance of this disease (p = 0.0001).
Analysis of the relation between QoL measures and disease duration indicated significant outcomes for selected QoL domains. The subjective perception of QoL as well as the QoL scores in the physical and psychological domains were better in patients aged <15 than in patients aged >15 years; in the environmental domain, QoL was higher in patients aged 6 to 15 years than in patients aged >15 years. This relationship was not confirmed by Alkan et al,20 who studied Turkish patients with AS and found no relationships between QoL and disease duration, age, and BMI of patients. On the other hand, this Turkish study demonstrated a strong and positive correlation between the ASQoL parameter and disease activity (r = 0.721; p < 0.001), and moderate correlations with functional status, spine mobility, and pain level.
Our study showed that the type of treatment influences acceptance of this disease (p < 0.011). Patients treated biologically (27.56 ± 10.25), especially those who were treated both biologically and pharmacologically (29.98 ± 6.94), had higher acceptance of the disease than patients treated only pharmacologically (23.24 ± 7, 88). Improvements in disease acceptance associated with biological treatment may result from the better efficacy of biological drugs than conventional drugs. For instance, Kotulska et al28 found that biological treatment improves the physical and functional conditions of patients in rheumatic diseases (RA, AS, PsA and JIA) and the interpersonal relations of patients. Particularly in the treatment of AS, the beneficial effect of biological treatment on sleep quality and improved sex life has additionally been emphasized. Ali et al29 noted the positive impact of treatment with TNF inhibitors and presented recommendations for the management of spondyloarthritis (including AS) in Kuwait. In a study of axial spondyloarthritis in Norway, Rohde et al30 found that patients’ QoL (the HRQoL score) did not deteriorate over the five years of follow-up, despite their increased age and comorbidities due to the effects of biological treatment. These authors argued that targeted treatment of AS represents a form of drug treatment that is efficiently adapted to this disease, thus positively impacting HRQoL.
The present results correspond with Puto et al’s24 general conclusion that AIS depends on clinical factors (eg, course and severity of the disease) and sociodemographic such as age, sex, material status, or education level.
This study did not show any correlation between marital status or place of residence and disease acceptance, as was also found by Piekutin et al. However, Puto et al24 found a relationship between disease acceptance, marital status, and place of residence. We also found that marital status had a significant impact on QoL, and people in a relationship had a better perception of their QoL, and a better QoL in the social field. On the other hand, the place of residence did not significantly affect the QoL of patients with AS.
In addition, the present study of AS showed that respondents living with a relative or relatives (28.17 ± 8.22; n = 94) displayed greater acceptance of this disease than those living alone (23.12 ± 10.24; n = 16). A further analysis of our data showed no correlation between social support and disease acceptance, even though most respondents (n = 93) indicated that they had support in the form of family or a lifelong companion. It turned out that living in close relationships with others positively influenced QoL. In particular, subjective perception of QoL (p < 0.001) and QoL in the psychological (p = 0.039) and social (p = 0.001) domains for those patients were better compared to those of people living alone. In comparison, Law et al26 showed that single people living without a partner had a significantly worse QoL in the physical domain (the SF-36 measure).
Most of the respondents had a disability certificate (33.64%), and their disease acceptance and QoL were significantly lower than in the group without such a certificate and in the group not hospitalized in the last 12 months. Also, patients who had poor social support or declared that they did not need it had a higher level of disease acceptance and a better QoL. These associations presumably resulted from greater disease activity or greater impairment among these groups of patients (with a certificate of disability or with support).
Significant correlations between disease acceptance and complications concerned vertebral fractures (p = 0.003), and digestive system (p < 0.001) and mood/depressive disorders (p = 0.006). Similarly, a significantly better QoL (p < 0.05) was observed in the group of people who did not have vertebral fractures, cardiovascular and digestive system complications, or mood/depressive disorders.
When examining QoL in patients with AS we can find gender differences in comorbidities eg women more often than men had depression and fibromyalgia, and men more often had arterial hypertension and heart disease.23,31 In the coexistence of two or more chronic diseases affects the QoL of patients with AS. Makovski et al found that QoL deteriorates as the number of comorbidities increases and is more likely to be affected by physical health than by mental health. Also analysis revealed that a bigger decrease in HRQoL occurred in younger individuals who had multiple comorbidities.10
AS is characterized, inter alia, by chronic fatigue, sleep disturbances, and lower-back pain. According to Uchmanowicz et al,32 sleep disturbances affect QoL in patients with chronic lower-back pain and have a negative impact on daily functioning and QoL. Fatigue, which is common in rheumatic diseases, is another negative factor that reduces QoL and the level of professional and social functioning. This was emphasized by Ali et al33 in a study of patients with autoimmune rheumatic diseases, including spondyloarthropathies.
This study also examined how having a pet affects disease acceptance and QoL in AS patients. By analysing the relationship between welfare and dog ownership in a study of Canadian patients with chronic back problems, Carr et al34 confirmed the beneficial effect of this factor on the physical, mental and social domains. Similar studies among older adults suggest that having pets may benefit owners in terms of social relationships and mental health.35,36 However, this analysis of pet ownership did not reveal any significant correlation with disease acceptance. However, QoL depended on having a pet because psychological (p = 0.037) and social (p = 0.03) QoL were better in the group of participants who owned a pet.
The above study and literature results show that AS negatively affects all dimensions of QoL. In the group of patients with AS, their acceptance of the disease and QoL depend on clinical factors, including those related to the disease, as well as sociodemographic factors. In addition to QoL and AIS, patients’ psychological factors are also important, including a sense of self-efficacy, a sense of coherence, or coping with stress.
Some limitations in our study should be taken into account when interpreting the results. Firstly, all data were collected in cross-sectional surveys, and therefore causal relationships could not be established. Also all patients were recruited from a one hospital, and as a result our findings need to be confirmed in other settings to assess their generalisability. In our study, subdomains of axial spondyloarthritis, including entheses and spinal mobility, were not examined.
Conclusion
The disease acceptance influences QoL in all its dimensions in the case of AS. Our results suggest that therapeutic measures aimed at strengthening AIS can improve QoL in patients with AS. Prevention of complications and biological treatment tailored to the progression of AS can enhance patients’ QoL. The presented analysis can also be used in planning effective therapeutic management in the treatment and care of patients with AS.
Abbreviations
AIS, Acceptance of Illness Scale; AS, ankylosing spondylitis; QoL, quality of life; M, mean; WHO, World Health Organization.
Data Sharing Statement
All relevant data are included with in the manuscript document. If it is necessary, it is possible to contact the corresponding author to get additional materials.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the Good Clinical Practice (GCP) guidelines and the recommendations of the Declaration of Helsinki developed by the World Medical Association. Participation in the survey was voluntary, no personal data were collected, and anonymity was always maintained. All potential participants received written information on the study (reason for the study, objective, processes, data protection) and had the opportunity to contact the investigators in case of questions at any time of the study. Informed consent to participate was assumed by individuals filling out the questionnaire and had to be confirmed (by ticking a box) at the beginning of the questionnaire. The study was approved by the Bioethics Committee of Wroclaw Medical University (KB 264/2020).
Acknowledgments
We wish to thank all the patients who participated in the study.
Funding
This research was funded by the Ministry of Science and Higher Education of Poland under the statutory grant of the Wroclaw Medical University (SUBZ.E250.23.020).
Disclosure
The authors declare that they have no competing interests.
References
1. Przepiera-Będzak H, Brzosko M. Zesztywniajace zapalenie stawów kręgosłupa [Ankylosing spondylitis]. In: Puszczewicz M, editor. Wielka Interna Reumatologia. Warszawa: Medical Tribune Polska; 2016:283–288.
2. Zimmermann-Górska I. Zesztywniajace zapalenie stawów kręgosłupa [Ankylosing spondylitis]. In: Gajewski P, editor. Interna Szczeklika 2020. Kraków: Medycyna Praktyczna; 2020:2104–2111.
3. Wieczorek-Chełmińska Z. Zesztywniające zapalenie stawów kręgosłupa Ważniejsze choroby układu kostno-stawowego [Ankylosing spondylitis. The important diseases of the osteoarticular system]. In: Wieczorek-Chełmińska Z, editor. Żywienie w chorobach kostno-stawowych [Nutrition in osteoarticular diseases]. Warszawa: Wydawnictwo Lekarskie PZWL; 2015:23–24.
4. Taurog J. Spondyloartropatie. In: Fauci A, Langford C, editors. Harrison Reumatologia. Lublin: Wydawnictwo Czelej Sp. z o.o; 2012:150–170.
5. Sierakowska M, Sierakowski S. Opieka pielęgniarska nad pacjentem z zesztywniającym zapaleniem stawów kręgosłupa [Nursing care of a patient with ankylosing spondylitis]. In: Jurkowska G, Łagoda K, editors. Pielęgniarstwo internistyczne. Warszawa: Wydawnictwo Lekarskie PZWL; 2015:462–471.
6. Piekutin A, Sierakowska M, Doroszkiewicz H, Krajewska-Kułak E. Evaluation of coping with chronic rheumatic disease, in the context of socio-demographic factors and disease duration, based on the example of patients with ankylosing spondylitis. Reumatologia. 2018;56(6):368–376. doi:10.5114/reum.2018.80714
7. Huang JC, Qian BP, Qiu Y, et al. Quality of life and correlation with clinical and radiographic variables in patients with ankylosing spondylitis: a retrospective case series study. BMC Musculoskelet Disord. 2017;18(1):1–10. doi:10.1186/s12891-017-1711-1
8. Dean LE, MacFarlane GJ, Jones GT. Five potentially modifiable factors predict poor quality of life in ankylosing spondylitis: results from the Scotland registry for ankylosing spondylitis. J Rheumatol. 2018;45(1):62–69. doi:10.3899/jrheum.160411
9. Sallam RA, Elbahnasawy AS. Health related quality of life (HRQoL) in ankylosing spondylitis patients: relation to clinical features, disease activity and radiographic damage. Egypt Rheumatol. 2020;42(4):287–290. doi:10.1016/j.ejr.2020.02.006
10. Makovski TT, Schmitz S, Zeegers MP, Stranges S. Multimorbidity and quality of life: systematic literature review and meta-analysis. Ageing Res Rev. 2019;52:53. doi:10.1016/j.arr.2019.04.005
11. Miniszewska J. Bycie z chorobą. Przystosowanie do wybranych przewlekłych chorób somatycznych z perspektywy psychologii pozytywnej i koncepcji poznawczych [Being with illness. Adapting to selected chronic somatic diseases from the perspective of positive psychology and cognitive concepts]. Łódź: Wydawnictwo Uniwersytetu Łódzkiego; 2019.
12. Bakan G, Inci FH. Predictor of self-efficacy in individuals with chronic disease: stress-coping strategies. J Clin Nurs. 2021;30(5–6):874–881. doi:10.1111/jocn.15633
13. Szcześniak M, Świątek AH, Cieślak M, Świdurska D. Disease acceptance and eudemonic well-being among adults with physical disabilities: the mediator effect of meaning in life. Front Psychol. 2020;11:1–10. doi:10.3389/fpsyg.2020.525560
14. Qiu C, Zhang X, Zang X, Zhao Y. Acceptance of illness mediate the effects of health literacy on self-management behaviour. Eur J Cardiovasc Nurs. 2020;19(5):411–420. doi:10.1177/1474515119885240
15. Livneh H, Antonak RF. Psychosocial Adaptation to Chronic Illness and Disability. Gaithersburg, MD: Aspen; 1997.
16. Felton BJ, Revenson TA, Hinrichsen GA. AIS-acceptance of illness scale. In: Juczyński Z, editor. Measurement Tools in Promotion and Health Psychology. Warszawa: Laboratory of Psychological Tests of Polish Psychological Association; 2001:158–167.
17. World Health Organization. Whoqol-bref introduction, administration, scoring and generic version of the assessment. Geneva: Programme on mental health world health organization. 1996. Available from: https://www.who.int/mental_health/media/en/76.pdf.
18. Cheung YB, Yeo KK, Chong KJ, Khoo EYH, Wee HL. Measurement equivalence of the English, Chinese and Malay versions of the world health organization quality of life (WHOQOL-BREF) questionnaires. Health Qual Life Outcomes. 2019;17(1):1–6. doi:10.1186/s12955-019-1130-0
19. R Core Team. R: A language and environment for statistical computing. Version 4.0.4. 2021. Vienna, Austria: R Foundation for Statistical Computing. Available from: http://www.R-project.org/.
20. Alkan H, Yildiz N, Ardiç F. The correlations between disease specific quality of life, short form-36 and clinical variables in patients with ankylosing spondylitis. Arch Rheumatol. 2020;35(4):468–476. doi:10.46497/ArchRheumatol.2020.7750
21. López-Medina C, Garrido-Castro JL, Castro-Jiménez J, et al. Evaluation of quality of life in patients with axial spondyloarthritis and its association with disease activity, functionality, mobility, and structural damage. Clin Rheumatol. 2018;37(6):1581–1588. doi:10.1007/s10067-018-4112-4
22. Chiowchanwisawakit P, Thaweeratthakul P, Wattanamongkolsil L, et al. Relationship between health-related quality of life and patient acceptable symptom state with disease activity and functional status in patients with ankylosing spondylitis in Thailand. J Clin Rheumatol. 2019;25(1):16–23. doi:10.1097/RHU.0000000000000750
23. Rosenbaum JT, Pisenti L, Park Y, Howard RA. Insight into the quality of life of patients with ankylosing spondylitis: real-world data from a US-based life impact survey. Rheumatol Ther. 2019;6(3):353–367. doi:10.1007/s40744-019-0160-8
24. Puto G, Repka I, Zurzycka P, Kowalska U. Socio-demographic determinants of the acceptance of systemic connective tissue diseases. Reumatologia. 2018;56(1):31–36. doi:10.5114/reum.2018.74746
25. Yang X, Fan D, Xia Q, et al. The health-related quality of life of ankylosing spondylitis patients assessed by SF-36: a systematic review and meta-analysis. Qual Life Res. 2016;25(11):2711–2723. doi:10.1007/s11136-016-1345-z
26. Law L, Beckman Rehnman J, Deminger A, et al. Factors related to health-related quality of life in ankylosing spondylitis, overall and stratified by sex. Arthritis Res Ther. 2018;20(1):1–12. doi:10.1186/s13075-018-1784-8
27. Nam B, Koo BS, Nam SW, et al. Gender differences in factors associated with low quality of life and depression in Korean patients with ankylosing spondylitis. Qual Life Res. 2021;30:2299–2310. doi:10.1007/s11136-021-02800-w
28. Kotulska A, Kucharz EJ, Wiland P, et al. Satisfaction and discontent of Polish patients with biological therapy of rheumatic diseases: results of a multi-center questionnaire study. Reumatologia. 2018;56(3):140–148. doi:10.5114/reum.2018.76901
29. Ali Y, Abutiban F, Alawadhi A, et al. Recommendation for the management of spondyloarthritis patients in Kuwait. Open Access Rheumatol Res Rev. 2020;12:147–165.
30. Rohde G, Berg KH, Pripp AH, Prøven A, Haugeberg G. No deterioration in health-related quality of life in patients with axial spondyloarthritis followed for 5 years in ordinary outpatient clinics in the biological treatment era. Qual Life Res. 2020;29(1):99–107. doi:10.1007/s11136-019-02308-4
31. Ben-Shabat N, Watad A, Shabat A, et al. Low vitamin D levels predict mortality in ankylosing spondylitis patients: a nationwide population-based cohort study. Nutrients. 2020;12:5. doi:10.3390/nu12051400
32. Uchmanowicz I, Kołtuniuk A, Stępień A, Uchmanowicz B, Rosińczuk J. The influence of sleep disorders on the quality of life in patients with chronic low back pain. Scand J Caring Sci. 2019;33(1):119–127. doi:10.1111/scs.12610
33. Ali S, Matcham F, Irving K, Chalder T. Fatigue and psychosocial variables in autoimmune rheumatic disease and chronic fatigue syndrome: a cross-sectional comparison. J Psychosom Res. 2017;92:1–8. doi:10.1016/j.jpsychores.2016.11.002
34. Carr ECJ, Wallace JE, Pater R, Gross DP. Evaluating the relationship between well-being and living with a dog for people with chronic low back pain: a feasibility study. Int J Environ Res Public Health. 2019;16:8. doi:10.3390/ijerph16081472
35. Hui Gan GZ, Hill AM, Yeung P, Keesing S, Netto JA. Pet ownership and its influence on mental health in older adults. Aging Ment Heal. 2020;24(10):1605–1612. doi:10.1080/13607863.2019.1633620
36. Tański W, Świątoniowska-Lonc N, Dudek K, Jankowska-Polańska B. Benefit of biological drugs for quality of life in patients with ankylosing spondylitis: a systematic review and meta-analysis of clinical trials. Adv Exp Med Biol. 2020. doi:10.1007/5584_2020_611
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
