Back to Journals » Clinical and Experimental Gastroenterology » Volume 16
Indications and Findings of Upper Gastrointestinal Endoscopy at a Tertiary Hospital in Ethiopia: A Cross-Sectional Study
Authors Argaw AM , Ethiopia SS , Lelisa G, Fisseha H , Mulugeta B
Received 21 August 2023
Accepted for publication 20 October 2023
Published 28 October 2023 Volume 2023:16 Pages 187—196
DOI https://doi.org/10.2147/CEG.S436329
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Vipul Yagnik
Abel Mureja Argaw,1 Samrawit Solomon Ethiopia,2 Geda Lelisa,1 Henok Fisseha,1 Biruk Mulugeta1
1Department of Internal Medicine, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2School of Public Health, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Correspondence: Abel Mureja Argaw, Department of Internal Medicine, St. Paul’s Hospital Millennium Medical College, Swaziland Street, P.O. Box – 1271, Addis Ababa, Ethiopia, Email [email protected]
Background: Gastrointestinal disease is a significant global health problem. Symptoms related to digestive system diseases negatively affect quality of life and impose a significant economic impact. Upper gastrointestinal symptoms are common in the Ethiopian population, and the associated pathologies are diverse. Real-time endoscopic visualization of the upper gastrointestinal tract is crucial for diagnosis. However, local data on the indications for endoscopic evaluation and the common underlying pathologies are limited. This study aimed to assess the common indications and upper gastrointestinal endoscopic findings of patients presenting to Saint Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia.
Methods: A cross-sectional study was conducted by reviewing the complete records of patients who underwent upper gastrointestinal endoscopic evaluation between January 2012 and December 2019. A structured checklist was used to screen records for completeness. Data were analyzed using Statistical Package for the Social Sciences software version 25. Chi-square test was used to compare variables, with statistical significance set at P < 0.05.
Results: A total of 5753 patients underwent complete upper gastrointestinal tract endoscopic evaluation during the study period. The median age of the patients was 37 years. Males accounted for 63.4% of the patients. Dyspepsia (27.8%) was the most common indication for upper gastrointestinal endoscopic evaluation, followed by upper gastrointestinal bleeding (17.1%), and screening for varices (16.8%). Esophageal varices (35.8%), gastritis (18.1%), and duodenal ulcers (10.6%) were the most common pathologies found on esophagus, stomach, and duodenum, respectively. Common upper gastrointestinal pathologies are predominant among males and patients in their third decade of life.
Conclusion: Dyspepsia was the most common indication for endoscopic evaluation of the upper gastrointestinal tract. Esophageal varices were the most common pathological finding, followed by gastroesophageal reflux disease, gastritis, portal hypertensive gastropathy, duodenal ulcer, and hiatal hernia. Esophagogastroduodenoscopy remains a vital tool for the diagnosis of pathologies of the upper gastrointestinal tract.
Keywords: dyspepsia, gastritis, GERD, esophageal varices, Ethiopia
Introduction
Symptoms of digestive system disorders are among the most common presenting complaints for primary healthcare practitioner visits.1,2 These symptoms negatively affect quality of life and have a significant economic impact on health service and society.3–5 They are common among the majority of the world. In population-based studies, the prevalence of uninvestigated dyspepsia has varied between 7% and 34.2%.6,7
Helicobacter pylori, a gram-negative bacillus, is associated with a number of upper gastrointestinal disorders, including chronic active gastritis, peptic ulcer disease, lymphoma, and gastric tumors.8 Although it is prevalent globally, its impact is immense in countries with poor environmental and socioeconomic status, including Ethiopia, with pooled prevalence of 52.2%.9–11
In addition to dyspepsia, patients with upper gastrointestinal (GI) pathologies may also present with, dysphagia, odynophagia, gastrointestinal bleeding, persistent anorexia, nausea/vomiting with or without weight loss.8 In an attempt to have a better understanding of these upper GI pathologies, different diagnostic modalities have been used for over 200 years.8,12
Upper gastrointestinal endoscopy, also called esophagogastroduodenoscopy (EGD), involves the visualization of the upper part of the gastrointestinal tract.13 It is performed by passing a flexible endoscope through the mouth into the esophagus all the way to the second part of the duodenum, with real-time assessment and interpretation of the findings encountered.8,13 EGD is the method of choice for examining the upper GI system. It is superior to the upper gastrointestinal radiographic series for the detection of gastric ulcers and flat mucosal lesions, such as Barrett’s esophagus.8 It is also the gold standard test for diagnosing malignancy of the upper GI tract, such as gastric tumors and esophageal adenocarcinoma.14 It not only achieves the diagnosis of these and many other upper GI diseases but also provides the opportunities for therapeutic interventions with minimally invasive options.8,12 Previous studies have shown that endoscopy is a fairly accurate and safe procedure that should be available and applied widely for the diagnosis of upper gastrointestinal diseases in developing countries.15,16
Different studies have found that upper gastrointestinal diseases are prevalent among adults in Ethiopia.17–20 Although four decades have passed since endoscopic evaluation of the gastrointestinal tract has been started in Ethiopia, it is not widely available and patients are referred from remote places to central areas for evaluation.15
There is a paucity of published data regarding upper gastrointestinal diseases in Ethiopians with symptoms who are referred for endoscopy. To our knowledge, there are only four digitally published studies regarding endoscopic evaluations of upper gastrointestinal diseases in the country, of which two are more than a decade old and others were conducted in northern Ethiopia.15,16,21,22 Given this gap in the literature, and the importance of information on upper gastrointestinal diseases, this study aimed to assess the indications and upper gastrointestinal endoscopic findings of patients presenting to Saint Paul’s Hospital Millennium Medical College (SPHMMC), Addis Ababa, Ethiopia, to see the change in pattern of endoscopic findings, upper gastrointestinal pathologies over time and differences based on geographic area.
Materials and Methods
The study was conducted at St. Paul’s Hospital Millennium Medical College, the second-largest governmental tertiary care hospital in Addis Ababa, Ethiopia. It is a medical center with a catchment area of more than five million people. The Gastroenterology and Hepatology unit has four subspecialists and has been providing endoscopic evaluation of the gastrointestinal tract service since 2011.23,24
A hospital-based descriptive cross-sectional study was conducted using documented reports of patients who underwent diagnostic upper gastrointestinal endoscopic examination from January 2012 to December 2019 at St. Paul’s Hospital Millennium Medical College endoscopy unit, including patients from the hospital and those referred from other health institutions. Patients with incomplete upper gastrointestinal endoscopic reports, duplicate records and therapeutic endoscopic reports were excluded from this study.
Data on the age and sex of the patients, indications for upper gastrointestinal endoscopy (UGIE), and endoscopic findings were retrieved from the endoscopy results available at the endoscopy unit. The investigators manually checked the patient records for completeness before data entry. The computerized data were checked by a data supervisor for incompleteness.
The following definitions of endoscopic findings were used during the procedure: Esophageal varices (EV) were defined as dilated submucosal veins in the lower third of the esophagus. Grade 1 EV: small, straight varices; Grade 2 EV: enlarged, tortuous varices that occupy less than one-third of the lumen; and Grade 3 EV: large, coil-shaped varices that occupy more than one-third of the lumen. Gastroesophageal varices (GOV) are esophageal varices that extend down to the stomach, with GOV-1 being esophageal varices extending along the lesser curvature of the stomach, and GOV-2 being esophageal varices extending along the greater curvature. Gastroesophageal reflux disease (GERD) is a condition that develops when reflux of the stomach contents causes troublesome symptoms and/or complications. Los Angeles (LA) classification of GERD was used with LA Grade A: one or more mucosal breaks each ≤5 mm in length; LA Grade B: at least one mucosal break >5 mm long, but not continuous between the tops of adjacent mucosal folds; LA Grade C: at least one mucosal break that is continuous between the tops of adjacent mucosal folds, but which is not circumferential; and LA Grade D: mucosal break that involves at least three-quarters of the luminal circumference.12
Data were analyzed using Statistical Package for the Social Sciences (SPSS) software version 25. Data were summarized using descriptive statistics, including frequencies, medians, and percentages, and are summarized in tables and graphs. Chi-square test was used to compare variables, with statistical significance set at P < 0.05.
Results
Demographic Characteristics of the Study Sample
A total of 6374 documented records of upper gastrointestinal endoscopic evaluations performed between January 2012 and December 2019 were reviewed; 621 were ineligible because of incomplete documentation (n = 529) and duplicate records (n = 92). Data from 5753 patient records were analyzed, yielding a completeness rate of 90.3%.
Of the 5753 patients, 3648 (63.4%) were male and 2105 (36.6%) were female. The median age was 37 years, with the youngest and oldest patients aged 4 and 97 years, respectively. Half of the population were in the age groups of 21–30 years (28.8%) and 31–40 years (22.9%) (Table 1).
 |
Table 1 Age and Sex Distribution of Patients Who Underwent Upper Gastrointestinal Endoscopy at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, 2012 to 2019 (N = 5753) |
Indications for Upper Gastrointestinal Endoscopy and Findings
Dyspepsia, which accounted for 27.8% (n = 1597) cases, was the most common indication for undergoing upper gastrointestinal endoscopy, followed by upper GI bleeding 17.1% (n = 983) and screening for varices in patients with chronic liver disease (CLD) 16.8% (n = 968) (Figure 1).
 |
Figure 1 Indications for upper gastrointestinal endoscopy at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, 2012 to 2019 (N = 5753). |
Less common indications which accounted for 2.2% included odynophagia, foreign body removal, weight loss, chronic diarrhea, caustic ingestion, halitosis, globus sensation, and chronic hiccups.
Upper gastrointestinal endoscopic examinations were normal in 10.7% (n = 616) patients, while pathologies were found in 89.3% (n = 5137), with 65.1% (n = 3344) being male.
In patients with dyspepsia, the predominant pathologies identified were gastritis 34.9% (n = 557), gastroesophageal reflux disease 27% (n = 431), and duodenal ulcers 12.7% (n = 203). Eighteen percent (n = 287) of dyspeptic patients had normal upper gastrointestinal endoscopy.
Among patients with upper gastrointestinal bleeding, 51.8% (n = 509) had esophageal varices, followed by duodenal ulcers 15.4% (n = 151), gastritis 11.2 (n = 110), gastric ulcers 6.0% (n = 59), gastric tumors 3.3% (n = 32), and Mallory Weiss tears 0.4% (n = 4). Normal findings were reported in 6.7% (n = 66) of the patients. Esophageal varices also accounted for 87.4% (n = 692) of patients who underwent repeat UGIE with indication of follow-up.
The most common lesions identified in individuals with dysphagia (n = 375) were esophageal tumors 42.9% (n = 161), achalasia 13.3% (n = 50), and esophageal stricture 5.3% (n = 20), while no pathology was identified in 18.9% (n = 71) of them.
Endoscopic Findings on Esophagus
The most common findings on esophageal endoscopic evaluation were esophageal varices (35.8%), followed by normal examination (34.9%), gastroesophageal reflux disease (14.7%), and hiatal hernia (9.2%) (Table 2).
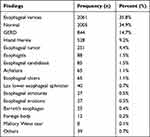 |
Table 2 Common Findings on Esophageal Endoscopy at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, 2012 to 2019 (N = 5753) |
Less common findings on esophagus (others) included pseudo-diverticulum, tracheoesophageal fistula, extrinsic compressions, vascular ectasias, and non-malignant esophageal masses, which altogether were observed in 0.7% of the population.
Among patients with esophageal varices (n = 2061), the majority had grade 3 (42.6%) and grade 2 (39.2%) varices, while 17.2% had grade 1 varices, and 1% did not have grading of varices documented. In approximately 12% (n = 247) of these patients, varices had extended down to the stomach, of which the most common type was Gastro-Oesophageal Varices type-1 55.1% (n = 133), followed by GOV-2 32.8% (n = 79), while the rest had GOV-1 and GOV-2 combined.
In patients with GERD, nearly half of the cases (47.7%) were type Los Angeles (LA) grade A, LA grade B (30%), and LA grade C (11%), while LA grade D was the least common (3.7%) type. LA grade was not documented in 8%. Reflux related mucosal changes suggestive of Barrett’s esophagus were observed in only 0.4% (n = 25).
Esophageal tumors were found only in 4.4% (n = 251) of the study population, and nearly half (45.4%) were located in the distal part, while 41.8% were in the mid esophagus.
Endoscopic Findings on Stomach
Thirty-seven percent (n = 2131) of the study population had normal findings. The most frequently identified abnormal endoscopic findings were gastritis (18.1%), portal hypertensive gastropathy (15.3), gastric ulcers (4.2%), and gastric tumors (4.1%) (Table 3).
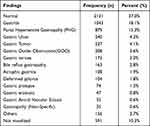 |
Table 3 Common Findings on Endoscopy of Stomach at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, 2012 to 2019 (N = 5753) |
Less common findings (others) on stomach included vascular ectasias, deformed antrum, gastric diverticula, extrinsic compression, foreign bodies in the stomach, gastric volvulus, and situs inversus, which altogether were observed in 2.7% of the population.
The antrum was the most commonly affected region of stomach, by both gastritis (56%) and gastric ulcers (32.9%).
Isolated gastric varices (IGV) were found in 2.9% (n = 166) of the study sample, in which IGV-l was the predominant subtype (89.2%), and both IGV-1 and 2 were seen in three patients.
Endoscopic Findings on Duodenum
More than half of the study population had a normal duodenal endoscopic finding (62.9%). The common abnormal findings were duodenal ulcers (10.6%), duodenitis (4.8%), and duodenal cap deformities (2.9%) (Table 4).
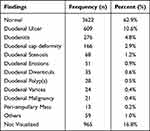 |
Table 4 Common Findings on Endoscopy of Duodenum at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, 2012 to 2019 (N = 5753) |
In 64% (n = 390) of patients with duodenal ulcer, it was located in the first part of the duodenum, of which 41.5% (n = 162) were in the duodenal bulb/cap.
Less frequent findings on duodenal endoscopy (others) included duodenal fistula, atrophic duodenitis, pseudo-diverticula, and vascular ectasias, found in 1% of the study population.
Gender Wise Distribution of Upper Gastrointestinal Endoscopic Findings
Among the main findings, esophageal varices and hiatal hernias were found more frequently among males than females with p-values of <0.001 and 0.042, respectively, while esophageal tumors showed a slight female predominance (P < 0.001). Similarly, gastritis, portal hypertensive gastropathy, and duodenal ulcers were more frequently diagnosed in males (P < 0.001), while atrophic gastritis was more frequently seen in females (P < 0.001). Duodenal ulcer (P < 0.001), duodenal stenosis (P = 0.003) and duodenal cap deformity (P = 0.004) were also more frequently diagnosed in males.
Age Wise Distribution of Upper Gastrointestinal Endoscopic Findings
Patients in the age group of 21–30 years had the highest prevalence of esophageal varices 33.4% (n = 688), GERD 26.8% (n = 226), and hiatal hernias 24.2% (n = 128), followed by age groups of 31–40 years and 41–50 years in a similar order.
Esophageal tumors were more predominant in the age groups of 51–60 years (27.1%), followed by 41–50 years (21.9%) and 61–70 years (17.5%), respectively.
Discussion
This study presents a comprehensive overview of upper gastrointestinal endoscopic findings and common indications among patients at St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia. The findings have shown that upper GI tract diseases are common among Ethiopians, with 89.3% of the endoscopic evaluations reporting one or more pathological findings.
Dyspepsia, the most common indication for patients to undergo UGIE, in this study was lower (27.8%) than similar local studies conducted in Tikur Anbessa teaching hospital, in Addis Ababa, and at University of Gondar, northwestern Ethiopia, in which it accounted for 59.4% and 53.8%, respectively.15,21 On the contrary, indications like work up for upper GI bleeding (17.1%), variceal screening (16.8%), and follow-up endoscopy (13.7%), of which 89.2% had varices, were higher in the current study. This may be due to the fact that SPHMMC, being a center with gastroenterology and hepatology fellowship training program, accepts more patients with liver diseases who have complications and require repeated endoscopic evaluations. In addition, it has been proposed that the use of variable terminology for symptoms in different settings could result in differences in indications.25
The pathology most frequently identified with esophageal endoscopy in the current study was esophageal varices (35.8%); which is much higher than similar Ethiopian studies from Addis Ababa (9%), Gondar (2.9%) and Mekelle (12.7%);15,16,21 and studies from other African countries.26–28 Esophageal varices were found to be more prevalent among males than females, which is in agreement with a study from Gizan, Saudi Arabia.25 This study also found that esophageal varices were the predominant lesions in patients with upper GI bleeding (51.8%). These findings can be explained by the better availability of human and material resources in SPHMMC for the treatment of esophageal varices, such as endoscopic band ligation, compared with the rest of the country, which attracts more referrals of patients with such pathologies.
In the present study, gastritis was the most common pathologic finding (18%) in endoscopy of stomach, which is less than studies from southwestern Uganda (40.2%),27 Kashmir India (23.3%);29 this can be explained by differences in communities related to diet and prevalence of risk factors like H. pylori infection. A lower percentage (6%) was reported in a study carried out more than two decades ago in a similar setting at the Tikur Anbessa Teaching Hospital, Addis Ababa, Ethiopia,15 showing that there is a possible progressive increase in gastritis prevalence among the Ethiopian population, which requires in-depth investigation.
Duodenal ulcer was the predominant pathological lesion identified (10.6%) in this study on duodenal endoscopy, much lower than similar reports from teaching hospitals in Gondar (25.4%) and Addis Ababa (41%) Ethiopia,15,21 and a Nigerian study (30.6%);30 but in agreement with studies conducted in Eldoret, Kenya (11%), and Gizan, Saudi Arabia (9%).25,31 The prevalence of duodenitis (4.8%), the second most common pathology on duodenal endoscopy in this study, was slightly higher compared to other studies.15,29 This difference could be explained by the differences in the populations studied and the underlying risk factors, such as H. Pylori infection, use of substances such as alcohol and smoking.
With regard to upper gastrointestinal malignancies, in this study, esophageal tumor was slightly predominant than gastric tumor (4.4% vs 4.1%), similar to a study in Gondar, Ethiopia, with comparable prevalence (4.3% vs 3.6%).21 A higher proportion of gastric tumor (5%) than of esophageal tumor (5% vs 1.3%) was found in an Indian study.32 A study in Ghana reported a lower prevalence of gastric tumor (2.1%).33 These differences observed with studies from other countries could be from population’s difference in lifestyle, dietary factors and genetics. Consistent with a local study in Gondar, Ethiopians living in different parts of the country have comparable findings.21
This study has found that most common upper GI pathologies affected men (65.1%) compared to females, which is consistent with studies from Gondar, Ethiopia, Lagos, Nigeria, Jammu, Gadag, and Gizan, India.21,25,29,34,35 Atrophic gastritis has shown slight female predominance, with male-to-female ratio of 1:1.3, similar to a study in northwestern Ethiopia that found ratio of 1:1.2.21 Regarding the age of the participants, in the current study, upper gastrointestinal diseases were commonly seen in patients aged 21–30 years, accounting for 32.8% of pathologic findings on endoscopy, reflecting diseases involving younger populations in our community. This is in contrast to studies conducted elsewhere that reported incidence of 59.7% among patients older than 40 years in southwestern Uganda and highest incidence in 41 to 50 years age group (24.9%) in India.27,28 Previous studies conducted among Ethiopians have also shown that positive endoscopic findings were seen more in the younger population, and the incidence of duodenal ulcer was approximately 10 years younger than in the Western world.21,36
The higher prevalence of common upper gastrointestinal pathologies among male patients and the predominance among the younger population cannot be explained by this study, and requires further in-depth investigation of the underlying risk factors.
This study retrospectively evaluated a large number of procedures performed over a long period of time. Therefore, this is a good representation of the study population. In addition, common indications and endoscopic findings were assessed, which helped to identify prevalent upper gastrointestinal pathologies among our patients and characterize them appropriately.
Certain limitations of this study should be considered when interpreting its results. Since secondary data were used, the demographic information of the patients was limited to age and sex. This was a single-center study. Exclusion of nearly 10% of the total records due to incompleteness and duplicate reports could have skewed the results. Finally, since this study was conducted in a tertiary hospital where severe forms of illnesses are treated, it may have overestimated some results and may not reflect the exact prevalence of upper gastrointestinal pathologies in the community.
Conclusions
In conclusion, dyspepsia was the most common indication for upper gastrointestinal endoscopy followed by upper GI bleeding. Esophageal varices, GERD and gastritis were the most common abnormal findings. The incidence of benign lesions is higher than that of malignancies. EGD remains a vital tool for the diagnosis and proper characterization of pathologies involving the upper gastrointestinal tract and should be readily available to assist healthcare professionals in the treatment of patients with upper gastrointestinal diseases. Focus must be given to the availability of resources needed for the timely treatment of patients with common pathologies such as varices. Future studies that consider our limitations should be done.
Abbreviations
CLD, Chronic Liver Disease; EGD, Esophagogastroduodenoscopy; GERD, Gastro-Esophageal Reflux Disease; GI, Gastrointestinal; GOO, Gastric Outlet Obstruction; GOV, Gastro-Oesophageal Varices; IGV, Isolated Gastric Varices; LA, Los-Angeles; PHG, Portal Hypertensive Gastropathy; SPHMMC, St. Paul’s Hospital Millennium Medical College; SPSS, Statistical Package for the Social Sciences; UGIE, Upper Gastrointestinal Endoscopy.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was conducted following Helsinki Declaration. Ethical clearance was obtained from the Institutional Review Board of St. Paul’s Hospital Millennium Medical College (approval number: P.M. 23/738). We reviewed the patient records from the endoscopy unit of the institution. As part of the preprocedural requirement of the unit, each patient who was referred for upper GI endoscopy signed a consent form for the procedure, which also states that the study information/findings can be used by the institution for academic and research purposes. For underaged patients, informed consent was obtained from legally authorized representatives. Therefore, individual patient informed consent for this study was not applicable, and a waiver of informed consent was obtained from the institutional review board of St. Paul’s Hospital Millennium Medical College.
The confidentiality of information collected from patient records was protected by making the data collection coded. Specific identifying information, such as patient name or chart number, was not included in this study, and all information was treated with utmost confidentiality.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by a grant from St. Paul’s Hospital Millennium Medical College.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Salvi S, Apte K, Madas S, et al. Symptoms and medical conditions in 204 912 patients visiting primary health-care practitioners in India: a 1-day point prevalence study (the POSEIDON study). Lancet Glob Heal. 2015;3(12):e776–84. doi:10.1016/S2214-109X(15)00152-7
2. Etyang AO, Munge K, Bunyasi EW, et al. Burden of disease in adults admitted to hospital in a rural region of coastal Kenya: an analysis of data from linked clinical and demographic surveillance systems. Lancet Glob Health. 2014;2(4):e216–e224. doi:10.1016/S2214-109X(14)70023-3
3. Ford AC, Forman D, Bailey AG, Axon ATR, Moayyedi P. Initial poor quality of life and new onset of dyspepsia: results from a longitudinal 10-year follow-up study. Gut. 2007;56:321–327. doi:10.1136/gut.2006.099846
4. Van Zanten SV, Wahlqvist P, Talley NJ, et al. Alimentary Pharmacology and Therapeutics Randomised clinical trial: the burden of illness of uninvestigated dyspepsia before and after treatment with esomeprazole – results from the STARS II study. Aliment Pharmacol Ther. 2011;34(August):714–723. doi:10.1111/j.1365-2036.2011.04789.x
5. Lacy BE, Weiser KT, Kennedy AT, Crowell MD, Talley NJ. Functional dyspepsia: the economic impact to patients. Aliment Pharmacol Ther. 2013;38(2):170–177. doi:10.1111/apt.12355
6. Mahadeva S, Goh KL. Epidemiology of functional dyspepsia: a global perspective. World J Gastroenterol. 2006;12(17):2661–2666. doi:10.3748/wjg.v12.i17.2661
7. Marwaha A, Ford AC, Lim A, Moayyedi P. S1069 the worldwide prevalence of dyspepsia: systematic review and meta-analysis. Gastroenterology. 2009;136(5):A–182.
8. Kasper DL, Fauci AS, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison’s Principles of Internal Medicine. Mcgraw-hill; 2018.
9. Melese A, Genet C, Zeleke B, Andualem T. Helicobacter pylori infections in Ethiopia; Prevalence and associated factors: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19(1):1–15. doi:10.1186/s12876-018-0927-3
10. Suerbaum S, Michetti P. Helicobacter pylori infection. N Engl J Med. 2002;347(15):1175–1186. doi:10.1056/NEJMra020542
11. Negash M, Baynes HW, Geremew D. Helicobacter pylori infection and its risk factors: a prospective cross-sectional study in resource-limited settings of Northwest Ethiopia. Can J Infect Dis Med Microbiol. 2018;2018. doi:10.1155/2018/9463710
12. Yamada T, Alpers DH, Kalloo AN, Kaplowits N, Owyang CP. Yamada’s Textbook of Gastroenterology.
13. Cohen J, Greenwald DA. Overview of upper gastrointestinal endoscopy; 2018. Available from: https://www.uptodate.com/contents/overview-of-upper-gastrointestinal-endoscopy-esophagogastroduodenoscopy?search=upper%20gi%20endoscopy&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1.
14. Moayyedi PM, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N. ACG and CAG clinical guideline: management of dyspepsia. Am J Gastroenterol. 2017;112(7):988–1013. doi:10.1038/ajg.2017.154
15. Taye M, Kassa E, Mengesha B, Gemechu T, Tsega E. Upper gastrointestinal endoscopy: a review of 10,000 cases. Ethiop Med J. 2004;42(2):97–107.
16. Kebede Y, Tsegay B, Abreha H. Endoscopic and histopathological correlation of gastrointestinal diseases in ayder referral hospital, Mekelle University, Northern Ethiopia. Ethiop Med J. 2017;55(4):285–291.
17. Henriksen T-H, Nysaeter G, Madebo T, et al. Peptic ulcer disease in south Ethiopia is strongly associated with Helicobacter pylori. Trans R Soc Trop Med Hyg. 1999;93(2):171–173. doi:10.1016/S0035-9203(99)90297-3
18. Seid A, Tamir Z, Demsiss W, Gianotti R, Marzano AV. Uninvestigated dyspepsia and associated factors of patients with gastrointestinal disorders in Dessie referral hospital, Northeast Ethiopia. BMC Gastroenterol. 2018;18:1–10. doi:10.1186/s12876-017-0727-1
19. Ayele B, Molla E. Dyspepsia and associated risk factors at yirga cheffe primary hospital, clinical microbiology: open access. Clin Microbiol. 2017;6(3). doi:10.4172/2327-5073.1000282
20. Bulcha GG, Leon ME, Gwen M, et al. Epidemiology of esophageal cancer (EC) in Oromia region, Ethiopia 2016: a 4-year medical record review. J Glob Oncol. 2018;4(Supplement 2):14s. doi:10.1200/jgo.18.41700
21. Woreta SA, Yassin MO, Teklie SY, Getahun GM, Abubeker ZA. Upper gastrointestinal endoscopy findings at Gondar. Int J Pharm H Care Res. 2015;03(02):60–65.
22. Tsega E, Gebre W, Manley P, Asfaw T. Helicobacter pylori, gastritis and non-ulcer dyspepsia in Ethiopian patients. Ethiop Med J. 1996;34(2):65–71.
23. Global REACH. Doctors help establish GI fellowship in Ethiopia’s St. Paul Hospital; 2019 Available from: http://globalreach.med.umich.edu/articles/doctors-help-establish-ethiopia’s-first-ever-gifellowship.
24. About – Saint Paul’s millennium medical college; 2019. Available from: https://sphmmc.edu.et/about/.
25. Ageely H. Indications and findings of upper gastrointestinal endoscopy (UGIE) in Patients of Gizan - Saudi Arabia: a Retrospective Study. World Fam Med J. 2015;13(8):4–10. doi:10.5742/MEWFM.2015.92745
26. Koura M, Zongo Napon DP, Ouattara ZD, et al. Upper gastrointestinal endoscopy at University Hospital Souro Sanou Bobo-Dioulasso (Burkina Faso), about 1022 cases: signs and lesions observed. Open J Gastroenterol. 2017;07(11):287–296. doi:10.4236/ojgas.2017.711030
27. Obayo S, Muzoora C, Ocama P, Cooney MM, Wilson T, Probert CS. Upper gastrointestinal diseases in patients for endoscopy in South-Western Uganda. Afr Health Sci. 2015;15(3):959–966. doi:10.4314/ahs.v15i3.33
28. Okello T, Ogwang D, Alema N, Pecorella I. An evaluation of 605 endoscopic examination in a rural setting, lacor hospital in northern Uganda. Br J Med Res. 2016;15(10):1–7. doi:10.9734/BJMMR/2016/24412
29. Singh Chandail V, Sambyal V, Jamwal V. Role of Endoscopy in Evaluating Upper Gastrointestinal Tract Lesions at a Tertiary Care Hospital. Int J Adv Res. 2019;7(4):112–117. doi:10.21474/IJAR01/8798
30. Alatise OI, Aderibigbe AS, Adisa AO, Adekanle O, Agbakwuru AE, Arigbabu AO. Management of overt upper gastrointestinal bleeding in a low resource setting: a real world report from Nigeria. BMC Gastroenterol. 2014;14(1):1–9. doi:10.1186/s12876-014-0210-1
31. Ayuo PO, Some FF, Kiplagat J. Upper gastrointestinal endoscopy findings in patients referred with upper gastrointestinal symptoms in Eldoret, Kenya: a retrospective review. East Afr Med j. 2014;91(8):267–273.
32. Rajendran K, Chidambaranathan S, Sathyanesan J, Palaniappan R. Spectrum of upper gastrointestinal endoscopy findings in patients with dyspepsia and its relation to alarm symptoms. Int J Med Heal Res. 2018;4(10):175–177.
33. Gyedu A, Yorke J. Upper gastrointestinal endoscopy in the patient population of Kumasi, Ghana: indications and findings. Pan Afr Med J. 2014;8688:1–7.
34. Ainapure R, Tanga V. A clinico-endoscopic study of upper GI disorders in rural population. Int Surg J. 2018;5(3):1111. doi:10.18203/2349-2902.isj20180840
35. Jeje E, Lajide T, Akande B. Upper gastrointestinal endoscopy - Our findings, our experience in Lagoon hospital, Lagos, Nigeria. Maced J Med Sci. 2013;6(2):168–173.
36. Tsega E, Mengistu M. Peptic diseases in Ethiopia: a prospective analysis of 200 endoscopically proven cases. Trop Geogr Med. 1985;37(2):150–155.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
