Back to Journals » Therapeutics and Clinical Risk Management » Volume 13
Increased risk of endotracheal intubation and heart failure following acute myocardial infarction in patients with urolithiasis: a nationwide population-based study
Authors Lin SK , Liu JM , Chang YH, Ting YT, Pang ST, Hsu RJ , Lin PH
Received 2 October 2016
Accepted for publication 27 January 2017
Published 23 February 2017 Volume 2017:13 Pages 245—253
DOI https://doi.org/10.2147/TCRM.S123702
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Shun-Ku Lin,1,2,* Jui-Ming Liu,3,* Ying-Hsu Chang,4 Yuan-Tien Ting,5 See-Tong Pang,4 Ren-Jun Hsu,6–8 Po-Hung Lin4,9
1Institute of Traditional Medicine, School of Medicine, National Yang-Ming University, 2Department of Chinese Medicine, Taipei City Hospital, Ren-Ai Branch, Taipei, 3Division of Urology, Department of Surgery, Taoyuan General Hospital, Ministry of Health and Welfare, 4Division of Urology, Department of Surgery, Chang Gung Memorial Hospital at Linkou, Taoyuan, 5Division of Urology, Department of Surgery, Chang Bing Show Chwan Memorial Hospital, Changhua, 6Biobank Management Center of the Tri-Service General Hospital, 7Department of Pathology and Graduate Institute of Pathology and Parasitology, the Tri-Service General Hospital, 8Graduate Institute of Life Sciences, National Defense Medical Center, Taipei, 9Graduate Institute of Clinical Medical Science, College of Medicine, Chang Gung University, Taoyuan, Taiwan, Republic of China
*These authors contributed equally to this work
Background: Urolithiasis is a common urinary tract disease worldwide. It has been connected to systemic diseases, including hypertension, diabetes mellitus, metabolic syndrome, and cardiovascular disease. In the current study, we aimed to evaluate the relationship between urolithiasis and the complications of acute myocardial infarction (AMI).
Materials and methods: Data were obtained from the Longitudinal Health Insurance Database 2005 of the National Health Insurance Research Database. All AMI cases, both those who were hospitalized and those who were treated in the emergency department, were identified using the International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) code.
Results: A total of 37,052 patients with urinary calculi and 148,209 control subjects were enrolled in this study. The average follow-up period was 9.51 years. The risk of AMI was higher among patients with urolithiasis (adjusted hazard ratio [aHR] 1.07, 95% confidence interval [95% CI] 1.03–1.13). We detected a significant association between urolithiasis and intubation (aHR 1.53, 95% CI 1.36–1.73), intensive care unit treatment (aHR 1.22, 95% CI 1.13–1.32), heart failure (aHR 1.59, 95% CI 1.42–1.78), shock (aHR 1.53, 95% CI 1.32–1.77), and arrhythmias (aHR 1.18, 95% CI 1.06–1.33). Furthermore, certain medical treatments for urolithiasis were found to be related to myocardial infarction (MI). Nonsteroidal anti-inflammatory drugs (NSAIDs) were significantly associated with a high risk of AMI. In contrast, allopurinol, thiazide diuretic, potassium-sparing diuretics, and a-blockers have negative association with AMI.
Conclusion: Urolithiasis had a significantly increased risk of endotracheal intubation and heart failure following AMI. In addition, urolithiasis was also associated with a high risk of intensive care unit treatment, shock, and arrhythmias after AMI. Medical treatments for urolithiasis may decrease the risk of MI, except the use of NSAIDs.
Keywords: urolithiasis, renal calculi, acute myocardial infarction, National Health Insurance Research Database, endotracheal intubation, heart failure
Introduction
Urolithiasis is a common urinary tract disease worldwide. The prevalence of nephrolithiasis, which has been found to be 8.8% (10.6% in men and 7.1% in women) in the United States and 9.6% (14.5% in men and 4.3% in women) in Taiwan, has increased in modern society.1–5 Urolithiasis may be marked by symptoms such as renal colic, hematuria, dysuria, and even deterioration of renal function. In several studies, urolithiasis has been connected to systemic diseases, including hypertension,6 diabetes mellitus,7 metabolic syndromes,8 and cardiovascular disease.9,10 Rule et al11 performed a longitudinal study which reported that patients with kidney stones had a 31% increased risk of myocardial infarction (MI). However, the relationship between urolithiasis and the complications of MI including endotracheal intubation or heart failure has not been discussed. In the current study, we used National Health Insurance Research Database (NHIRD) of Taiwan to perform a nationwide, population-based study with 10-year follow-up period to investigate the relationship between urolithiasis and the complications of MI.
Materials and methods
Data source and study design
In this population-based, retrospective cohort study, we analyzed 1 million samples randomly chosen from beneficiaries of Taiwan’s NHIRD between January 1, 1997, and December 31, 2012.
The database was obtained from the NHIRD’s Longitudinal Health Insurance Database 2005 (LHID2005). The NHIRD, which covers >97% of Taiwanese people, records all insurance information, including demographic data such as sex, date of birth, location, and insured amount and medical records of clinical visits, admissions, and medical procedures, as well as 3 major diagnoses coded according to the International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM).12,13 The LHID2005 contained the information of 1 million beneficiaries, randomly selected from all insured people entered in the NHIRD in 2005. There was no distribution difference in age, sex, or insured costs between the LHID2005 and origin population.14
Study population
The flowchart of data extraction is shown in Figure 1. We selected a national cohort consisting of 656,627 adults without ischemic heart disease (ICD-9-CM codes 410, 411, 412, 413, 414, or 440) from the LHID2005, of whom 86,368 participants (13.2%) had a diagnosis of urinary calculus (ICD-9-CM codes 592 and 594) before January 1, 2003. Patients without urinary calculi were matched with the study group at a ratio of 1:4 with regard to sex, age, insured region, urbanization, and comorbidities associated with MI (diabetes mellitus, hypertension, hyperlipidemia, chronic kidney disease, cerebral vascular accident, and atherosclerosis). The patient’s date of diagnosis of urolithiasis was assigned as the index date and considered the start of investigation. Participants were followed until sustaining an acute MI (AMI) or dying or the submission of the last medical claim before the end of 2012. All medical diagnoses, procedures, and drugs were recorded completely during the follow-up period.
Ethics statement
This study was conducted after we received approval from the Institutional Review Board of Chang Gung Memorial Hospital at Linkou (CGMH IRB 103-3238B). As this was a retrospective study and all the data were anonymous, the Institutional Review Board department agreed with the authors that it was not necessary to obtain patient consent.
Study outcomes
The primary end point was AMI. All AMI cases, both those sustained during a hospitalization and those seen in the emergency department, were identified with ICD-9-CM code 410. Tracheal intubation, coronary artery bypass grafting (CABG), and cardiac catheterization treatment were recorded as secondary end points. Severe complications of AMI, including heart failure, cardiac arrhythmia, shock, and cardiac arrest, were also considered.
Variables
We systematically identified potential confounders for AMI, such as diabetes mellitus, hypertension, hyperlipidemia, chronic kidney disease, cerebrovascular accident, and atherosclerosis. The location of calculi (ie, kidney, ureter, urinary bladder, or unspecified) was also noted. Sociodemographic characteristics (eg, age, sex, amount of insurance, and level of urbanization) were also studied.
Age was classified into 6 groups: younger than 25 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years, and older than 65 years. Place of residence in Taiwan was divided into 7 regions: Taipei city, Kaohsiung city, northern region, middle region, eastern region, southern region, and outlying islands. Urbanization in Taiwan was divided into 4 categories.15 Insurance amount in New Taiwan Dollars (NT$) was categorized into 4 levels: dependent (no constant income), NT$1 to NT$19,999, NT$20,000 to NT$39,999, and NT$40,000 or more. Medications used for treating urolithiasis according to clinical guidelines (eg, smooth muscle relaxants such as scopolamine butylbromide and pipoxolan hydrochloride), urine-alkalinizing agents (eg, potassium citrate), uric-acid-reducing agents (allopurinol, benzbromarone), nonsteroidal anti-inflammatory drugs (NSAIDs; eg, diclofenac, ibuprofen, mefenamic acid, indomethacin, sulindac), and α-adrenergic blockers (eg, tamsulosin, terazosin, alfuzosin, doxazosin) were also analyzed in an effort to assess possible effects.
Statistical analyses
To guarantee the effect of the matching, we compared the distribution of demographic factors and the proportions of comorbidities between the urinary calculi and non-urinary calculi cohorts with the use of the chi-square test. Case number and incidence density of AMI were calculated during the follow-up period, and we performed Cox proportional regression models to analyze hazard ratios accompanying 95% confidence intervals (CIs). The adjusted variables included age, sex, insurance amount, urbanization level, comorbidities (diabetes mellitus, hypertension, hyperlipidemia, chronic kidney disease, cerebral vascular accident, atherosclerosis, gout, hyperparathyroidism), and medications for urolithiasis (urine alkalizer, antigout preparations, stone expulsion, symptom relief, diuretics). A significance level (α) of 0.05 was selected. We also used Kaplan–Meier survival curves and log-rank analyses to analyze the difference between patients with urolithiasis and control groups. The statistical software package SAS, version 9.4 (SAS Institute, Cary, NC, USA), was used for data analysis.
Results
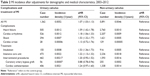
The database contained 86,368 patients with urinary calculi without MI between 1997 and 2002. After we performed matching at a ratio of 1:4, 185,261 patients were enrolled in this study, including 37,052 patients with urinary calculi and 148,209 control subjects. The characteristics of the sampled patients are listed in Table 1. Patients with urinary calculi were mostly men, middle aged, and residents of northern Taiwan. Diabetes mellitus, hypertension, and hyperlipidemia were the 3 most common comorbidities in the patients with urinary calculi. After the matching process, chi-square testing showed no significant difference between the urinary calculi and control groups. The average follow-up period was 9.51 years (standard deviation [SD] =2.58 years).
  | Table 1 Demographic characteristics and comorbidities of the matched cohort |
During the follow-up period, the adjusted risk of AMI was higher among patients with urinary calculi (adjusted hazard ratio [aHR] 1.07, 95% CI 1.03–1.13). The total number of patients with urinary calculi and AMI was 1,362 in our cohort study. The aHR of AMI statistically increased in older age group. We detected significant associations between urinary calculi and intubation (aHR 1.53, 95% CI 1.36–1.73) and intensive care unit (ICU) treatment (aHR 1.22, 95% CI 1.13–1.32), which are listed in Table 2. The adjusted risk of severe AMI complications, including heart failure (aHR 1.59, 95% CI 1.42–1.78), shock (aHR, 1.53; 95% CI 1.32–1.77), and arrhythmias (aHR, 1.18; 95% CI 1.06–1.33) was significantly higher among patients with urinary calculi. Kaplan–Meier survival curves and log-rank analyses revealed significant differences in the rates of MI between patients with urolithiasis and control groups, which shown in Figure 2 (log-rank test, P=0.016).
Diabetes mellitus, hypertension, hyperlipidemia, chronic kidney disease, cerebrovascular accident, atherosclerosis, gout, and hyperparathyroidism were all found to be associated with AMI (Table 3).
Various medical treatments for urolithiasis were found to be related to MI. In Table 4, we show that NSAIDS, including sulindac (aHR 1.54, 95% CI 1.06–2.21), ibuprofen (aHR 1.55, 95% CI 1.25–1.90), and mefenamic (aHR 1.22, 95% CI 1.01–1.45), were significantly associated with MI (Table 4). Allopurinol, an antigout medication, had a negative association with MI (aHR, 0.72; 95% CI 0.53–0.88), and so did colchicine preparations (aHR, 0.89; 95% CI 0.81–0.96). In view of diuretics, thiazide diuretic (aHR, 0.91; 95% CI 0.86–0.97) and potassium-sparing diuretics (aHR, 0.85; 95% CI 0.79–0.91) might decrease the incidence of MI; α-blocker preparations also showed the same trend (aHR 0.85, 95% CI 0.79–0.93).
  | Table 4 MI incidence associated with different medication treatments of urolithiasis, 2003–2012 |
Discussion
The complications of MI can be assessed based on clinical course, treatment, and complications. For a patient who has sustained a minor AMI, bed rest and medical treatment with antiplatelet drugs may be useful. However, in severe AMI, cardiogenic shock may be encountered and intubation and ICU care may be necessary. Interventions such as cardiac catheterization or CABG may be arranged thereafter. Depending on the severity of AMI, multiple complications may be encountered, including arrhythmias, heart failure, and even cardiac arrest.
In this population-based study, we analyzed 1 million samples, randomly selected from 22 million people in the Taiwanese NHIRD. Our study is the first population-based cohort study to reveal an increased risk of severe AMI, requiring ICU treatment or resulting in severe complications, in patients with urinary calculi during a 10-year follow-up period.
Several studies have revealed an increased risk of AMI in people with urinary calculi.10,11,16–18 Rule et al11 conducted a study of 4,564 patients with renal stones over 9 years of follow-up. Patients with renal stones had a risk of AMI 38% greater than that of those without stones. However, the relationship between urolithiasis and the complications of AMI was not investigated. Ferraro et al16 published 3 cohort studies of 19,678 patients with renal stones with 18 years of follow-up. Between 2 cohorts, female kidney stone formers had an 18% and a 48% increased risk of coronary heart disease, but this was not seen in male patients. Alexander et al19 conducted a cohort study of 25,532 kidney stone formers with 11 years of follow-up. They found that kidney stone formers were more likely to experience cardiovascular events, with a higher risk of AMI (aHR 1.40, 95% CI 1.30–1.51) and percutaneous transluminal coronary angioplasty (PTCA)/CABG (aHR 1.63, 95% CI, 1.51–1.76), especially in younger people versus older people and in women versus men.
We noted an increased risk of AMI in urinary calculi formers, both male and female, in our study (aHR 1.07, 95% CI 1.03–1.13). AMIs in patients with urinary calculi tend to be more severe, involving a higher chance of intubation and ICU care. Moreover, urinary calculi were linked to severe AMI complications, including heart failure (aHR 1.59, 95% CI, 1.42–1.78), shock (aHR 1.53, 95% CI 1.32–1.77), and arrhythmias (aHR 1.18, 95% CI 1.06–1.33). In light of these data, we conclude that urinary calculi could be a risk factor for severe AMI, and this study is the first to provide evidence of this association. According to the results of this study, we concluded that patients with urolithiasis should be evaluated for the risk of AMI during the follow-up for stone disease, and if AMI is encountered, more intensive and aggressive treatments should be given.
There are several theories to explain the relationship between urolithiasis and MI. Urinary calculi may cause renal function impairment, which is a well-known major risk factor in coronary artery disease and could increase the likelihood of cardiovascular complications after AMI.20 The association between kidney stones and metabolic syndrome has been established in previous studies, and metabolic syndrome is also a risk factor for AMI.21 Patients with kidney stones have an increased risk of hypertension,22,23 diabetes mellitus,7,24 and subclinical atherosclerosis, all risk factors for AMI.25
Proinflammation status, which was recently evaluated as a high neutrophil to lymphocyte count ratio (NLCR), was considered to be associated with many chronic diseases. Sen et al26 conducted a retrospective study and revealed that NLCR >2.50 was associated with a higher risk of sepsis after stone surgery. Acet et al27 evaluated the relationship of NLCR with the severity of MI and found that higher NLCR was associated with higher thrombolysis in MI (TIMI) score. These findings may explain the possible mechanism of higher risk of MI among patients with urinary calculi.
NSAIDs are commonly used to relieve pain in patients with urinary calculi, but they have been found to increase the risk of AMI.28–30 In our study, NSAID use in urinary calculi formers was also linked to an increased risk of AMI. We also found that allopurinol treatment for gout was associated with a decreased risk of AMI. This finding is similar to a recent study conducted by de Abajo et al,31 which revealed that allopurinol is associated with a reduced risk of nonfatal AMI. Similar trends were also seen in the use of thiazide diuretic, potassium-sparing diuretics, and α-blocker preparations. These findings may imply that early treatment for urolithiasis may decrease the risk of MI. However, NSAIDs should be used carefully. Since the use of these medications may increase the risk of MI, we also evaluated the risk of MI for patients with or without calculi adjusted for the medications. The results showed that after adjusting for medication use, patients with urinary calculi still had a higher risk of MI (Table S1).
Since surgical procedure itself is a risk factor for MI, we analyzed the impact of surgical managements for urolithiasis, to MI. In our study, patients who had suffered an MI within 14 days after surgical management of urolithiasis accounted for only 1.32% of all patients. On the contrary, 89.10% of patients had suffered from MI >1 year after surgical management of urolithiasis. The aHR was 1.08 with 95% CI of 0.72–1.31, which was not statistically significant. The data are shown in Table S2. Thus, there was no time relationship between surgical procedures and MI.
Calcium metabolism may be another mechanism of increased risk of AMI in patients with urinary calculi. Formation of calcium precipitations in the urinary tract may be a result of a high calcium concentration. A high calcium concentration may induce the activation of calcification inhibitor and increase the risk of both kidney stones and AMI.32 Vitamin D is important in the metabolism of calcium. Some studies showed that a low level of vitamin D was found in around 54%–80% of stone formers.33,34 Recently, vitamin D was proved to play an important role in the regulation of the mechanism in coronary collateral circulation development.35 A lower level of vitamin D may lead to less collateral circulation of the coronary artery, hence increases the risk of MI.
The most typical symptom of urinary calculi is pain, which includes renal colic, flank pain, and back pain. Pain is also a symptom of AMI. AMI-related pain is located in the chest, back, jaw, and other parts of the upper body. Urinary calculi formers could misidentify back pain as stone pain and ignore what is actually a sign of AMI. The pain associated with urinary calculi and that of AMI can be very similar and may lead to delays in the diagnosis and treatment of AMI.
Our NHIRD study was subject to some limitations. First, the size and composition of urinary calculi and laboratory findings such as creatinine and blood urea nitrogen concentrations were not available in the NHIRD database. Therefore, we could not see the influence of renal function (glomerular filtration rate), stone composition, and stone burden on AMI. Second, electrocardiography data were not available in the NHIRD database, so we could not use the TIMI risk score to evaluate AMI severity. Third, different practices of each physician with regard to the treatment of AMI and urinary calculi could not be seen in the NHIRD database. Although there are medical guidelines, every physician’s method of management was different. This could have influenced the outcomes of AMI and urinary calculi. Fourth, the NHIRD did not include patient’s weight or body mass index (BMI), but obesity is one of the known risk factors for MI. This could have influenced the outcomes of AMI and urinary calculi. Finally, this is a retrospective study rather than a prospective randomized study. Further prospective studies are necessary to determine the link between urinary calculi and AMI.
Conclusion
This population-based study is the first study to show that patients with urolithiasis have an increased risk of endotracheal intubation and heart failure following AMI. This study also showed an increased risk of severe AMI complications, including ICU treatment, shock, and arrhythmias among patients with urolithiasis. These results may be valuable in both medical care and public health.
Acknowledgments
We would like to express our appreciation for the support provided by the National Health Insurance Administration; the Ministry of Health and Welfare, Executive Yuan, Taiwan; and the Taipei City Hospital. The work was supported by grants from the Ministry of Health and Welfare (10510).
Author contributions
S-KL wrote the manuscript and performed data analysis. J-ML wrote the proposal and designed the manuscript. R-JH and Y-TT contributed to the conception of the study. P-HL revised the manuscript. All the authors contributed toward data analysis, drafting and critically revising the article, read and approved the final manuscript, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Scales CD Jr, Smith AC, Hanley JM, Saigal CS; Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(3):160–165. | ||
Lee YH, Huang WC, Tsai JY, et al. Epidemiological studies on the prevalence of upper urinary calculi in Taiwan. Urol Int. 2002;68(3):172–177. | ||
Hesse A, Brändle E, Wilbert D, Köhrmann KU, Alken P. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol. 2003;44(6):709–713. | ||
Huang WY, Chen YF, Carter S, Chang HC, Lan CF, Huang KH. Epidemiology of upper urinary tract stone disease in a Taiwanese population: a nationwide, population based study. J Urol. 2013;189(6):2158–2163. | ||
Lin PH, Lin SK, Hsu RJ, Cheng KC, Liu JM. The use and the prescription pattern of traditional Chinese medicine among urolithiasis patients in Taiwan: a population-based study. J Altern Complement Med. 2016;22(1):88–95. | ||
Madore F, Stampfer MJ, Willett WC, Speizer FE, Curhan GC. Nephrolithiasis and risk of hypertension in women. Am J Kidney Dis. 1998;32(5):802–807. | ||
Chung SD, Chen YK, Lin HC. Increased risk of diabetes in patients with urinary calculi: a 5-year follow-up study. J Urol. 2011;186(5):1888–1893. | ||
West B, Luke A, Durazo-Arvizu RA, Cao G, Shoham D, Kramer H. Metabolic syndrome and self-reported history of kidney stones: the National Health and Nutrition Examination Survey (NHANES III) 1988–1994. Am J Kidney Dis. 2008;51(5):741–747. | ||
Domingos F, Serra A. Nephrolithiasis is associated with an increased prevalence of cardiovascular disease. Nephrol Dial Transplant. 2011;26(3):864–868. | ||
Elmfeldt D, Vedin A, Wilhelmsson C, Tibblin G, Wilhelmsen L. Morbidity in representative male survivors of myocardial infarction compared to representative population samples. J Chronic Dis. 1976;29(4):221–231. | ||
Rule AD, Roger VL, Melton LJ 3rd, et al. Kidney stones associate with increased risk for myocardial infarction. J Am Soc Nephrol. 2010;21(10):1641–1644. | ||
Lee YC, Huang YT, Tsai YW, et al. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res. 2010;10:225. | ||
World Health Organization. International Classification of Diseases, Ninth Revision (ICD-9). Geneva, Switzerland: World Health Organization; 1977. | ||
National Health Research Institutes [webpage on the Internet]. National Health Insurance Research Database. Available from: http://nhird.nhri.org.tw/en/Data_Subsets.html#. Accessed September 1, 2016. | ||
Liu CY, Hung YT, Chuang YL, et al. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manage. 2006;4:1–22. | ||
Ferraro PM, Taylor EN, Eisner BH. History of kidney stones and the risk of coronary heart disease. JAMA. 2013;310(4):408–415. | ||
Hamano S, Nakatsu H, Suzuki N, Tomioka S, Tanaka M, Murakami S. Kidney stone disease and risk factors for coronary heart disease. Int J Urol. 2005;12(10):859–863. | ||
Zimmerer T, Weiss C, Hammes HP, et al. Evaluation of urolithiasis; a link between stone formation and diabetes mellitus? Urol Int. 2009;82(3):350–355. | ||
Alexander RT, Hemmelgarn BR, Wiebe N, et al. Kidney stones and cardiovascular events: a cohort study. Clin J Am Soc Nephrol. 2014;9(3):506–512. | ||
Anavekar NS, McMurray JJ, Velazquez EJ, et al. Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med. 2004;351(13):1285–1295. | ||
Sakhaee K. Nephrolithiasis as a systemic disorder. Curr Opin Nephrol Hypertens. 2008;17(3):304–309. | ||
Borghi L, Meschi T, Guerra A, et al. Essential arterial hypertension and stone disease. Kidney Int. 1999;55(6):2397–2406. | ||
Cappuccio FP, Strazzullo P, Mancini M. Kidney stones and hypertension: population based study of an independent clinical association. BMJ. 1990;300(6734):1234–1236. | ||
Taylor EN, Stampfer MJ, Curhan GC. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 2005;68(3):1230–1235. | ||
Reiner AP, Kahn A, Eisner BH, et al. Kidney stones and subclinical atherosclerosis in young adults: the CARDIA study. J Urol. 2011;185(3):920–925. | ||
Sen V, Bozkurt IH, Aydogdu O, et al. Significance of preoperative neutrophil-lymphocyte count ratio on predicting postoperative sepsis after percutaneous nephrolithotomy. Kaohsiung J Med Sci. 2016;32(10):507–513. | ||
Acet H, Ertaş F, Bilik MZ, et al. The relationship between neutrophil to lymphocyte ratio, platelet to lymphocyte ratio and thrombolysis in myocardial infarction risk score in patients with ST elevation acute myocardial infarction before primary coronary intervention. Postepy Kardiol Interwencyjnej. 2015;11(2):126–135. | ||
Graham DJ, Campen D, Hui R. Risk of acute myocardial infarction and sudden cardiac death in patients treated with cyclo-oxygenase 2 selective and non-selective non-steroidal anti-inflammatory drugs: nested case-control study. Lancet. 2005;365(9458):475–481. | ||
Johnsen SP, Larsson H, Tarone RE, et al. Risk of hospitalization for myocardial infarction among users of rofecoxib, celecoxib, and other NSAIDs: a population-based case-control study. Arch Intern Med. 2005;165(9):978–984. | ||
Coxib and Traditional NSAID Trialists’ (CNT) Collaboration, Bhala N, Emberson J, et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013;382(9894):769–779. | ||
De Abajo FJ, Gil MJ, Rodríguez A, et al. Allopurinol use and risk of non-fatal acute myocardial infarction. Heart. 2015;101(9):679–685. | ||
Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: randomized controlled trial. BMJ. 2008;336(7638):262–266. | ||
Elkoushy MA, Sabbagh R, Unikowsky B, Andonian S. Prevalence and metabolic abnormalities of vitamin D-inadequate patients presenting with urolithiasis to a tertiary stone clinic. Urology. 2012;79:781–785. | ||
Eisner BH, Thavaseelan S, Sheth S, et al. Relationship between serum vitamin D and 24-h urine calcium in patients with nephrolithiasis. Urology. 2012;80:1007–1010. | ||
Lima J Jr, Kunadian V. Vitamin D: evidence for an association with coronary collateral circulation development? Postepy Kardiol Interwencyjnej. 2015;3(41):174–176. |
Supplementary materials
  | Table S1 MI risk adjusted for medication use |
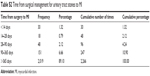  | Table S2 Time from surgical management for urinary tract stones to MI |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.