Back to Journals » International Journal of Women's Health » Volume 7
Increased cesarean section rate in Central Saudi Arabia: a change in practice or different maternal characteristics
Authors Al-Kadri H, Al-Anazi S, Tamim H
Received 21 March 2015
Accepted for publication 12 May 2015
Published 10 July 2015 Volume 2015:7 Pages 685—692
DOI https://doi.org/10.2147/IJWH.S85215
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Hanan M Al-Kadri,1 Sultana A Al-Anazi,1 Hani M Tamim2
1Department of Obstetrics and Gynecology, King Abdulaziz Medical City, 2College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Kingdom of Saudi Arabia
Background: Cesarean section (CS) rate has shown creepy increase. We aimed in this work to identify factors contributing to increasing rate of CS in central Saudi Arabia.
Methods: A retrospective cohort study was conducted at King Abdulaziz Medical City. Two groups of women were included (G1 and G2). G1 had delivered by CS during the year 2002 (CS rate 12%), and G2 had delivered by CS during the year 2009 (CS rate 20%). We compared the included women’s characteristics, neonates, CS indications, and complications. Data were analyzed using SPSS version 15 program. Odds ratios and confidence intervals were calculated to report precision of categorical data results. A P-value of ≤0.05 was considered significant.
Results: A total of 198 women were included in G1 and 200 in G2. Both groups had comparable maternal and fetal characteristics; however, absence of antenatal care has resulted in 70% increase in CS deliveries for G2, P=0.008, OR =0.30, CI 0.12–0.76. Previous vaginal surgeries have contributed to tenfold increase in CS deliveries for G2, P=0.006, OR =10.37, CI 1.32–81.78. G2 had eight times increased CS deliveries than G1 due to intrauterine growth restriction, P=0.02, OR =8.21, CI 1.02–66.25, and 80% increased risk of CS was based on maternal demand, P=0.02, OR =0.20, CI 0.02–1.71. Decision taken by less-experienced staff was associated with 2.5-fold increase in CS deliveries for G2, P=0.002, OR =2.62, CI 1.39–4.93. There was a significant increase in CS deliveries under regional analgesia and shorter duration of hospital stay for G2, P=0.0001 and P=0.001, respectively. G2 women had 2.75-fold increase in neonatal intensive care unit admission, P=0.03, OR =2.75, CI 1.06–7.15.
Conclusion: CS delivery rate significantly increased within the studied population. The increased rate of CS may be related to a change in physician’s practice rather than a change in maternal characteristics, and it appears to be reducible.
Keywords: cesarean section, maternal morbidity, neonatal morbidity, cesarean section rate
Introduction
Cesarean sections (CSs) are performed for various fetal and maternal indications; these include labor and delivery abnormalities, placental and cord abnormalities, and repeated CS deliveries.1 Recently, CS has been performed to satisfy women’s desire; therefore, cesarean delivery on maternal request (CDMR) was added to the known common CS indications.2
CS delivery is associated with increased maternal and fetal complications:3–5 higher rate of injuries of abdominal organs, infections, thromboembolic complications, placenta previa, placenta accreta, placenta increta, placenta percreta, and neonatal respiratory problems.6 These complications may result in serious consequences for both mother and baby.7 Even when a high-standard practice is implemented and most possible complications are successfully avoided, recovery after a CS delivery usually takes longer duration than that experienced after a normal vaginal delivery.8
In the last few decades, CS delivery rate has increased across the world. CS rate was noted to vary based on variations in countries, regions, financial status, and women preferences. The rate also varies based on the type of medical practice: a significant increase is observed when pregnant women are managed through private practice compared to governmental practice.9,10
CDMR and women and physician’s preferences are contributing to increasing rate of CS across the world.11 The common misbelief that vaginal delivery may traumatize the delivering women’s pelvic floor muscles resulting in stress urinary incontinence and postpartum pelvic organ descent was an important factor behind increased CDMR.12 Moreover, the significant increase in medicolegal litigations in obstetrics, the increased awareness of patients’ rights, and the increased obstetricians’ tendency to protective medical practice have resulted in more liberal CS decisions.13–15
A wide range of CS delivery rate was reported across the world. CS delivery rate between 20% and 22.5% was reported in the United Kingdom and Canada. Moreover, CS rate was as high as 85% of all birth in Italy and South America.13,16,17 Private practice has contributed to the increased CS rate internationally. For example, in Rome (Italy), the general rate of CS delivery was reported to be approximately 44%; however, this rate was as high as 85% of all birth in some private clinics of Rome.10
Ten years review of CS delivery in Saudi Arabia has shown 80% increase in CS delivery rate between the years 1997 and 2006.18 The published Saudi data did not explore several determinants that are known internationally to affect CS delivery rate.9,10,16,17 This incompleteness in the published review was particularly related to private sector data. Knowing that internationally increased CS rate has been reported to be significantly prominent in private sectors compared to governmental ones,9,10 further research investigating increase in CS rate in Saudi Arabia was recommended by the review authors.18
Over the last two decades, a gradual increase in CS delivery rate was observed at King Abdulaziz Medical City (KAMC), Riyadh, Saudi Arabia. In fact, CS delivery rate has crept up from 8% to 21% between the years 1993 and 2013. This gradual increase rate did not have clear justification factors. Considering KAMC as an example of a Saudi tertiary health care governmental institution localized in the central region of Saudi Arabia, our objective in this study was to identify factors contributing to CS increased rate in this region of the country.
Methods
A retrospective cohort study was conducted at KAMC in Riyadh, Saudi Arabia. KAMC is a tertiary referral health care center with a capacity of >1,000 beds. Attached to the tertiary center, there are multiple primary and secondary health care centers scattered across the central region of Saudi Arabia. These centers on top of providing primary medical care for patients function as referring centers for required patients from different central region areas to the tertiary center. The Department of Obstetrics and Gynecology at KAMC has approximately 100 beds for inpatients and approximately 20 beds for laboring women located in the labor and delivery suite (L&D). In L&D, there are two operating rooms (ORs) that are assigned to perform CS deliveries and other obstetrics operative interventions that require anesthesia. Daily obstetric clinics are running with a capacity of >300 antenatal women daily. During the study period, no active/organized antenatal education program was implemented.
Two groups of women, G1 and G2, were included in this research. The first group (G1) was arbitrarily sampled through KAMC medical records computer system. The sample was selected out of all women who had delivered by CS during the year 2002 and whose gestational age (GA) was ≥24 weeks. All types of CS deliveries were included, including elective and emergency CS deliveries. All women were Saudi national, and there was no restriction regarding the women’s age, parity, and CS indication. The second group (G2) was another similar arbitrarily sampled group out of those who had delivered during the year 2009. Similar inclusion and exclusion criteria were implemented for the selection of the participants of two groups. All included women were eligible to be treated at KAMC and were covered by full medical insurance. All included women’s computerized and paper-based records as well as their babies’ records were reviewed.
We collected data on the included women’s general characteristics, such as their age, parity, body mass index, and GA. CS type; being emergency or elective, CS delivery indications, presence or absence of provided antenatal care service or women’s booking status where those who experienced at least one visit at KAMC antenatal clinics were considered booked. Maternal medical diseases were assessed for G1 and G2. We assessed their diabetes status in being with type I, type II, or gestational diabetes mellitus (GDM), diabetes that is diagnosed for the first time during pregnancy. Hypertension disorders during pregnancy were also assessed: preeclampsia, eclampsia, and essential hypertension where the hypertension is preexisting before pregnancy. The presence of other medical history, such as sickle cell anemia, epilepsy, major depression, infections, and sepsis, was assessed. Data were collected on the pregnancy complications of women, abnormal placentation, antepartum hemorrhage (APH), postpartum hemorrhage (PPH), and other morbidities that were related directly or indirectly to CS delivery indication or performance.
Women’s surgical history was explored mainly on surgeries that can contribute to future vaginal delivery chances (particularly pelvic surgeries): anterior and posterior colpoperineorrhaphy, urinary incontinence surgeries, uterine cervix surgeries, and previous classical CS delivery. CS operative complications were collected; short-term postoperative complications were defined as any complication that has occurred within 24 hours of CS delivery, while long-term complications were defined as any complication that has occurred after 24 hours and within 6 weeks of the CS delivery. We have collected data also on the presence of abnormal fetal lie and/or presentations and multiple pregnancies, where more than one fetus is present in utero. The collected neonatal data have included newborn weight, Apgar score, cord pH, the place of neonate admission, and the length of hospital stay.
Data analysis
Collected data were entered into SPSS version 15 program. As descriptive analyses, we calculated the number and percentage for the categorical variables and mean and standard deviation (SD) for the continuous ones. The difference between G1 and G2 in relation to the different studied factors was calculated for both continuous and categorical variables by using either the χ2 test or Student’s t-test, as appropriate. Moreover, for categorical variables, the odds ratio (OR) and 95% confidence interval (CI) were calculated. The P-value of ≤0.05 was considered statistically significant.
The approval of King Abdullah International Medical Research Center was obtained prior to the conduction of the study through its retrospective research committee. As the study conduction did not interfere with patients’ management, no consent was obtained from the involved participants.
Results
The data were collected from 198 women representing G1, where the incidence of CS during the year 2002 was approximately 12%, and from another 200 women representing G2, where the incidence of CS during the year 2009 was approximately 20%.
Table 1 represents the data characteristics of the included women in G1 and G2 during the two study periods. There was no significant difference between G1 and G2 with respect to their age, body mass index, and GA. Antenatal care provided (booking) was significantly lower for G2, P=0.008. G1 women tended to have higher parity compared with G2 women, P=0.02. The distribution of the included women according to the different types of CS deliveries–primary, secondary, elective, or emergency CS–was similar between G1 and G2.
Although there was similarity in the past medical history of the two groups, their past pelvis surgery history was significantly different. G2 women’s past surgical history has increased their risk for CS delivery more than ten times, P=0.006. The most important contributing surgical history to the increased incidence of CS delivery in G2 was their previous history of anteroposterior colpoperineorrhaphy and urinary incontinence surgeries. On the other hand, there was no difference between G1 and G2 in their documented fetal condition in labor represented by the fetuses’ cardiotocography tracing abnormalities.
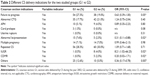
In Table 2, we have presented the different CS delivery indications for the two studied groups. Failure to progress was 37% lower for G2 compared with G1 women, and abnormal lie and presentations were 70% lower for G2 compared to G1 women, P=0.05 and P=0.02, respectively. CS deliveries performed due to intrauterine growth restriction (IUGR) were eight times higher for G2 women compared with G1 women, P=0.02. On the other hand, CS deliveries that were performed based on maternal demand were 80% higher for G2 women compared to G1 women, P=0.01.
In Table 3, upon assessing the level of experience of CS delivery decision taker, we noted 2.5-fold increase in CS decided by the intermediate level staff for G2 compared to G1, OR 2.62, CI 1.39–4.93, and P=0.002. These intermediate level staff were board-certified physicians but not the most responsible physicians. Within G2, there was a significant increase in CS delivery under spinal anesthesia, OR 13.17, CI 7.99–21.71, and P=0.0001, and epidural anesthesia, OR 10.15, CI 4.09–25.18, and P=0.0001. There was also a significant decrease in the length of hospital stay with P=0.001. On the other hand, there was no difference in intraoperative, immediate postoperative, and late postoperative maternal complications between G1 and G2.
Neonatal outcomes were similar between the two studied groups concerning their sex, weight, Apgar score, and cord pH. The only difference identified between G1 and G2 is 2.75 times increase in neonatal intensive care unit (NICU) admissions, OR 2.75, CI 1.06–7.15, and P=0.03, and approximately 70% decrease in intermediate care nursery (ICN) admissions for G2 neonates compared with G1 neonates, OR 0.32, CI 0.13–0.78, and P=0.009.
Discussion
At KAMC, CS delivery rate has increased from 8% in 1993 to ~21% of all deliveries in 2011. This significant increase is similar to what has been noted in many national and international studies. For example, Ba’aqeel18 has reported that over the period between 1997 and 2006, CS delivery rate rose from 10.6% to 19.1% in Saudi Arabia. A Chinese publication reported that CS delivery rate rose dramatically from 3.4% to 39.3% between the years 1988 and 2008.19 A similar rise in CS rate was observed in developed countries such as USA20 and Australia.21
Despite the significant increase in CS delivery rate in the studied institution, most of the studied maternal demographic data were similar in both groups. Obviously, CDMR has increased in 2009 women compared with 2002. Easy decision for CS delivery by both pregnant women and their obstetricians became more acceptable,2,22 even in societies where large families are preferred.23
Vaginal delivery is blamed to be an important factor contributing to women’s pelvic floor dysfunction. Pudendal nerve trauma and levator ani muscle defects that can occur during vaginal delivery may lead to this dysfunction. As a consequence, urinary incontinence, fecal incontinence, and pelvic organ prolapse happen.24 Therefore, it is sometimes difficult to convince women to go for vaginal delivery when we consider the possibility of pelvic floor dysfunction.24 In fact, pregnant women need to know that they may possibly develop short-term or even long-term pelvic floor defects, leading to some degree of pelvic organ prolapse and objective urinary incontinence. These symptomatic defects are likely to be significantly reduced after 6 months of delivery.25 However, symptoms may persist even after 5 years of vaginal delivery. In general, symptoms are likely to decrease as time increases from vaginal delivery.26 It is important to note that the prevalence of urinary incontinence symptoms in women who delivered vaginally is higher than those who delivered by CS even after 20 years from their delivery.27 The question that present itself: will these facts justify CS delivery for all women aiming to prevent the possible occurrence of pelvic floor dysfunction?
Research has shown that eight to nine CSs need to be performed to avoid one urinary incontinence case.28 Therefore, the risks associated with repeated CS delivery3–6 may not be justified, neither financially nor medically by the possible prevention of 1/8–9 different degrees of pelvic floor dysfunction.
A scoring system to predict future risk of pelvic floor dysfunction was proposed based on different known risk factors: urinary incontinence before confinement, family history of pelvic floor dysfunction, age, ethnicity, body mass index, and fetal weight.24 Knowing the pregnant woman score may assist in her counseling, particularly when she asks for CDMR. To further reduce women’s request of CDMR and control performing unnecessary CS, properly implemented antenatal care and antenatal education programs with clear strategies to enhance women’s knowledge and confidence in vaginal delivery are needed.29 Antenatal education implemented by the managing team should encourage vaginal delivery in the absence of fetal or maternal indications for CS.22 In Saudi community and within communities that encourage and desire big families, this sort of counseling appears to be important.
In the studied population, booking status or provided antenatal care was significantly lower for G2 compared to G1. Women who are deprived of antenatal care services are at higher risks of CS complications compared with those who enjoy antenatal care services.30 Antenatal care helps in early diagnosis and management of both maternal and fetal comorbidities occurring during pregnancy. It provides the proper setup where antenatal counseling is done.31,32
It seems that women with previous vaginal surgeries such as anterior and/or posterior colpoperineorrhaphy and those with previous urinary incontinence operation such as transvaginal tape were more in G2. Physicians’ training and women’s awareness about the available solution to their sexual dysfunction and incontinence agony have increased the popularity of these surgeries. Women with previous pelvic floor surgeries had significantly more CS delivery. Research has recommended performing elective CS delivery for women with previous successful incontinence surgeries.33 Women who undergo vaginal delivery after pelvic incontinence surgeries have higher tendencies for further pelvic floor surgeries,33 while CS deliveries carry a protective effect. However, systematic elective CS delivery for all patients with previous pelvic floor surgeries or incontinence surgeries is not liberally recommended. CS-associated morbidity and mortality need to be taken into consideration.34 Giving the literature results on the effect of vaginal delivery on women with previous pelvic floor surgery, we can conclude that both vaginal and CS delivery seem to be acceptable modes of delivery. Cases need to be individualized taking into consideration women’s medical history, preferences, incontinence risk factors, and the type of surgical repair done.33–37 An area for future randomized controlled trial and a possible area to be tackled in an effort to reduce CS delivery rate.
In 2009 compared to 2002, the decision for CS delivery was taken more frequently by junior staff (18% vs 8%). As a result, CS delivery rate was increased. Shortening of training duration and the reduction in daily working hours of obstetrics and gynecology trainees internationally have reduced their exposure and affected their experience in instrumental delivery conduction. Thus, many junior trainees may opt for safer procedure that they master better, such as early performance of CS delivery.38 Moreover, the generous availability of free medical care may lead to early admissions of laboring women. The prolonged observed latent phase of labor is known to be a significant predictor of more intervention in labor, including CS delivery. Therefore, it is recommended that initial preadmission laboring woman vaginal assessment is done by the most experienced medical staff present.39 Finally, defensive medicine do encompasses the practice of all physicians’ categories. More experienced mature physicians may have better understanding and less fear of malpractice problems.40 Those with less experience may be less tolerable to labor and cardiotocography abnormalities. Therefore, active involvement of the most responsible experienced physician in the decision taken for CS delivery may help in reducing its rate.
CS delivery remains a significant risk factor for transient tachypnea of the newborn, respiratory distress syndrome, and pulmonary hypertension.41 This fact could have contributed to the increased NICU admissions for G2 on top of the availability of more NICU beds during the year 2009 compared to 2002 in the studied institution.
Although this research did not include all the Saudi Arabian institutions and did not consider different private institutions, it has presented a population sample that could very well represent the Saudi Arabian pregnant population in the central region; the studied center is a referral center that accepts women from all over the Saudi central region. However, despite the effort taken to be as accurate as possible, this research may carry some errors related to its retrospective nature where due to the research methodology, the required data cannot be collected prospectively.
Conclusion
The trend of CS delivery rate is significantly increasing in the Saudi tertiary health care center. The reasons behind this increase are mainly related to the possible easy access to safer types of anesthesia and availability of intensive neonatal care unit, more involvement of juniors in decision making, more incontinence and pelvic repair surgeries, lack of maternal antenatal education, and inconsistency in the antenatal care provided. CS increased rate may be related to a change in physician’s practice rather than a change in maternal characteristics, and it appears to be reducible.
Acknowledgments
The authors acknowledge King Abdullah International Medical Research Center for approving the research conduction through its research committee.
Disclosure
The authors report no conflicts of interest in this work.
References
Abenhaim HA, Benjamin A. Higher caesarean section rates in women with higher body mass index: are we managing labour differently? J Obstet Gynaecol Can. 2011;33(5):443–448. | ||
Billard M. Cesarean section on demand: is it a fad or an advance in medical practice? Can Fam Physician. 2011;57(11):e406,1243. | ||
Ashtiani N, Hagmolen of ten Have W, Vreede WT, Vogt WP, van Elburg RM. Respiratoire complicaties bij vroege electieve sectio caesarea [Respiratory complications in early elective caesarean section]. Ned Tijdschr Geneeskd. 2009;153:A57. | ||
McDonnell NJ, Paech MJ, Clavisi OM, Scott KL, Group AT. Difficult and failed intubation in obstetric anaesthesia: an observational study of airway management and complications associated with general anaesthesia for caesarean section. Int J Obstet Anesth. 2008;17(4):292–297. | ||
Maric T, Tomic V, Darko K. Puerperalne komplikacije u prvorotki porodenih carskim rezom: studija parova [Puerperal complications in nulliparous women delivered by section caesarean: pair study]. Med Arh. 2006;60(4):246–250. | ||
Bulow-Lehnsby AL, Gronbeck L, Krebs L, Langhoff-Roos J. Komplikationer i forbindelse med kejsersnit i elektivt sectio-team [Complications of elective caesarean section performed by a special section team]. Ugeskr Laeger. 2006;168(47):4088–4090. | ||
Jonsdottir G, Bjarnadottir RI, Geirsson RT, Smarason A. Eru tengsl a milli ti[eth]ni keisaraskur[eth]a og bur[eth]armalsdau[eth]a a Islandi undanfarin 15 ar? [No correlation between rates of caesarean section and perinatal mortality in Iceland]. Laeknabladid. 2006;92(3):191–195. | ||
Hounton SH, Newlands D, Meda N, De Brouwere V. A cost-effectiveness study of caesarean-section deliveries by clinical officers, general practitioners and obstetricians in Burkina Faso. Hum Resour Health. 2009;7:34. | ||
Murray SF. Relation between private health insurance and high rates of caesarean section in Chile: qualitative and quantitative study. BMJ. 2000;321(7275):1501–1505. | ||
Giani U, Bruzzese D, Pugliese A, Saporito M, Triassi M. [Risk factors analysis for elective caesarean section in Campania region (Italy)]. Epidemiol Prev. 2011;35(2):101–110. | ||
Kmietowicz Z. NICE advises against caesarean section on demand. BMJ. 2004;328(7447):1031. | ||
Sultan AH, Stanton SL. Preserving the pelvic floor and perineum during childbirth – elective caesarean section? Br J Obstet Gynaecol. 1996;103(8):731–734. | ||
Scioscia M, Vimercati A, Cito L, Chironna E, Scattarella D, Selvaggi LE. Social determinants of the increasing caesarean section rate in Italy. Minerva Ginecol. 2008;60(2):115–120. | ||
Barton A. Caesarean section and litigation. Lancet. 2001;357(9255):556. | ||
Belizan JM, Quaranta P, Paquez E, Villar J. Caesarean section and fear of litigation. Lancet. 1991;338(8780):1462. | ||
McCallum C. Explaining caesarean section in Salvador da Bahia, Brazil. Sociol Health Illn. 2005;27(2):215–242. | ||
Nuttall C. Caesarean section controversy. The caesarean culture of Brazil. BMJ. 2000;320(7241):1074. | ||
Ba’aqeel HS. Cesarean delivery rates in Saudi Arabia: a ten-year review. Ann Saudi Med. 2009;29(3):179–183. | ||
Feng XL, Xu L, Guo Y, Ronsmans C. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull World Health Organ. 2012;90(1):30–39,39A. | ||
Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. | ||
Stavrou EP, Ford JB, Shand AW, Morris JM, Roberts CL. Epidemiology and trends for caesarean section births in New South Wales, Australia: a population-based study. BMC Pregnancy Childbirth. 2011;11:8. | ||
American College of Obstetricians and Gynecologists. ACOG committee opinion no. 559: cesarean delivery on maternal request. Obstet Gynecol. 2013;121(4):904–907. | ||
al-Mubarak KA, Adamchak DJ. Fertility attitudes and behavior of Saudi Arabian students enrolled in U.S. universities. Soc Biol. 1994;41(3–4):267–273. [Fall-Winter]. | ||
Wilson D, Dornan J, Milsom I, Freeman R. UR-CHOICE: can we provide mothers-to-be with information about the risk of future pelvic floor dysfunction? Int Urogynecol J. 2014;25(11):1449–1452. | ||
Rogers RG, Leeman LM, Borders N, et al. Contribution of the second stage of labour to pelvic floor dysfunction: a prospective cohort comparison of nulliparous women. BJOG. 2014;121(9):1145–1153. discussion 1154. | ||
Handa VL, Pierce CB, Munoz A, Blomquist JL. Longitudinal changes in overactive bladder and stress incontinence among parous women. Neurourol Urodyn. 2015;34(4):356–361. | ||
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I. A comparison of the long-term consequences of vaginal delivery versus caesarean section on the prevalence, severity and bothersomeness of urinary incontinence subtypes: a national cohort study in primiparous women. BJOG. 2013;120(12):1548–1555. | ||
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I. The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120(2):144–151. | ||
Faisal I, Matinnia N, Hejar AR, Khodakarami Z. Why do primigravidae request caesarean section in a normal pregnancy? A qualitative study in Iran. Midwifery. 2014;30(2):227–233. | ||
Adekanle DA, Adeyemi AS, Fadero FF. Booking status and caesarean section outcome in LAUTECH teaching Hospital, Osogbo. Niger J Med. 2008;17(1):25–28. | ||
Kottmel A, Hoesli I, Traub R, et al. Maternal request: a reason for rising rates of cesarean section? Arch Gynecol Obstet. 2012;286(1):93–98. | ||
Shaaban MM, Ahmed WS, Khadr Z, El-Sayed HF. Obstetricians’ perspective towards cesarean section delivery based on professional level: experience from Egypt. Arch Gynecol Obstet. 2012;286(2):317–323. | ||
Pradhan A, Tincello DG, Kearney R. Childbirth after pelvic floor surgery: analysis of Hospital Episode Statistics in England, 2002–2008. BJOG. 2013;120(2):200–204. | ||
Demoulin G, Thubert T, Faivre E, Trichot C, Deffieux X. Grossesse et post-partum des patientes porteuses de bandelette sous-uretrale: revue de la litterature [Pregnancy and postpartum of women with mid-urethral sling procedure: a review of the literature]. J Gynecol Obstet Biol Reprod (Paris). 2013; 42(6):518–524. | ||
Tommaselli GA, Di Carlo C, Formisano C, Fabozzi A, Nappi C. Vaginal delivery following single incision sling (TVT-Secur) for female stress urinary incontinence. J Obstet Gynaecol Res. 2013;39(2):608–610. | ||
Kohorst F, Flock F, Kreienberg R, Reich A. Pregnancy and delivery after tension-free vaginal tape (TVT) procedure: literature review and case report. Eur J Obstet Gynecol Reprod Biol. 2010;151(1):10–13. | ||
Tan HJ, Siu W, Faerber GJ, McGuire EJ, Latini JM. Long-term durability of pubovaginal fascial slings in women who then become pregnant and deliver. Int Urogynecol J. 2010;21(6):631–635. | ||
Ebulue V, Vadalkar J, Cely S, Dopwell F, Yoong W. Fear of failure: are we doing too many trials of instrumental delivery in theatre? Acta Obstet Gynecol Scand. 2008;87(11):1234–1238. | ||
Gharoro EP, Enabudoso EJ. Labour management: an appraisal of the role of false labour and latent phase on the delivery mode. J Obstet Gynaecol. 2006;26(6):534–537. | ||
Vimercati A, Greco P, Loizzi V, Loverro G, Selvaggi L. Medicina Difensiva nella scelta del taglio cesareo [“Defensive medicine” in the choice of cesarean section]. Acta Biomed Ateneo Parmense. 2000;71(Suppl 1):717–721. | ||
Kornacka MK, Kufel K. Ciecie cesarskie a stan noworodka [Neonatal outcome after cesarean section]. Ginekol Pol. 2011;82(8):612–617. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.