Back to Journals » Journal of Asthma and Allergy » Volume 14
Increase in Indoor Inhalant Allergen Sensitivity During the COVID-19 Pandemic in South China: A Cross-Sectional Study from 2017 to 2020
Authors Li Y , Hu H, Zhang T, Wang G, Huang H, Zheng P, Sun B , Zhang XD
Received 29 May 2021
Accepted for publication 23 July 2021
Published 29 September 2021 Volume 2021:14 Pages 1185—1195
DOI https://doi.org/10.2147/JAA.S322034
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Luis Garcia-Marcos
Yusi Li,1,* Haisheng Hu,2,* Teng Zhang,1,* Guoliang Wang,1 Huimin Huang,2 Peiyan Zheng,2 Baoqing Sun,2 Xiaohua Douglas Zhang1
1Faculty of Health Sciences, University of Macau, Taipa, Macau, China; 2Department of Allergy and Clinical Immunology, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, First Affiliated Hospital of Guangzhou Medical University, Guangzhou Medical University, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Baoqing Sun
Department of Allergy and Clinical Immunology, State Key Laboratory of Respiratory Disease, National Clinical Research Center for Respiratory Disease, Guangzhou Institute of Respiratory Health, First Affiliated Hospital of Guangzhou Medical University, Guangzhou Medical University, Guangzhou, People’s Republic of China
Tel +86 2083062865
Fax +86 2083062719
Email [email protected]
Xiaohua Douglas Zhang
Faculty of Health Sciences, University of Macau, Avenida da Universidade, Taipa, Macau, China
Tel +853 8822 4813
Email [email protected]
Purpose: Public health measures during COVID-19 have led to an unprecedented change in social lifestyle which might have an impact on the allergen sensitization in population. We sought to explore the prevalence patterns of serum inhalant and food allergen-specific IgE (sIgE) sensitization and serum total immunoglobulin E (tIgE) level among patients with clinical symptoms of suspected allergic diseases before and during the COVID-19 pandemic in south China.
Patients and Methods: A large epidemiology study was conducted on the prevalence patterns of sIgE sensitization and serum tIgE level among 13,715 patients with allergic symptoms in south China from 2017 to 2020. Chi-square test and Fisher exact test were used to test statistical significance of allergen sensitization difference among years. Logistic regression was performed to assess the magnitudes of the differences among years by adjusted odds ratios and 95% confidence intervals.
Results: The number of hospital visits for patients with suspected allergy symptoms decreased during COVID-19. The positive rates of indoor inhalant allergens (house dust mites, German cockroach, dog dander) and tIgE increased significantly in 2020, while no significant differences were found in food allergens (egg white, milk, soya bean, shrimp) before and during the COVID-19 pandemic. The odds of sIgE positives in indoor inhalant allergens and tIgE positive for 2017 and 2020 were all larger than 1.00. After grouping by age and gender, there were significant differences in the positive rates of indoor inhalant allergens and tIgE when comparing 2020 with 2017.
Conclusion: The prevalence of sensitization increased significantly to indoor inhalant allergens but not to food allergens in south China during the COVID-19 pandemic.
Keywords: allergy, epidemiology, specific immunoglobulin E, total immunoglobulin E
Introduction
Allergic disease is one of the most common diseases worldwide. The onset can happen at any stage of life and have a cross-life impact. Allergic diseases might result in poor sleep quality, absence from school or low work capacity, which inflict a high indirect cost of health care for the family and the society.1 Moreover, asthma elicited the outcome exacerbation of COVID-19 patients from the research of the Centers for Disease Control and Prevention of the United States.2 The mechanism of allergic disorders is complex and is not fully understood, which results in the limitation of the current therapy and poses challenges in disease diagnosis and management for clinicians. Former studies demonstrated that serum immunoglobulin E (IgE) level was significantly related to allergic symptoms with asthma3 and allergic rhinitis.4 The amount of the total IgE (tIgE) increases with the number and content of allergens exposed.5 The level of certain kind of allergen-specific IgE (sIgE) were the predictors of symptoms.6 The distributions and levels of tIgE and sIgE were influenced by genetic factors,7 environmental factors,8 and lifestyle.8 Hence, studying the prevalence patterns of sIgE sensitization and tIgE level could effectively prevent allergic diseases. The COVID-19 outbroke in south China on 19, January 2020 and public health measures like traffic control, mandatory mask use, social distancing, school suspension, home confinement, centralized quarantine had been carried out from late January 2020 which had led to an unprecedented change in social lifestyle changes caused by public health measures might affect the distribution of allergens, but the changes in the distribution of allergens during the pandemic were currently unclear.
Studies from the United States and the United Kingdom had shown that during the COVID-19 pandemic, the number of people suffering from asthma had decreased, but the causes were not confirmed.9–11 This might be caused by the decrease in other human-to-human respiratory virus-borne diseases, the decrease in outdoor and indoor allergens, or the reduction of air pollution. The content of serum sIgE and tIgE could indicate the exposure level of allergens. No studies have been conducted to evaluate the change in prevalence patterns of serum indoor inhalant and food sIgE sensitization and tIgE level in population before and during the COVID-19 pandemic. The study aimed to analyze the changes in the sIgE positive rate of four common indoor inhalant allergens, four common food allergens and tIgE level among patients with clinical allergic symptoms before and during the COVID-19 pandemic in south China through a 4 years’ cross-sectional study. The distribution of allergen prevalence patterns in gender and age groups among different years was then discussed. Furthermore, the factors affecting the change prevalence to allergen sensitization before and during the COVID-19 pandemic were also explored. This study could reveal the change of prevalence patterns of allergen sensitization during the pandemic. It could provide an epidemiology basis for the prevention and diagnosis of allergic diseases during the COVID-19 pandemic.
Patients and Methods
Study Population
This was a cross-sectional study. Data were obtained from the First Affiliated Hospital of the Guangzhou Medical University. We collected data on patients with suspected allergic diseases in the hospital and their results of the concentration of serum sIgE and tIgE every year to explore the distribution and changes of allergen sensitization in south China each year. In this study, data from 2017 to 2020 (February and June) were extracted. A total number of 13,725 patients were included with 2835, 3906, 4501 and 2473 from 2017 to 2020, respectively. And the concentration of serum sIgE and tIgE was tested. The data for analysis included patients’ disease type, gender, age, serum sIgE/tIgE test items and levels. Suspected allergic diseases included asthma, allergic rhinitis, eczema, catarrhal otitis media or atopic dermatitis. Four indoor inhalant allergens, namely, house dust mites (Dermatophagoides pteronyssinus, Dermatophagoides farina), German cockroach and dog dander, four food allergens, namely, egg white, milk, soya bean and shrimp and tIgE were evaluated in this study. All the allergens included in this study were common in south China.12 The study was approved by the ethics committee of the First Affiliated Hospital of Guangzhou Medical University (Reference number: GYFYY-2016-73) of Guangzhou Medical University. Written informed consent was obtained from all adults and legal guardians of the participating children. This study was performed in accordance with the Declaration of Helsinki.
Allergen IgE Detection
Patients’ serum sIgE and tIgE were collected by the nurses and detected by the chemist of the hospital laboratory using the ImmunoCAP 1000 system (Thermo Fisher Scientific Inc., California, USA). All procedures had standardized procedure guidelines. For sIgE, negative reactivity was defined as the detection content less than 0.35 kUA/L and content equal to or greater than 0.35 kUA/L was considered as positive reactivity.13 For the absolute sIgE levels, the reactivity was categorized quantitatively into six classes: class 1 (≥0.35 to <0.70 kUA/L), class 2 (≥0.70 to <3.50 kUA/L), class 3 (≥3.50 to <17.50 kUA/L), class 4 (≥17.50 to <50.00 kUA/L), class 5 (≥50.00 to <100.00 kUA/L), and class 6 (≥100.00 kUA/L).13 For tIgE, the detection content less than 113kU/L was defined as negative reactivity, while equal or more than 113kU/L meant positive reactivity.14
Statistical Analysis
The prevalence of positive sIgE and tIgE was shown as proportion. Chi-square test and Fisher exact test were used to test statistical significance of allergen sensitization among years. When the expected number of studied people who were sensitive to allergen is less than 5, Fisher’s exact test is used, and the chi-square test is used in other cases. Logistic regression was performed to assess the magnitudes of the differences between the prevalence of positive sIgE and tIgE among years by adjusted odds ratios and 95% confidence intervals. Then, to further understand the influence of the COVID-19 pandemic on allergen sensitization in the targeted population, it was also used to estimate the adjusted odds ratios in different genders and different age groups. Ninety-five percent confidence intervals were used to assess the magnitudes of the associations and P<0.05 was considered statistically significant. R studio 3.6.2 was used for data analysis.
Results
Demographic Characteristics
Table 1 shows the number of patients tested for each allergen/tIgE and the positive rate of each allergen/tIgE in 2017, 2018, 2019 and 2020, respectively. Compared with previous years, the number of hospital visits for patients with suspected allergy symptoms decreased. Figure S1 and S2 showed the ratio of allergic patients with higher inhalant allergen and food allergen content (Class 4–6) to those with lower indoor inhalant allergen and food allergen content (Class 1–3) from February to June between 2017 and 2020 in south China. Among all allergic patients, the proportion of patients with higher allergen content and patients with lower allergen content did not change significantly among 2017 and 2020, except for the dog dander allergen. In each year, the overall prevalence of positive serum sIgE responses to the 8 allergens in south China from highest to lowest was house dust mites (Dermatophagoides farina, Dermatophagoides pteronyssinus), milk, egg white, German cockroach, shrimp, dog dander, soya bean. The positive rate was higher in the male population than the female population in the analyzed allergens shown in Table S1. School-age children aged 6–17 had a higher positive rate of house dust mites (Dermatophagoides pteronyssinus, Dermatophagoides farina) than preschoolers and adults. In China, children at the age of 0–5, and 6–17 were defined as preschoolers and schoolers, respectively. Adult was people equal or over the age of 18. Allergies to egg white and milk were more common in preschoolers aged 0–5 shown in Table S2.
 |
Table 1 Characteristics Background of Patients with Clinical Symptoms of Suspected Allergic Diseases from February to June Between 2017 and 2020 in South China |
Serum sIgE Reactivities to Allergens and tIgE Reactivities in Patients in Different Years
Figure 1 shows the adjusted odds ratio of sIgE reactivities to allergens and tIgE reactivity among patients with clinical symptoms of suspected allergic diseases in south China in 2017, 2018, 2019, 2020. For indoor inhalant allergens, the positive rate was statistically significant different (P<0.05) in 2020 compared with 2017, while no significant differences were found when comparing 2018 and 2019 with 2017. The odds of positives in indoor inhalant allergens for 2017 and 2020 were all larger than 1.00, with 1.57 (P<0.001) for Dermatophagoides pteronyssinus, 1.43 (P=0.024) for Dermatophagoides farina, 1.50 (P<0.001) for German cockroach and 2.00 for dog dander, respectively. For food allergens, the differences in positive rate of milk, soya bean, shrimp were not significant when comparing 2018, 2019, 2020 with 2017, respectively. The positive rate of egg white had the odds of 1.42 for 2017 and 2020 which is significantly different. For the positive rate of tIgE, a significant difference was found for 2017 and 2020 with the odds of 1.27 (p<0.001).
Serum sIgE Reactivity to Allergens and tIgE Reactivities in Patients in Male and Female in Different Years
No significant changes were found in male and female in the serum sIgE positive rates of indoor inhalant allergen in 2017, 2018 and 2019, while there were increasing serum sIgE positive rates of indoor inhalant allergens both in male and female in 2017, when compared with 2020 as shown in Figure 2 and Table 2. For food allergen, slight changes of serum sIgE positive rates were shown in male and female in 2017 and 2020, but most of them were not statistically significant different except shrimp in male group. No changes in the serum sIgE positive rates of food allergens were found in male and female in 2017, 2018 and 2019. In 2017, 2018 and 2019, the positive rates of tIgE in male and female had been maintained at about 0.47 and 0.36, respectively, without much fluctuation. In 2020, the male tIgE positive rate was 0.55 and the female tIgE positive rate was 0.46. Compared with the previous three years, the positive rate of male tIgE and the positive rate of female tIgE were significantly higher in 2020 with statistically significant difference.
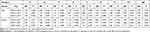 |
Table 2 Adjusted Odds Ratio of sIgE Reactivities to Allergens and tIgE Reactivity Among Patients with Clinical Symptoms of Suspected Allergic Diseases in Different Genders in South China |
Serum sIgE Reactivity to Allergens and tIgE Reactivities in Patients in Age Groups in Different Years
In Figure 3 and Table 3, the positive rates of serum sIgE of indoor inhalant allergens fluctuated slightly at an average level in all age groups in 2017, 2018 and 2019, while increasing serum sIgE positive rates of indoor inhalant allergens were shown in all age groups in 2020, when compared with 2017. Compared with 2017, the positive rates of serum sIgE of Dermatophagoides pteronyssinus were significantly different in each age group in 2020. The positive rates of serum sIgE of German cockroach allergen were significantly different in the adult group, and the positive rates of serum sIgE of dog dander allergen were significantly different between the school-age children group and the adult group in 2020 when compared with 2017. No significant differences were found for serum sIgE positive rates in all food allergens of different age groups from 2017 to 2020. The rising positive rates were also seen in tIgE in all age groups in 2017 compared with 2020 with significant difference. When comparing 2018 and 2019 with 2017, the positive rates decreased with significant differences in the pre-school age group and no differences were found in the school-age group and adult group.
 |
Table 3 Adjusted Odds Ratio of sIgE Reactivities to Allergens and tIgE Reactivity Among Patients with Clinical Symptoms of Suspected Allergic Diseases in Different Age Groups in South China |
Discussion
COVID-19 could cause an asthma attack by affecting the respiratory tract and asthma elicited the outcome exacerbation of COVID-19 patients from the research of the Centers for Disease Control and Prevention of the United States.2 Particularly, severe asthma was an aggravating factor for the severity of COVID-19.15,16 Hence, it is critical to reduce the occurrence of allergic diseases to help reduce the COVID-19 fatality rate and the public health burden of society during the COVID-19 pandemic. Public health measures like the school suspension, home confinement, centralized quarantine during the COVID-19 pandemic had a profound influence on every aspect of daily life. Change in lifestyle could trigger the change of people’s susceptibility to various allergens. Avoiding contact with allergens could effectively reduce the occurrence of allergic symptoms. Therefore, research on the changes of prevalence patterns of allergen sensitization was very important to provide an updated epidemiology basis for the prevention of allergic diseases and to help clinicians offer effective individual treatments for unique patient groups during the COVID-19 pandemic. Although there are studies revealing the prevalence patterns of allergen sensitization by region, gender, age, and season among patients with allergic symptoms in mainland China,17 no studies have been published to reveal the change of prevalence patterns of allergen sensitization before and during the COVID-19 pandemic yet. To fill this gap, in this study, four common indoor inhalant allergens and four food allergens in south China were included, namely house dust mites (Dermatophagoides pteronyssinus, Dermatophagoides farina), German cockroach, dog dander, egg white, milk, soya bean, shrimp to explore prevalence patterns of allergen sensitization before and during the COVID-19 pandemic.
In this four-year cross-sectional study, the number of hospital visits for patients with suspected allergy symptoms decreased during the COVID-19 compared with previous years. Our finding was similar to previous research. In the Northern United States, there was a dramatic decrease around 76% drop in asthma-related Emergency Department use of all severities in children during the COVID-19 pandemic.10 In the United Kingdom, there was a drop between 76% and 90% in emergency visits for asthma attack among children.9,11 This might be caused by the decrease in other human-to-human respiratory virus-borne diseases, the decrease in outdoor and indoor allergens, or the reduction of air pollution.9,10,18 In addition, some patients might prefer to control the onset of allergic symptoms at home rather than going to the hospital due to the pandemic of COVID-19, which could also lead to a reduction in the number of hospital visits.
The interesting finding of our research was that the positive rates of indoor inhalant allergens, including house dust mites (Dermatophagoides pteronyssinus, Dermatophagoides farina), German cockroach, dog dander and tIgE were not significantly different in 2017, 2018, and 2019, while the positive rates in 2020 were significantly higher than in 2017, 2018, and 2019, which might be caused by the change in behaviors and the hygiene of the home environment during the pandemic period.
The increasing positive rate of house dust mite during the COVID-19 pandemic might be because people stayed at home for a long time with poor ventilation. Southern China had a subtropical monsoon climate with high humidity. The lack of ventilation led to long-term high relative humidity and lack of sunshine in the house, which were more conducive to the accumulation and reproduction of dust mites in carpets, pillows, and mattresses.19,20
The increase in the positive rate of allergies to German cockroach might be related to the increase in the positive rate of allergies to house dust mite because these two allergens had a positive cross-reactivity in allergic diseases.21 The poor ventilation of the house also resulted in the reproduction of cockroaches. Moreover, during the pandemic, many families stored lots of food to avoid frequent trips to the supermarket where crowds of people gathered. This would also lead to the breeding of cockroaches and increase allergens in the house. In our study, the positive rates of German cockroach had increased significantly in the male population and adults during the COVID-19 pandemic. It might be because the male population and adults were more sensitive to German cockroach than in female population and children in mainland China based on a cross-sectional study conducted in nationwide.21
The increase in the positive rate of dog danger might be related to the prolonged exposure to pets during the pandemic, because direct exposure to dog dander was an independent risk factor for the development of allergic diseases.22 Moreover, the increased exposure of house dust mite also resulted in the higher dog dander sensitivity of patients as there was a positive interaction between these two allergens.22 In our research, the increase of the positive rate of dog dander was significant different in school-age children and adults, while no significant difference in preschoolers before and during the pandemic. It was because that adult had more severe allergic symptoms like asthma when exposed to a greater amount of dog dander, while children had lower prevalence of allergic diseases under the exposure of greater amount of dander based on a large cross-sectional study conducted in US.22,23 The increase of tIgE during the pandemic, partly as the result of the increase of indoor inhalant sIgE. Previous research found that for people sensitized to some allergen, their certain serum sIgE and tIgE level would increase.14 When the content of sIgE was low, the high level of tIgE could predict poly-sensitization to several allergens.24
No significant differences were found in food allergen before and during the COVID-19 pandemic except egg white and shrimp allergen. The overall positive rates of egg white allergen sensitization were significantly different, while no differences were found when stratified by gender or age. Simpson’s Paradox could explain this phenomenon.25 In this study, data comparison among different groups was preferred as allergen sensitization was greatly influenced by gender and age. Thus, the positive rates of egg white were not significantly different before and during the COVID-19 pandemic. For shrimp allergen, a slight difference was found with stratified gender which might be related to the co-sensitization with the increasing positive rate of house dust mite26 and German cockroach.27 Overall, the positive rate of food allergens did not change significantly during the COVID-19 pandemic. The reason can be that people’s eating habits had not been changed during the pandemic. By comparing with the positive rates of food allergens remaining the same, we were more certain to believe that the hygiene of the home environment was associated with the increase in the positive rate of indoor inhalant allergens and tIgE, rather than other factors like the different characteristics of the populations and the climate change in different years.
To confirm that the increase positive rates of indoor inhalant allergens were not due to the situation that more severe asthma patients were seeking hospital care during COVID, we analyzed the ratio of allergic patients with higher allergen content (Class 4–6) to those with lower allergen content (Class 1–3) from 2017 to 2020. No significant change of these ratios was found before and during the COVID-19 except dog dander (Figure S1 and S2). It illuminated that both patients with mild allergic symptoms and patients with severe allergic symptoms decreased proportionally during the pandemic. The decrease of allergic disease visits was also found in the latest study, in which the proportions of all levels of triage acuity were similar before and during the COVID-19 pandemic in the United States, so the delays in care-seeking behavior for lower acuity events might not be the reason for this phenomenon.10
There were strengths in this study. Firstly, the data collected were representative as they came from the largest respiratory disease research center in Guangdong Province which was also the State Key Laboratory of Respiratory Disease and all data were based on real-life medical data. Secondly, it was a four-year cross-sectional study with a large sample size. The positive rate of allergens and tIgE in the targeted population did not change significantly in the first three years, while the positive rate of indoor inhalant allergens and tIgE increased significantly in the fourth year, which provided more favorable evidence for the inference of this study. Thirdly, in this study, data were from patients in the same region from February to June in each year, which excluded the influence of regional and genetic differences on allergen sensitivity and removed the climate and season influence factors as there were no major climate changes or population migration in south China in the past four years. Fourthly, studying the change in the allergens positive rate in the same area before and after the policy could better attribute the change in the positive rate to the influence of policy factors that led to the differences in people’s behavior. Because before and after the policy was conducted, other characteristics of populations, including education level, and social status did not change significantly in addition to the changes in crowd behavior. The limitation of this study was that pollen allergens and cat dander allergen were not included. Only allergens tested more frequently were analyzed in this study. The reasons that pollen allergens were less tested were that pollens were not the main allergens in south China and hospital decreased the number of tests in pollen allergens to reduce the burden on medical staff and reduce medical consumables during the pandemic. The reason for the decrease in the number of cat dander allergen tests was unknown. It might be related to the patient’s explanation that the symptoms were not closely related to the exposure on cat.
Conclusion
This four-year cross-sectional study conducted in south China finds that the number of hospital visits for patients with suspected allergy symptoms decreased during the COVID-19 pandemic in 2020, when compared with previous years. In addition, the data in this study showed that only the positive rates of indoor inhalant allergens increased, whereas the positive rates of food allergens remained stable during the COVID-19 pandemic. The increasing prevalence of sensitization to indoor inhalant allergens might be influenced by the lifestyle change during the pandemic. Staying at home for a long time without frequent ventilation and insufficient sunshine might result in these changes in positive rate. Our study could provide an evidence for deeper research about the epidemiology of allergic diseases and better prevention and diagnosis of allergic diseases during the COVID-19 pandemic.
Data Sharing Statement
Survey data are available from the corresponding author on request.
Acknowledgments
This study was supported by the University of Macau (grant numbers: FHS-CRDA-029-002-2017, EF005/FHS-ZXH/2018/GSTIC and MYRG2018-00071-FHS), the Science and Technology Development Fund, Macau SAR (File no. 0004/2019/AFJ and 0011/2019/AKP), the National Natural Science Foundation of China (81802076 and 81871736), the National Key Technology R&D Program (2018YFC1311902), the Guangdong Science and Technology Foundation (2019B030316028), the Guangzhou Municipal Health Foundation (20191A011073), and the Guangzhou Science and Technology Foundation (201804020043). Kuan Cheok Lei helped the proofreading of the work.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Hellgren J, Cervin A, Nordling S, Bergman A, Cardell LO. Allergic rhinitis and the common cold high cost to society. Allergy. 2010;65(6):776–783. doi:10.1111/j.1398-9995.2009.02269.x
2. Chow N, Fleming-Dutra K, Gierke R, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with Coronavirus disease 2019 - United States, February 12–March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382–386. doi:10.15585/mmwr.mm6913e2
3. Simpson A, Soderstrom L, Ahlstedt S, Murray CS, Woodcock A, Custovic A. IgE antibody quantification and the probability of wheeze in preschool children. J Allerg Clin Immunol. 2005;116(4):744–749. doi:10.1016/j.jaci.2005.06.032
4. Siroux V, Ballardini N, Soler M, et al. The asthma-rhinitis multimorbidity is associated with IgE polysensitization in adolescents and adults. Allergy. 2018;73(7):1447–1458. doi:10.1111/all.13410
5. Yilmaz NBZ, Ozaslan J, Özaslan J. Efficiency of some in vitro allergy tests for evaluating atopy in children and adults. Clin Chem Lab Med. 1999;37(10):981–985. doi:10.1515/CCLM.1999.145
6. Petra EDE, Gerben Ter R, Rob CA, et al. Accuracy of specific IgE in the prediction of asthma: development of a scoring formula for general practice. Br J Gen Pract. 2005;55(511):125–131.
7. Valenta R. The future of antigen-specific immunotherapy of allergy. Nat Rev Immunol. 2002;2(6):446–453. doi:10.1038/nri824
8. Park HJ, Kim EJ, Yoon D, et al. Prevalence of self-reported allergic diseases and IgE levels: a 2010 KNHANES analysis. Allergy Asthma Immunol Res. 2017;9(4):329–339. doi:10.4168/aair.2017.9.4.329
9. Gupta A, Bush A, Nagakumar P. Asthma in children during the COVID-19 pandemic: lessons from lockdown and future directions for management. Lancet Respir Med. 2020;8(11):1070–1071. doi:10.1016/S2213-2600(20)30278-2
10. Kenyon CC, Hill DA, Henrickson SE, Bryant-Stephens TC, Zorc JJ. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allerg Clin Immunol Pract. 2020;8(8):2774–2776.e1. doi:10.1016/j.jaip.2020.05.045
11. Chavasse RJ. Covid-19: reduced asthma presentations in children. BMJ. 2020;370:m2806–m2806. doi:10.1136/bmj.m2806
12. Luo W, Wang D, Zhang T, et al.Prevalence patterns of allergen sensitization by region, gender, age, and season among patients with allergic symptoms in Mainland China: a four-year multicenter study. Allergy. 2020. doi:10.1111/all.14597
13. Zeng G, Luo W, Wu Z, et al. A cross-sectional observational study on allergen-specific IgE positivity in a southeast coastal versus a southwest inland region of China. Sci Rep. 2017;7(1):9593. doi:10.1038/s41598-017-10109-3
14. Sun BQ, Wei NL, Wang HY, Jing L, Zhong N. Detection and significance of serum total IgE in patients with respiratory allergies. Chin Public Health. 2008;24(1):103–104. doi:10.3321/j.issn:1001-0580.2008.01.039
15. Maes T, Bracke K, Brusselle GG. Reply to Lipworth et al.: inhaled corticosteroids and COVID-19. Am J Respir Crit Care Med. 2020;202(6):900–902. doi:10.1164/rccm.202006-2129LE
16. Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature (London). 2020;584(7821):430–436. doi:10.1038/s41586-020-2521-4
17. Luo W, Wang D, Zhang T, et al. Prevalence patterns of allergen sensitization by region, gender, age, and season among patients with allergic symptoms in mainland China: a four‐year multicenter study. Allergy. 2021;76(2):589–593. doi:10.1111/all.14597
18. Poole S, Brendish NJ, Tanner AR, Clark TW. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir Med. 2020;8(12):e92–e93. doi:10.1016/S2213-2600(20)30502-6
19. Crisafulli D, Almqvist C, Marks G, Tovey E. Seasonal trends in house dust mite allergen in children's beds over a 7-year period. Allergy. 2007;62(12):1394–1400. doi:10.1111/j.1398-9995.2007.01533.x
20. Tsakok TD, Weinmayr GP, Jaensch AM, Strachan DPP, Williams HCP, Flohr CP. Eczema and indoor environment: lessons from the International Study of Asthma and Allergies in Childhood (ISAAC) phase 2. Lancet. 2015;385:S99–S99. doi:10.1016/S0140-6736(15)60414-7
21. Bao-qing SUN, Xu-xin LAI, Birgitte G, Michael Dho S, Nan-shan Z. Prevalence of sensitivity to cockroach allergens and IgE crossreactivity between cockroach and house dust mite allergens in Chinese patients with allergic rhinitis and asthma. Chin Med J. 2010;123(24):3540–3544. doi:10.3760/cma.j.issn.0366-6999.2010.24.007
22. Park Y-B, Mo E-K, Lee J-Y, et al. Association between pet ownership and the sensitization to pet allergens in adults with various allergic diseases. Allergy Asthma Immunol Res. 2013;5(5):295–300. doi:10.4168/aair.2013.5.5.295
23. Shargorodsky J, Garcia‐Esquinas E, Umanskiy R, Navas‐Acien A, Lin SY. Household pet exposure, allergic sensitization, and rhinitis in the U.S. population. Int Forum Allergy Rhinol. 2017;7(7):645–651. doi:10.1002/alr.21929
24. Xi C, Sun B. IgE cross-reactivity between house dust mite and shrimp. Eur Respir J. 2016;48(suppl 60):PA1092. doi:10.1183/13993003.congress-2016.PA1092
25. Janket S-J, Ackerson LK, Diamandis E. Simpson’s paradox in proof-of-concept studies. Nat Med. 2019;25(11):1640. doi:10.1038/s41591-019-0624-y
26. Luo W, Hu H, Tang W, et al. Allergen sensitization pattern of allergic adults and children in southern China: a survey based on real life data. Allerg Asthma Clin Immunol. 2019;15(1):42. doi:10.1186/s13223-019-0357-y
27. Liao C, Hu H, Huang Z, et al. Shrimp and cockroach co-sensitization in Southern China: association with moth sensitization. Allerg Asthma Proc. 2020;41(3):e54–e60. doi:10.2500/aap.2020.41.200013
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



