Back to Journals » Clinical Interventions in Aging » Volume 18
Incidence, Predictors, and Strategies for Retrograde Wire Tracking Failure via Poor Septal Collateral Channels in Chronic Total Occlusion
Authors Wang CF, Chen BJ, Luan B, Wang Y , Zhang XJ, Qu HB
Received 7 June 2023
Accepted for publication 8 September 2023
Published 13 September 2023 Volume 2023:18 Pages 1503—1512
DOI https://doi.org/10.2147/CIA.S424882
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Cheng-Fu Wang,1 Bao-Jun Chen,1 Bo Luan,1 Yong Wang,2 Xiao-Jiao Zhang,1 Hai-Bo Qu1
1Department of Cardiology, The People’s Hospital of China Medical University, The People’s Hospital of Liaoning Province, Shenyang, People’s Republic of China; 2Department of Cardiology, Shenzhen Luohu Hospital Group Luohu People’s Hospital (The Third Affiliated Hospital of Shenzhen University), Shenzhen, People’s Republic of China
Correspondence: Hai-Bo Qu, Email [email protected]
Background: Retrograde guidewire (GW) tracking success via a poor septal collateral channel (CC) when an antegrade approach fails is crucial for successful revascularization of coronary chronic total occlusion (CTO) with poor septal CC. However, the incidence, predictors, and management strategies for retrograde GW tracking failure via poor septal CC remain unclear.
Methods: In total, 122 CTO patients who underwent retrograde septal percutaneous coronary intervention (PCI) with poor CC between January 2017 and May 2022 were retrospectively analyzed. Patients were divided into the retrograde GW tracking success group (success group) and the retrograde GW tracking failure group (failure group). Clinical and angiographic data were compared to investigate the predictors of retrograde GW tracking failure.
Results: The incidence of GW tracking failure was 22.1% (27/122). Patients in the failure group had a higher prevalence of left anterior descending artery (LAD) CTO (66.7% vs 37.9%; p = 0.009) and a higher incidence of well-developed non-septal collateral (66.7% vs 30.5%; p = 0.001). Patients with a septal CC diameter ≥ 1 mm (48.1% vs 70.5%; p = 0.040), ≥ 3 septal CCs (44.4% vs 66.3%; p = 0.046), and initial retrograde application of Guidezilla (37.0% vs 60.0%; p = 0.048) were significantly lower in the failure group than in the success group. The binary logistics regression model showed that a CC diameter < 1 mm, well-developed non-septal collateral, and LAD CTO were independent predictors for GW tracking failure in patients undergoing retrograde CTO PCI via poor septal CC.
Conclusion: The success rate of retrograde GW tracking via poor septal CC was high, with a relatively high procedural success rate. A CC diameter < 1 mm, well-developed non-septal collateral, and LAD CTO were independent predictors of GW tracking failure in patients undergoing retrograde CTO PCI via poor septal CC.
Keywords: coronary chronic total occlusion, retrograde, PCI, septal collateral channels
Introduction
Coronary chronic total occlusion (CTO) is defined as angiographically proven thrombolysis in myocardial infarction (TIMI) grade 0 flow with a duration > 3 months.1 As coronary angiography (CAG) has been widely used in the diagnosis and treatment of coronary artery disease (CAD), the prevalence of CTO in patients with CAD undergoing CAG has been reported as 16–18%.1 CTO percutaneous coronary intervention (PCI) had been considered the most challenging procedure with only an approximately 70% procedural success rate before the retrograde technique was introduced.2 However, with the development of a dedicated CTO guidewire (GW) and microcatheter (MC), as well as some specific CTO strategies and experiences, the procedural success rate has crossed 90%. Despite the advanced retrograde PCI strategies, GW and MC tracking failure is not uncommon in a considerable proportion of patients, especially in those with poor collateral circulation (CC), which is a major reason for CTO PCI failure.
Retrograde CTO PCI via septal CC has been considered more effective and safer than epicardial collaterals due to its lower risk of vascular perforation.3 A previous study suggested that no angiographically visible septal collaterals were unsuitable for retrograde PCI and were a risk factor for failure of CTO PCI.4
However, some scholars have suggested the surfing technique, in which non-visible septal CC is used as a channel for retrograde CTO PCI.5 It is safe and effective to use the surfing technique to track non-visible septal CC during retrograde CTO PCI. Nonetheless, the predictors for failure of CTO PCI via poor septal CC remain unclear. To date, the detailed management strategies for this clinical issue have been scarcely discussed. In light of the controversial opinion and unclear clinical predictive risk factors on this issue, we aimed to investigate the incidence and predictors of retrograde wire tracking failure via poor septal CC during CTO PCI and summarize the principles and single-center management strategies for this clinical issue in order to improve the understanding and management of these specific patients.
Methods
Study Population
From January 2017 to May 2022, we continuously enrolled 122 CTO patients who underwent retrograde septal PCI with poor CC at the People’s Hospital of Liaoning Province. The inclusion criteria were either failure of previous antegrade intervention or inability to cross an antegrade GW during CTO PCI. The exclusion criteria included cerebral infarction or cerebral hemorrhage within 6 months, severe liver or renal failure, acute or chronic infection, moderate to severe valvular heart disease, contraindications to antiplatelet therapy, the New York Heart Association (NYHA) functional class IV, and refusal to participate in this study. All procedures were performed by an experienced cardiologist who had performed quite a high volume of CTO procedures. The right radial artery and right femoral artery were preferred for routine access for bilateral CAG and retrograde PCI. The standard dose of unfractionated heparin (100 IU/kg) was used, and 2000 IU was added every hour to maintain an activated clotting time of 300–350 s. The study was approved by the local research ethics committee and performed in accordance with the Declaration of Helsinki. All patients provided informed consent prior to their participation in this study.
Definitions
Coronary collateral circulation grade was estimated by the Werner score with a CC 0–2 grade. CC0 was defined as a discontinuous connection between the donor and recipient vessels; CC1 as a continuous thread-like connection; and CC2 as a continuous, small side branch-like connection.6 Poor septal CC was defined as CC0 and CC1. CC tortuosity was defined as the presence of more than two successive curves (within 2 mm) > 180° within a segment length and < 3 times the diameter of the collateral channel.7 Retrograde GW tracking success was defined as the GW crossing the poor septal CC to the distal cap of the CTO lesions. Technical success was defined as successful stent implantation with residual stenosis < 30% and a TIMI flow grade of 3.7 Procedural success was defined as technical success without major complications.7 Major complications were defined as severe perforation (including of the collateral and target vessels) or other complications requiring emergency pericardiocentesis or cardiac surgery.
Interventional Procedures
Bilateral angiography was performed in all included individuals to comprehensively evaluate the morphology of the CTO lesions. An antegrade attempt was performed first. The included patients all had failure of antegrade CTO PCI. Next, retrograde CTO PCI was attempted. The first septal was the first choice for retrograde GW tracking, and the selection of GWs for retrograde CC tracking was left to the physician’s discretion. Retrograde GW tracking was performed with either hydrophilic polymer-coated GWs or stiffer CTO GWs. The GW tracking techniques and the procedural strategies were determined by the cardiologist based on the lesion characteristics. The retrograde wire crossing was attempted for short CTO lesions, and reverse-controlled antegrade or retrograde subintimal tracking was performed for long lesions.
Statistical Analysis
Categorical variables were expressed as percentages, and continuous variables were expressed as the mean and standard deviation. The Student’s t-test or Mann–Whitney U-test was performed for continuous variables, and the chi-square test or Fisher exact test was performed for categorical variables. A CC diameter < 1 mm, ≥ 3 CCs, well-developed non-septal collateral, initial retrograde application of Guidezilla with strong support, and left anterior descending artery (LAD) CTO were tested in the univariate analysis. A binary logistics regression model was performed to investigate the independent predictors of successful retrograde GW tracking via poor septal CC. All tests were two-sided, and p < 0.05 was considered statistically significant.
Results
Baseline and Clinical Characteristics
A total of 122 CTO patients with poor septal CC who underwent retrograde septal PCI were consecutively included in this study from the People’s Hospital of Liaoning Province between January 2017 and May 2022. The incidence of GW tracking failure was 22.1% (27/122). The baseline characteristics of the two groups, including gender, age, diabetes mellitus, hypertension, dyslipidemia, current smoking status, prior myocardial infarction, prior PCI, prior coronary artery bypass grafting, prior failed attempt, left ventricular ejection fraction, and NYHA cardiac function grade 2–3 on admission, were comparable between the two groups (p > 0.05; Table 1).
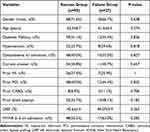 |
Table 1 Clinical Characteristics of the Two Groups |
Angiographic and Procedural Characteristics of the Two Groups
Coronary angiography results showed that there were no significant differences in in-stent CTO, failed previous antegrade attempt, J-CTO score, or Werner score of 0–1 (p > 0.05). However, patients in the failure group had a higher prevalence of LAD CTO (66.7% vs 37.9%; p = 0.009) and a higher incidence of well-developed non-septal collateral (66.7% vs 30.5%; p = 0.001). Patients with a septal CC diameter ≥ 1 mm (48.1% vs 70.5%; p = 0.040), ≥ 3 septal CCs (44.4% vs 66.3%; p = 0.046), and initial retrograde application of Guidezilla (37.0% vs 60.0%; p = 0.048) were significantly lower in the failure group than in the success group (Table 2). In the success group, an MC could not be advanced after successful GW tracking in 10.5% (10/95) of patients. After two patients successfully underwent retrograde epicardial collateral PCI and three patients successfully underwent antegrade PCI, there were five patients with failed CTO PCI, among whom three developed severe complications, with a 94.7% technical success rate and a 91.4% procedural success rate. In the failure group, 14 patients successfully underwent retrograde epicardial collateral PCI, and eight patients underwent antegrade PCI, resulting in five patients with failed CTO PCI, among whom three developed severe complications, with an 81.5% technical success rate and a 70.4% procedural success rate (Figure 1). However, the overall technical and procedural success rates were relatively high at 91.8% (112/122) and 86.9% (106/122), respectively. Nonetheless, the technical success rate (81.5% vs 94.7%; p = 0.042) and procedural success rate (91.4% vs 70.4%; p = 0.008) were significantly lower in the failure group than in the success group (Table 2). The GWs used in the success group are shown in Figure 2. Sion Black was the most widely used GW in retrograde PCI via poor septal CC, followed by Sion and Sion03 (Figure 3).
 |
Table 2 Angiographic and Procedural Characteristics of the Two Groups |
 |
Figure 1 Clinical management of the procedure. Abbreviations: GW, guide wire; CC, collateral channels; MC, microcatheter; CTO, chronic total occlusion. |
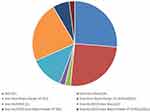 |
Figure 2 The usage of GW for collateral channels tracking in the studied populations. |
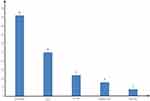 |
Figure 3 The final GW for poor septal collateral channel tracking success. |
Procedural Complications of the Two Groups
There were no significant differences in procedural complications between the two groups in terms of septal hematoma, donor vessel dissection, CC perforation, target vessel perforation, or cardiac tamponade (p > 0.05). However, the overall procedural complications were significantly higher in the failure group than in the success group (48.1% vs 25.3%; p = 0.032; Table 3).
 |
Table 3 Procedural Complications of the Two Groups |
Predictors of GW Tracking Failure in Patients with Poor Septal Collaterals
GW tracking failure was associated with a CC diameter < 1 mm, ≥ 3 CCs, well-developed non-septal collateral, an initial retrograde application of Guidezilla with strong support, and LAD CTO. After multiple factors were included, a CC diameter < 1 mm, well-developed non-septal collateral, and LAD CTO were still risk factors for GW tracking failure (Table 4). These factors were independent predictors of GW tracking failure in patients undergoing retrograde CTO PCI via poor septal CC.
 |
Table 4 Univariable and Multivariable Analyses for Predictors of GW Tracking Failure in Patients with Poor Septal Collaterals |
Discussion
In this study, we first systematically evaluated the incidence, predictors, and management strategies for retrograde wire tracking failure via poor septal CC. We discovered that the incidence of retrograde GW tracking failure via poor septal CC was 22.1%. A CC diameter < 1 mm, well-developed non-septal collateral, and LAD CTO were independent predictors of GW tracking failure in patients undergoing retrograde CTO PCI via poor septal CC. This is the first study to focus on the predictors and management of retrograde GW tracking via poor septal CC.
Retrograde CTO PCI is the most challenging interventional procedure. During retrograde CTO PCI, the choice of CC and techniques of GW tracking are fundamental for successful PCI. The septal or epicardial CC may be used for retrograde CTO PCI in patients in whom antegrade CTO PCI has failed. Previous studies have shown that septal CC is more effective and safer than epicardial collaterals, with a lower risk of vascular perforation.3 In retrograde CTO PCI, GW tracking success is of vital importance success.8 However, in some specific cases, especially in patients with poor septal CC, the GW tracking routine was unclear, which increased procedural difficulty. Therefore, retrograde GW tracking via poor septal CC remains a challenge for interventional cardiologists. A previous registry study showed that the success rate of GW tracking via CC0 septal collaterals was 84% using the surfing technique; however, the incidence of septal perforation during the procedure was as high as 29%.5 In the present study, the incidence of GW tracking success via poor septal CC was 77.9% (95/122), which is similar to that in a recent study.9
Previous studies have focused on investigating the predictors of technical retrograde CTO PCI success and concluded that septal CC0 was a predictor of technical failure.10 Although a previous study suggested that CC0 was a predictor for the failure of CTO PCI, with the development of procedural techniques and the accumulation of experiences during the past decades, especially with the wide usage of the surfing technique, septal CC0 was not a stumbling block for CTO PCI success. Nonetheless, few studies were performed to explore the possible predictors of GW tracking failure. Prof. Huang suggested that in retrograde CTO PCI, the CC size and tortuosity were independent predictors for both GW CC tracking success and technical success.11 Dr. Dautov suggested that the Werner class does not affect retrograde CC crossing success or GW tracking time during CTO PCI and that Werner CC0 (invisible septal) was often attempted with similar or even faster success rates than the larger CCs.5 A recent study from China suggested that retrograde PCI via CC0 septal collaterals is feasible and safe, and that well-developed non-septal CC and short post descending artery length were independent predictors for GW tracking success via CC0 septal channels.9 Despite these studies, the predictors of retrograde GW crossing failure via poor septal CC remain unclear.
Dr. Wang Y suggested the principle of the choice of septal CC for retrograde GW tracking. They discovered that a larger CC was preferred during retrograde septal CC CTO PCI with a diameter ≥ 0.9 mm (comparable to the internal diameter of the Corsair MC).7 Similarly, the present study found that the incidence of septal CC diameter ≥ 1 mm was significantly lower in the failure group than in the success group. A septal CC diameter < 1 mm was an independent predictor of GW tracking failure in patients undergoing retrograde CTO PCI via poor septal CC. Increasing studies have demonstrated that the tortuosity and length of CC are risk factors for GW tracking failure.5,11–13 However, the tortuosity and length of CC0 collaterals could not be assessed, as they were not visible on CAG. Some physicians have suggested that even though the CC0 septal cannot be seen on CAG, it may usually be straighter.12 Therefore, we speculate that a straighter path is more important than the CC grade in septal CC. In septal CC0 patients, a well-developed epicardial collateral may play a role in reducing myocardial ischemia, which in turn may inhibit the development of septal collaterals. Our results showed that patients in the failure group had a higher incidence of well-developed non-septal collateral. As a suboptimal choice for retrograde CTO PCI, a well-developed non-septal collateral could further improve the success rate of CTO PCI. Further analysis showed that a well-developed non-septal collateral was an independent predictor of GW tracking failure via poor septal CC.
However, retrograde extra backup with a Guidezilla may improve retrograde catheter support, which may in turn improve the success rate of GW tracking.14 However, this study found no correlation between this technique and GW tracking success. Nonetheless, during CTO PCI, especially retrograde CTO PCI, guiding support is of vital importance for both GW and MC tracking success. Therefore, a stronger catheter should be chosen for retrograde CTO PCI, especially in patients with poor CC. The septal collaterals from the right coronary artery (RCA) to the LAD are usually more tortuous and longer than the CC from the LAD to the RCA.7 Meanwhile, the entry of CC is more difficult and the exit angle is smaller during LAD CTO PCI via septal CC, making LAD CTO PCI more complex. Our study revealed that patients in the failure group had a higher incidence of LAD CTO.
Retrograde CTO PCI via septal CC was considered more effective and safer than epicardial collaterals, with a lower risk of vascular perforation.3 A meta-analysis showed that the prevalence of collateral perforation was 6.9% and that of cardiac tamponade was 1.4% during retrograde CTO PCI.15 A previous registry study showed that the incidence of septal perforation was as high as 29% during retrograde CTO PCI via septal CC using the surfing technique.5 However, the majority of patients were minor and asymptomatic. This finding also confirmed that septal CCs are safer than non-septal CCs, which should be used first, even in patients with CC0. The CC and target vessel perforation in this retrospective study were similar to previous studies. The incidence of septal hematoma was much lower than in a previous study, which might have been due to the fact that all the procedures were performed by a well-experienced, high-volume interventional cardiologist.
Based on this study and a previous study, as well as our experiences, the tips for GW tracking via poor septal CC can be summarized as follows: 1) a big profile and strong support catheter; 2) retrograde extra backup with a Guidezilla; 3) the first septal CC usually comes first; 4) Fielder XT-R and Sion Black GW could be used for uncrossable CC; 5) in the case of MC being uncrossable, a small balloon can go through or dilatation with low pressure can be tried, and if MC is still uncrossable, changing the MC may be helpful; and 6) if all attempts still fail, consider retrograde epicardial CC PCI or antegrade PCI again (Figure 4).
 |
Figure 4 Clinical management for GW collateral channel tracking in patients with poor septal collateral circulation. Abbreviations: GW, guide wire; CTO, chronic total occlusion; MC, microcatheter. |
Some tips for GW tracking via poor septal CC are summarized as follows: 1) if a soft-tip hydrophilic polymer-coated GW is preferred, Sion or SUOH03 comes first; 2) rapid rotation of the GW combined with the surfing technique may be helpful; 3) XTR GW may be considered in patients with a small vessel size CC, which may increase the risk of vessel perforation; 4) Sion Black GW was mostly widely used in GW tracking via poor septal CC, which is suitable for tortuous CC; and 5) tip injection may be helpful in some specific patients with a difficult retrograde connection but should not be performed regularly in cases of septal perforation. The final GW crossing the poor septal CC is displayed in Figure 3. The most commonly used GW in this study was Sion Black.
Limitations
First, the included patients were from a single center with a relatively small size, and although they were continuously selected, there was some bias due to the retrospective nature of the study. Second, all the procedures were performed by a well-experienced, high-volume interventional cardiologist, so the results could not be applied to other patients in real-world clinical practice. Third, the J-CTO scores of the study patients were relatively high and were not applicable to all study populations. Despite these limitations, our study suggests predictors and clinical management for these specific patients and may provide the substrate for further studies in this field.
Conclusion
The success rate of retrograde GW tracking via poor septal CC was high, with a relatively high procedural success rate. A CC diameter < 1 mm, well-developed non-septal collateral, and LAD CTO were independent predictors of GW tracking failure in patients who underwent retrograde CTO PCI via poor septal CC.
Abbreviations
CC, collateral channel; CTO, coronary chronic total occlusion; TIMI, thrombolysis in myocardial infarction; GW, Guide wire, MC, microcatheter, CART, controlled antegrade or retrograde subintimal tracking; LVEF, left ventricular ejection fraction.
Data Sharing Statement
The datasets generated and analysed during the current study are not publicly available due to a further study of this area but are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study was approved by the ethics committee of The People’s Hospital of Liaoning Province and all the subjects provided their written informed consent before participation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas. All authors took part in drafting, revising or critically reviewing the article and gave final approval of the version to be published. They have agreed on the journal to which the article has been submitted and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59(11):991–997. doi:10.1016/j.jacc.2011.12.007
2. Noguchi T, Miyazaki MDS, Morii I, et al. Percutaneous transluminal coronary angioplasty of chronic total occlusions. Determinants of primary success and long-term clinical outcome. Catheter Cardiovasc Interv. 2000;49(3):258–264. doi:10.1002/(SICI)1522-726X(200003)49:3<258::AID-CCD7>3.0.CO;2-L
3. Kwon O, Lee PH, Lee SW, et al. Retrograde approach for the percutaneous recanalisation of coronary chronic total occlusions: contribution to clinical practice and long‐term outcomes. EuroIntervention. 2019;15(4):e354–e361. doi:10.4244/EIJ-D-18-00538
4. Zhong X, Ge L, Ma J, et al. Microcatheter collateral channel tracking failure in retrograde percutaneous coronary intervention for chronic total occlusion: incidence, predictors, and management. EuroIntervention. 2019;15(3):e253–e260. doi:10.4244/EIJ-D-18-01003
5. Dautov R, Urena M, Nguyen C, et al. Safety and effectiveness of the surfing technique to cross septal collateral channels during retrograde chronic total occlusion percutaneous coronary intervention. EuroIntervention. 2017;12(15):e1859–e1867. doi:10.4244/EIJ-D-16-00650
6. McEntegart MB, Badar AA, Ahmad FA, et al. The collateral circulation of coronary chronic total occlusions. Eurointervention. 2016;11(14):e1596–1603. doi:10.4244/EIJV11I14A310
7. Wang Y, Zhang XJ, Zhao HW, et al. Incidence, predictors and strategies for failure of retrograde microcatheter tracking after successful wiring of septal collateral channels in chronic total occlusions. Clin Interv Aging. 2020;15:1727–1735. doi:10.2147/CIA.S263216
8. Morino Y, Abe M, Morimoto T, et al. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (multicenter CTO registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011;4(2):213–221. doi:10.1016/j.jcin.2010.09.024
9. Zhang YJ, Ma WR, Xu B, et al. Retrograde percutaneous coronary intervention of chronic total occlusion via discontinuous septal channels. Catheter Cardiovasc Interv. 2023;102(1):64–70. doi:10.1002/ccd.30678
10. Rathore S, Katoh O, Matsuo H, et al. Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv. 2009;2(2):124–132. doi:10.1161/CIRCINTERVENTIONS.108.838862
11. Huang CC, Lee CK, Meng SW, et al. Collateral channel size and tortuosity predict retrograde percutaneous coronary intervention success for chronic total occlusion. Circ Cardiovasc Interv. 2018;11(1):e005124. doi:10.1161/CIRCINTERVENTIONS.117.005124
12. Nagamatsu W, Tsuchikane E, Oikawa Y, et al. Successful guidewire crossing via collateral channel at retrograde percutaneous coronary intervention for chronic total occlusion: the J‐Channel score. EuroIntervention. 2020;15(18):e1624–e1632. doi:10.4244/EIJ-D-18-00993
13. Ioppolo AM, Hovasse T, Benamer H, et al. Angiographic predictors of septal collateral tracking during retrograde percutaneous coronary intervention for chronic total occlusion: anatomical analysis or rolling the dice? J Invasive Cardiol. 2022;34(4):286. PMID: 35366224.
14. Wang Y, Zhang XJ, Zhao HW, et al. Active retrograde extra backup with a mother-and-child catheter to facilitate retrograde microcatheter collateral channel tracking in recanalization of coronary chronic total occlusion. J Interv Cardiol. 2020:4245191. doi:10.1155/2020/4245191
15. El Sabbagh A, Patel VG, Jeroudi OM, et al. Angiographic success and procedural complications in patients undergoing retrograde percutaneous coronary chronic total occlusion interventions: a weighted metal-analysis of 3482 patients from 26 studies. Int J Cardiol. 2014;174(2):243–248. doi:10.1016/j.ijcard.2014.04.004
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
