Back to Journals » Vascular Health and Risk Management » Volume 16
Incidence of Venous Thromboembolism, Risk Factors and Prophylaxis in Hospitalized Patients in the South West Region of Cameroon
Authors Nkoke C, Tchinde Ngueping MJ, Atemkeng F, Teuwafeu D, Boombhi J , Menanga A
Received 19 February 2019
Accepted for publication 13 June 2019
Published 22 July 2020 Volume 2020:16 Pages 317—324
DOI https://doi.org/10.2147/VHRM.S205935
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Pietro Scicchitano
Clovis Nkoke,1 Marius Jordan Tchinde Ngueping,2 Faustin Atemkeng,3 Denis Teuwafeu,2 Jerome Boombhi,4 Alain Menanga4
1Buea Regional Hospital, Department of Internal Medicine, Buea, South West Region, Cameroon; 2University of Buea, Faculty of Health Sciences, Department of Medicine, Buea, South West Region, Cameroon; 3Deido District Hospital, Department of Surgery, Douala, Littoral Region, Cameroon; 4University of Yaounde I, Faculty of Medicine and Biomedical Sciences, Department of Internal Medicine, Yaounde, Center Region, Cameroon
Correspondence: Clovis Nkoke
Buea Regional Hospital, Department of Internal Medicine, Buea, South West Region, Cameroon
Tel +237 677970131
Email [email protected]
Background: Venous thromboembolism (VTE) is a serious complication in hospitalized patients. It is associated with considerable morbidity and mortality. Therefore, its prevention is of great importance. There is paucity of data on the incidence of VTE in hospitalized patients in Cameroon. The aim of this study was to determine the incidence of symptomatic VTE, its risk factors and the proportion of patients at risk that receive thromboprophylaxis in patients hospitalized in the medical and surgical units in two hospitals in the South West Region of Cameroon.
Methods: A prospective study was performed in the medical and surgical units from January to March 2018. All consecutive eligible patients admitted for at least 3 days were included. Patient profile and risk factors were recorded. Patients were followed and evaluated for signs and symptoms of VTE until discharge from hospital. Suspected VTE was confirmed using compression ultrasonography and computed tomography.
Results: A total of 314 patients were included of which 58.7% were females. The mean age was 46± 17.9 years. Patients aged < 40 years represented 42% of the study population. Three cases of symptomatic VTE were recorded. The incidence of symptomatic VTE was 1% (95% CI: 0.3– 2.8%). The prevalence of VTE risk was 93.6% with 32.5% being at high risk. The risk was 94.6% in medical patients and 92.8% in surgical patients. Among the patients at risk, only 32.5% received thromboprophylaxis. Thromboprophylaxis was significantly higher in surgical patients compared to medical patients (45.2% versus 18.7%; p< 0.0001).
Conclusion: The incidence of VTE in hospitalized medical and surgical patients appeared low but likely underestimated considering the high prevalence of patients at risk of VTE coupled with the underutilization of thromboprophylaxis. Clinicians should assess risk of VTE in conjunction with the clinical situation to determine the most appropriate type of prophylaxis as well as the duration of prophylaxis for VTE.
Keywords: venous thromboembolism, incidence, risk factors, prophylaxis, Cameroon
Introduction
Venous thromboembolism (VTE) includes deep vein thrombosis (DVT) and pulmonary embolism (PE). It is a common and potentially preventable cause of morbidity and mortality in hospitalized medical and surgical patients.1 The Center for Disease Control and Prevention (CDC) in a 3-year study reported an annual incidence of 547,596 cases of VTE in the hospitalized adult population.2 A recent systematic review on VTE in Africa revealed a prevalence of DVT following surgery to range from 2.4% to 9.6%. Similarly, the prevalence of pulmonary embolism varied between 0.14% and 61.5%.3 A recent study conducted in an urban medical center in Cameroon highlighted an in-hospital prevalence of 4.4 per 1000 admissions and a mortality of 10%.4
Pulmonary embolism is regarded as the most common cause of hospital preventable deaths, accounting for 10–30% of hospital deaths.5,6 The incidence of VTE rises during hospitalization as a result of an increase in risk factors. Reports show that about 78% of hospitalized patients have more than one risk factor for VTE and about 20% of patients have more than three risk factors.7 Studies reported fractures (pelvic or lower limb), hip or knee replacement, major general surgery, major trauma, spinal cord injury, immobilization, intensive care unit (ICU) admission, chronic pulmonary disease, obesity and chronic heart failure to be the most frequent VTE risk factors found in hospitalized patients.8–11 The absence of proper VTE prophylaxis in hospitalized patients leads to 10–80% cases of VTE with mortality of 30–40% and 0.2–0.9% secondary to DVT and PE, respectively.1,12 In the multinational ENDORSE study, 51.8% of surgical patients were at risk of VTE while 41.5% of medical patients were at risk. Of the surgical patients at risk, 58.5% received VTE prophylaxis while 39.5% at-risk medical patients received prophylaxis.13 Available evidence shows that primary thromboprophylaxis reduces the risk of DVT and PE. Despite its proven efficacy, VTE prophylaxis remains underutilized in medical and surgical patients.14,15
Due to the generally non-specific presentation of VTE and of its potentially rapid mortality, the identification of its risk factors and the use of prophylaxis remain the key methods to address the problem. There is paucity of data concerning the incidence of VTE, its risk factors and use of thromboprophylaxis in hospitalized patients in Cameroon. The aim of this study was to study the incidence of VTE, its risk factors and prophylaxis practice in hospitalized medical and surgical patients in the South West Region of Cameroon.
Methods
Study Design and Setting
It was a prospective study. The study was carried out in the medical and surgical units of the Buea and Limbe Regional Hospitals in the South West Region of Cameroon. These two hospitals are referral hospitals in the South West Region.
Study Population
All consecutive patients of age ≥18 years admitted in the medical and surgical units were included between January and March 2018. Patients had to be admitted for at least 3 days to be eligible. We excluded patients who were admitted for the management of VTE, those with incomplete medical records (such as medical charts not containing information concerning duration of surgeries or treatment received by the patient or medical history of the patients) and those on long-term anticoagulation.
Data Collection
At the time of admission, all consecutive eligible patients were approached to participate in the study. Written informed consent was obtained from all participants. At day 3 of admission, all participants were interviewed using a structured questionnaire and the medical records were reviewed extensively. The data collected included socio-demographic data, weight, height, clinical characteristics of the participants, diagnosis that led to admission, risk factors for VTE, VTE prophylaxis received, reasons of non-prophylaxis, and contraindication to anticoagulant prophylaxis. The Caprini score was calculated for each participant and classified as being at very low, low, moderate, and high using the modified Caprini risk assessment model.16 Patients were evaluated for signs and symptoms of VTE during their stay in hospital until hospital discharge. All clinically suspected cases of DVT or PE led to the relevant diagnostic testing for confirmation. These were all symptomatic cases of VTE. The diagnosis of DVT was made using compression ultrasonography and the diagnosis of PE was made using computed tomography.
Ethical Consideration
To precede data collection, an ethical approval was obtained from the institutional review board of the Faculty of Health Sciences of the university of Buea (IRBFHS, no: 2018/143/UB/SG/IRB/FHS), and then administrative approvals from hospital authorities. Written informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki.
Statistical Analysis
The data collected were analyzed using Epi-info software version 7.2. Frequencies and percentages were computed for categorical variables. Continuous variables were expressed as mean ± standard deviation or median (interquartile range) where necessary. Comparison of variables was done using the chi-square test. The proportion of hospitalized patients at risk of VTE was evaluated as the number of patients at risk of VTE on the total number of patients included in our study. To determine the proportion of at-risk patients who received thromboprophylaxis, we divided the number of at-risk patients who received thromboprophylaxis on the total number of at-risk patients. Incidence of VTE, defined as the frequency of venous thromboembolic events among evaluable patients, was calculated with 95% confidence interval (CI). p<0.05 was considered statistically significant.
Results
Socio-Demographic Characteristics
During the study period, 314 patients from the medical and surgical units of the Buea Regional Hospital (BRH) and Limbe Regional Hospital (LRH) were enrolled (Figure 1). Patients aged ≤40 years represented 42% of our study population. The mean age of participants was 46 ± 17.9 years. Out of the 314 patients enrolled 58.7% were females (Table 1). The median length of hospital stay at the time of the survey was 5 (IQR 4–8) days.
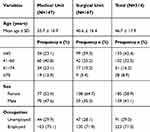 |
Table 1 Socio-Demographic Characteristics |
 |
Figure 1 Flow chart of patient recruitment. |
Incidence of Venous Thromboembolism During Admission
During follow-up in the hospital, 3 patients developed VTE, 2 from the surgical unit and 1 from the medical unit. Two patients had symptomatic DVT confirmed by compression ultrasonography and one had PE confirmed by computed tomography. The incidence of symptomatic VTE during admission was 1% (95% CI: 0.3–2.8%). The 3 subjects that developed symptomatic VTE were at high risk and none was on thromboprophylaxis. The 2 patients from the surgical unit had major trauma with immobilization. One had a pelvic fracture and the other had a leg fracture. The subject from the medical unit had stroke with paralysis and immobilization. The PE was nonfatal.
Risk Factors for Venous Thromboembolism
The frequent reasons for admission in the medical unit included neurological diseases (35.4%), infectious disease (29.3%), and cardiovascular diseases (19.7%) (Table 2). In the surgical unit, the main reasons for hospitalization were major surgeries (41.9%), orthopaedic trauma (16.8%), and other surgical conditions (16.8%) (Table 3).
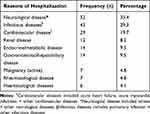 |
Table 2 Reasons for Admission in the Medical Unit (N=147) |
 |
Table 3 Reasons for Admission to the Surgical Unit (N=167) |
Assessment of VTE risk factors before admission showed that: age >40 years (57.6%), long-term immobility (23.9%), and swollen legs (21.9%) were predominant (Table 4) and during hospitalization: immobility with bathroom privileges (31.5%), bed confinement (29.9%), and complete immobilization (8.3%) were the most common ones (Table 5). In female patients (n=185), the most common risk factors were pregnancy/postpartum 22.2% followed by oral contraceptive use at 5.4%. Of the 314 participants, 294 were classified at risk according to the Caprini score, giving an overall prevalence of 93.6%. The risk was 94.6% in surgical patients and 92.8% in medical patients. Using the Caprini score, 32.5%, 37.6%, 23.6% and 6.4% of the subjects were at high, moderate, low and very low risk, respectively.
 |
Table 4 Risk Factors of VTE Among Patients on Admission |
 |
Table 5 Risk Factors of VTE Among Patients After Admission |
Thromboprophylaxis in At-Risk Patients
Of the 294 patients deemed at risk, 32.7% (n=96) received thromboprophylaxis (Table 6). Only 37.3% of patients at high risk received VTE prophylaxis. And, 35.6% of moderate-risk patients and 16.2% patients received VTE. No patient in the low-risk group received VTE prophylaxis. There was significant difference in the utilization of thromboprophylaxis between surgical and medical patients with surgical receiving more (45.2% versus 18.7%, p<0.0001). Pharmacological prophylaxis was the most frequently used VTE prophylaxis with low-molecular-weight heparin (LMWH) being the most prescribed anticoagulant. Early and frequent ambulation was the only prescribed non-pharmacological method. No mechanical means of VTE prevention was prescribed. Of the patients deemed at risk, 10.2% (n=30) of patients had contraindications to anticoagulation prophylaxis. Intracranial haemorrhage 3.4% (n=10) and bleeding at hospital admission 3.1% (n=9) were the most prevailing contraindications to anticoagulation (Table 7). There was no incident bleeding in patients on anticoagulant prophylaxis.
 |
Table 6 Thromboprophylaxis Coverage in the At-Risk Patients |
 |
Table 7 Contraindications to Anticoagulant Prophylaxis |
Discussion
The aims of this study were to determine the incidence of symptomatic venous thromboembolism (VTE), its risk factors and the proportion of patients at risk that receive thromboprophylaxis in two hospitals in the South West Region of Cameroon. The findings show that the incidence of symptomatic VTE was 1%. There was high prevalence of patients at risk for VTE. Medical and surgical patients were at comparable risk. Only 32.7% of patients at risk received thromboprophylaxis. Thromboprophylaxis was significantly higher in surgical patients compared to medical patients. This is the first study reporting on the incidence of symptomatic VTE in hospitalized patients in Cameroon. The screening for VTE was not systematic. There were no investigations performed routinely to detect VTE. The incidence might have been higher but only patients with signs and symptoms of VTE were tested. Also, patients were not followed up after hospital discharge even though the risk of VTE can persist several weeks after discharge. In a systematic screening for VTE in a psychiatric unit, Delluc et al reported an incidence of VTE of 2.2% at day 10 of admission which was twice that reported in our study.17 Previous studies reported that VTE risk persists up to 90 days after surgery and beyond hospital stay.18,19 Studies have shown that a significant proportion of VTE occur after medical discharge.17 In one report in a psychiatric unit, the incidence of VTE disease increased from 2.2% to 3.5% at 90 days after discharge.17 The majority of patients in our study were at risk of VTE but there was no follow up after discharge. Thus, it is possible that some patients might have developed VTE after discharge which went undiagnosed or were readmitted for VTE. In our study, the prevalence of patients at risk for VTE was 93.6%. This prevalence was almost twice that reported by Cohen et al in the ENDORSE study where the prevalence of at-risk patients was 51.8%.13 It was also higher than that reported in Sub-Saharan Africa by Kingue et al who had a prevalence of 50.4%.11 Our enrollment criteria were slightly different from those of these previous studies where the age more than 40 years was a criterion for enrollment in the medical ward and patients aged more than 18 years and admitted for major surgeries was that for the surgical ward. In our study, medical patients were at higher risk compared to surgical patients though the difference was not significant. This was in accordance with the findings of Kingue et al.11 Despite the high prevalence of VTE disease risk, only 32.7% of at-risk patients received thromboprophylaxis. This was lower than that reported by Kingue et al with 51.1% of at-risk patients receiving prophylaxis.11 This difference can be explained by difference in the study setting as our study was carried out in a semi-urban setting. The use of thromboprophylaxis in our study was higher among surgical patients compared to medical patients. This was a similar finding in previous studies.20,21 In the ENDORSE study, 58.5% of at-risk surgical patients received recommended prophylaxis while 39.5% of at-risk medical patients received prophylaxis compared to 45.2% of at-risk surgical patients and 18.7% of at-risk surgical patients in our study.13 Surgery is a well-established VTE risk factor and the use of thromboprophylaxis is generally higher amongst surgical patients than medically ill patients.13 Generally, thromboprophylaxis is suboptimal as shown by numerous studies.13,15,22,23 There are numerous reasons that could explain this suboptimal utilization of thromboprophylaxis in our setting including physician awareness, availability of guidelines, education factors, reimbursement, and national healthcare resources. International guidelines recommend calculating the risk of VTE development and the bleeding risk before starting VTE prophylaxis on both surgical and non-surgical patients.16,24
Limitations
The main limitation in our study is due to the fact that patients were not followed up after discharge given that the risk of VTE persists after hospital discharge and studies have shown that a significant proportion of VTE occur post hospitalization. Also, there were no investigations performed routinely to detect asymptomatic VTE. Despite this limitation, this study is the first to report on the incidence of VTE amongst hospitalized patients in our setting and to assess VTE risk factors and prophylaxis out of the two major cities of Cameroon which are Douala and Yaounde.
Conclusion
This study showed that the incidence of symptomatic venous thromboembolism in hospitalized medical and surgical patients was 1%. The prevalence of patients at risk for VTE was very high with only a small proportion of at-risk patients receiving recommended prophylaxis. In case of contraindication, no thromboprophylaxis was given at all. Therefore, graded compression stockings and intermittent pneumatic compression as alternative treatment modalities deserve more attention and should be used as there is enough evidence for their beneficial use.
Abbreviations
DVT, deep venous thrombosis; PE, pulmonary embolism; VTE, venous thromboembolism.
Data Sharing Statement
Data are available from the authors upon reasonable request.
Ethics Approval and Consent to Participate
The protocol was approved by the Institutional Review Board of the University of Buea and the administrative authorities of the hospitals.
Acknowledgments
We thank all the patients who accepted to participate in this study.
Author Contributions
All authors contributed towards data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no funding and no conflicts of interest in this work.
References
1. Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines (8th edition). Chest. 2008;133:381S–453S. doi:10.1378/chest.08-0656
2. Yusuf HR, Tsai J, Atrash HK, Boulet S, Grosse SD. Venous thromboembolism in adult hospitalizations –United States, 2007–2009. MMWR. 2012;61:401–404.
3. Danwang C, Temgoua MN, Agbor VN, Tankeu AT, Noubiap JJ. Epidemiology of venous thromboembolism in Africa: a systematic review. J Thromb Haemost. 2017;15:1770–1781. doi:10.1111/jth.13769
4. Kamdem F, Ngahane BHM, Hamadou B, et al. Epidemiology, clinical presentations and in-hospital mortality of venous thromboembolism at the douala general hospital: a cross-sectional study in Cameroon, Sub-Saharan Africa. World J Cardiovasc Dis. 2018;08:123–132. doi:10.4236/wjcd.2018.82012
5. Beckman MG, Hooper WC, Critchley SE, et al. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38(4):S495–501. doi:10.1016/j.amepre.2009.12.017
6. Baglin TP, White K, Charles A. Fatal pulmonary embolism in hospitalised medical patients. J Clin Pathol. 1997;50:609–610. doi:10.1136/jcp.50.7.609
7. Anderson F. The prevalence of risk factors for venous thromboembolism among hospital patients. Arch Intern Med. 1992;152(8):1660. doi:10.1001/archinte.1992.00400200092017
8. Anderson FA. Risk factors for venous thromboembolism. Circulation. 2003;107:9–16. doi:10.1161/01.CIR.0000078469.07362.E6
9. Hadi AG, sherif S, Alaa M, Mounir AR, George S. Venous thromboembolism risk and prophylaxis in the acute hospital care setting: report from the ENDORSE study in Egypt. Thromb J. 2012;10:20. doi:10.1186/1477-9560-10-20
10. Bâ SA, Badiane S, Diop SN, et al. A cross-sectional evaluation of venous thromboembolism risk and use of venous thromboembolism prophylaxis in hospitalized patients in Senegal. Arch Cardiovasc Dis. 2011;104:493–501. doi:10.1016/j.acvd.2011.05.007
11. Kingue S, Bakilo L, Ze Minkande J, et al. Epidemiological African day for evaluation of patients at risk of venous thrombosis in acute hospital care settings: cardiovascular topic. Cardiovasc J Afr. 2014;25:159–164. doi:10.5830/CVJA-2014-025
12. Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism. Chest. 2004;126:338S–400S. doi:10.1378/chest.126.3_suppl.338S
13. Cohen AT, Tapson VF, Bergmann JF, et al. ENDORSE investigators. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet. 2008;371(9610):387–394. doi:10.1016/S0140-6736(08)60202-0
14. Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in medical patients with enoxaparin study group. N Engl J Med. 1999;341:793–800. doi:10.1056/NEJM199909093411103
15. Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the international medical prevention registry on venous thromboembolism. Chest. 2007;132:936–945. doi:10.1378/chest.06-2993
16. Gould MK, Garcia DA, Wren SM, et al. Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practical guidelines. Chest. 2012;141:e227S. doi:10.1378/chest.11-2297
17. Delluc A, Montavon S, Canceil O, et al. Incidence of venous thromboembolism in psychiatric units. Thromb Res. 2012;130(6):e283–8. doi:10.1016/j.thromres.2012.10.002
18. White RH, Zhou H, Romano PS. Incidence of symptomatic venous thromboembolism after different elective or urgent surgical procedures. Thromb Haemost. 2003;90:446–455. doi:10.1160/TH03-03-0152
19. Sweetland S, Green J, Liu B, et al. Duration and magnitude of the postoperative risk of venous thromboembolism in middle aged women: prospective cohort study. BMJ. 2009;339:b4583. doi:10.1136/bmj.b4583
20. Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated heparin or low-molecular weight heparins: a meta-analysis of randomized clinical trials. Thromb Haemost. 2000;83:14–19. doi:10.1055/s-0037-1613749
21. Kakkar AK, Davidson BL, Haas SK, et al. Compliance with recommended prophylaxis for venous thromboembolism: improving the use and rate of uptake of clinical practice guidelines. J Thromb Haemost. 2004;2:221–227. doi:10.1111/j.1538-7933.2004.00588.x
22. Rashid ST, Thursz MR, Razvi NA, et al. Venous thromboprophylaxis in UK medical inpatients. J R Soc Med. 2005;98(11):507–512. doi:10.1177/014107680509801112
23. Rocha AT, Braga P, Ritt G, Lopes AA. Inadequacy of thromboprophylaxis in hospitalized medical patients. Rev Assoc Med Bras. 2006;52(6):441–446. doi:10.1590/S0104-42302006000600026
24. Falck-Ytter Y, Francis CW, Johanson NA, et al. Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141:e278. doi:10.1378/chest.11-2404
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
