Back to Journals » Clinical Interventions in Aging » Volume 17
Incidence and Risk Factors of Mortality in Nonagenarians and Centenarians After Intertrochanteric Fracture: 2-Year Follow-Up
Authors Wang T, Guo J, Long Y, Hou Z
Received 26 January 2022
Accepted for publication 27 March 2022
Published 5 April 2022 Volume 2022:17 Pages 369—381
DOI https://doi.org/10.2147/CIA.S360037
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Tao Wang,1,2,* Junfei Guo,1,2,* Yubin Long,1,2 Zhiyong Hou1– 3
1Department of Orthopaedic Surgery, Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China; 2Orthopaedic Research Institute of Hebei Province, Shijiazhuang, Hebei, People’s Republic of China; 3NHC Key Laboratory of Intelligent Orthopaedic Equipment (Third Hospital of Hebei Medical University), Shijiazhuang, Hebei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhiyong Hou, Department of Orthopaedic Surgery, Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China, Email [email protected]
Purpose: The purpose of this study was to explore risk factors for mortality after intertrochanteric fracture (IF) surgery in nonagenarians and centenarians based on subgroups of follow-up time.
Patients and Methods: A total of 144 nonagenarians and centenarians who underwent IF surgery between Jan. 2014 and Dec. 2018 were included. Data were compared between the mortality and the survival groups based on the subgroups of follow-up time in univariate, logistic regression, and Cox regression analyses.
Results: In our study, the rates of mortality were 7.6%, 13.9%, and 28.5% at 6-month, 1-year, and 2-year follow-up, respectively. Univariate analysis showed that prolonged time from injury to surgery, more transfusion volume, lower hemoglobin (minimum), and complications (respiratory failure and anemia) were associated with mortality at 6-month follow-up. However, three factors were found to be related to mortality at 1-year and 2-year follow-up, respectively. Our results showed that postoperative respiratory failure and anemia were independent risk factors for mortality after IF surgery at 6-month in logistic regression analysis. However, postoperative respiratory failure was found as an independent risk factor for mortality at 1-year and 2-year follow-up. Moreover, Cox regression analysis showed that postoperative respiratory failure was an independent risk factor for mortality after IF surgery, which was consistent with results in logistic regression analysis.
Conclusion: Postoperative respiratory failure was an independent risk factor for mortality in nonagenarians and centenarians at any follow-up. Additionally, postoperative anemia was closely related to mortality. Preoperative measures should be taken to lower mortality.
Keywords: nonagenarians and centenarians, mortality, intertrochanteric fracture, risk factors
Introduction
With the advancement of living standards and medical care, the number of nonagenarians, and even centenarians, is growing substantially, particularly in developed areas. Kontis1 estimated that national female life expectancy will exceed the 90-year barrier by 2030.1 Epidemiological research2 found that hip fractures, including femoral neck fractures and intertrochanteric fractures (IF), accounted for nearly one-third of all fractures in over 500,000 individuals over the age of 65. Without a doubt, the risk of hip fracture rises with age. Regarding nonagenarians and centenarians, some publications3,4 revealed 40% of the rates for in-hospital complications and death rates ranging from 35.5% to 60% in the first year, posing a significant cost on people and society. Kim5 discovered that greater ASA and longer time intervals between trauma and surgery were risk factors for death in nonagenarians with hip fractures.
A few studies have concentrated on nonagenarians and centenarians with hip fractures. We concluded after reviewing related articles on patients older than 90 years old that most articles only reported the rate of mortality and failed to evaluate risk factors due to small numbers of patients, or that some focused on comparisons between nonagenarians or centenarians and other stages of age, such as octogenarians. As a result, we conducted this study to investigate the risks of mortality in nonagenarians and centenarians following IF based on a subgroup of follow-up time.
Patients and Methods
Ethics Statement
The study was approved by the Institutional Review Board of the third hospital of Hebei Medical University (K2020-032-1) before data collection and analysis.
Patients
We included 144 patients who underwent IF surgery between Jan. 2014 and Dec. 2018 in our hospital. According to the time of follow-up, these patients were divided into mortality and survival groups. The inclusion criteria for this study were as follows: 1) patients who underwent IF surgery; 2) patients who were no younger than 90 years old; and 3) no comorbidity was present at the time of admission. The exclusion criteria were as follows: 1) patients with a history of IF; 2) patients who have had hip surgery; 3) multiple fractures or injuries; and 4) open intertrochanteric fractures. Possible factors were collected, including baseline factors-age, sex, time from injury to hospital, body mass index (BMI), hemoglobin (admission, leave the hospital, minimum), type of fracture, ASA classification, time from injury to surgery, hospital stay, vein thrombosis (admission); surgical factors-transfusion (yes or no), blood transfusion volume, operation time, blood loss, general anesthesia (yes or no); Comorbidities: a history of electrolyte disturbance, anemia, dementia, lung disease, arteriosclerosis, cerebrovascular disease, hypoproteinemia, arrhythmia, heart failure, diabetes, cerebral infarction, coronary heart disease, and hypertension; complications – heart failure, respiratory failure, cerebral infarction, stress ulcer, arrhythmia, lung infection, delirium, anemia, vein thrombosis, electrolyte disturbance, hypoproteinemia, and high blood sugar. The standard for anemia is less than 120 g/L for males and less than 110 g/L for females. Blood tests were routinely conducted at admission, before and 1, 3, 5 days after surgery, and before discharge.
The methods were carried out following the approved guidelines. Two authors identified and collected all the data of patients according to inclusion and exclusion criteria. In addition, two authors were responsible for data analysis. When data met normality criteria with p > 0.05, all measurement data were presented as the mean SD (standard deviation). If the data did not meet the criteria for normality and variance homogeneity, the rank-sum test was used to perform statistical analysis between groups. For count data, the chi-square test was used for data analysis. Statistical significance levels were considered to be p<0.05. To identify the best predictors of mortality, univariate, logistic regression, and Cox regression analyses were computed based on subgroups of follow-up time using SPSS, version 21.0 (SPSS Inc., Chicago, IL).
Results
In our study, the occurrence of mortality in nonagenarians and centenarians after IF was 7.6%, 13.9%, and 28.5% at 6-month, 1-year, and 2-year follow-up, respectively. As shown in Table 1, a longer time from injury to surgery, more blood transfusion volume, and lower levels of hemoglobin (minimum) were found in the mortality group than in the survival group at 6-month follow-up. We also found that patients with complications such as respiratory failure and anemia were associated with mortality at 6-month (Table 1). Our findings showed that longer time from injury to surgery, postoperative respiratory failure, and anemia were associated with mortality at 1-year follow-up in Table 2. Additionally, Table 3 shows that lower BMI, longer time from injury to surgery, and postoperative respiratory failure were related to mortality at 2-year follow-up.
 |  | 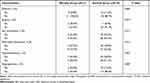 |
Table 1 Comparison of Possible Factors Associated with Mortality in 6-Month Follow-Up Between Two Groups |
 |  |  |
Table 2 Comparison of Possible Factors Associated with Mortality in 1-Year Follow-Up Between Two Groups |
 |  |  |
Table 3 Comparison of Possible Factors Associated with Mortality in 2-Year Follow-Up Between Two Groups |
Cox regression analysis showed that respiratory failure after surgery (p=0.001, HR=5.026, 95% CI [1.969, 12.833]) was a risk factor of mortality after IF surgery. Postoperative respiratory failure was found as an independent risk factor of of mortality after IF surgery at 6-month follow-up (p=0.004, OR=18.010, 95% CI [2.575, 125.956]), 1-year follow-up (p=0.024, OR=10.336, 95% CI [1.367, 78.167]), and 2-year follow-up (p=0.011, OR=12.815, 95% CI [1.809, 90.782]) in the logistic regression analysis, as shown in Table 4. Postoperative anemia (p=0.023, OR=5.872, 95% CI [1.277, 26.989]) was a risk factor of mortality after IF surgery at 6-month follow-up, as shown in Table 4.
 |
Table 4 Logistic Regression in Mortality Based on Subgroup of Follow-Up Time |
Discussion
According to Cooper,6 6.26 million individuals will suffer from hip fractures globally by 2050, with a sharp increase in Asian nations. Families and societies will bear a significant burden as a result of hip fractures in rapidly aging populations, particularly nonagenarians and centenarians. As far as we know, little research on mortality following hip fracture in China has been published. Chang7 conducted a meta-analysis and discovered that malignancy, nursing home residency, duration to surgery (>2 days), pulmonary illness, diabetes, and cardiovascular disease were all associated with an increased risk of death following hip fracture surgery in elderly patients. While Kim5 did a retrospective analysis in nonagenarians with hip fractures and concluded that the mortality rates at 1-year and 2-year follow-up were 23.4% and 40.6%, respectively. Meanwhile, at the most recent follow-up, he established that high ASA and duration from trauma to operation were substantial risk factors for mortality. According to Barceló,8 the number of comorbidities is a risk factor for death in nonagenarians and centenarians.
Recently, a few papers have focused on the risk factors for mortality in nonagenarians and centenarians with hip fracture, a contentious subject. As a result, we collected data from 144 patients to investigate the risk variables for mortality after IF surgery using univariate, logistic regression analysis, and Cox regression analysis. It is the first study to assess risk factors for mortality in nonagenarians and centenarians following IF surgery based on a subgroup of follow-up time in China.
The results of Kim5 from South Korea showed 23.4% and 40.6% mortality rates in nonagenarians with hip fractures at 1-year and 2-year follow-up. In Taiwan, China, the mortality rates were 20.3% at 6 months, 29.5% at 1 year, and 45.0% at 2 years after surgery in nonagenarians with hip fractures.9 In our study, the mortality rates were 7.6%, 13.9%, and 28.5% at 6-month, 1-year, and 2-year follow-up, respectively, which was lower than the consequences of previous studies.5,9 Two possible reasons may explain the difference in the mortality rate between this study and previous studies. First, it might be related to different demographics, including age, distribution of gender, and comorbidity in each study. Second, our institution, based on a collaborative multidisciplinary team care model, has specialist geriatric wards in the management of older trauma and orthopedic patients who are over 75 years old. Professional physicians provide professional treatment for internal medical diseases of the elderly before and after surgery to minimize postoperative complications and allow the elderly to recover more quickly, which has greatly contributed to lowering post-discharge mortality.
Recently, the role of comorbidity as a factor associated with the risk of mortality has been controversial.10 Kim5 believed that an ASA grade related to a patient’s comorbidity was considered a risk for mortality. The data of our study indicated that anemia was a risk for mortality at 1-year after surgery, which was related to an important measure that systematically prevented and cured internal diseases by our physicians before the operation. The mean number of complications was found to be a risk factor for mortality in the study by Barceló.8 Although just 6 of 144 patients suffering from postoperative respiratory failure, whether in univariate, logistic regression, or Cox regression analysis, respiratory failure, as a rare and serious complication, was identified as an important risk factor for mortality at any time of follow-up in our study. With regard to patients over the age of 90 years, IF was the first burden and surgery was the second burden for their physical condition, which made it easy to induce a mortal disease like respiratory failure to influence mortality at follow-up.
Regarding time from injury to surgery, Chang7 performed a meta-analysis and indicated that a delay of >2 days significantly increased the mortality rate. Meng11 obtained the same results as Chang and recommended that orthopedic surgery should be performed within 1 or 2 days after injury. On the contrary, other studies12,13 demonstrated that surgery delay was not more important in influencing mortality compared to other factors such as medical conditions, age, and sex. However, our findings showed that time from injury to surgery was markedly longer in the mortality group than in the survival group by univariate analysis, but not an independent risk of mortality in logistic regression and Cox regression analyses. Furthermore, no significant difference was found at any follow-up between the three subgroups (2 vs 2–5 vs >5 days). In our opinion, it should be dialectically treated. First, a surgical delay is easy to cause inflammation, which in turn increases mortality. Second, early surgery may not obtain good outcomes for patients because the fracture is the first burden and surgery is the second one for the physical condition of patients, especially nonagenarians and centenarians. A short interval between the two burdens (fracture and surgery) may lead to fatal diseases such as cerebrovascular diseases due to excessive blood loss. Third, we infer that an optimum surgical interval not only provides a buffer between the two burdens for patients but also regulates the comorbidity. Future studies will find a lower mortality rate.
Ryan14 reviewed data of 34,805 patients with hip fracture and demonstrated that anemia at presentation, causing hypoperfusion, which was closely related to cardiocerebral diseases, was independently associated with higher rates of 30-day postoperative mortality in old patients. However, Mantilla15 found the opposite conclusion, that preoperative anemia was not an independent risk factor for death, which was the same as our findings. There were 15 out of 144 preoperative anemia patients who all received transfusions during surgery, and only one patient died 3 months after surgery. Surprisingly, postoperative anemia was found to be related to 6-month mortality, and the minimum level of hemoglobin during hospital stay was significantly lower in the mortality group than in the survival group at 6-month follow-up. The level of hemoglobin should be monitored in the same way, whether it is before or after surgery. Additionally, a marked difference was found in blood transfusion volume between the two groups in short-term follow-up. It is well established that allogenic blood transfusions can cause clinically significant immunosuppression in recipients, increasing the risk of infections, organ dysfunction, and even death.16 More blood transfusion volume means a higher rate of mortality.17,18
Limitations
Although this study provides several novel findings, it has some limitations. This was a retrospective, single-center study. A large sample, multicenter, randomized controlled study was needed. Secondly, another factor such as the Charlson comorbidity index that might influence mortality was not fully included due to retrospective studies’ limitations. Finally, although four doctors conducted the operations, they were all surgeons who have worked in orthopedic surgery for more than 10 years with good surgical skills and experience.
Conclusions
Respiratory failure after surgery was an independent risk factor for mortality in nonagenarians and centenarians at any follow-up. Additionally, postoperative anemia was associated with an increased risk of mortality in nonagenarians and centenarians at short follow-up. This article aimed to share some experience with surgeons and suggests that preoperative measures should be taken to lower the incidence of mortality in nonagenarians and centenarians with IF surgery.
Abbreviations
IF, intertrochanteric fracture; BMI, body mass index; ASA, American Society of Anesthesiologists.
Data Sharing Statement
The dataset generated and/or analyzed during the current study is not publicly available due to patient-related confidentiality, but it is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the institutional review board of the third Hospital of Hebei Medical University (K2020-032-1) in compliance with the Declaration of Helsinki and consent was waived for this non-interventional, observational, and retrospective study, in which the patient data used were kept strictly confidential.
Funding
The study was financially supported by the National Key R&D Program of China (No. 2019YFC0120600), the 2019 Hebei Provincial Department of Finance Geriatric Disease Prevention and Control Funds, and Baoding City Science and Technology and Intellectual Property Bureau (No. 2041ZF260).
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
1. Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389(10076):1323e35. doi:10.1016/S0140-6736(16)32381-9
2. Zhang Y. Clinical Epidemiology of Orthopedic Trauma. Stuggart: Thieme; 2016.
3. Tarity D, Smith EB, Dolan K, Rasouli MR, Maltenfort MG. Mortality in centenarians with hip fractures. Orthopedics. 2013;36:e282–87. doi:10.3928/01477447-20130222-15
4. Warner MA, Saletel RA, Schroeder DR, Warner DO, Offord KP, Gray DT. Outcomes of anesthesia and surgery in people 100 years of age and older. JAGS. 1998;46:988–993. doi:10.1111/j.1532-5415.1998.tb02754.x
5. Kim JW, Kim DH, Jang EC, Lee YK, Koo KH, Ha YC. Mortality and its risk factors in nonagenarians after hip fractures. J Orthop Sci. 2019;24(5):850–854. doi:10.1016/j.jos.2019.02.019
6. Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2(6):285–289. doi:10.1007/BF01623184
7. Chang W, Lv H, Feng C, et al. Preventable risk factors of mortality after hip fracture surgery: systematic review and meta-analysis. Int J Surg. 2018;52:320–328. doi:10.1016/j.ijsu.2018.02.061
8. Barceló M, Francia E, Romero C, Ruiz D, Casademont J, Torres OH. Hip fractures in the oldest old. Comparative study of centenarians and nonagenarians and mortality risk factors. Injury. 2018;49(12):2198–2202. doi:10.1016/j.injury.2018.09.043
9. Lin JC, Liang WM. Mortality, readmission, and reoperation after hip fracture in nonagenarians. BMC Musculoskelet Disord. 2017;18(1):144. doi:10.1186/s12891-017-1493-5
10. Mazzucchelli Esteban R, Pérez-Fernández E, Crespí-Villarías N, et al. Trends in osteoporotic hip fracture epidemiology over a 17-year period in a Spanish population: Alcorcón 1999–2015. Arch Osteoporos. 2017;12(1):84. doi:10.1007/s11657-017-0376-6
11. Meng D, Bai X, Wu H, et al. Patient and perioperative factors influencing the functional outcomes and mortality in elderly hip fractures. J Invest Surg. 2021;34(3):262–269. doi:10.1080/08941939.2019.1625985
12. Sebestyen A, Boncz I, Sandor J, Nyarady J. Effect of surgical delay on early mortality in patients with femoral neck fracture. Int Orthop. 2008;32:375–379. doi:10.1007/s00264-007-0331-z
13. Smektala R, Endres HG, Dasch B, Maier C, Trampisch HJ, Bonnaire F. The effect of time-to-surgery on outcome in elderly patients with proximal femoral fractures. BMC Musculoskelet Disord. 2008;9:171. doi:10.1186/1471-2474-9-171
14. Ryan G, Nowak L, Melo L, et al. Anemia at presentation predicts acute mortality and need for readmission following geriatric hip fracture. JB JS Open Access. 2020;5(3):
15. Mantilla CB, Wass CT, Goodrich KA, et al. Risk for perioperative myocardial infarction and mortality in patients undergoing hip or knee arthroplasty: the role of anemia. Transfusion. 2011;51(1):82–91. doi:10.1111/j.1537-2995.2010.02797.x
16. Gupta P, Kang KK, Pasternack JB, Klein E, Feierman DE. Perioperative transfusion associated with increased morbidity and mortality in geriatric patients undergoing hip fracture surgery. Geriatr Orthop Surg Rehabil. 2021;12:21514593211015118. doi:10.1177/21514593211015118
17. Diaz-Martin A, Escoresca-Ortega AM, Hernandez-Caballero C, et al. Considerations regarding major bleeding after cardiac transplantation. Transplant Proc. 2010;42:3204–3205. doi:10.1016/j.transproceed.2010.05.047
18. Turan A, Yang D, Bonilla A, et al. Morbidity and mortality after massive transfusion in patients undergoing non-cardiac surgery. Can J Anaesth. 2013;60:761–770. doi:10.1007/s12630-013-9937-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
