Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 15
Incidence and Predictors of an Abnormal Liver Function Test Among 674 Systemic Sclerosis Patients: A Cohort Study
Authors Sawadpanich K, Promasen P, Mairiang P, Sukeepaisarnjareon W, Sangchan A, Suttichaimongkol T, Tangvoraphonkchai K, Foocharoen C
Received 9 March 2023
Accepted for publication 2 May 2023
Published 16 May 2023 Volume 2023:15 Pages 81—92
DOI https://doi.org/10.2147/OARRR.S410165
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Chuan-Ju Liu
Kookwan Sawadpanich,1 Palinee Promasen,1 Pisaln Mairiang,1 Wattana Sukeepaisarnjareon,1 Apichat Sangchan,1 Tanita Suttichaimongkol,1 Kawin Tangvoraphonkchai,1 Chingching Foocharoen2
1Division of Gastroenterology and Hepatology, Department of Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, 40002, Thailand; 2Division of Rheumatology, Department of Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, 40002, Thailand
Correspondence: Chingching Foocharoen, Division of Rheumatology, Department of Medicine, Faculty of Medicine, Khon Kaen University, Khon Kaen, 40002, Thailand, Tel +66-43-363-746 ; +66-43-363-664, Email [email protected]
Background: Abnormal liver function tests (LFTs) can indicate cirrhosis or liver cancer leading to mortality among systemic sclerosis (SSc) patients. No recent studies have investigated the clinical predictors of an abnormal LFT in SSc. We aimed to determine the incidence of abnormal LFT (including from hepatitis and cholestasis) and to identify its clinical predictors in SSc patients.
Methods: An historical cohort was conducted on 674 adult SSc patients who attended the Scleroderma Clinic, Khon Kaen University, between January 2012 and November 2019 and who underwent routine screening for LFT. A Cox regression was used to analyze the clinical predictors of abnormal LFT.
Results: Four hundred and thirty cases, representing 4190 person-years, had abnormal LFTs (viz, from hepatitis, cholestasis, and cholestatic hepatitis) for an incidence rate of 10.2 per 100 person-years. The respective incidence of hepatitis, cholestasis, and cholestatic hepatitis was 20.5, 12.9, and 20.4 per 100 person-years. The respective median first-time detection of hepatitis, cholestasis, and cholestatic hepatitis was 3.0, 5.9, and 2.8 years, and none had signs or symptoms suggestive of liver disease. According to the Cox regression analysis, the predictors of an abnormal LFT in SSc were elderly onset of SSc (hazard ratio (HR) 1.02), alcoholic drinking (HR 1.74), high modified Rodnan Skin Score (mRSS) (HR 1.03), edematous skin (HR 2.94), Raynaud’s phenomenon (HR 1.39), hyperCKaemia (HR 1.88), and methotrexate use (HR 1.55). In contrast, current sildenafil treatment (HR 0.63) and high serum albumin (HR 0.70) were protective factors.
Conclusion: Occult hepatitis, cholestasis, and cholestatic hepatitis can be detected in SSc patients using LFT screening, especially in cases of early disease onset. The long-term outcome is uncertain, and more longitudinal research is required.
Keywords: systemic sclerosis, scleroderma, scleroderma and related disorders, hepatitis, cholestasis, cholestatic hepatitis, abnormal liver function test, liver, cohort study
Introduction
Systemic sclerosis (SSc) is an immune system disorder that can include complications of liver disease with or without symptoms. Previous clinical studies reported abnormal liver function tests (LFTs) in SSc patients ranging from 1% to 37%,1,2 with cholestasis being the most common, followed by hepatitis.3 Long-lasting drug-induced liver injury, active organ involvement, and fatty liver2 can induce liver fibrosis and cirrhosis.2,4 In most cases, cholestasis or hepatitis in scleroderma do not progress to the point of requiring a liver transplant or death.5
Abnormal liver function tests have been reported among SSc patients since 1934, and primary biliary cholangitis (PBC) is a leading cause of liver disease in SSc.6 Primary sclerosing cholangitis (PSC) and autoimmune hepatitis (AIH) have also been reported in SSc, but their prevalence is relatively rare.7–14 Owing to the various causes of abnormal LFT, the etiologies of abnormal LFT other than those related to autoimmune diseases like SSc—like alcohol consumption and hepatotoxic agents—should be ruled out.8,15–18 Once hepatitis or cholestasis has developed, cirrhosis and its complications (liver cancer) can ensue.19 Previous reports revealed that the prevalence of liver cancer among SSc patients was higher than in the normal population. The respective standardized incidence ratio of liver cancer in female and male SSc patients was 20 and 16 times greater than the general population without any association with specific autoantibodies of SSc (viz., the anti-U1 RNP, anti-Scl70, or anti-centromere antibodies).5 Proper screening of LFT might be beneficial for the early detection of liver cancer, particularly in SSc patients at high risk of developing liver cancer. Currently, there is a lack of research on (a) how often LFT screening should be performed in SSc patients and (b) the risk association or predictors (ie, disease duration, disease severity, and concomitant medications) for hepatitis or cholestasis in SSc patients. We thus aimed to (a) determine the incidence of hepatitis and/or cholestasis and (b) identify the predictors of the abnormal LFT among SSc patients.
Methods
A historical cohort of adult SSc patients who attended the Scleroderma Clinic of Khon Kaen University was conducted between January 2012 and November 2019. We reviewed the clinical data from the medical records and the SSc registry database. We included all patients 18 and older diagnosed with SSc either by the 1980 American College of Rheumatology (ACR)20 or 2013 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) Classification Criteria for Scleroderma.21 The SSc subset was classified as diffuse cutaneous SSc (dcSSc) or limited cutaneous SSc (lcSSc), according to LeRoy et al.22 We excluded all patients with incomplete liver function data.
Clinical data included age, sex, alcohol consumption, duration of disease, SSc subset, organ involvements, skin tightness assessed by the modified Rodnan skin score (mRSS), concomitant medications, and body mass index (BMI). Routine laboratory data included hemoglobin, ALT, AST, alkaline phosphatase (ALP), and serum creatine phosphokinase (CPK). Other information evaluated included hepatitis B surface antigen (HBsAg), anti-hepatitis C virus (anti-HCV), serology (anti-nuclear antibody (ANA), ACA, ATA, anti-mitochondrial antibody (AMA), anti-smooth muscle antibody (ASMA), immunoglobulin G (IgG) level, liver ultrasound, computer tomography, magnetic resonance imaging, liver histology.
SSc was diagnosed by either the 1980 ACR20 or 2013 ACR/EULAR classification.21 The SSc subset was classified according to LeRoy et al.22 The date of onset was the date of the first non-Raynaud’s phenomenon SSc symptoms as reported by the patients. Disease duration was calculated by the visit date and the onset date.
Hepatitis was defined by the increase in serum alanine aminotransferase (ALT) above the normal range (>33 U/L in males and >25 U/L in females). Cholestasis was defined by an increase in serum alkaline phosphatase (ALP) above the normal range (>121 U/L).23 Abnormal LFT was defined if hepatitis or cholestasis were detected.
Edematous skin was defined when physicians documented puffy fingers and/or feet.
mRSS was based on a skin tightness assessment from 17 body sites, including the face, chest, abdomen, arms, forearms, hands, fingers, thighs, legs, and feet. The assessment score was 0 for normal skin tightness, 1 for mild skin tightness, 2 for moderate skin tightness, and 3 for severe skin tightness with the inability to make skin folds between two fingers. The score was calculated by summing the rating from all 17 areas (range, 0–51).24,25
Pulmonary involvement was defined by findings of pulmonary fibrosis, ground-glass opacity, or traction bronchiectasis performed by high-resolution and computed tomography (HRCT) of the chest.
Pulmonary arterial hypertension (PAH) was diagnosed when the mean pulmonary arterial pressure (mPAP) was > 20 mmHg at rest with a pulmonary artery wedge pressure of ≤ 15mmHg and a pulmonary vascular resistance of ≥ 3 Wood units, as confirmed by right heart catheterization.26
Scleroderma renal crisis (SRC) included (a) recent onset of severe hypertension (systolic blood pressure (SBP) ≥ 140 mmHg; diastolic blood pressure (DBP) ≥ 90 mmHg; a rise in SBP ≥ 30 mmHg and/or a rise in DBP ≥ 20 mmHg); (b) a rapid increase in serum creatinine (≥ 50% over baseline or serum creatinine > 120% of the upper limit of normal for local laboratory); and, (c) microangiopathic hemolytic anemia.27
Gastrointestinal involvement was defined when the patients had SSc esophageal symptoms (ie, esophageal dysphagia, heartburn, or reflux symptoms), stomach symptoms (ie, dyspepsia, early satiety, and bloating), or intestinal symptoms (ie, diarrhea, bloating, malabsorption, constipation, and/or ileus or pseudo-intestinal obstruction).28,29
Statistical Analysis
Descriptive data were reported as proportions or percentages for categorical data and median (interquartile range; IQR) for continuous data. The respective incidence rate of abnormal LFT, hepatitis, cholestasis, and cholestatic hepatitis with their 95% confidence interval (95% CI) was calculated. Using the Cox proportional hazards model, the secondary outcomes were analyzed on a time-to-first event basis (abnormal LFT). The hazard ratio (HR) was calculated for identifying the predictors of abnormal LFT. The hazard ratios that accounted for p-value <0.10 were entered into a Cox regression model. The clinical difference in the abnormal LFT pattern was evaluated using the Chi-square test for categorical data and the one-way ANOVA or Kruskal Wallis test for continuous data. A P-value less than 0.05 was considered statistically significant. All statistical analyses were performed with STATA version 16.0.
Results
Seven hundred and twelve SSc patients from among 7818 visits were reviewed, of whom 38 were excluded due to lack of LFT data. A total of 674 patients were included in the analysis. Most of the patients were female (427 cases; 63.4%) and the dcSSc subset (468 cases; 69.5%). The respective mean age and median duration of disease duration was 56.7±11.4 years and 4.4 years (IQR 1.5–9.4).
Four hundred and thirty cases (comprising 4190 person-years) had an abnormal LFT (hepatitis, cholestasis, and cholestatic hepatitis), resulting in an incidence of abnormal LFT of 10.2 per 100 person-years. The median time to the first detection of abnormal LFT was 7.0 years (95% CI 5.9–7.9). According to the characteristics of abnormal LFT, hepatitis had the highest incidence, followed by cholestasis and cholestatic hepatitis. The respective number of patients with hepatitis, cholestasis, and cholestatic hepatitis was 323, 70, and 37 cases for a 100-person-year incidence rate of 20.5, 12.9, and 20.4. The respective median time to the first detection of hepatitis, cholestasis, and cholestatic hepatitis was 3.0, 5.9, and 2.9 years. The patient flow diagram is presented in Figure 1.
 |
Figure 1 Patient flow diagram. |
According to the Cox analysis, the risks of an abnormal LFT in SSc included elderly age at onset, alcohol consumption, extensive skin involvement assessment by mRSS, Raynaud’s phenomenon, edematous skin, tendon friction rub, arthritis, gastrointestinal involvement, hyperCKaemia, current methotrexate, and ATA positive. Meanwhile, protective factors against an abnormal LFT were pulmonary hypertension, current sildenafil use, ACA positive, and high serum albumin level (Table 1). The clinical difference between patients with a normal and an abnormal LFT is presented in Table 1.
 |
Table 1 Clinical Difference Between Patients with Normal and Abnormal LFT |
According to the Cox regression analysis, the respective risk of an abnormal LFT increased with (a) every 1-year increase in age at onset, (b) alcohol consumption, (c) every 1-point increase in mRSS, (d) having edematous skin, (e) Raynaud’s phenomenon, (f) hyperCKaemia, (g) current methotrexate use with respective adjusted HR by 1.02, 1.74, 1.03, 2.94, 1.40, 1.88, and 1.55. By contrast, the respective adjusted HR of the protective factors (a) current sildenafil treatment and (b) every 1 g/dL increase of serum albumin was 0.63 and 0.70 (Table 2).
 |
Table 2 Cox Regression Analysis of the Predictors of Abnormal LFT |
When comparing the characteristics of abnormal LFT, the patients with hepatitis and cholestatic hepatitis vs other groups had (a) a longer duration of the disease during abnormal LFT detection, (b) a more extensive skin thickness, (c) a more frequent tendon friction rub, and (d) greater hyperCKaemia. In addition, the patients with hepatitis vs other groups experienced more frequent edematous skin but less ACA-positive and pulmonary hypertension. The patients who received MMF or sildenafil developed hepatitis, cholestasis, and cholestatic hepatitis less frequently than those who did not receive the medications. The clinical differences between each characteristic associated with abnormal LFT are presented in Table 3.
 |
Table 3 Clinical Differences Between the Patients with Hepatitis, Cholestasis, and Cholestatic Hepatitis |
Around 20% of patients with hepatitis and 29.7% of those with cholestatic hepatitis had an ALT level two times higher than the normal limit (Figure 2). The ALP was three times higher than the normal upper limit in 7% and 8% of patients with cholestasis and cholestatic hepatitis, respectively (Figure 3). One patient with cholestatic hepatitis was positive for HBsAg. A liver ultrasound was performed on ten patients and fatty liver was present—five patients with hepatitis and one with cholestatic hepatitis. None of the patients with an abnormal LFT underwent a liver biopsy due to lack of clinical symptoms, physician unawareness, and patient refusal.
 |
Figure 2 Proportion of patients having ALT 2 times above the normal limit. |
 |
Figure 3 Proportion of patients having ALP 3 times above the normal limit. |
The Kaplan-Meier graph of each characteristic of abnormal LFT is presented in Figure 4.
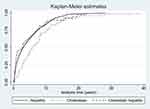 |
Figure 4 Kaplan-Meier graph of each characteristic of abnormal LFT. |
Discussion
The current study included 674 SSc patients in a large historical cohort of liver function assessments. There have been no studies on the incidence or factors associated with abnormal LFT in SSc patients. Our objective was to investigate the prevalence of, and factors associated with, abnormal LFT in SSc. The prevalence of hepatitis in the non-obese or lean population is between 7.6 and 53%.30–37 In the normal Thai population, the prevalence of an abnormal LFT is between 0.03 and 6.9%—the most common cause is drug or herb-induced abnormal LFT,38 followed by hepatitis B39 and C.40 Liver involvement in SSc is between 0.04 and 18%.6,41 Liver abnormalities included primary biliary cirrhosis (PBC),6,41 primary sclerosing cholangitis (PSC),9 and gallbladder dysmotility.42 Salem et al3 reported ALP increasing by 30% and ALT increasing above reference values by 17.5% in SSc patients compared to controls. Salem et al3 also found that gamma-glutamyl transferase (GGT) trended to be higher in patients with SSc. Our study revealed many patients with abnormal LFT by routine screening during follow-up (430 of 674 SSc cases), which seemed higher than in previous reports, although a direct comparison is not possible.6,41 The incidence of an abnormal LFT in SSc patients was around 10 per 100 person-years based on 4190 person-years. The abnormality was commonly detected in early-onset disease even without clinical symptoms suggestive of liver disease, and the abnormal LFT gradually increased during the follow-up period.
Edematous skin was a predictor of abnormal LFT in SSc. In general, edematous skin is an early presentation of SSc. According to our results, abnormal LFT was also found by routine screening in early-onset disease (in the first seven years), indicating that the liver presents occult organ involvement in early-onset disease. Unfortunately, no liver pathology was obtained, so we cannot conclude the nature of the abnormality—whether it was a vasculopathy, fibrosis, or immune-induced inflammation process, inherent in SSc pathogenesis.43
High serum albumin was a protective factor against abnormal LFT in SSc. On the other hand, low serum albumin is a marker of chronic liver disease,44 although it can also result from inflammation or malnutrition (inadequate protein intake).45 Our analysis did not show an association between abnormal LFT and inflammatory markers (ESR, CRP) or nutritional status (BMI), so the low serum albumin in our cohort could be directly associated with liver disease. However, the long-term outcome of liver disease in patients with low serum albumin and with abnormal LFT is unclear, so follow-up is suggested on the clinical course of liver disease and outcomes in those with low serum albumin in combination with abnormal LFT.
Abnormal LFT was less common in patients who received sildenafil treatment than in those who did not. Sildenafil is used as a vasodilator for PAH46,47 and vasculopathy treatment48 for SSc patients. The protective mechanism against the development of abnormal LFT in those who received sildenafil remains unclear. We thus hypothesize that vasculopathy could be the result of liver abnormality in SSc; however, further vascular studies and/or histopathological confirmations are needed. We do not have data on vasodilators other than sildenafil because it was the only cost-effective one approved by the Thai Food and Drug Administration for the treatment of PAH and vasculopathy of SSc. Analysis of the effect of other vasodilators on liver disease might help to demonstrate our hypothesis.
According to the Cox regression analysis, disease severity—particularly extensive skin thickness as evaluated by mRSS—was a risk for abnormal LFT among patients with SSc. Lee et al49 studied liver stiffness using transient elastography examination, and 7.4 kPa was adopted as the cut-off value for significant liver fibrosis in non-viral and non-heavy alcoholic consumption in Korean SSc patients. Lee et al49 also found a correlation between Medsger’s severity score and liver stiffness. Medsger et al50 showed that the SSc severity score, including mRSS, can be used to predict reduced survival. We demonstrated the association between abnormal LFT and disease severity (mRSS). The abnormal LFT might thus indicate a poor prognosis of the disease.
Methotrexate is a predictor of abnormal LFT in SSc. The finding is within expectations and is not a new finding. We know that a serious adverse drug reaction to methotrexate is hepatitis, so it is not surprising to find that methotrexate poses a risk of abnormal LFT in SSc. Methotrexate is the standard medical treatment for controlling arthritis symptoms, particularly rheumatoid arthritis (RA) and psoriatic arthritis (PsA). The prevalence of methotrexate-induced hepatotoxicity is higher in patients with PsA than in those with RA (14.5% and 7.5%, respectively).51 However, no recent data on the incidence or prevalence of methotrexate-induced hepatotoxicity in SSc are available. Our findings provide preliminary data on the risk of methotrexate-induced hepatitis among SSc patients. We suggest that SSc patients who receive methotrexate should be regularly tested for LFT, as with other rheumatic diseases.
PBC and PSC are liver diseases that result in elevation of ALP. PBC is a common liver disease in SSc, and it was commonly revealed in the lcSSc subset6,41 and in those who were positive for the anti-centromere antibody.52 While PSC overlap SSc is rare,53 the lcSSc subset tends to be a risk factor for cholestasis among Thais with SSc who might have either PBC or PSC overlap SSc. However, none of our patients had symptoms of PBC or PSC during follow-up, and dcSSc is a more common SSc subset in Thais than lcSSc.29 The low incidence of cholestasis and cholestatic hepatitis could be explained by the low prevalence of lcSSc in Thais. AMA is a specific antibody used to diagnose PBC; however, AMA and cholangiographic imaging were only tested in a small proportion of our patients due to limited resources; therefore, PBC or PSC could not be identified as the definitive cause of cholestasis.
AST, a liver enzyme, is also known as an isoenzyme of muscle. Once muscle injury occurs from any cause, AST can be elevated, so we did not include AST as a liver function test in this study in order to avoid confounding the interpretation. ALT is a liver enzyme that can increase due to muscle injury but less frequently than AST.54,55 We found that hyperCKaemia was associated with hepatitis in SSc; however, we cannot conclude whether ALT elevation in SSc patients was related to increased isoenzymes from muscle injury or directly due to liver disease. Due to the uncommon elevation of ALT in muscle injury, we assumed that the increased ALT in our study could represent liver disease rather than a muscle disease.
The highest incidence of abnormal LFT in SSc from our cohort was hepatitis, followed by cholestatic hepatitis and cholestasis. Liver injury—indicated by a rising ALT or hepatitis—was a more common characteristic of abnormal LFT than excretory dysfunction as evaluated by increased ALP or cholestasis. Most patients with an abnormal LFT had no clinical symptoms associated with hepatobiliary diseases and any abnormalities were mild, so ALT and ALP levels rose less than 2–3 times above normal upper limits. Special tests, such as imaging and serology, were only performed on a small number of our patients to assess the cause of the abnormality. Furthermore, the number of patients with ALT or ALP 2–3 times greater than the normal limit was too low to analyze the association of factors. As no test was performed for all patients with an abnormal LFT, we cannot conclude what caused the abnormal LFT in all those patients. However, we included the possible common causes of abnormal LFT in our analysis, thus ensuring that we had included the warrant parameters (ie, alcohol, drug, and BMI), which adequately explain the nature of an abnormal LFT. We plan to do a longitudinal analysis of patients with abnormal LFT to determine whether the finding persists.
The strengths of our historical cohort study include (a) the inclusion of a large number of SSc subjects who had given informed consent, ensuring confidence in the power of analysis; (b) the inclusion of the clinical characteristics of SSc and the possible causes associated with abnormal LFT, ensuring a complete set of data for the analysis; (c) the screening of most of our patients for LFT and inclusion of the factors that predict abnormal LFT detection for the first-time. Limitations include (a) some missing data in particular serology tests for SSc, so we cannot confirm or deny whether those serologies are predictors of abnormal LFT; (b) some investigations could not be performed as patients refused the invasive liver biopsy, and some tests were unavailable due to budget limitations (ie, computed tomography, fibroscan, specific serology for autoimmune liver diseases), so we cannot more completely categorize the etiology of liver disease among SSc patients; (c) a single-center study, so the results cannot be generalized; and, (d) a lack of detail of the course of liver disease and any changes in LFT (ie, whether persistent or transient abnormal) because these were not our objectives of the current study. The course of liver disease and changes in LFT will be further analyzed in a separate report.
Conclusion
By LFT screening, occult hepatitis, cholestasis, and cholestatic hepatitis can be detected in patients with SSc. Elderly age at onset, alcohol consumption, extensive skin tightness, active organs, and immunosuppressive use were predictors of abnormal LFT. However, the long-term outcome is questionable and needs further longitudinal analysis.
Ethics Approval and Consent to Participate
The Human Research Ethics Committee of Khon Kaen University, Khon Kaen, Thailand approved the study as per the Helsinki Declaration and the Good Clinical Practice Guidelines (HE631624). All eligible patients signed informed consent before entry into the cohort study.
Acknowledgments
The authors thank (a) the Research and Graduate Studies, Khon Kaen University, Thailand, the Scleroderma Research Group and Faculty of Medicine, Khon Kaen University, for the support, and (b) Mr. Bryan Roderick Hamman—under the aegis of the Publication Clinic Khon Kaen University, Thailand—for assistance with the English-language presentation.
Disclosure
All authors declare that they do not have any competing interests.
References
1. De Santis M, Crotti C, Selmi C. Liver abnormalities in connective tissue diseases. Best Pract Res Clin Gastroenterol. 2013;27(4):543–551. doi:10.1016/j.bpg.2013.06.016
2. Kojima H, Uemura M, Sakurai S, et al. Clinical features of liver disturbance in rheumatoid diseases: clinicopathological study with special reference to the cause of liver disturbance. J Gastroenterol. 2002;37:617–625.
3. Salem GIA, Abdulrahman AA. Evaluation of liver function tests in scleroderma patients. Rheumatol Int. 2012;32:2371–2375.
4. Rigamonti C, Bogdanos DP, Mytilinaiou MG, Smyk DS, Rigopoulou EI, Burroughs AK. Primary biliary cirrhosis associated with systemic sclerosis: diagnostic and clinical challenges. Int J Rheumatol. 2011;2011:976427.
5. Chatterjee S, Dombi GW, Severson RK, Mayes MD. Risk of malignancy in scleroderma: a population-based cohort study. Arthritis Rheum. 2005;52:2415–2424.
6. Assassi S, Fritzler MJ, Arnett FC, et al. Primary biliary cirrhosis (PBC), PBC autoantibodies, and hepatic parameter abnormalities in a large population of systemic sclerosis patients. J Rheumatol. 2009;36:2250–2256.
7. Akiyama Y, Tanaka M, Takeishi M, Adachi D, Mimori A, Suzuki T. Clinical, Serological and Genetic Study in Patients with CREST Syndrome. Intern Med. 2000;39:451–456.
8. Rodrigues CEM, Borges CL, de Carvalho JF. Diffuse systemic sclerosis and autoimmune hepatitis: a unique association. Clin Rheumatol. 2010;29:799–801.
9. Fraile G, Rodríguez-García JL, Moreno A. Primary sclerosing cholangitis associated with systemic sclerosis. Postgrad Med J. 1991;67:189–192.
10. Lu Q. The critical importance of epigenetics in autoimmunity. J Autoimmun. 2013;41:1–5. doi:10.1016/j.jaut.2013.01.010
11. Marie I, Levesque H, Tranvouez J, et al. Autoimmune hepatitis and systemic sclerosis: a new overlap syndrome? Rheumatology. 2001;40(1):102–106. doi:10.1093/rheumatology/40.1.102
12. Yabe H, Noma K, Tada N, Mochizuki S, Nagano M. A Case of CREST Syndrome with Rapidly Progressive Liver Damage. Intern Med. 1992;31(1):69–73. doi:10.2169/internalmedicine.31.69
13. Toyoda M, Yokomori H, Kaneko F, et al. Primary Biliary Cirrhosis-Autoimmune Hepatitis Overlap Syndrome Concomitant with Systemic Sclerosis, Immune Thrombocytopenic Purpura. Internal Med. 2009;48(23):2019–2023. doi:10.2169/internalmedicine.48.2687
14. Ngo Mandag N, Van Gossum M, Rickaert F, Golstein M. [Autoimmune hepatitis and CREST syndrome]. Rev Med Brux. 2007;28:528–531.
15. Assandri R, Monari M, Montanelli A. Development of systemic sclerosis in patients with autoimmune hepatitis: an emerging overlap syndrome. Gastroenterol Hepatol Bed Bench. 2016;9:211–219.
16. Ben-Ari Z, Czaja AJ. Autoimmune hepatitis and its variant syndromes. Gut. 2001;49:589–594.
17. Mack CL, Adams D, Assis DN, et al. Diagnosis and Management of Autoimmune Hepatitis in Adults and Children: 2019 Practice Guidance and Guidelines From the American Association for the Study of Liver Diseases. Hepatology. 2020;72:671–722.
18. Washington MK. Autoimmune liver disease: overlap and outliers. Modern Pathology. 2007;20:S15–30.
19. You BC, Jeong SW, Jang JY, et al. Liver cirrhosis due to autoimmune hepatitis combined with systemic sclerosis. Korean J Gastroenterol. 2012;59:48–52.
20. Preliminary criteria for the classification of systemic sclerosis (scleroderma). Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Arthritis Rheum. 1980;23:581–590.
21. van den Hoogen F, Khanna D, Fransen J, et al. 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis. 2013;72:1747–1755.
22. LeRoy EC, Black C, Fleischmajer R, et al. Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol. 1988;15:202–205.
23. Kwo PY, Cohen SM, Lim JK, Clinical Guideline ACG. Evaluation of Abnormal Liver Chemistries. Am J Gastroenterol. 2017;112:18–35.
24. Brennan P, Silman A, Black C, et al. Reliability of skin involvement measures in scleroderma. The UK Scleroderma Study Group. Br J Rheumatol. 1992;31:457–460.
25. Black CM. Measurement of skin involvement in scleroderma. J Rheumatol. 1995;22:1217–1219.
26. Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J. 2019;53:1801913.
27. Steen VD, Mayes MD, Merkel PA. Assessment of kidney involvement. Clin Exp Rheumatol. 2003;21:S29–31.
28. Savarino E, Furnari M, de Bortoli N, et al. Gastrointestinal involvement in systemic sclerosis. Presse Med. 2014;43:e279–291.
29. Foocharoen C, Peansukwech U, Mahakkanukrauh A, et al. Clinical characteristics and outcomes of 566 Thais with systemic sclerosis: a cohort study. Int J Rheum Dis. 2020;23:945–957.
30. Manco M, Alisi A, Real JMF, et al. Early interplay of intra-hepatic iron and insulin resistance in children with non-alcoholic fatty liver disease. J Hepatol. 2011;55:647–653.
31. Vos B, Moreno C, Nagy N, et al. Lean non-alcoholic fatty liver disease (Lean-NAFLD): a major cause of cryptogenic liver disease. Acta Gastroenterol Belg. 2011;74:389–394.
32. Margariti A, Deutsch M, Manolakopoulos S, Tiniakos D, Papatheodoridis GV. The severity of histologic liver lesions is independent of body mass index in patients with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2013;47:280–286.
33. Alam S, Gupta UD, Alam M, Kabir J, Chowdhury ZR, Alam AKMK. Clinical, anthropometric, biochemical, and histological characteristics of nonobese nonalcoholic fatty liver disease patients of Bangladesh. Indian J Gastroenterol. 2014;33:452–457.
34. Leung JCF, Loong TCW, Wei JL, et al. Histological severity and clinical outcomes of nonalcoholic fatty liver disease in nonobese patients. Hepatology. 2017;65:54–64.
35. Cruz A, Bugianesi E, George J, et al. 379 Characteristics and Long-Term Prognosis of Lean Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2014;146:S–909.
36. Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–923.
37. Cruz ACD, Bugianesi E, George J, et al. 379 Characteristics and Long-Term Prognosis of Lean Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2014;5(146):S909.
38. Roongrawee T, Thanapirom K, Chaiteerakij R, Komolmit P, Phathong C, Treeprasertsuk S. Drugs-Herbs-Dietary Supplements-induced Liver Injury: a Hidden but Emerging Clinical Problem. J Med Assoc Thai. 2020;103:92–98.
39. Leroi C, Adam P, Khamduang W, et al. Prevalence of chronic hepatitis B virus infection in Thailand: a systematic review and meta-analysis. Int J Infect Dis. 2016;51:36–43.
40. Wasitthankasem R, Pimsingh N, Treesun K, et al. Prevalence of Hepatitis C Virus in an Endemic Area of Thailand: burden Assessment toward HCV Elimination. Am J Trop Med Hyg. 2020;103:175–182.
41. Jacobsen S, Halberg P, Ullman S, et al. Clinical features and serum antinuclear antibodies in 230 Danish patients with systemic sclerosis. Br J Rheumatol. 1998;37:39–45.
42. Posthuma WF, Ledeboer M, Masclee AA, et al. Do patients with systemic sclerosis have abnormal gallbladder function? Eur J Gastroenterol Hepatol. 1997;9:675–677.
43. Stern EP, Denton CP. The pathogenesis of systemic sclerosis. Rheum Dis Clin North Am. 2015;41:367–382.
44. Bernardi M, Angeli P, Claria J, et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020;69:1127–1138.
45. Don BR, Kaysen G. Serum albumin: relationship to inflammation and nutrition. Semin Dial. 2004;17:432–437.
46. Chaisson NF, Hassoun PM. Systemic sclerosis-associated pulmonary arterial hypertension. Chest. 2013;144:1346–1356.
47. Klinger JR, Elliott CG, Levine DJ, et al. Therapy for Pulmonary Arterial Hypertension in Adults: update of the CHEST Guideline and Expert Panel Report. Chest. 2019;155:565–586.
48. Henness S, Wigley FM. Current drug therapy for scleroderma and secondary Raynaud’s phenomenon: evidence-based review. Curr Opin Rheumatol. 2007;19:611–618.
49. Lee SW, Kim BK, Park JY, et al. Disease duration and Medsger’s severity score are associated with significant liver fibrosis in patients with systemic sclerosis. Clin Exp Rheumatol. 2015;33:S68–74.
50. Medsger TA, Bombardieri S, Czirjak L, Scorza R, Della Rossa A, Bencivelli W. Assessment of disease severity and prognosis. Clin Exp Rheumatol. 2003;21:S42–46.
51. Tilling L, Townsend S, David J. Methotrexate and hepatic toxicity in rheumatoid arthritis and psoriatic arthritis. Clin Drug Investig. 2006;26:55–62.
52. Almaabdi K, Ahmad Z, Johnson SR. Advanced Autoantibody Testing in Systemic Sclerosis. Diagnostics. 2023;13:851.
53. Powell A, McNeil J. Primary sclerosing cholangitis associated with CREST (calcinosis, Raynaud phenomenon, oesophageal dysmotility, sclerodactyly and telangiectasia) in an elderly woman: a case report. J Med Case Rep. 2015;9:272.
54. Mathur T, Manadan AM, Thiagarajan S, Hota B, Block JA. Serum transaminases are frequently elevated at time of diagnosis of idiopathic inflammatory myopathy and normalize with creatine kinase. J Clin Rheumatol. 2014;20:130–132.
55. Volochayev R, Csako G, Wesley R, Rider LG, Miller FW. Laboratory Test Abnormalities are Common in Polymyositis and Dermatomyositis and Differ Among Clinical and Demographic Groups. Open Rheumatol J. 2012;6:54–63.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
