Back to Journals » Infection and Drug Resistance » Volume 12
In vitro reduction of colistin susceptibility and comparative genomics reveals multiple differences between MCR-positive and MCR-negative colistin-resistant Escherichia coli
Authors Luo Q , Niu T, Wang Y, Yin J, Wan F, Yao M, Lu H, Xiao Y, Li L
Received 30 March 2019
Accepted for publication 13 May 2019
Published 12 June 2019 Volume 2019:12 Pages 1665—1674
DOI https://doi.org/10.2147/IDR.S210245
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Qixia Luo,1,* Tianshui Niu,1,* Yuan Wang,1 Jianhua Yin,2 Fen Wan,3 Mingfei Yao,1 Haifeng Lu,1 Yonghong Xiao,1 Lanjuan Li1
1State Key Laboratory for Diagnosis and Treatment of Infectious Diseases, Hangzhou, The First Affiliated Hospital, College of Medicine, Zhejiang University, People’s Republic of China; 2College of Biotechnology and Bioengineering, Zhejiang University of Technology, Hangzhou, People’s Republic of China; 3College of Laboratory Medicine, Hangzhou Medical College, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Objectives: Although resistance to colistin is increasingly reported from clinical settings, the genetic mechanisms that lead to colistin resistance in Escherichia coli have not been fully characterized. Here, we assess the evolution of colistin resistance in clinical isolates of mobilized colistin resistance (MCR)-negative and MCR-positive Escherichia coli.
Methods: Spontaneously mutated colistin-resistant progeny were evolved using a step-wise reduction of colistin susceptibility. Resistance phenotypes were confirmed by minimum inhibitory concentration (MIC) determination, and the probable resistance mechanisms were investigated using PCR and reverse transcription-quantitative PCR. Mutated genes of the laboratory-evolved mutants were identified by whole-genome sequencing and comparative genomics. Fitness costs and serum resistance of the mutants were also compared to the corresponding wild types.
Results: MCR-negative isolates displayed higher increases in MICs than did MCR-positive isolates following colistin exposure. Upregulation of pmrAB and associated genes was evident among MCR-negative isolates but not MCR-positive isolates. Comparative genomic analysis of mutants and their corresponding wild-types (WTs) revealed numerous mutations in genes encoding membrane transporters and two-component systems. Additionally, MCR-negative mutants exhibited higher fitness costs than MCR-positive mutants compared with their corresponding WTs but displayed similar serum resistance.
Conclusion: Our findings reveal multiple differences between MCR-positive and MCR-negative E. coli strains following colistin exposure, which provide reference values for clinical medication.
Keywords: colistin resistance, MCR, comparative genomic, Escherichia coli
Introduction
The interest in colistin (polymyxin E) as a treatment option and antibiotic of last resort has been revived, since the increasing incidence of infections caused by multidrug-resistant Gram-negative bacteria in clinical settings.1 However, the emergence of plasmid-mediated colistin resistance via mobilized colistin resistance (mcr) genes has become a challenge to public health worldwide. MCR-positive Enterobacteriaceae have been isolated from various sources including humans, other animals, and food, most of which were Escherichia coli.2–5 Except for MCR, colistin resistance in Gram-negative bacteria can also be conferred by mutations in chromosomal genes associated with the biosynthesis and modification of lipopolysaccharide (LPS), and include a large array of genes and operons.6–8 Two different colistin resistance mechanisms caused by mutations in chromosomal genes have been described; the first involves the loss of LPS due to mutations in the lpxABCD genes, as demonstrated in Acinetobacter baumannii.8,9 The second mechanism entails mutations in genes involved in the regulation of LPS modifications and includes genes involved in PmrAB and PhoPQ two-component systems (2CSs), as well as the negative regulator gene mgrB in Klebsiella pneumoniae.10,11
Previously described chromosomal mutations responsible for acquired colistin resistance in isolates of E. coli have been associated with amino acid changes in PmrAB and PhoPQ.1,10,12 In a recent study, we described for the first time a close to equivalent clinical isolation ratio of MCR-negative and MCR-positive colistin-resistant isolates of E. coli, with no demonstrable nosocomial transmission.13 Five unique amino acid substitutions were identified among these colistin-resistant MCR-negative E. coli strains, four in PmrB and one in PhoQ.13 However, amino acid changes in PmrAB and PhoPQ might not be essential for colistin resistance in E. coli. Mutations in other chromosomal genes and other non-transferable mechanisms conferring colistin resistance in E. coli isolates are likely to exist, but have not yet been elucidated; hence further study is warranted.
The clinical breakpoint of colistin is >2 mg/L for Enterobacteriaceae (EUCAST 2018), and E. coli producing MCR generally display MICs of 4–8 mg/L for colistin.13 However, MCR-negative colistin-resistant E. coli generally exhibit higher MICs (16–64 mg/L) than MCR-positive isolates without additional resistance mechanisms.13 We hypothesize that acquired colistin resistance due to chromosomal mutations is less likely to evolve in isolates producing MCR than isolates non-producing MCR. In the present study, we assess the evolution of colistin resistance in clinical isolates of MCR-negative and MCR-positive E. coli. The results deepen our understanding of colistin resistance mechanisms in MCR-positive and MCR-negative E. coli strains.
Methods
Bacterial isolates and antimicrobial susceptibility testing
Clinical E. coli isolates were identified using matrix-assisted laser desorption-ionization time-of-flight mass spectrometry. Isolates evaluated in this study included clinical isolates and laboratory-evolved colistin-resistant mutants (Table 1). The broth microdilution method was used for colistin MIC determination in accordance with the Clinical and Laboratory Standards Institute (CLSI-2018).
Laboratory evolution of mutants with reduced colistin susceptibility
A step-wise reduction in colistin susceptibility was performed according to a previous study.14 Briefly, a single colony of each clinical isolate was grown in Muller-Hinton (MH) broth overnight at 37°C, and cultures were diluted 1:100 in MH broth containing serially increasing concentrations of colistin, starting at the one-half MIC value of the respective isolate, and doubling every 24 hrs until bacterial growth was completely inhibited (with no bacteria growth after spreading 100 µL of the culture on MH agar plates supplemented with corresponding concentration of colistin). The concentration of colistin at which bacterial growth was completely inhibited was recorded as the final colistin concentration (FCC). Subsequently, overnight cultures were plated on MH agar plates containing one-half FCC. Twenty mutants of each WT strain were randomly selected from plates containing one-half FCC. The stability of the selected mutants was tested by serial passage in MH broth without colistin, and the colistin resistance phenotype was tested by the MICs. In addition, we measured the frequency of appearance of the colistin-resistant mutants under the first concentration of the step-wise induction, half MICs of the WT strains. Induced cultures were plated on MH agar with or without colistin (2 mg/L for MCR-negative group and 4 mg/L for the MCR-positive group). All the plates were incubated overnight at 37°C, and the colony counts on colistin-containing plates after 24 hrs of growth were regarded as the number of derived mutants.15
Whole-genome sequencing and bioinformatic analysis
Single colonies of WTs and their two laboratory-evolved mutants were cultured overnight at 37°C in MH broth, and genomic DNA was prepared using a Yeast/Bact. Kit (cat. no. 8,510,633; QIAGEN) according to the manufacturer’s instructions. After library preparation, genomes were sequenced using the Illumina HiSeq 2500-PE150 platform (Illumina, San Diego, CA, USA). Quality-trimmed raw sequence data were assembled using Velvet 1.2.7. Annotation was performed by uploading data to the RAST server (rast.nmpdr.org). Sequence data from all isolates were deposited in GenBank under the accession numbers indicated in Supplementary
Reverse transcription-quantitative PCR (RT-qPCR)
Overnight cultures of WTs and their corresponding mutants were diluted 1:100 and subcultured in MH medium for ~3 hrs at 37°C (absorbance at 600 nm [OD600] ~0.6) without colistin. Cells were collected at 4°C by centrifuging at 10,000 rpm for 1 min, and RNA was extracted using TRIzol Reagent (Invitrogen). DNase I-treated RNA was obtained using an RNeasy Mini Kit (QIAGEN, No. 75,142), and mRNA expression levels of genes involved in colistin resistance were examined using real-time PCR primers (EC-gene-RT-F/R) listed in Supplementary
Fitness cost measurement
We determined the growth of WTs and mutants in MH broth respectively, before fitness measurement, to exclude the effect of original growth. Fresh medium was inoculated with overnight cultures grown from a single colony by 1:100 dilution, and growth was determined by recording the optical density (OD) of cultures at OD600. Fitness costs of mutants compared with their respective WTs were determined by competition experiment as described previously.17 Briefly, overnight cultures of WTsand their corresponding mutants were diluted 1:100 into fresh MH broth and cultivated to an OD600 of 0.5. A 1:1 volumetric mixture of WT and corresponding mutants was diluted 1:400 into 10 mL of fresh MH medium with no colistin addition, and 200 μL of the diluted culture was removed and used for viable colony counting on MH agar. Viable colony counting was performed on MH agar both with and without colistin (2 mg/L in MCR-negative groups and 8 mg/L in MCR-positive groups). The remaining culture was incubated at 37°C for 20 hrs with shaking at 200 rpm, after which viable colony counting was performed again. Relative fitness was calculated as described previously.18
Serum resistance assay
Serum resistance assay was measured according to the previous study.19 Briefly, after cultured in MH broth for 14 hrs, the bacteria were washed and resuspended in phosphate-buffered saline to an OD of 1.0. Human serum from healthy individuals was mixed, and bacterial suspensions were then added to human serum to obtain a bacterial cell concentration of 1×107CFU/mL. Then, samples were incubated at 37°C for 2 hrs. Viable counts were determined at 0 and 2 hrs time points. Three independent experiments were performed.
Statistical analysis
For statistical analysis, values are presented as means ± standard deviation (SD). Rank-sum tests were performed for pair-wise comparisons of groups, and p<0.05 (two-tailed) was considered significant.
Ethics statement
Serum was obtained from four healthy volunteers who gave their written informed consent to the study, which was approved by the medical ethics committee of the First Affiliated Hospital, College of Medicine, Zhejiang University.
Results
MCR-negative isolates could be induced to higher FCCs than MCR-positive isolates
Two groups of E. coli were involved in this study; the colistin-susceptible, MCR-negative group includes ATCC 25,922 and three randomly selected clinical isolates (1,273, 1,876, and 1,910); the colistin-resistant, MCR-positive (harboring MCR-1) group includes four randomly selected clinical isolates (16,802, 18,017, 24,990, and 25,315). Colistin MICs of these eight isolates were measured (Table 1). In vitro reduction of colistin susceptibility was conducted. We measured the frequency of appearance of the resistant mutants under the first concentration of the step-wise induction and discovered no significant differences between MCR-positive group and MCR-negative group. Twenty mutants of each WT strain were randomly selected from the one-half FCC plates. Mutants from the same WT strain displayed the same MIC value after measuring in triplicate. The MICs of mutants from the MCR-negative group ranged from 32 to 64 mg/L, whereas MICs for mutants from the MCR-positive group were 8–16 mg/L. Thus, MICs of mutants from the MCR-negative group were higher than those from the MCR-positive group (p<0.01). Isolates from the MCR-negative group displayed higher FCCs than isolates from the MCR-positive group (Table 1). We then randomly selected two mutants (labeled −1 and −2) of each WT strain (Table 1) for further study.
MCR-negative mutants possess mutations in pmrAB
Mutations in the 2CS genes pmrAB and phoPQ, and the PhoPQ negative regulator gene mgrB, which are known to engender colistin resistance via their role in LPS modification, were analyzed. WT and mutant sequences were compared, and mutations were confirmed by PCR using primers described previously13 (Supplementary
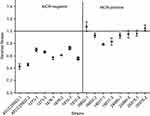
Expression of pmrB and several pmrB regulated genes are elevated in MCR-negative mutants, but not in all MCR-positive mutants
Expression levels of pmrAB, phoPQ, and mgrB in MCR-negative and MCR-positive mutants were compared with those in their corresponding WTs. No discernable changes in expression levels of phoPQ and mgrB were observed in any pairs. However, differences between mutants and WT isolates were observed for pmrA and pmrB (Figure 1A-B); relative expression in MCR-negative mutants was higher than in WTs. By contrast, no regular pattern in the expression of pmrA and pmrB was observed for MCR-positive isolates.
The PmrAB 2CS regulates a set of genes associated with the chemical alteration of LPS, which in turn affects colistin susceptibility in E. coli. These regulated genes including eptA (phosphoethanolamine transferase), the arnB operon (polymyxin resistance-associated operon), and yibD (galactosyltransferase). As expected, expression of PmrB regulated genes was increased when the pmrB expression was increased (Figure 1C–E). Expression levels of eptA, arnB, and yibD were significantly higher in MCR-negative mutants than in their corresponding WTs (p<0.05). This was not the case for the MCR-positive group.
Comparative genomics reveals the importance of membrane transporters and 2CSs for acquired, chromosomal colistin resistance
In addition to known colistin resistance-related genes in E. coli, other chromosomal genes associated with colistin resistance can be explored using comparative genomics. All 16 selected mutants and their WT strains were whole genome-sequenced. Nucleotide sequences of other genes encoding proteins associated with LPS modifications (arnC, arnT, and pmrDGJML) were analyzed, but no point mutations or sequence inserts were found. Furthermore, nucleotide sequences of genes associated with colistin resistance via loss of LPS (lpxA, lpxB, lpxC, and lpxD) were also analyzed, but amino acid alterations were not present in mutants.
To investigate the diversity of mutations potentially responsible for increasing colistin MICs in the laboratory-evolved mutants, pair-wise genetic relatedness among mutants and their corresponding WTs was analyzed using whole-genome SNP data. A total of 333 genes carrying non-synonymous SNPs among the 16 mutants were identified (Supplementary
 | Table 2 Mutated membrane transporter genes and two-component system genes |
Due to the important contributions of 2CSs in colistin resistance, we paid particular attention to other mutated 2CSs in the mutants. In addition to PmrA/PmrB, there were non-synonymous mutations in three other 2CSs: EvgS/EvgA (regulation of MDR transporters), AtoS/AtoC 2CS (associated with calcium channels), and KdpE/KdpD (regulation of potassium transporters; Table 2). The four 2CSs mutated in this study account for more than 10% of all 30 2CSs present in E. coli (
MCR-positive mutants exhibit lower fitness costs than MCR-negative mutants, but display similar serum resistance
To investigate the effects of the mutations on E. coli fitness, growth competition experiments between mutant and WTs were conducted after confirmation of no original growth differences between WTs and their corresponding mutants. The fitness costs of MCR-negative mutants vs corresponding WTs were higher than those of MCR-positive mutants vs corresponding WTs (p<0.01), and the relative fitness ranged from 0.42 to 1.09 among isolates (Figure 2). Furthermore, mutants of ATCC 25,922 displayed more severe fitness costs than other mutants from the MCR-negative group (p<0.05; Figure 2).
To analyze whether the survival in human blood of the mutants is different from the WTs, serum resistance analysis was conducted. The results of serum resistance assays are shown in Table 1 as survival of mutants compared with WTs. There were no obvious differences in survival between WTs and mutants in both MCR-negative and MCR-positive groups. In conclusion, mutants from the MCR-positive group exhibited lower fitness costs than mutants from the MCR-negative group, and displayed similar serum resistance.
Discussion
In this study, colistin MICs of in vitro mutants of E. coli are lower than those of other bacteria such as A. baumannii (>256 mg/L). A plausible explanation for this may be that loss of LPS in E. coli could lead to cell death, whereas this is not the case for A. baumannii.20 In other words, loss of LPS may be the mechanism engendering high colistin MICs, whereas modification of LPS leads to lower MICs. In addition, MCR-negative isolates could be induced to higher FCCs than MCR-positive isolates, which indicates that MCR has the capacity to protect bacteria to be induced to high-level colistin resistant mutants from exposure to colistin in vitro.
Isolates in the MCR-negative group tended to possess amino acid changes in chromosomal genes related to colistin resistance, particularly pmrA and pmrB. The lack of such mutations in MCR-positive group indicates that isolates producing MCR are less likely to evolve chromosomally mediated colistin resistance, resulting in lower MICs compared with MCR-negative group. This could explain why MCR-positive isolates tend to have lower MICs in the previous study.13 Mutations observed in PmrB in this study have not been described in the previous studies.
In the DNA level, we discovered that the mutated position of the mutants focuses on PmrAB in the MCR-negative group, while the MCR-positive group possessed less PmrAB mutations (Table 1). In the expression level, we found that expression of pmrAB and pmrAB regulated genes was elevated in all MCR-negative mutants, but it was not always the case in the MCR-positive group. These results suggest that mutations in the sensor kinase PmrB, which might lead to altered expression of the PmrB-regulated genes, could be a common colistin resistance mechanism in E. coli. Furthermore, we hypothesize that the differences of these two groups might because of the expression of MCR, a phosphoethanolamine transferase, could feedback to PmrAB, and affect the expression of pmrAB (PmrB regulates the chromosomal phosphoethanolamine transferase in E. coli). The differences expression pattern of pmrAB and its regulated genes in these two groups indicated that MCR might affect the regulation mechanism of colistin resistance. Further study is needed, especially focusing on the role of MCR in the colistin resistant regulation. The significant discordance in the expression of each gene (Figure 1 A–E) between mutant −1 and −2 for mcr-1 isolates 24,990 and 25,315 was observed. The mechanisms for this phenomenon may because of the different gene mutations other than the known genes between these mutants.
In addition to mutations in genes known to be associated with colistin resistance, mutations in several other genes were also observed in the comparative genomic analysis. Herein, we paid more attention to genes potentially encoding outer membrane components, the target site of polymyxins. Several studies suggest that membrane transporters are involved in colistin resistance,21,22,23,24, but their roles remain poorly understood. In this study, the high frequency of mutations in membrane transporter genes among mutants indicated there may be an important role for membrane transporters in acquired, chromosomal colistin resistance. It is likely that resistance via chromosomal mutations often results from a combination of resistance mechanisms, such as defects in outer membrane proteins combined with a structural modification of LPS. Additionally, the frequency of mutations in genes associated with 2CSs was observed, including EvgS/EvgA, AtoS/AtoC, and KdpE/KdpD. EvgS/EvgA regulates acid resistance genes25 and multidrug efflux pump genes.26 AtoS/AtoC and KdpE/KdpD are associated with cationic iron transporters. When colistin binds to the cell membrane of bacteria, the negatively charged outer membrane is disrupted through electrostatic binding of positively charged regions of colistin.27 Malfunction of cationic iron transporters may increase the concentration of cationic iron around the cell, potentially shielding the outer membrane from neutralization by colistin, and thus reducing the cell’s susceptibility to colistin. These results indicate that membrane transporters and 2CSs play important roles in acquired, chromosomal colistin resistance in E. coli, and provide a potentially interesting area for further study.
Mutations in MCR-negative mutants resulted in a considerably higher cost in terms of fitness than those in MCR-positive mutants compared with their corresponding WTs, a phenomenon that may be associated with the higher colistin MICs of the MCR-negative group mutants. Mutations with higher colistin MICs possessed higher fitness costs were also found in other bacteria, such as A. baumannii.28 Extracellular polysaccharides such as LPS and capsule (K antigen) contribute to virulence in many bacterial pathogens by providing resistance to phagocytosis and protecting against complement-mediated killing, which is often measured by serum resistance. However, mutants in both MCR-negative and MCR-positive groups displayed similar serum resistance to their corresponding WTs, suggesting similar immune defense systems in response to infection.
As the last-line therapy against Gram-negative infection, polymyxins are used when all other treatment modalities have failed. In our study, the colistin susceptibility of MCR-negative and MCR-positive E. coli isolates could be reduced easily in vitro. These results may to some degree, explain the previously reported fact that the mortality was high with polymyxin monotherapy.29 For another, our in vitro data revealed a tendency of induced colistin resistant mutants of MCR-negative E. coli to display high colistin MICs, which might provide reference values for polymyxin dosing in clinical medication, because current polymyxin dosing recommended are largely empirical.30
Conclusion
Our experimental data reveal multiple differences between colistin susceptibility-reduced mutants of MCR-positive and MCR-negative E. coli, including a tendency for mutants of MCR-negative E. coli to display higher colistin MICs, which provide reference values for clinical medication. Until now, the colistin resistance mechanisms of MCR-positive and MCR-negative E. coli still need further studies.
Nucleotide Sequence Accession Numbers
The whole genome sequences described in this paper have been deposited in DDBJ/ENA/GenBank under the accession numbers QYJU00000000-QYKR00000000, (BioProject: PRJNA488336). The accession numbers and the corresponding isolates are listed in supplementary
Acknowledgments
This work was supported by grants from The National Key R&D Program of China (2017YFC1600100), National Natural Science Foundation of China (81702040) and Medical Health Science Projects in Zhejiang Province (2017KY343, 2018KY399).
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Poirel L, Jayol A, Nordmann P. Polymyxins: antibacterial activity, susceptibility testing, and resistance mechanisms encoded by plasmids or chromosomes. Clin Microbiol Rev. 2017;30(2):557–596. doi:10.1128/CMR.00064-16
2. Liu YY, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16(2):161–168. doi:10.1016/S1473-3099(15)00424-7
3. Wang X, Liu Y, Qi X, et al. Molecular epidemiology of colistin-resistant Enterobacteriaceae in inpatient and avian isolates from China: high prevalence of mcr-negative Klebsiella pneumoniae. Int J Antimicrob Agents. 2017;50(4):536–541. doi:10.1016/j.ijantimicag.2017.05.009
4. Cao L, Li X, Xu Y, Shen J. Prevalence and molecular characteristics of mcr-1 colistin resistance in Escherichia coli: isolates of clinical infection from a Chinese University Hospital. Infect Drug Resist. 2018;11:1597–1603. doi:10.2147/IDR.S166726
5. Li Y, Lin X, Yao X, et al. Synergistic antimicrobial activity of colistin in combination with rifampin and azithromycin against Escherichia coli producing MCR-1. Antimicrob Agents Chemother. 2018;62(12):e01631–e01618. doi:10.1128/AAC.01631-18
6. Lee JY, Ko KS. Mutations and expression of PmrAB and PhoPQ related with colistin resistance in Pseudomonas aeruginosa clinical isolates. Diagn Microbiol Infect Dis. 2014;78(3):271–276. doi:10.1016/j.diagmicrobio.2013.11.027
7. Thi Khanh Nhu N, Dw R, Do Hoang Nhu T, et al. The induction and identification of novel Colistin resistance mutations in Acinetobacter baumannii and their implications. Sci Rep. 2016;6:28291. doi:10.1038/srep28291
8. Hua X, Liu L, Fang Y, et al. Colistin resistance in acinetobacter baumannii MDR-ZJ06 revealed by a multiomics approach. Front Cell Infect Micro. 2017;7:45. doi:10.3389/fcimb.2017.00045
9. Fernandez L, Alvarez-Ortega C, Wiegand I, et al. Characterization of the polymyxin B resistome of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013;57(1):110–119. doi:10.1128/AAC.01583-12
10. Quesada A, Porrero MC, Tellez S, Palomo G, Garcia M, Dominguez L. Polymorphism of genes encoding PmrAB in colistin-resistant strains of Escherichia coli and Salmonella enterica isolated from poultry and swine. J Antimicrob Chemother. 2015;70(1):71–74. doi:10.1093/jac/dku320
11. Arena F, Henrici De Angelis L, Cannatelli A, et al. Colistin resistance caused by inactivation of the mgrb regulator is not associated with decreased virulence of sequence type 258 KPC carbapenemase-producing klebsiella pneumoniae. Antimicrob Agents Chemother. 2016;60(4):2509–2512. doi:10.1128/AAC.02981-15
12. Phan MD, Nhu NTK, Achard MES, et al. Modifications in the pmrB gene are the primary mechanism for the development of chromosomally encoded resistance to polymyxins in uropathogenic Escherichia coli. J Antimicrob Chemother. 2017;72(10):2729–2736. doi:10.1093/jac/dkx204
13. Luo Q, Yu W, Zhou K, et al. Molecular epidemiology and colistin resistant mechanism of MCR-Positive and MCR-Negative clinical isolated Escherichia Coli. Front Microbiol. 2017;8:2262.
14. Zhou K, Luo Q, Wang Q, et al. Silent transmission of an IS1294b-deactivated mcr-1 gene with inducible colistin resistance. Int J Antimicrob Agents. 2018;51(6):822–828. doi:10.1016/j.ijantimicag.2018.01.004
15. Rosche WA, Foster PL. Determining mutation rates in bacterial populations. Methods. 2000;20(1):4–17. doi:10.1006/meth.1999.0901
16. Deatherage DE, Barrick JE. Identification of mutations in laboratory-evolved microbes from next-generation sequencing data using breseq. Methods Mol Biol. 2014;1151:165–188. doi:10.1007/978-1-4939-0554-6_12
17. San Millan A, Toll-Riera M, Qi Q, MacLean RC. Interactions between horizontally acquired genes create a fitness cost in Pseudomonas aeruginosa. Nat Commun. 2015;6:6845. doi:10.1038/ncomms7845
18. Liu D, Liu ZS, Hu P, et al. Characterization of surface antigen protein 1 (SurA1) from Acinetobacter baumannii and its role in virulence and fitness. Vet Microbiol. 2016;186(15):126–138. doi:10.1016/j.vetmic.2016.02.018
19. Bachman MA, Breen P, Deornellas V, et al. Genome-Wide Identification of Klebsiella pneumoniae Fitness Genes during Lung Infection. mBio. 2015;6(3):e00775. doi:10.1128/mBio.00775-15
20. Garcia-Quintanilla M, Pulido MR, Moreno-Martinez P, et al. Activity of host antimicrobials against multidrug-resistant Acinetobacter baumannii acquiring colistin resistance through loss of lipopolysaccharide. Antimicrob Agents Chemother. 2014;58(5):2972–2975. doi:10.1128/AAC.02642-13
21. Lin MF, Lin YY, Lan CY. Contribution of EmrAB efflux pumps to colistin resistance inAcinetobacter Baumannii. J Microbiol. 2017;55(2):130–136.
22. Machado D, Antunes J, Simoes A, et al. Contribution of efflux to colistin heteroresistance in a multidrug resistant Acinetobacter baumannii clinical isolate. J Med Microbiol. 2018;67(6):740–749. doi:10.1099/jmm.0.000741
23. Ni W, Li Y, Guan J, et al. Effects of efflux pump inhibitors on colistin resistance in multidrug-resistant gram-negative bacteria. Antimicrob Agents Chemother. 2016;60(5):3215–3218. doi:10.1128/AAC.00248-16
24. Poole K, Lau CH, Gilmour C, Hao Y, Lam JS. Polymyxin susceptibility in pseudomonas aeruginosa linked to the MexXY-OprM multidrug efflux system. Antimicrob Agents Chemother. 2015;59(12):7276–7289. doi:10.1128/AAC.01785-15
25. Eguchi Y, Okada T, Minagawa S, et al. Signal transduction cascade between EvgA/EvgS and PhoP/PhoQ two-component systems of Escherichia Coli. J Bacteriol. 2004;186(10):3006–3014.
26. Nishino K, Yamaguchi A. Overexpression of the response regulator evgA of the two-component signal transduction system modulates multidrug resistance conferred by multidrug resistance transporters. J Bacteriol. 2001;183(4):1455–1458. doi:10.1128/JB.183.4.1455-1458.2001
27. Velkov T, Deris ZZ, Huang JX, et al. Surface changes and polymyxin interactions with a resistant strain of Klebsiella Pneumoniae. Innate Immun. 2014;20(4):350–363. doi:10.1177/1753425913493337
28. Mu X, Wang N, Li X, et al. The effect of colistin resistance-associated mutations on the fitness of acinetobacter baumannii. Front Microbiol. 2016;7:1715. doi:10.3389/fmicb.2016.01715
29. Zusman O, Altunin S, Koppel F, Dishon Benattar Y, Gedik H, Paul M. Polymyxin monotherapy or in combination against carbapenem-resistant bacteria: systematic review and meta-analysis. J Antimicrob Chemother. 2017;72(1):29–39. doi:10.1093/jac/dkw377
30. Gregoire N, Aranzana-Climent V, Magreault S, Marchand S, Clinical pharmacokinetics CW. Pharmacodynamics of colistin. Clin Pharmacokinet. 2017;56(12):1441–1460. doi:10.1007/s40262-017-0561-1
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.