Back to Journals » Clinical Interventions in Aging » Volume 13
Improving well-being in patients with major neurodegenerative disorders: differential efficacy of brief social robot-based intervention for 3 neuropsychiatric profiles
Authors Demange M, Lenoir H, Pino M , Cantegreil-Kallen I, Rigaud AS, Cristancho-Lacroix V
Received 27 September 2017
Accepted for publication 23 December 2017
Published 20 July 2018 Volume 2018:13 Pages 1303—1311
DOI https://doi.org/10.2147/CIA.S152561
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker

Manon Demange,1,2 Hermine Lenoir,1,2 Maribel Pino,1,2 Inge Cantegreil-Kallen,1,2 Anne Sophie Rigaud,1,2 Victoria Cristancho-Lacroix1,2
1Department of Geriatrics, Broca Hospital, Greater Paris University Hospitals (APHP), Paris, France; 2Research Team 4468, Paris Descartes University, Paris, France
Background: Behavioral and psychological symptoms of dementia (BPSD) affect patients’ daily life and subjective well-being. International recommendations stress nonpharmacological interventions as first-line treatment. While newer psychosocial initiatives adapted to geriatric populations based on social robot therapy have emerged, to our knowledge, no studies on differential efficacy depending on BPSD profiles have been conducted yet.
Objectives: This pilot study examined the impact of short exposure to a social robot (Paro®) on the subjective emotional well-being of patients with major neurocognitive disorder as well as its impact on differential effects for 3 BPSD profiles.
Methods: Seventeen patients with major NCD with apathy (n=6), depression (n=7), and agitation (n=4) were recruited. The intervention was composed of four 15-minute individual sessions. Exposure occurred without the simultaneous presence of a health care provider. A pre–post assessment of emotional well-being was conducted with the International Positive and Negative Affect Schedule Short-Form, which measures positive and negative affectivity.
Results: Overall findings showed a significant increase of positive affectivity (p=0.02). Subgroup analysis demonstrated that agitated patients reduced negative affectivity significantly more than depressed patients (p=0.03). Results also confirmed users’ overall acceptability of the robot.
Conclusion: These findings support the usefulness of brief interactive sessions with the Paro robot for elderly patients with major NCD. These preliminary results encourage further research focused on brief interventions using social robotics, as well as on their specific benefits depending on the behavioral typology of patients with neurocognitive disorders.
Keywords: neurodegenerative disorders, agitation, depression, apathy, well-being, social robot
Introduction
Over the past decade, major neurocognitive disorder (NCD) has become a public health priority. According to the World Health Organization and to Alzheimer’s Disease International, more than 110 million people will suffer from major NCD by 2050.1 The increasing number of people living with major NCD raises the question of care, especially when behavioral and psychological symptoms of dementia (BPSD) affect 90% of people at any stage of the disease.2 Apathy is the most frequent BPSD in dementia with a median prevalence rate of 44.5%, followed by depressive (28%), agitation (27%), irritability (25%), and anxiety symptomatology (22.5%), whereas psychosis (18.5%) and delusion (12.5%) are the least frequent ones.3–5 Though the presence of these symptoms is quite heterogeneous among patients,6 its consequences are severe. Indeed, behavioral symptoms increase the risk of hospitalization,7 nursing home placement,8 and the burden of professional and informal caregivers,3,9 and as a consequence lead to increased care costs.10 Moreover, BPSD is negatively correlated to patients’ well-being.11,12
New initiatives based on psychosocial interventions such as social-robot-based therapy have been developed to improve the quality of life of patients and caregivers. Thus, increased interest in the Paro® robot (Intelligent System Co., Kyoto, Japan) has been noted in the recent scientific literature.13 Paro (Figure 1) is an animal-like robot modeled after a baby harp seal. Some authors hypothesized that Paro might improve well-being in older adults because it meets some of their needs – it is companionable, it has the capacity for artificial empathy, it can respond to a person’s voice and touch, and it looks like an unfamiliar animal.14 The later characteristic seems to make it more acceptable to users.15 This kind of pet robot could have promising effects such as those observed with traditional pets, without the disadvantages (eg, hygiene and safety issues).16 Paro triggers with most physical interaction, eye contact, and verbal communication, like a dog.17
  | Figure 1 Paro® robot seal. |
Over the past years, a growing number of studies have assessed the impact of Paro-based therapies on BPSD.16,18–22 These studies have shown a positive impact on emotions and subjective well-being, as well as on feelings of loneliness.16,18 Nevertheless, some methodological aspects limited the generalizability and reproducibility of these studies, such as the lack of control group, a small number of participants, or the unclear research protocol allowing replication.18,22 There is a need for increased studies on Paro impacts to enable the reliability of findings,24 but also to promote the research outcomes’ application into the clinical areas.23,25
There is little literature on the differential effects of social robots depending on neuropsychiatric profiles in geriatric populations. However, we were encouraged by informal observations conducted in our hospital indicating that Paro’s effectiveness may depend on neuropsychiatric profiles. In fact, these observations suggested that agitated patients would benefit more from Paro than patients with symptoms of depression or apathy. To our knowledge, this hypothesis had not been addressed yet. Thus, this research aimed to explore the differential effect of a brief interaction with Paro for 3 neuropsychiatric profiles in a pilot study.
This work tackled 3 main aspects. First, the methodological dimension – a clear, standardized intervention protocol is defined to enable replication. Second, the clinical dimension – not only do we study the overall intervention efficacy, but we also analyze the differential effect of the intervention based on neuropsychiatric profiles. This aims to save health care providers from unrealistic expectations and subsequent burnout,26 as well as to avoid spending unnecessary time and financial resources. Third, we assessed the efficacy of an intervention protocol that could easily be implemented in a real context, with limited resources, by keeping the intervention of the health care provider as short as possible.
Methodology
Participants
This quasi-experimental pilot study was conducted between January and June 2016 in a geriatric hospital in Paris. The 3 units involved in this study admit patients for between 20 days until many years. The geriatrists and nurses were given information about the study protocol during formal meetings and in posters. All the participants (and their legal representatives when necessary) received written and oral information about the protocol in accordance with the Declaration of Helsinki. Only those who gave written consent were included in the study. This study was submitted and approved by the Hospital Broca clinical research committee.
Participants were hospitalized in a geriatric unit and had been diagnosed with major NCD according to the criteria of the Diagnostic and Statistical Manual, 5th Edition.27 Patients scored between 10 and 20 at the Mini Mental State Examination (MMSE),28 and presented one of the following neuropsychiatric symptoms – agitation, apathy, or depression – as measured by the Neuropsychiatric Inventory for Health Staff (NPI-ES).29 Participants who had visual, hearing limitations, or aphasia and could not complete the assessment protocol were excluded. Participants with severe motor deficits who could not physically interact with the Paro robot were also ineligible.
Paro robot
Paro is an animal-like robot modeled after a baby harp seal.30 Paro is covered with white artificial fur and weighs approximately 2.7 kg. It is equipped with light, tactile, and sound-recognition sensors. Paro was designed/developed “to track human motion and pay attention to someone interacting with it.”18,30,31
Assessment and intervention protocols
The pre- and postintervention assessments were conducted by a trained neuropsychologist. Each participant was given 2 weekly sessions of 15 minutes over 2 weeks (Figure 2).
The intervention sessions were conducted in a private room with the patient either sitting or lying on a bed. Each session was video-recorded. Any patient refusal or negative reaction interrupted the session. Consistently with the research study aim (evaluating Paro robot efficacy) during the intervention, the patient only interacted with the Paro robot, with the practitioner leaving the room but waiting in the next room in order to supervise the interaction. In order to control implementation error,32 practitioners were trained to implement this 6-step predetermined protocol:
(a) |
Meeting Paro: the health care providers introduced him/herself and introduced the robot as follows: “I would like to show you Paro, it is a plush coated, animal-like robot. It reacts to your touch and to your voice, so it moves or makes sounds when you touch it or if you talk to it.” The health care providers kept the robot in her/his arms, and showed the patient how to touch the robot’s back, whiskers, or head. |
(b) |
Proposing contact and modeling: the health care providers handed the robot to the patient and asked if he/she wished to try by him/herself. If the patient agreed, the health care providers placed it in his/her arms, or on a nearby chair or table if necessary. Again, the health care provider showed how to touch the robot’s back, whiskers, or head, and encouraged the patient to touch it: “You can hold it in your arms, cuddle it, talk to it, and caress it if you want.” |
(c) |
Using Paro individually (I): if the participant accepted to touch Paro, the health care providers offered to let the participant to use Paro alone for a brief period of time (7 minutes 30 seconds). If the participant accepted, the health care providers added: “Ok, I will leave the room for you to be alone with the robot, but I will be by the door, you can call me if you need anything.” Whenever the patient asked for help or refused to continue, the session was interrupted. No persuasive arguments were used when the participant refused. The health care providers just asked why and asked if the participant was willing to try it another day. |
(d) |
Mid-session checking: the health care providers came back to the room and checked whether the participant agreed to continue the interaction. If the patient accepted, the health care providers repeated: “I will be by the door, you can call me if you need anything” and left the room. |
(e) |
Using Paro individually (II): participants were given additional time (7 minutes 30 seconds) with Paro. The session was interrupted at any moment if the patient asked for help, or refused to continue, whatever the reason was. If the patient seemed disoriented or did not understand the context, the health care professional acted reassuringly and mitigated the feeling of uneasiness. |
(f) |
Ending exposure: after 15 minutes (less when the sessions were interrupted), the health care professional asked the participant for brief feedback on how he/she experienced this time. Due to frequent memory impairment in these participants, it was necessary to check that each participant still agreed to continue after each session. |
Measures
Primary outcome: emotional well-being
Kahneman et al33 underline the strong influence of emotional experiences on subjective evaluations. As stated by these authors “an individual who was recently experienced mostly negative effects is unlikely to describe herself as very happy or satisfied.”33 Thus, we hypothesized that a pleasant experience might increase the subjective perception of well-being by improving positive effects and diminishing negative ones, as assessed by the International Positive and Negative Affect Schedule Short-Form (I-PANAS SF),34,35 one of the most common scale used to evaluate positive and negative effects.
The 10-item scale measures positive (determined, attentive, active, inspired, alert) and negative (upset, hostile, ashamed, nervous, afraid) affects through simple sentences. Individuals have to answer the question “Thinking about yourself and how you normally feel, to what extent do you generally feel” by rating each affect on a Likert scale from never (1) to always (5). The I-PANAS SF scale offers a subscale score for positive affectivity (PA) and negative affectivity (NA), each one scoring between 5 and 25, with higher scores representing a higher mood level (positive or negative).
Secondary outcome: robot’s usability and perception
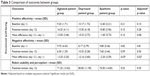
Paro’s usability was subjectively measured by participants with the System Usability Scale (SUS) after the intervention.36 This scale is composed of 10 statements measuring Paro’s perceived effectiveness, efficiency, and satisfaction, with a 5-point Likert scale from strongly disagree (1) to strongly agree (5). The total score varies from 0 to 100 with a cutoff of 68 (Table 1).
  | Table 1 Usability and perception measures of Paro® robot |
We also measured with a 3-point Likert scale the perceived intrusiveness, infantilizing, and stigmatization, when using Paro (Table 1).
Controlled variables
Cognitive status was measured with the MMSE. This scale is the most common instrument to screen global cognitive status in aging people.28 This 11-item scale evaluates 5 cognitive functions: orientation, immediate memory, attention, calculation, short-term memory, and language functions. This scale ranges from 0 to 30. Higher scores are interpreted as better cognitive status.
Neuropsychiatric symptoms were assessed with the NPI-ES.29 This French version of the NPI was mainly developed to evaluate 12 different neuropsychiatric symptoms of patients with NCD, living in a geriatric unit or in a nursing home, based on reports by health care staff. In this study, only the scores for apathy, depression, and anxiety were analyzed. The cutoff score selected for each neuropsychiatric symptom was 3. Total scores ranged from 0 to 12. When a participant displayed more than 1 neuropsychiatric symptom, the predominant symptom was retained after clinical confirmation by the patient’s geriatrist.
Data analysis
Participants’ anonymity was preserved while conducting data analysis. Participants’ characteristics were described using means, SDs, and percentages for categorical variables.
After checking normality and homoscedasticity of primary outcome (emotional well-being) using Shapiro–Wilk and Brown–Forsythe tests, respectively, a general linear model, repeated measures analysis of variance, was used on I-PANAS SF scores across pre- and postintervention assessments.
Then, Kruskal–Wallis nonparametric test was used when data did not meet assumptions to use parametric analysis, to test for differences between each behavioral profile on I-PANAS SF scores.
Finally, Pearson linear correlations were drawn between primary outcome and robot’ usability and perception measurements.
All analyses were conducted using Statistica 10.0 software (Statsoft®, Tulsa, OK USA).37 A 2-tailed α level of <0.05 was adopted.
Qualitative data of patients’ behavioral and verbal manifestation during the interaction were informally analyzed. Each recorded intervention was examined by a trained psychologist (MD) who was briefed on the thematic analysis method (Braun and Clarke38), though the verbalizations were not transcribed. For that, verbal and nonverbal manifestations were noted, classified into emerging themes and categories of behaviors, then discussed and validated with investigators. For the purpose of the current publication, verbal interactions were translated from French to English and verified by two bilingual neuropsychologists (VCL and MD).
Results
As summarized in the flowchart (Figure 3), out of 24 hospitalized patients screened, 7 refused to participate for 3 main reasons: 1) being uninterested in robots (n=4), 2) finding the robot “childlike” (n=2), and 3) refusing all care (n=1). No significant sociodemographic or clinical differences were found between the patients who accepted and those who refused the intervention.
  | Figure 3 Flowchart of the quasi-experimental pilot study. |
Most of the participants were women (80%), aged 77–95 (mean =83 y/o, SD =7.9). The MMSE mean score was 16.1 (SD =3.9). The participants’ sociodemographic characteristics are summarized in Table 2. The cognitive and sociodemographic variables of the 3 neuropsychiatric groups were similar.
In terms of adherence, 88% of the participants completed at least 3 sessions out of the 4 sessions initially planned and 76% (n=15) completed all the sessions. Two patients were excluded because of adverse events after 2 therapeutic sessions. One patient suffered from an acute physical disease. Though this impeded the intervention, it seemed unrelated to the robot exposure. The second patient had nightmares on the night following the Paro session which subsided the next day. Since this might have been due to the interaction with Paro, the patient was excluded from the study to prevent further sleep disturbances.
Primary outcome: emotional well-being
Regardless of patient profile, the results showed an overall significant difference (t[14] =–2.15, p=0.02) between pre- and post-measures of positive affectivity, as assessed by the I-PANAS SF (Figure 4). No significant intervention effect was found on negative affect scores between pre- and postintervention assessments (t[14] =0.88, p=0.19).
  | Figure 4 Overall affectivity scores pre- and postintervention. |
Further analysis of the differential impact of the intervention for each behavioral profile (apathetic, agitated, and depressed) was also conducted. Thus, the Kruskal–Wallis test and post hoc analysis of NA between the 3 groups showed that the scores of depressed patients differed significantly from those with agitation (H[2,15] =6.98, p=0.03). NA decreased in patients with agitation than in patients with depression (Table 3). No statistical differences were found between the apathetic group and the other groups (depressed and agitated patients).
  | Table 3 Comparison of outcomes between groups |
Secondary outcome: robot usability and perception
The mean patient score on the SUS scale regarding the robot-based intervention was 76.17 (SD =13.05) with minimal and maximal scores of 52.5 and 97.5, respectively. The mean score was higher than the cutoff score of 68 provided for SUS. No significant differences were observed between groups (Table 3). Analyses of linear correlations also showed that higher acceptance level was positively associated with the improvement of PA reported between baseline and the follow-up period (r =0.56; p<0.05). Overall most participants in the study had higher negative than positive reactions (“strongly disagree”, “tend to disagree”) in respond to the robot’s qualifying adjectives. This trend concerns 60% of participants for the item “I think that Paro is childish” and 67% for the item “I think that Paro is stigmatizing”. For the item “intrusive”, reactions were more divided among participants.
Qualitative analysis
Qualitative analysis of the interaction between the patient and Paro’s robot enabled to identify 3 main topics, as shown in Table 4.
- Expression of emotional feelings: most of the patients displayed verbal and/or nonverbal affective behaviors toward the robot such as caresses, smiles, kisses, and hugs during the interaction with Paro. They also communicated and shared feelings and moods with Paro.
- Interpretation of Paro’s behavior: patients tried to understand or to explain Paro’ behavior. For instance, they compared its movements and sounds with behaviors in other well-known situations (eg, for the patients the robot’s sounds mean that the robot is crying). In some cases, patients ascribed human feelings to Paro.
- Triggering memories: during and after exposure, nearly 30% (5/17) of participants mentioned to investigators and health care providers that Paro had triggered positive or negative past memories.
Discussion
This study aimed to evaluate the impact of a brief intervention with Paro on the subjective emotional well-being of hospitalized older adults with major NCD displaying 3 different neuropsychiatric profiles.
Our findings showed that a brief Paro-based intervention of a few individual sessions and without the simultaneous physical presence of a health care provider may significantly increase PA as measured by the I-PANAS SF, and this is regardless of participants’ neuropsychiatric profile. While studies evaluating individual or group interventions with Paro conclude the improvement of well-being of patients with major NCD, many of these have different methodological limitations, notably the lack of a control group or small sample-sizes. Moreover, these effects are found after longer intervention periods.22,39,40 In this regard, the present study has fostered a brief, innovative, and possibly cost-effective intervention.
Further analysis of the differential impact of the intervention in 3 groups (agitated, apathetic, and depressed) was also conducted. We could confirm the previous clinical impressions based on the clinical staff’s informal observations. We found a higher impact of the intervention in agitated patients compared to depressed patients. In fact, agitated patients showed a significant decrease of NA in comparison with depressed patients. This differential effect might be explained by the distinctive factors associated with agitation (behavioral disturbance) and depression (mood disturbance) in major NCD.41 Agitation seems related to disturbing environmental stimuli (eg, disruption of routines, lack of relatives, or under- or overstimulation),42,43 while depressive symptoms which may begin in adulthood or in late life could be due to various causes and could often be associated with atrophy of subcortical and amygdala regions when they begin in late life.2,41 In accordance with our results, a literature review reports positive effects of stimulation-oriented approaches on patients with major NCD with agitation,44 such as massage and touch, aromatherapy, music therapy, or animal-assisted therapy. Paro’s effect on agitated patients was attributed to the acute calming effect of tactile stimulation23,45 and to a reduction of cortisol levels.46–48 Also, Robinson et al49 have shown significant reduction in systolic and diastolic blood pressure, suggesting that a pet robot could provide an experience that buffers stress reactions.49 Nevertheless, since these studies are for the most in a pilot stage, the conclusions should be considered cautiously.
Globally, the positive effect on well-being resulting from Paro-based interventions was described regardless of the psychometric instrument used (eg, The Faces scales, The Dementia Care Mapping™, University of Bradford, Bradford, UK). Based on definitions of well-being,50,51 individuals’ subjective emotional perception would influence the levels of their subjective well-being in this study. We chose the I-PANAS SF to measure the subjective well-being linked to the individual’s current positive and NA. Thus, we hypothesized that interacting with Paro would influence the individuals’ affects, while their moods would remain stable in the short-term. Interestingly, this scale offers an affect measure within a continuum ranging from negative to positive mood, whereas most of the tools only assess improvement of positive feelings. We thought that targeting the reduction of negative feelings would also be a useful measure especially in patients in medium- or long-stay facilities, who may suffer from pain or/and other chronic illness.
The dimensions of usability and perception were also analyzed since these variables are known to significantly influence pharmacological and nonpharmacological outcomes.52,53 In the present study, findings are entirely consistent with this. Usability positively affected the impact of the intervention. Thus, a positive correlation was observed between levels of usability and the improvement of PA after the intervention. It should be noted that the average score of usability was very high, regardless of neuropsychiatric profile. However, this study also revealed a higher percentage of refusals than these described in the literature. Two reasons for refusals were particularly highlighted: being uninterested in robots (n=4) and finding the robot “childlike” (n=2). Hence, in spite of Paro’s positive impact, its use might be constrained by attitudes toward robots.54
Informal qualitative analysis of video recordings enabled us to identify different kinds of interactions between the patient and the robot, when no one else was in the room. It should be noted that no negative reactions were observed, but spontaneous, empathetic reactions were. For instance, most of the participants demonstrated positive verbal or nonverbal affective behaviors toward Paro.55 Interestingly some participants tried to understand or seemed to interpret Paro’s behavior(s). They also brought up memories during or after the sessions.54
In our study, only one participant had a negative reaction possibly linked to exposure to the robot (nightmares following the session). This possible reaction led us to believe that an interview about the patient’s history would be necessary to prevent negative reactions during or after the interaction with Paro.
Limitations and perspectives
Despite our efforts to conform to methodological standards over the course of this study, we have to underline some limitations.
First, the protocol calls for larger sample size, participants’ follow-up, and a control group to improve the reliability of these results. Second, the recruitment was based on pragmatic sampling and included mostly women (80%). This gender imbalance may skew the analyses. In fact, Miller et al56 have described in a small sample, a significant difference in women’s serum oxytocin levels pre- and postinteraction with their dogs, while this difference was not observed in men. Third, some factors that may affect subjective well-being were not controlled. For instance, the modification of pharmacological treatment in patients suffering from pain or other comorbidities during the intervention should be taken into account.57 Fourth, the studies assessing behavioral disorders (eg, screaming, wandering, etc) seem warranted after a short exposure to Paro. Fifth, the choice of the I-PANAS SF scale limited the profile of recruited patients, since it demanded that patients be able to understand questions and produce coherent answers. Thus, we had to exclude patients with severe stages of major NCD, whereas other studies have reported higher effects of animal-like robots in these patients.25 Sixth, early-onset depression should be distinguished from late-onset depression, and neuropsychiatric comorbidities should be identified, to control these confounding variables.41 Finally, as mentioned earlier investigating patients’ past experience, will help to limit the consequences of negative reminiscences (as much as possible).
Conclusion
This study shows that a brief intervention using Paro without the simultaneous physical presence of a health care provider appears to improve the psychological well-being in patients with major NCD. Interestingly, analysis also revealed a differential effect depending on the neuropsychiatric profile. The intervention reduced the NA of agitated patients more significantly than those of depressed patients. From a qualitative perspective, Paro seems to stimulate PA and the reminiscing of memories. These results have paved the way for further research into short Paro robot exposure in patients with major NCD with neuropsychiatric problems.
Acknowledgments
This study was funded by the Group La Dynamique du Vieillir [Dynamics of Aging Group] (Programs Interdisciplinaires [interdisciplinary research program], Sorbonne Paris Cité [a research association of universities and higher education institutions in Paris and Seine-Saint-Denis] 2013–2017) and by La Fondation de France [a philanthropic foundation in France].
Disclosure
The authors report no conflicts of interest in this work.
References
Prince MJ. World Alzheimer Report 2015: The Global Impact of Dementia: An Analysis of Prevalence, Incidence, Cost and Trends. London, UK: Alzheimer’s Disease International; 2015. | ||
Cerejeira J, Lagarto L, Mukaetova-Ladinska EB. Behavioral and psychological symptoms of dementia. Front Neurol. 2012;3:73. | ||
Fauth EB, Gibbons A. Which behavioral and psychological symptoms of dementia are the most problematic? Variability by prevalence, intensity, distress ratings, and associations with caregiver depressive symptoms. Int J Geriatr Psychiatry. 2014;29(3):263–271. | ||
Bergh S, Engedal K, Røen I, Selbæk G. The course of neuropsychiatric symptoms in patients with dementia in Norwegian nursing homes. Int Psychogeriatr. 2011;23(8):1231–1239. | ||
Robert PH, Verhey FR, Byrne EJ, et al. Grouping for behavioral and psychological symptoms in dementia: clinical and biological aspects. Consensus paper of the European Alzheimer disease consortium. Eur Psychiatry. 2005;20(7):490–496. | ||
Tschanz JT, Corcoran CD, Schwartz S, et al. Progression of cognitive, functional, and neuropsychiatric symptom domains in a population cohort with Alzheimer dementia: the Cache County Dementia Progression study. Am J Geriatr Psychiatry. 2011;19(6):532–542. | ||
Voisin T, Andrieu S, Cantet C, Vellas B; REAL.FR Group. Predictive factors of hospitalizations in Alzheimer’s disease: a two-year prospective study in 686 patients of the REAL.FR study. J Nutr Health Aging. 2010;14(4):288–291. | ||
Hersch EC, Falzgraf S. Management of the behavioral and psychological symptoms of dementia. Clin Interv Aging. 2007;2(4):611–621. | ||
Song JA, Oh Y. The association between the burden on formal caregivers and behavioral and psychological symptoms of dementia (BPSD) in Korean elderly in nursing homes. Arch Psychiatr Nurs. 2015;29(5):346–354. | ||
Herrmann N, Tam DY, Balshaw R, et al. The relation between disease severity and cost of caring for patients with Alzheimer disease in Canada. Can J Psychiatry. 2010;55(12):768–775. | ||
Gómez-Gallego M, Gómez-Amor J, Gómez-García J. Determinants of quality of life in Alzheimer’s disease: perspective of patients, informal caregivers, and professional caregivers. Int Psychogeriatr. 2012;24(11):1805–1815. | ||
Beerens HC, Zwakhalen SM, Verbeek H, Ruwaard D, Hamers JP. Factors associated with quality of life of people with dementia in long-term care facilities: a systematic review. Int J Nurs Stud. 2013;50(9):1259–1270. | ||
Goeldner M, Herstatt C, Tietze F. The emergence of care robotics – a patent and publication analysis. Technol Forecast Soc Change. 2015;92:115–131. | ||
Hutson S, Lim SL, Bentley PJ, Bianchi-Berthouze N, Bowling A. Abstract presented at: International Conference on Affective Computing and Intelligent Interaction; October 9–12, 2011; Memphis, TN, USA. | ||
Shibata T. An overview of human interactive robots for psychological enrichment. IEEE. 2004;92(11):1749–1758. | ||
Petersen S, Houston S, Qin H, Tague C, Studley J. The utilization of robotic pets in dementia care. J Alzheimers Dis. 2017;55(2):569–574. | ||
Thodberg K, Sørensen LU, Videbech PB, et al. Behavioral responses of nursing home residents to visits from a person with a dog, a robot seal or a toy cat. Anthrozoös. 2016;29(1):107–121. | ||
Broekens J, Heerink M, Rosendal H. Assistive social robots in elderly care: a review. Gerontechnology. 2009;8(2):94–103. | ||
De Sant’ Anna M, Morat B, Rigaud AS. [Adaptabilité du robot Paro dans la prise en charge de la maladie d’Alzheimer sévère de patients institutionnalisés]. NPG Neurologie-Psychiatrie-Gériatrie. 2012;12(67):43–48. French. | ||
Roger K, Guse L, Mordoch E, Osterreicher A. Social commitment robots and dementia. Can J Aging. 2012;31(1):87–94. | ||
Soler MV, Agüera-Ortiz L, Rodríguez JO, et al. Social robots in advanced dementia. Front Aging Neurosci. 2015;7:133. | ||
Jøranson N, Pedersen I, Rokstad AM, Ihlebaek C. Change in quality of life in older people with dementia participating in Paro-activity: a cluster-randomized controlled trial. J Adv Nurs. 2016;72(12):3020–3033. | ||
Mordoch E, Osterreicher A, Guse L, Roger K, Thompson G. Use of social commitment robots in the care of elderly people with dementia: a literature review. Maturitas. 2013;74(1):14–20. | ||
Moyle W, Jones CJ, Murfield JE, et al. Use of a robotic seal as a therapeutic tool to improve dementia symptoms: a cluster-randomized controlled trial. J Am Med Dir Assoc. 2017;18(9):766–773. | ||
Smits C, Anisuzzaman S, Loerts M, Valenti-Soler M, Heerink M. Towards practical guidelines and recommendations for using robotics pets with dementia patients. Can Int J Soc Sci Educ. 2015;3:656–670. | ||
Schaufeli WB, Salanova M. Efficacy or inefficacy, that’s the question: Burnout and work engagement, and their relationships with efficacy beliefs. Anxiety Stress Coping. 2007;20(2):177–196. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Association; 2013. | ||
Folstein MF, Folstein SE, Mchugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. | ||
Sisco F, Taurel M, Lafont V, et al. Les troubles du comportement chez le sujet dément en institution: évaluation à partir de l’inventaire neuropsychiatrique pour les équipes soignantes (NPI/ES). L’Année Gérontologique. 2000;14:151–171. | ||
Shibata T, Wada K. Robot therapy: a new approach for mental healthcare of the elderly – a mini-review. Gerontology. 2010;57(4):378–386. | ||
Calo CJ, Hunt-Bull N, Lewis L, Metzler T. Ethical implications of using the Paro robot, with a focus on dementia patient care. Paper presented at: 2011 AAAI Workshop; Conference: Human-Robot Interaction in Elder Care; August 7–11, 2011; San Francisco, CA, USA. | ||
Vernooij-Dassen M, Moniz-Cook E. Raising the standard of applied dementia care research: addressing the implementation error. Aging Ment Health. 2014;18(7):809–814. | ||
Kahneman D, Diener E, Schwarz N. Well-Being: Foundations of Hedonic Psychology. New York, NY: Russell Sage Foundation; 1999. | ||
Thompson ER. Development and validation of an internationally reliable short-form of the positive and negative affect schedule (PANAS). J Cross-Cult Psychol. 2007;38(2):227–242. | ||
Bruchon-Schweitzer M, Boujut E. Psychologie de la santé: Modèles, concepts et méthodes. 2nd ed. Dunod; 2014. | ||
Brooke J. System usability scale (SUS): a quick-and-dirty method of system evaluation user information. Reading, UK: Digital Equipment Co Ltd; 1986. | ||
Statistica S. 10.0 (data analysis software system); 2012. | ||
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. | ||
Inoue K, Wada K, Uehara R. How effective is robot therapy? Paro and people with dementia. In: 5th European Conference of the International Federation for Medical and Biological Engineering; September 14–18; 2011; Budapest. | ||
Bemelmans R, Gelderblom GJ, Jonker P, de Witte L. Effectiveness of robot Paro in intramural psychogeriatric care: a multicenter quasi-experimental study. J Am Med Dir Assoc. 2015;16(11):946–950. | ||
Abou-Saleh MT, Katona C. Principles and Practice of Geriatric Psychiatry. Hoboken, NJ: John Wiley & Sons; 2011. | ||
Cohen-Mansfield J, Werner P. Predictors of aggressive behaviors: a longitudinal study in senior day care centers. J Gerontol B Psychol Sci Soc Sci. 1998;53(5):P300–P310. | ||
Kunik ME, Martinez M, Snow AL, et al. Determinants of behavioral symptoms in dementia patients. Clin Gerontol. 2003;26(3–4):83–89. | ||
O’Neil ME, Freeman M, Christensen V, Telerant R, Addleman A, Kansagara D. A systematic evidence review of non-pharmacological interventions for behavioral symptoms of dementia. Washington, DC: Department of Veterans Affairs; 2011. | ||
Jøranson N, Pedersen I, Rokstad AM, Ihlebæk C. Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: a cluster-randomized controlled trial. J Am Med Dir Assoc. 2015;16(10):867–873. | ||
Wada K, Shibata T. Living with seal robots – its sociopsychological and physiological influences on the elderly at a care house. IEEE Trans Robot. 2007;23(5):972–980. | ||
Saito T, Shibata T, Wada K, Tanie K. Examination of change of stress reaction by urinary tests of elderly before and after introduction of mental commit robot to an elderly institution. In: Proceedings of the Seventh International Symposium on Artificial Life and Robotics; January 16–18; 2002; Oita, Japan. | ||
Chau D, Osborne TF. Using Technology to Improve Care of Older Adults. New York: Springer Publishing Company; 2017. | ||
Robinson H, Macdonald B, Broadbent E. Physiological effects of a companion robot on blood pressure of older people in residential care facility: a pilot study. Australas J Ageing. 2015;34(1):27–32. | ||
Diener E. New findings and future directions for subjective well-being research. Am Psychol. 2012;67(8):590–597. | ||
Diener E, Oishi S, Lucas RE. Personality, culture, and subjective well-being: emotional and cognitive evaluations of life. Annu Rev Psychol. 2003;54:403–425. | ||
Sabate E. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. | ||
Jin J, Sklar GE, Oh VMS, Li SC. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–286. | ||
Wu YH, Pino M, Boesflug S, et al. Robots émotionnels pour les personnes souffrant de maladie d’Alzheimer en institution. NPG Neurologie-Psychiatrie-Gériatrie. 2014;14(82):194–200. | ||
Takayanagi K, Kirita T, Shibata T. Comparison of verbal and emotional responses of elderly people with mild/moderate dementia and those with severe dementia in responses to seal robot, PARO. Front Aging Neurosci. 2014;6:257. | ||
Miller SC, Kennedy CC, DeVoe DC, Hickey M, Nelson T, Kogan L. An examination of changes in oxytocin levels in men and women before and after interaction with a bonded dog. Anthrozoös. 2009;22(1):31–42. | ||
Achterberg WP, Pieper MJC, van Dalen-Kok AH, et al. Pain management in patients with dementia. Clin Interv Aging. 2013;8:1471–1482. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



