Back to Journals » Clinical Ophthalmology » Volume 16
Improving Medical Students’ Awareness About Retinoblastoma: A Practical Strategy
Authors Elfalah M , AlNawaiseh T , Atoum D, AlKhassawneh A, Mohammad M, AlNawaiseh I, Yousef YA
Received 26 December 2021
Accepted for publication 11 February 2022
Published 7 June 2022 Volume 2022:16 Pages 1807—1814
DOI https://doi.org/10.2147/OPTH.S355876
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mutasem Elfalah,1 Tamara AlNawaiseh,1 Dima Atoum,2 Ahmad AlKhassawneh,2 Mona Mohammad,3 Ibrahim AlNawaiseh,3 Yacoub A Yousef3
1School of Medicine, The University of Jordan, Amman, Jordan; 2School of Medicine, AlYarmouk University, Irbid, Jordan; 3Department of Surgery (Ophthalmology), King Hussein Cancer Center, Amman, Jordan
Correspondence: Yacoub A Yousef, Department of Surgery (Ophthalmology), King Hussein Cancer Center, Queen Rania Al-Abdullah Street, P.O Box 1269, Amman, 11941, Jordan, Tel +00962787228749, Email [email protected]
Background: Eye salvage and survival for patients with retinoblastoma (RB) can be improved by enhancement of early diagnosis. This study aims to investigate the impact of modifying the teaching curriculum for medical students about awareness of this condition.
Methods: Medical students completed a questionnaire about RB, preluded by a photograph of a child with leukocoria. Participants were divided into group A (138 participants) and group B (151 participants) who are medical students who have completed the ophthalmology rotation before and after implementing modifications on teaching curriculum that focuses on the red flags of RB consecutively.
Results: Most participants considered leukocoria an abnormal sign. Group A had significantly lower knowledge about diagnosis for RB (P=0.0001). Participants scored higher in group B for the critical questions, such as knowing that RB is a fatal disease (P=0.041) that needs urgent treatment (P=0.042). Only three (2%) students adopted the “watch and wait” strategy in group B, compared to 16 (12%) in group A (P=0.0013). Overall, proficiency score (≥ 90%) was achieved by 12 (8%) students in group B, but only three (2%) students in group A. Only 41 (27%) students in group B, compared to 90 (65%) students in group A, failed to obtain a sufficiency score (≥ 70%) in the questionnaire.
Conclusion: Modifying the teaching curriculum of the ophthalmology rotation with an intensified focus on awareness of the life-threatening condition retinoblastoma improved medical students’ knowledge of this malignancy. This intervention is one of the modalities that can lead to a reduction in diagnosis and referral delays and improvement in outcome and survival.
Keywords: leukocoria, medical students, retinoblastoma
Introduction
Retinoblastoma (RB) is the most common intraocular malignancy in children,1,2 and leukocoria in infants could be a sign of a life threatening malignancy like RB, infectious disease like toxocariasis, congenital anomaly like persistent fetal vasculature (PFV), and others like retinopathy of prematurity or Coats’ disease.2 Globally, RB affects one in 15,000–20,000 live births, and 90% of them are 5 years old or younger at time of diagnosis.1,3 The incidence in Jordan is 9.32 cases per million children who are 5 years old or younger,3 and one fifth (20%) of them have familial RB, compared to only 10% in western countries.3,4
Treatment modalities for RB have improved significantly over the past 2 decades, and this, side-by-side with early diagnosis, has improved the prognosis in terms of survival and globe salvage. However, delayed diagnosis, mainly in developing countries, is still a major poor prognostic factor for management outcome, therefore prompt recognition of the common RB signs and symptoms by parents and healthcare providers is very important.5–7
The most common presenting sign for RB is leukocoria (50–60% of cases), and this is seen when the tumor size is large enough to be detected by parents. The second and third most common presenting signs are strabismus (25%) and ocular inflammation (6–10%).8–11 These alarming signs are very important to be recognized by health care givers to avoid delayed diagnosis. Unfortunately, a previous questionnaire about the level of knowledge about RB and its presenting signs among first contact physicians in Jordan showed a major deficiency in knowledge about the need for immediate referral of patients with signs of RB. Furthermore, 45% of graduated medical students failed to recognize leukocoria as a possible sign of a life-threatening malignancy.12 This indicated a defect in the teaching system for medical students.
Medical students will be the first-contact health care providers for children with signs of RB in the future. The aim of this study is to analyze the impact of modifying their teaching curriculum in a way that focuses on the red flags and signs of RB, and on medical students’ awareness level and basic knowledge about RB.
Methods
The institutional review board (IRB) committee at The University of Jordan and King Hussein Cancer Center, Amman, Jordan approved this cross-sectional study. Ocular oncologists treating RB in Jordan designed and prepared the questionnaire, based on data taken from relevant literature on RB. All participants provided informed consent to participate in this questionnaire. Thereafter, participants were shown a mid-face photo of a child with right eye leukocoria (Figure 1), and were asked clear clinical questions to evaluate their decision-making skills; such as recognizing the normal vs abnormal eye, methods for diagnosis of RB, and the need for immediate referral for treatment vs observation. (Supplementary Table). It was not possible to demonstrate the change in scores of the same group of students before and after the focused learning on RB. Therefore, we compared the scores between students who completed the ophthalmology rotation after implementing the focused RB learning, and the scores of a heterogeneous group of medical students from different medical schools in Jordan, who completed ophthalmology rotations that lacked the focused RB learning, and this group is expected to be representative of the medical graduates in the country.
 |
Figure 1 A mid-face photo for a child with unilateral retinoblastoma who presented with right white pupil reflex (leukocoria), while the left eye was normal. |
Participants were divided into two groups; group A, students in the 6th year of medical school (that is the last year in medical school in Jordan), who underwent a 2-week rotation in the department of ophthalmology (during their 5th year of medical school) before implementing modifications on the teaching curriculum that highlights and focuses on the red flags of RB. And group B, students in the last 2 months of their 6th year of medical school (that is 1–2 years after completing the ophthalmology rotation in the 5th year of medical school), who underwent a 2-week rotation in the department of ophthalmology (during their 5th year of medical school) after implementing modifications on the teaching curriculum that highlight and focuson the red flags of RB. Participants who failed to complete the survey were excluded from this study. The modifications on the teaching curriculum included adding a standing item that includes discussing a photo with leukocoria with all students during the ophthalmology rotation in the 5th medical year. In addition, a standing question in the final exam was mandated to be about a photo with leukocoria. The discussion about the photo with leukocoria was done under the supervision of ME at The University of Jordan (UoJ) and YAY at Al Yarmouk University (YU).
The participants were asked to complete the questionnaire. Responses of both groups were analyzed for descriptive statistics. The score was calculated based on the assumption that the answer was either correct or not. The knowledge level was based on cut-off scores (70% for sufficiency and 90% for proficiency). Each student’s score was calculated, as well as an overall score for each group. Participants for this study were final year medical undergraduates recruited from four universities in Jordan.
The questionnaire was constructed in survey format and distributed to participants using Survey Monkey (SurveyMonkey Inc. San Mateo, CA, USA). The first section of the survey was about students’ demographics, followed by 19 multiple-choice questions distributed as follows: clinical scenario (3), diagnosis (6), general aspects (8), and referral (2) including one colored image of leukocoria and one clinical scenario. Sixty-two initial responses were used to validate the questionnaire, internal consistency was demonstrated by a Cronbach’s alpha of 0.80, and therefore the questionnaire was not altered.
The modified teaching curriculum highlights and focuses on the red flags of RB, and on medical students’ level of basic knowledge about RB. One standard 1-hour educational seminar for 5th year medical students starts with a photo of a child with leukocoria. The discussion included all the differential diagnoses and approach for a child with leukocoria, starting with life-threatening causes (RB), sight-threatening causes, and others. Furthermore, a standing question in the final written exam was about the approach for leukocoria.
Results
This was a 19 multiple-choice questions questionnaire, and 138 medical students in Group A and 151 medical students in Group B answered it completely. Tables 1 and 2 show the demographics of the participants, and the detailed results of the final test (correct vs incorrect) of every single question for all the participants in both groups. For group B, out of 151 participants, 103 were from the University of Jordan and 48 from Al-Yarmouk University.
 |
Table 1 Demographics of the Participants of the Survey* |
 |
Table 2 Questionnaire Results |
Comparison Between Participants in Group A and Group B
Overall, proficiency score (≥90%) was achieved by 12 (8%) students in Group B, but only three (2%) students in Group A. Only 41 (27%) students in Group B compared to 90 (65%) students in Group A failed to obtain a sufficiency score (≥70%) in the questionnaire (Table 3).
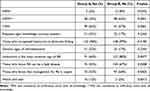 |
Table 3 Most Significant Findings of the Questionnaire |
In addition, participants generally scored higher in Group B mainly for the critical questions about the level of danger for RB, as they identified leukocoria as the most common sign for RB (P=0.007), knew that RB is a fatal disease (P=0.041), and that treatment is urgently required (P=0.042) better than Group A. Only three (2%) adopted the “watch and wait” strategy in Group B, compared to 16 (12%) in Group A (P=0.0013) (Table 3).
The abnormal eye was recognized by most of the participants, with no significant difference between the two groups (P=0.05). Group A had significantly lower knowledge about how to diagnose RB (P=0.0001) and 126 (83%) from Group B were familiar with the pathogenesis of RB compared to 96 (67%) from Group A (P=0.008). Both groups had similar answers when asked about signs of RB (P=0.234), the specialty that treats RB (P=0.36), and in which specialized center in Jordan (P=0.27) (Table 2).
Comparison Between Participants from the Two Different Medical Schools in Group B
Responses from students of both the University of Jordan (UoJ) and Al-Yarmouk University (YU) did not show a significant difference in the level of knowledge in this questionnaire. Both sub-groups were able to diagnose RB (P=0.237), knew the presenting signs of RB (P=0.642), were familiar with the pathogenesis (P=0.489), and knew who should treat this disease (P=0.307). However, students at YU had a greater knowledge about the most common sign being leukocoria, where 44 (92%) answered this question correctly compared to only 77 (75%) at UoJ. Students at YU also knew how to ideally diagnose RB, where 27 (56%) answered correctly, while only 41 (40%) had a correct answer at UoJ. Of interest, almost 50% of participants in both groups still did not know that RB is a fatal disease (Table 4).
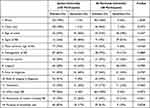 |
Table 4 Comparison Between Two Different Medical Schools in Group B |
Discussion
Awareness about the common signs of RB among both parents and first-contact physicians are the main keys to improve the outcome of management for RB as they should enhance early recognition, and prompt referral for accurate treatment.5–7,12 Our study here showed that improving the teaching strategies, with a modified teaching curriculum that focuses on the red flags for RB, could significantly improve the level of knowledge about presenting signs of RB among medical students, who will be the first contact physicians in the future. In return, that should increase the chance of early identification, early diagnosis, higher survival, and better eye and vision salvage rates. However, physicians need to know that leukocoria in infants is not always a sign of RB. Multiple diseases (called pseudo-retinoblastoma) may affect children, like ocular toxocariasis (infectious disease), persistent fetal vasculature (a rare congenital developmental anomaly of the eye), Coats’ disease (characterized by abnormal development of the blood vessels in the retina), and retinopathy of prematurity.2,8,9
Early diagnosis was shown to have a positive impact on visual outcome, as patients who were diagnosed through a screening process in families with a genetic predisposition for RB were diagnosed earlier and had more favorable outcomes than proband cases with no previous awareness of this condition.7,13 Once an abnormality involving the eye is detected by the parents, awareness regarding RB in the physician who first encounters such cases also significantly shortens the time between presentation and diagnosis, as well as initiation of treatment. Unfortunately, leukocoria, which is seen when the tumor is large in size, is the most frequent presenting sign (50–60% of cases), followed by strabismus (25%) and ocular inflammation (6–10%).8–11 Thus, signs of disease present when the tumor is already large in size, and this should be recognized immediately by medical caregivers to avoid more advanced stages at diagnosis.
Yousef et al12 and Leal-Leal et al14 identified insufficient awareness regarding RB as a cause for late detection and referral to a specialist in the developing world. Despite the fact that this topic was covered in the medical curriculum, students did not reach sufficient knowledge scores in these two studies conducted in Jordan and Mexico, respectively. Half of the participants were not aware of the appropriate action plan if leukocoria was detected.12,14,15 In a trial to solve this issue in Jordan, we implemented modifications on the teaching curriculum which focuses on the red flags of RB, and we did this new survey to evaluate the impact of this modification. The first group (Group A) of students in this survey who completed medical school before implementing the new modifications recognized white pupil reflex (leukocoria) as something abnormal in 96% of cases, however, only half of the participants associated this finding with the possibility of a life-threatening condition, and most of them demonstrated poor knowledge about retinoblastoma in general, including age of onset, frequent findings, and mode of diagnosis. After implementing the new modifications in the teaching curriculum our current study (Group B) shows more promising results; 99% of students recognized leukocoria, almost 70% knew that it is life threatening. They had a better understanding about the pathogenesis and how urgently treatment is needed. This indicates how important it is to stress red flags, and to educate students on any rare, but potentially fatal diseases, even in short rotations with limited time allocation. We should mention that this new group (B) completed the questionnaire 1–2 years after the end of the ophthalmology rotation, therefore we are planning to repeat it again 3 years after graduation to check if this knowledge is still retained and remembered by the students or not.
A delayed diagnosis of RB can be attributed to a multitude of factors, including social and economic status and insufficient awareness regarding the possibility of eye cancer.13 It cannot be denied, however, that knowledge and performance of the physician managing the case is of paramount importance. In Jordan, most cases presenting with possible signs of RB encounter first contact-physicians, who are usually not ophthalmologists. This is part of the patient’s journey where early detection makes a vast difference. The participants of this study were on the verge of becoming general practitioners, some with the prospect of practicing in rural areas where ophthalmologists are not routinely available. They should, for this reason, be equipped with the basic knowledge that enables them to diagnose and refer such cases in a timely manner.14–17
In Central America better outcomes were achieved in patients suffering from retinoblastoma by running educational campaigns which resulted in decreasing the time to referral and management.18 As mentioned in the American Pediatric Association guidelines, the red reflex test should be done for any child in their first year of life at least once as part of routine check up.19 This is considered a simple, cost-effective, and non-invasive method that can lead to the diagnosis of a number of significant conditions, making it an excellent screening tool as per World Health Organization criteria, hence justifying the need for educational interventions among first contact physicians.
Recommendations
Previous research elaborated on the central role of early detection of RB.13,20 In this study we suggest educational interventions and changes within the teaching methods that help students attain a better knowledge level of this condition. We could also suggest increasing the time a medical student spends in an ophthalmology rotation, as this might reinforce some of the most vital information that they would have to retain in the future. Furthermore, first-contact physicians in Jordan should be exposed to targeted training aiming to enhance the quality of care of those affected by this disease and their families, in terms of assuring early detection and prompt referral for appropriate treatment to achieve optimal outcome.
Conclusion
This study demonstrates the impact of modifying the teaching curriculum of the ophthalmology rotation in the 5th year of medical school in two Jordanian Universities on the awareness of medical undergraduates about the life-threatening condition retinoblastoma. Compared to a previous study evaluating students’ awareness about this condition, its significance, diagnosis, referral pathways, and management, the participants performed significantly better in all aspects after more emphasis was put on educating students regarding this ophthalmic malignancy during their 2-week clinical ophthalmology rotation. Educating first-line physicians to recognize this condition promptly and improving their knowledge of how to deal with any suspected cases in an accurate and timely manner is therefore recommended as one of the modalities that have the potential to lead to an improved outcome and survival for retinoblastoma patients through minimizing delays in the diagnosis and appropriate referral of such cases.
Acknowledgments
We acknowledge Jannat Falah (Autonomous Systems, Faculty of Artificial Intelligence, Al-Balqa Applied University) for the comprehensive language and scientific editing of the manuscript. We also acknowledge Reem AlJabari (Department of Surgery, King Hussein Cancer Center) for providing assistance with questionnaire data collection.
Funding
This research was supported in part by King Hussein Cancer Center, Amman, Jordan.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Stacey AW, Bowman R, Foster A, et al. Global retinoblastoma study group. incidence of retinoblastoma has increased: results from 40 European countries. Ophthalmology. 2021;128(9):1369–1371. doi:10.1016/j.ophtha.2021.01.024
2. Balmer A, Munier F. Differential diagnosis of leukocoria and strabismus, first presenting signs of retinoblastoma. Clin Ophthalmol. 2007;1(4):431–439.
3. Jaradat I, Yousef YA, Mehyar M, et al. Retinoblastoma in Jordan: an epidemiological study (2006–2010). Hematol Oncol Stem Cell Ther. 2011;4(3):126–131. doi:10.5144/1658-3876.2011.126
4. Dimaras H, Corson TW, Cobrinik D, et al. Retinoblastoma. Nat Rev Dis Primers. 2015;1:15021. doi:10.1038/nrdp.2015.21
5. Gündüz AK, Mirzayev I, Temel E, et al. A 20-year audit of retinoblastoma treatment outcomes. Eye. 2020;34(10):1916–1924. doi:10.1038/s41433-020-0898-9
6. Rodrigues KE, Latorre Mdo R, de Camargo B. Delayed diagnosis in retinoblastoma. J Pediatr. 2004;80(6):511–516. doi:10.2223/1266
7. Yousef YA, Alkhoms A, AlJabari R, et al. Programmed screening for retinoblastoma enhances early diagnosis and improves management outcome for high-risk children. Ophthalmic Genet. 2020;20:1–7.
8. Mirzayev I, Gündüz AK, Biçer Ö, Tarlan B. The final diagnosis: retinoblastoma or pseudoretinoblastoma. J Pediatr Ophthalmol Strabismus. 2021;58(3):161–167. doi:10.3928/01913913-20210108-01
9. Ghassemi F, Bazvand F, Makateb A. Lesions simulating retinoblastoma At A Tertiary Care Center. J Ophthalmic Vis Res. 2015;10(3):316–319. doi:10.4103/2008-322X.170351
10. Dimaras H, Kimani K, Dimba EA, et al. Retinoblastoma. Lancet. 2012;379(9824):1436–1446. doi:10.1016/S0140-6736(11)61137-9
11. Shields CL, Schoenberg E, Kocher K, Shukla SY, Kaliki S, Shields JA. Lesions simulating retinoblastoma (pseudoretinoblastoma) in 604 cases: results based on age at presentation. Ophthalmology. 2013;120(2):311–316. doi:10.1016/j.ophtha.2012.07.067
12. Yousef YA, AlNawaiseh T, AlJabari R, Muhsen S, Al-Nawaiseh I. Retinoblastoma awareness among first contact physicians in Jordan. Ophthalmic Genet. 2019;40(3):191–195. doi:10.1080/13816810.2019.1605387
13. Al-Nawaiseh I, Ghanem AQ, Yousef YA. Familial retinoblastoma: raised awareness improves early diagnosis and outcome. J Ophthalmol. 2017;2017:5053961. doi:10.1155/2017/5053961
14. Leal-Leal CA, Dilliz-Nava H, Flores-Rojo M, Robles-Castro J. First contact physicians and retinoblastoma in Mexico. Pediatr Blood Cancer. 2011;57(7):1109–1112. doi:10.1002/pbc.23227
15. Chantada G, Fandin˜o A, Urrutia L, et al. Late diagnosis of retinoblastoma in a developing country. Arch Dis Child. 1999;80:171–174. doi:10.1136/adc.80.2.171
16. Wong ES, Choy RW, Zhang Y, et al. Global retinoblastoma survival and globe preservation: a systematic review and meta-analysis of associations with socioeconomic and health-care factors. Lancet Glob Health. 2022;10:e380–e389. doi:10.1016/S2214-109X(21)00555-6
17. Finger PT, Tomar AS. Retinoblastoma outcomes: a global perspective. Lancet Glob Health. 2022;10:e307–e308. doi:10.1016/S2214-109X(21)00598-2
18. Wilimas JA, Wilson MW, Haik BG, et al. Development of retinoblastoma programs in Central America. Pediatr Blood Cancer. 2009;53:42–46. doi:10.1002/pbc.21984
19. American Academy of Pediatrics; Section on Ophthalmology; American Association for Pediatric Ophthalmology And Strabismus; American Academy of Ophthalmology; American Association of Certified Orthoptists. Red reflex examination in neonates, infants and children. Pediatrics. 2008;122:1401–1404. doi:10.1542/peds.2008-2624
20. Yousef YA, Al-Nawaiseh I, Mehyar M, et al. How telemedicine and centralized care changed the natural history of retinoblastoma in a developing country: analysis of 478 patients. Ophthalmology. 2021;128(1):130–137. doi:10.1016/j.ophtha.2020.07.026
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
