Back to Journals » Clinical Ophthalmology » Volume 13
Improvement in ocular symptoms and signs in patients with Demodex anterior blepharitis using a novel terpinen-4-ol (2.5%) and hyaluronic acid (0.2%) cleansing wipe
Authors Messaoud R, El Fekih L, Mahmoud A, Ben Amor H, Bannour R, Doan S, Khairallah M
Received 18 December 2018
Accepted for publication 3 April 2019
Published 20 June 2019 Volume 2019:13 Pages 1043—1054
DOI https://doi.org/10.2147/OPTH.S198585
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Riadh Messaoud,1 Lamia El Fekih,2,3 Anis Mahmoud,1 Hager Ben Amor,4 Radhouane Bannour,5 Serge Doan,6,7 Moncef Khairallah4
1Department of Ophthalmology, Tahar Sfar University Hospital, Mahdia, Tunisia; 2Department of Ophthalmology, Internal Security Forces Hospital, La Marsa, Tunisia; 3Faculty of Medicine, Tunis-El Manar University, Tunis, Tunisia; 4Fattouma Bourguiba University Hospital, Monastir, Tunisia; 5Ophthalmology Private Practice, Monastir, Tunisia; 6Department of Ophthalmology, Bichat Hospital, Paris, France; 7Fondation A de Rothschild, Paris, France
Purpose: To evaluate the clinical improvement in ocular symptoms and signs in patients suffering from Demodex anterior blepharitis after using a novel cleansing wipe impregnated with 2.5% terpinen-4-ol and 0.2% hyaluronic acid.
Study design: This was an exploratory, multicenter, open, randomized, two-parallel group comparative study.
Methods: Forty-eight patients with Demodex anterior blepharitis were randomly assigned to apply the sterile wipe T1172 (Blephademodex®), either once daily (n=24, Group 1) or twice daily (n=24, Group 2) for 29 days. Overall ocular discomfort and other individual symptoms were measured using a 0–10 numeric rating scale at Day 8 and Day 29. Ocular signs, including eyelid margin hyperemia and number of cylindrical dandruff, were examined at slit lamp. Overall treatment performance by investigator, patient satisfaction and tolerance were evaluated with questionnaires.
Results: Overall ocular discomfort was significantly reduced from baseline (p<0.0001) in both groups at Day 8 (−3.6±0.3 in Group 1 and −4.0±0.4 in Group 2) and Day 29 (−5.7±0.4 and −6.8±0.7, respectively), with no difference between groups (D8: p=0.718; D29: p=0.505). Each ocular symptom associated with Demodex blepharitis was improved in both groups. Eyelid margin hyperemia was significantly reduced at Day 8 (−0.7±0.7; p<0.001) and Day 29 (−1.1±0.7; p<0.0001) in Group 1. Similar results were observed in Group 2 (Day 8: p<0.001; Day 29: p<0.0001). Total disappearance of cylindrical dandruff was reported in 30.4% of patients in Group 1 and 43.5% in Group 2. Improvements in other ocular signs were observed in both groups. The product was well tolerated. All patients were satisfied or very satisfied and would continue using it.
Conclusion: Daily eyelid hygiene using this cleansing wipe impregnated with 2.5% terpinen-4-ol and 0.2% hyaluronic acid during a 4-week period led to a rapid and marked reduction in ocular symptoms and signs associated with Demodex anterior blepharitis and was well tolerated.
Keywords: blepharitis, cleansing wipe, Demodex, eyelid hygiene, terpinen-4-ol, hyaluronic acid
Introduction
Demodex mites are the most common microscopic ectoparasites to infest the human eye (D. folliculorum on the human lash follicles and D. brevis in lash sebaceous glands) and may lead to a wide range of anterior segment findings.1,2 The rate of Demodex infestation increases with age and has been noted in 84% of individuals at age 60, increasing up to 100% in those over 70 years.3 Mites present in lash follicles may induce inflammatory events, causing hair bulb damage, subsequently leading to cylindrical dandruff (CD) formation and potential eyelash loss.4 Lashes with CD are a pathognomonic sign of ocular Demodex infestation and patients with more clinically evident CD tend to have a more severe Demodex infestation.1 Demodex infestation should be suspected in all patients with chronic blepharitis or ocular surface inflammation, including recurrent trichiasis, chalazia, conjunctivitis, blepharoconjunctivitis, and keratitis that are refractory to conventional treatments.5–7 Affected patients usually present with ocular symptoms such as itching, redness, burning, foreign body sensation, eyelid crusting, and blurred vision.5 Clinical signs frequently include eyebrow and eyelash loss, inflammatory edema of the eyelids and conjunctiva, in addition to secondary bacterial infection.4 However, Demodex infestation may be easily overlooked or misdiagnosed as there is a significant overlap with other anterior segment inflammatory diseases.2
The latest Preferred Practice Pattern for blepharitis from the American Academy of Ophthalmology suggests the following management to be helpful: a daily eyelid hygiene regimen, warm compresses, antibiotics (topical and/or systemic), and topical anti-inflammatory agents (eg, corticosteroids, cyclosporine).8 However, the management of blepharitis is frequently unsatisfactory because of insufficient patient compliance to a regular, long-term, and rigorous eyelid hygiene regimen.9 Treatment of Demodex-associated disease is difficult and the performance of most available eyelid hygiene treatments is limited as they are not expected to kill Demodex mites. Tea tree oil (TTO) is a natural oil distilled from Melaleuca alternifolia that exhibits antibacterial, antifungal, anti-inflammatory, and acaricidal properties.10 Treatment with a weekly office, 50% TTO eyelid scrub in addition to a daily 10% TTO shampoo scrub using a cotton tip was shown to be effective in reducing ocular signs and symptoms of Demodex blepharitis, conjunctivitis, and keratitis.11–14 However, contact dermatitis, allergic reactions, and ocular irritation are well-known complications of TTO treatment14 as a reaction to organic compounds, including terpinolene, α-terpinene, ascaridol, and 1,2,4-trihydroxymethane.15 Thus, elimination of these unwanted chemical ingredients in TTO should reduce ocular irritation and promote overall safety.15 Terpinen-4-ol (T4O), the main active component of TTO, accounting for about 40% of its composition, has been shown to be more potent in killing Demodex mites compared to TTO (at equivalent concentrations), and to remain effective in exerting a miticidal effect at a concentration as low as 1%.15 The anti-demodectic effect of T4O impregnated wipes (4% T4O-Cliradex,® Bio-Tissue, Doral, FL, USA) has been demonstrated in vivo in 1 patient treated for 8 weeks15 and found comparable to 50% TTO in vitro.17 In a recent study, most participants judged this method of eyelid hygiene easy to use (94%) and convenient (90%); however, 48% of them found it uncomfortable and felt stinging upon application.18 A foam formulation with 2% T4O confirmed its ability to exert a broad-spectrum antimicrobial effect without causing ocular or skin irritation.19 Hyaluronic acid (HA) is a well-known natural polysaccharide with unique viscoelastic, moisturizing, soothing, and regenerative properties20–22 that, in combination with T4O, could help alleviate ocular discomfort in patients with Demodex anterior blepharitis.
The aim of this exploratory study was to evaluate the clinical benefits of a novel, sterile cleansing wipe impregnated with a preservative-free lotion containing 2.5% T4O and 0.2% HA on ocular symptoms and signs in patients suffering from Demodex anterior blepharitis.
Materials and methods
Study design and participants
This was an exploratory, multicenter, open, randomized, two-parallel group, two-dose regimen study performed in three clinical centers in Tunisia between December 2016 and April 2017. The study was conducted in accordance with Good Clinical Practice, the Declaration of Helsinki, and local health regulations. Ethics committee approvals (Comité d’éthique du Ministère de l’Intérieur et Hôpital des Forces de Sécurité Intérieure de la Marsa and Comité d’éthique EPS Tahar Sfar de Madhia) were obtained for all centers prior to enrolling any patient. All participants provided written informed consent.
Male and female patients were aged ≥18 years and had recurrent symptomatic anterior blepharitis associated with Demodex in at least one eye. All patients had to present with at least one eye with one ocular symptom among itching, burning/stinging, sticky eye in the morning or foreign body sensation with a score ≥2 (graded on a 0–10 numeric rating scale (NRS) from 0: no symptom to 10: most intense symptom imaginable). In addition, patients had to show an eyelid margin hyperemia score ≥1 (as graded using a 4-point scale from 0: none to 3: severe) and at least three CD at the base of the eyelashes. The main study-specific exclusion criteria were: far best-corrected visual acuity (BCVA) ≤2/10 (equivalent to 0.7 logMAR); non-Demodex infectious blepharitis; eyelid papilloma; obstruction of the lacrimal drainage; eyelid malposition; severe dry eye syndrome; a history of inflammatory ocular disease; and ocular trauma or infection within the three months prior to inclusion. The following treatments were prohibited: any cataract or corneal surgery (within 12 months prior to and during the study); systemic retinoids; punctal plugs; immunosuppressive treatments; antiparasitics, antibiotics, or any other treatments used to treat Demodex blepharitis. Non-study ocular medications, including contact lenses, were prohibited during the run-in and study period.
At inclusion (D1), patients were randomly assigned to use the sterile wipes T1172 (Blephademodex®, Laboratoires Théa, France), impregnated with a preservative-free cleansing lotion containing 2.5% T4O and 0.2% hyaluronic acid, to be applied either once daily in the evening (Group 1), or twice daily in the morning and evening (Group 2). Patients were instructed to gently massage both eyelids and the base of the eyelashes in small circular movements, carefully removing any crusts or secretions whilst keeping the eye closed. This procedure was repeated on the other eye using a new wipe. Each patient was instructed to continue the eye hygiene routine for 29 days, and to visit the study site on Day 8±1 (D8, follow-up) and Day 29±3 (D29, final visit) where an ophthalmic examination was performed by the same investigator. Patients were instructed that they could use artificial tears (Physiol®, 0.9% sodium chloride, Laboratoires Théa, France), in particular, if they touched their eye with the wipe during the cleaning process or felt an unpleasant sensation during the day, with a maximum of 4 daily instillations permitted in both eyes. However, no instillation during the 2-hr period prior to the visit was allowed.
Symptoms and signs assessments
Overall ocular discomfort related to demodex anterior blepharitis was verbally rated by the patient using the 0–10 NRS (from 0: no ocular discomfort to 10: most intense ocular discomfort imaginable) at D1 (baseline), D8, and D29. Individual ocular symptoms (itching, burning/stinging, sticky eye in the morning, fluctuating blurred vision, light sensitivity, foreign body sensation) were assessed using this same scoring system.
At each study visit, patients underwent a detailed slit lamp examination of both the study and contralateral eye to assess eyelid margin hyperemia, number of CD (which were counted at the inferior and superior base of the eyelashes), eyelid edema, eyelash abnormalities, conjunctival hyperemia and discharge, and corneal staining. The study eye was determined, if both eyes were eligible, as the eye with the highest eyelid margin hyperemia score at baseline. If both eyes had the same score, the study eye was the right eye. The investigator assessed eyelid hyperemia, eyelid edema, eyelash abnormalities and conjunctival discharge using a 4-point ordinal scale (0: none; 1: mild; 2: moderate; 3: severe). Conjunctival hyperemia was measured using the MacMonnies photographic 6-point scale and corneal fluorescein staining using the 0–5 point Oxford scale.
The overall performance of T1172 in improving symptoms and signs was assessed by the investigator at D29 as either “very satisfactory”, “satisfactory”, “not very satisfactory”, or “unsatisfactory”.
Patient satisfaction and compliance
A patient questionnaire was administered at D8 and D29 to determine the overall satisfaction with the test product. Questions included: “the wipe bag is easy to open”, “the perfume is pleasant”, “the texture of the wipe is soft/pleasant”, “the product is easy to use” and were answered as “I agree”, “I slightly agree”, “I slightly disagree”, or “I disagree”. Two other questions: “overall, are you satisfied with the product?” and “how satisfied would you be to continue with this product?” were assessed as “very satisfied”, “satisfied”, “unsatisfied”, or “very unsatisfied”.
To verify compliance, patients were instructed to bring back the study products (used and unused) at each post-baseline visit. Patients were defined as compliant if they undertook 80–120% of the treatment regimen over the 29-day period.
Safety assessments
Ocular and systemic adverse events (AE) were collected throughout the study. The investigator evaluated the far BCVA of both eyes using the Snellen chart on D1 and D29, and the patient and investigator determined overall ocular tolerability at D29 as either “very satisfactory”, “satisfactory”, “not very satisfactory”, or “unsatisfactory”.
Statistical analyses
Statistical analyses were performed using the SAS software (version 9.4; SAS Institute). Due to the nature of the study (exploratory, open study, parallel groups), the primary analysis was descriptive in nature and therefore no formal hypothesis was tested. However, statistical tests were performed for exploratory analysis purposes.
For the overall ocular discomfort, the change from the baseline in each group was tested using a mixed ANOVA model for repeated measures. This was fitted to the raw data, including the factor time as fixed (3 levels), center as fixed, and center by time interaction and patient effect as random. Comparison between groups was performed using the same model with the addition of group by time interaction. The same analyses were carried out for the CD number assessment (post-hoc exploratory analysis). For eyelid hyperemia, the change from the baseline in each group was assessed using a Wilcoxon signed rank test, whilst Mann–Whitney tests were performed on the change from baseline for between-group comparison. Comparisons between groups of improvement/no improvement (no change or worsening) in eyelid margin hyperemia were performed using the Chi-Square test. The statistical level of significance was set to 0.05%.
All performance analyses were performed in the Full Analysis Set (FAS; all randomized patients who used at least one application of the study treatment and with at least one post-baseline performance assessment) and in the Per Protocol Set (PPS; all patients from the FAS without major protocol deviations). Safety analysis was performed in the Safety Set (all patients who used at least one application of the study treatment). The following results are described for the FAS and correlate with the PPS.
Results
Participants studied
Forty-eight patients were randomized on D1 and treated with T1172 wipes either once (Group 1, n=24) or twice daily (Group 2, n=24). All but one patient in each group (one patient request in Group 1 and one lost-to-follow-up in Group 2) completed the study.
The FAS and Safety Set were composed of the 48 randomized and treated patients. The PPS was composed of 23 patients in Group 1 (one patient excluded due to missing data for the main assessment variable, ie, ocular discomfort) and 21 patients in Group 2 (one patient excluded due to missing data for the main assessment variable, one due to poor compliance (<80%), and one due to D29 visit performed outside the acceptable visit window).
There were no relevant differences between groups in baseline characteristics, including ocular symptoms and signs (Table 1). However, minor clinical differences were noted at baseline for the mean number of CD (difference not statistically significant), frequency of abnormal eyelash aspect, corneal fluorescein staining, and corneal vascularization, which were all slightly higher in Group 2.
 | Table 1 Demographic and baseline characteristics (FAS) |
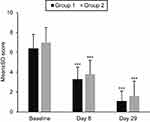
Overall ocular discomfort and individual symptoms
There was a statistically significant reduction in overall ocular discomfort from 6.4±1.4 at baseline to 3.3±1.2 (adjusted mean change ± SE: −3.6±0.3, p<0.0001) at D8 and 1.1±1.0 (−5.7±0.4, p<0.0001) at D29 in Group 1. A similar reduction was observed in Group 2 (−4.0±0.4, p<0.0001 at D8; −6.8±0.7, p<0.0001 at D29) (Figure 1). The between-group difference was not statistically significant at D8 (p=0.718) and D29 (p=0.505). There was a reduction in discomfort of at least 3 points from baseline in 91.3% and 87.0% of patients in Groups 1 and 2, respectively.
Each ocular symptom associated with Demodex blepharitis was improved at D8 and D29 in both groups, with a slightly more pronounced improvement in Group 2 (Figure 2). The mean scores of the most severe symptoms at baseline (ie, itching, burning/stinging and foreign body sensation) were reduced by approximately 3 points at D8 and 5 points at D29.
Ocular signs at slit lamp examination
There was a statistically significant reduction in eyelid hyperemia from 1.5±0.7 at baseline to 0.8±0.6 (mean change ± SD: −0.7±0.7, p<0.001) at D8 and 0.4±0.5 (−1.1±0.7, p<0.0001) at D29 in Group 1. A similar reduction was observed in Group 2 (−0.6±0.7, p<0.001 at D8; −1.1±0.8, p<0.0001 at D29) (Figure 3). The between-group difference was not statistically significant at D8 (p=0.643) and D29 (p=0.871). Compared with baseline, eyelid margin hyperemia was improved in 58.3% vs 50.0% of patients at D8 (p=0.562) and 82.6% vs 77.3% at D29 (p=0.655) in Groups 1 and 2, respectively.
The number of CD was reduced from 15.1±11.7 at baseline to 6.9±6.9 (adjusted mean change ± SE: −7.2±2.0, p=0.001) at D8 and 3.9±5.8 (−10.1±2.5, p<0.001) at D29 in Group 1. A similar reduction was observed in Group 2 (−9.5±3.8, p=0.019 at D8; −12.3±4.0, p=0.006 at D29) (Figure 4). The between-group difference was not statistically significant at D8 (p=0.054) and D29 (p=0.131). The percentage of patients with >10 CD in the study eye reduced dramatically from 54.2% to 12.5% in Group 1 and from 70.8% to 20.8% in Group 2 at D8. Whilst the percentage of patients with >10 CD remained constant in Group 1 (13.0%) at D29, a further decrease was observed in Group 2, down to 4.3%. Total CD disappearance was observed in 12.5% of patients in both groups at D8, and 30.4% and 43.5% of patients in Groups 1 and 2, respectively, at D29.
Improvements in other ocular signs were observed at D29 in both groups and were reported in conjunctival hyperemia (65.2% of patients), abnormal eyelashes aspect, eyelid edema and conjunctival discharge (30.4%), and corneal fluorescein staining (21.7%) in Group 1 (Figure 5). In Group 2, improvements were observed in conjunctival hyperemia (69.6%), abnormal eyelash aspect and eyelid edema (34.8%), conjunctival discharge (39.1%), and corneal fluorescein staining (43.5%). In addition, telangiectasis was the most frequently reported other eyelid margin abnormality (seven patients) and was improved until full disappearance in five patients by the end of the treatment period. Similar results were observed for the contralateral eye.
The overall performance assessed by the investigator at D29 was satisfactory or very satisfactory in 95.7% and 100% of patients in Groups 1 and 2, respectively.
Patient satisfaction and compliance
At the end of the study, all patients in both groups agreed or slightly agreed on all questions proposed in the questionnaire, including the product's ease of use (Figure 6). All patients were satisfied with the product (very satisfied in 52.2% and 47.8% in Groups 1 and 2, respectively) and all reported that they would be satisfied to continue with this product (very satisfied in 52.2% and 56.5% in Groups 1 and 2, respectively).
Compliance, assessed by the number of wipes returned at each post-baseline visit, was 100% of patients in Group 1 and 96% in Group 2.
Safety
T1172 was well tolerated in both groups. One patient in Group 1 reported moderate and transient burning sensation after each wipe application, which resolved after 3 s. The use of T1172 was not stopped, and the therapeutic regimen was not changed due to this adverse effect. This event was reported as recovered at the end of the clinical investigation. Distance BCVA did not change during the study for all patients in Group 1. In Group 2, two patients experienced an increase in their visual acuity. At the end of the study, the ocular tolerability of the T1172 was considered by the investigator and the patient as satisfactory or very satisfactory for all patients in both groups.
Discussion
The present study aimed at demonstrating the clinical improvements in ocular symptoms and signs in patients suffering from Demodex anterior blepharitis after using a novel cleansing wipe, impregnated with 2.5% T4O and 0.2% HA, administered either once or twice daily. Data from our study showed an improvement in overall ocular discomfort and individual symptoms, in addition to a decrease in the characteristic ocular signs of Demodex infestation, including eyelid margin hyperemia and CD, with both regimens. The overall performance was reported as (very) satisfactory whether wipes were used once or twice daily and treatment compliance was demonstrated as excellent.
Other studies have shown a reduction in ocular discomfort and individual symptoms in patients infested with Demodex. In a previous study by Murphy et al23 a daily face wash treatment regimen using a commercially available TTO product (Dr Organic® Tea Tree Face Wash) was effective at reducing symptoms, as shown by a decrease in the OSDI from 27.4±16.7 to 18.3±15.7 after two weeks and to 16.2±15.2 after 4 weeks. A study by Alver et al24 also reported an improvement in ocular symptoms of blepharitis in 89.2% of Demodex positive patients after a 1 month treatment of 4% TTO eyelid gel and 10% eyelash shampoo, administered twice daily. A longer-term study (three months) similarly demonstrated the efficacy of such a treatment against Demodex blepharitis, using 5% TTO applied once daily on patients with chronic ocular disease and Demodex infestation, reducing ocular symptoms by 91%.25 However, these results are based on treatments using varying concentrations of TTO and at present, there is very little data regarding the performance and safety of T4O in reducing Demodex mites and improving symptoms. Tighe et al15 have reported the case of a 61-year-old woman treated twice daily for 8 weeks with T4O wipes (Cliradex®). The treatment was effective in resolving symptoms (for example, bilateral persistent ocular pain and scratchy eyelid) associated with Demodex blepharitis and in eliminating Demodex mites, although the safety of the treatment was not reported.15 Encouragingly, in the present study, a dramatic reduction of overall ocular discomfort and the main ocular symptoms of Demodex-associated blepharitis was observed with both treatment regimens after just seven days using T1172 wipe.
Demodex-associated blepharitis is a chronic inflammatory condition which presents itself by severe clinical signs such as eyelid margin hyperemia, telangiectasis, and conjunctival hyperemia.26 An improvement in these three clinical signs was demonstrated after treatment, which could be explained by the reported anti-inflammatory properties of T4O, independent of its efficacy to kill the Demodex mites.7 For instance, an in vitro study by Hart et al27 showed that T4O was able to suppress pro-inflammatory mediators produced by activated human monocytes, including TNFα, IL-1β, and IL-8. This is in agreement with a similar study which showed that T4O was able to suppress superoxide production and pro-inflammatory cytokines, principally TNFα.28 HA has also demonstrated its potential anti-inflammatory properties in various inflammation conditions. A formulation of HA sodium salt, 0.2% cream applied twice daily for eight weeks by patients suffering from rosacea significantly reduced papules, erythema, burning, stinging, and dryness, with compliance and tolerance reported as excellent.29 The same formulation improved the inflammation signs (scale, erythema, pruritus) associated with facial seborrheic dermatitis in the adult population.30 These findings indicate that the association of T4O and HA in the T1172 cleansing wipes could have multiple beneficial effects for the management of Demodex-associated blepharitis.
Presence of CD is a pathognomonic sign for the presence of Demodex mites, and the proliferation of CD strongly correlates with a higher Demodex infestation.1 Whilst the number of mites was not counted in the present study, a notable decrease in the number of CD was observed, with a 41% (Group 1) and 67% (Group 2) reduction of patients with >10 CD, after 29 days of treatment. Promisingly, total CD disappearance was observed in 30.4% and 43.5% of patients within Groups 1 and 2, respectively. Other studies have counted the parasite numbers instead of CD. Koo et al14 showed that eyelid scrub treatment using a cotton tip wetted in 10% TTO twice daily effectively reduced the Demodex count (per 8 cilia) from 4.0±2.5 to 3.2±2.3 in the TTO group vs 4.3±2.7 to 4.2±2.5 in the control group. A study performed by Murphy et al23 showed that scrubbing the eyelid and lash margins once daily, with a cotton pad wetted in a commercially available TTO solution containing 38% T4O, significantly reduced the total Demodex mite count of 4 eyelashes from 4.9 at baseline, to 2.2 after 2 weeks and to 1.9 after 4 weeks. According to these findings, which counted mite numbers and results from the present study, which counted CD, a decrease in ocular symptoms is observed when there is a reduction in either parasite or CD numbers.
It has been previously reported that compliance is critical in the successful treatment of blepharitis. However, it can be difficult to ensure patients adhere to a treatment regimen, and the ease, comfort, and convenience of use are believed to facilitate compliance in the longer term.9,31 Whilst previous reports using differing concentrations of TTO have generally proved effective in reducing ocular signs and symptoms of Demodex-associated blepharitis,14,23–25,32 all have reported major compliance issues, potentially related to the adverse effects of other ingredients contained within TTO.15 A study performed by Koo et al14 previously showed that only 38% of patients adhered to the treatment (10% TTO daily scrubs in addition to a 50% TTO weekly scrub) with the efficacy of TTO vs control only observed in compliant patients. In a similar study by Nicholls et al,25 non-compliance was estimated at 25%. This is in comparison to our observed non-compliance rate of 0% in Group 1 and 4% in Group 2 (one patient with compliance <80%), which could be a result of the reduced adverse effects of T4O alone and at a lower concentration when compared with other Demodex treatment regimens.2 Alternatively, the unique formulation of the study wipe T1172, which also contains 0.2% HA, a natural moisturizing agent known to sooth29,30 and regenerate skin,20–22 may account for the improved compliance. Promisingly, all patients were sufficiently satisfied to continue using the study wipes, with no clear indication that compliance was lower with the once or twice daily regimen. This would suggest that the unique T1172 formulation may reduce compliance issues. An additional issue with moderate-to-severe cases of Demodex-associated blepharitis is the recommended treatment regimen which includes an in-office procedure once a week due to the higher concentration of TTO utilized.33 This could have an impact on treatment compliance, in addition to a socio-economic burden impact, particularly if the patient is located a distance away from the ophthalmologist practice. This study demonstrated that using a 2.5% T4O impregnated wipe once or twice daily could be safely administered at home.
One advantage of T1172 cleansing wipes is its improved tolerance compared to 5% or 10% TTO formulations. The study wipe is free from detergents and preservatives and was well tolerated when applied once or twice daily for one month. Only one adverse effect (transient burning sensation of 3 s after each wipe application) was reported, but this did not lead to treatment discontinuation. This transient effect is somewhat consistent with a recent prospective, randomized, controlled, cross-over study showing that 4% T4O impregnated wipes (Cliradex®) produced minimal discomfort upon eyelid application peaking at a score of 3 (out of 10) at 45 s and lasting 180 s.34 However, in a study by Qiu et al,18 48% of the participants felt adverse stinging upon application of these same wipes. By comparison, contact dermatitis, allergic reaction, and ocular irritation are well-known complications of TTO solutions or ointments. TTO can be toxic to the eye and cause ocular stinging and irritation if used in its pure form.35 In 2008, the Scientific Committee on Consumer Products in European Union considered that at concentrations above 5%, TTO is more likely to induce skin and eye irritation.36 This is in agreement with a previous study,14 where 5 of 106 patients (4.7%) reported ocular irritation in eyelid care using cotton tips wetted in 10% TTO.
The main limitation of the present study is the uncontrolled design. Eyelid scrubbing with commercial cleansing wipes not impregnated with TTO or with cotton tips wetted in baby shampoo has been shown to improve ocular signs and symptoms in patients with anterior blepharitis.37,38 However, it is not known if patients were positive for Demodex mites in these studies. Moreover, although the subjective improvement of patients after TTO treatment may be influenced by a placebo effect, a clear correlation between the dramatic alleviation of symptoms and marked reduction of lid margin inflammation and CD with the study wipes was documented in all patients. The low number of non-compliant patients observed in our study could also be explained by the shorter study period and small sample size. A prospective, controlled, randomized clinical trial with a larger sample size would be required to address all these issues. Finally, since both regimens were similarly effective, with no tolerance issues reported, a twice-daily regimen may be more appropriate for a more severe manifestation of the disease as some clinical signs, particularly CD, were slightly more pronounced in the twice-daily group at baseline. Further, randomized prospective studies with a larger population and longer follow-up are required to better assess the efficacy and safety of a more intensive therapeutic regimen on the resolution of Demodex blepharitis.
Conclusion
In conclusion, daily eyelid scrub with 2.5% T4O and 0.2% hyaluronic acid cleansing wipe improved ocular symptoms and signs in patients with Demodex anterior blepharitis. The product was well tolerated and convenient to use. As Demodex blepharitis is a chronic disease, we recommend the periodic use of this new wipe as part of a daily, effective, eyelid hygiene regimen.
Acknowledgments
The authors wish to thank the patients for their participation in this clinical trial, all the study site personnel, Axonal-Biostatem (Castries, France) for data management, and Dermscan (Lyon, France) for statistical analysis. This clinical investigation was sponsored by Laboratoires Théa, Clermont-Ferrand, France, whose staff participated in the study design, conducting the study, data collection, management, analysis and interpretation, and preparation of the manuscript.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
MK and SD are consultants for Laboratoires Théa. SD reports personal fees from Alcon-Novartis, Bausch&Lomb, Horus, Santen, and Théa, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Gao -Y-Y, Di Pascuale MA, Li W, et al. High prevalence of Demodex in eyelashes with cylindrical dandruff. Invest Ophthalmol Vis Sci. 2005;46(9):3089–3094.
2. Fromstein SR, Harthan JS, Patel J, Opitz DL. Demodex blepharitis: clinical perspectives. Clin Optometry. 2018;10:57–63. doi:10.2147/OPTO.S142708
3. Liu J, Sheha H, Tseng SCG. Pathogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505–510. doi:10.1097/ACI.0b013e32833df9f4
4. Rusiecka-Ziolkowska J, Nokiel M, Fleischer M. Demodex - an old pathogen or a new one? Adv Clinl Exp Med. 2014;23(2):295–298. doi:10.17219/acem/37081
5. Lindsley K, Matsumura S, Hatef E, Akpek EK. Interventions for chronic blepharitis. Cochrane Database Syst Rev. 2012;(5):CD005556.
6. Zhao Y-E, Wu L-P, Hu L, Xu J-R. Association of blepharitis with Demodex: a meta-analysis. Ophthalmic Epidemiol. 2012;19(2):95–102. doi:10.3109/09286586.2011.642052
7. Cheng AMS, Sheha H, Tseng SCG. Recent advances on ocular Demodex infestation. Curr Opin Ophthalmol. 2015;26(4):295–300. doi:10.1097/ICU.0000000000000168
8.
9. Benitez-Del-Castillo JM. How to promote and preserve eyelid health. Clin Ophthalmol. 2012;6:1689–1698. doi:10.2147/OPTH.S33133
10. Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (tea tree) oil: a review of antimicrobial and other medicinal properties. Clin Microbiol Rev. 2006;19(1):50–62. doi:10.1128/CMR.19.1.50-62.2006
11. Gao -Y-Y, Di Pascuale MA, Li W, et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmol. 2005;89(11):1468–1473. doi:10.1136/bjo.2004.059121
12. Gao -Y-Y, Di Pascuale MA, Elizondo A, Tseng SCG. Clinical treatment of ocular demodecosis by lid scrub with tea tree oil. Cornea. 2007;26(2):136–143. doi:10.1097/01.ico.0000244870.62384.79
13. Kheirkhah A, Casas V, Li W, Raju VK, Tseng SCG. Corneal manifestations of ocular demodex infestation. Am J Ophthalmol. 2007;143(5):743–749. doi:10.1016/j.ajo.2007.01.054
14. Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. J Korean Med Sci. 2012;27(12):1574–1579. doi:10.3346/jkms.2012.27.12.1574
15. Tighe S, Gao -Y-Y, Tseng SCG. Terpinen-4-ol is the most active ingredient of tea tree oil to kill Demodex mites. Transl Vis Sci Technol. 2013;2(7):2. doi:10.1167/tvst.2.7.2
16. Salvatori C, Barchi L, Guzzo F, Gargari M. A comparative study of antibacterial and anti-inflammatory effects of mouthrinse containing tea tree oil. Oral Implantol. 2017;10(1):59–70. doi:10.11138/orl/2017.10.1.059
17. Cheung IMY, Xue AL, Kim A, Ammundsen K, Wang MTM, Craig JP. In vitro anti-demodectic effects and terpinen-4-ol content of commercial eyelid cleansers. Cont Lens Anterior Eye. 2018;41(6):513–517.
18. Qiu TY, Yeo S, Tong L. Satisfaction and convenience of using terpenoid-impregnated eyelid wipes and teaching method in people without blepharitis. Clin Ophthalmol. 2018;12:91–98.
19. Su C-W, Tighe S, Sheha H, Cheng AMS, Tseng SCG. Safety and efficacy of 4-terpineol against microorganisms associated with blepharitis and common ocular diseases. BMJ Open Ophthalmol. 2018;3(1):e000094.
20. Rah MJ. A review of hyaluronan and its ophthalmic applications. Optometry. 2011;82(1):38–43. doi:10.1016/j.optm.2010.08.003
21. Chen LH, Xue JF, Zheng ZY, Shuhaidi M, Thu HE, Hussain Z. Hyaluronic acid, an efficient biomacromolecule for treatment of inflammatory skin and joint diseases: a review of recent developments and critical appraisal of preclinical and clinical investigations. Int J Biol Macromol. 2018;116:572–584. doi:10.1016/j.ijbiomac.2018.05.068
22. Bukhari SNA, Roswandi NL, Waqas M, et al. Hyaluronic acid, a promising skin rejuvenating biomedicine: a review of recent updates and pre-clinical and clinical investigations on cosmetic and nutricosmetic effects. Int J Biol Macromol. 2018;120(Pt B):1682–1695.
23. Murphy O, O‘Dwyer V, Lloyd-McKernan A. The efficacy of tea tree face wash, 1, 2-Octanediol and microblepharoexfoliation in treating Demodex folliculorum blepharitis. Cont Lens Anterior Eye. 2018;41(1):77–82. doi:10.1016/j.clae.2017.10.012
24. Alver O, Kıvanç SA, Akova Budak B, et al. System for diagnosis of ocular demodicosis. Med Sci Monit. 2017;23:5862–5869. doi:10.12659/MSM.907824
25. Nicholls SG, Oakley CL, Tan A, Vote BJ. Demodex treatment in external ocular disease: the outcomes of a tasmanian case series. Int Ophthalmol. 2016;36(5):691–696. doi:10.1007/s10792-016-0188-5
26. Bernardes TF, Bonfioli AA. Blepharitis. Semin Ophthalmol. 2010;25(3):79–83. doi:10.3109/08820538.2010.488562
27. Hart PH, Brand C, Carson CF, Riley TV, Prager RH, Finlay-Jones JJ. Terpinen-4-ol, the main component of the essential oil of melaleuca alternifolia (tea tree oil), suppresses inflammatory mediator production by activated human monocytes. Inflamm Res. 2000;49(11):619–626. doi:10.1007/s000110050639
28. Brand C, Ferrante A, Prager RH, et al. The water-soluble components of the essential oil of melaleuca alternifolia (tea tree oil) suppress the production of superoxide by human monocytes, but not neutrophils, activated in vitro. Inflamm Res. 2001;50(4):213–219. doi:10.1007/s000110050746
29. Schlesinger TE, Powell CR. Efficacy and tolerability of low molecular weight hyaluronic acid sodium salt 0.2% cream in rosacea. J Drugs Dermatol. 2013;12(6):664–667.
30. Schlesinger T, Rowland powell C. Efficacy and safety of a low molecular weight hyaluronic acid topical gel in the treatment of facial seborrheic dermatitis final report. J Clin Aesthet Dermatol. 2014;7(5):15–18.
31. Doan S. Tolerability and acceptability of Blephagel: a novel eyelid hygiene aqueous gel. Clin Ophthalmol. 2012;6:71–77.
32. GaoYY, Xu DL, Huang LJ, Wang R, Tseng SC. Treatment of ocular itching associated with ocular demodicosis by 5% tea tree oil ointment. Cornea. 2012;31(1):14–17. doi:10.1097/ICO.0b013e31820ce56c
33. Pflugfelder SC, Karpecki PM, Perez VL. Treatment of blepharitis: recent clinical trials. Ocul Surf. 2014;12(4):273–284. doi:10.1016/j.jtos.2014.05.005
34. Ngo W, Jones L, Bitton E. Short-term comfort responses associated with the use of eyelid cleansing products to manage Demodex folliculorum. Eye Contact Lens. 2018;44(Suppl 2):S87–S92. doi:10.1097/ICL.0000000000000415
35. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575–628. doi:10.1016/j.jtos.2017.05.006
36.
37. Guillon M, Maissa C, Wong S. Eyelid margin modification associated with eyelid hygiene in anterior blepharitis and meibomian gland dysfunction. Eye Contact Lens. 2012;38(5):319–325. doi:10.1097/ICL.0b013e318268305a
38. Guillon M, Maissa C, Wong S. Symptomatic relief associated with eyelid hygiene in anterior blepharitis and MGD. Eye Contact Lens. 2012;38(5):306–312. doi:10.1097/ICL.0b013e3182658699
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.