Back to Journals » Risk Management and Healthcare Policy » Volume 17
Impacts of the Zero-Markup Drug Policy on Hospitalization Expenses of Patients with Stroke in Western China: An Interrupted Time Series Analysis
Received 28 December 2023
Accepted for publication 23 March 2024
Published 3 April 2024 Volume 2024:17 Pages 777—788
DOI https://doi.org/10.2147/RMHP.S456977
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jongwha Chang
Yanghaotian Wu,1– 3 Xuemei Han,3 Jingfu Qiu1
1Department of Social Medicine and Health Service Management, School of Public Health, Chongqing Medical University, Chongqing, People’s Republic of China; 2Department of Social Medicine, School of Public Health, Southwest Medical University, Luzhou, People’s Republic of China; 3Institute of Social Medicine and Health Management, School of Public Health, Lanzhou University, Lanzhou, People’s Republic of China
Correspondence: Jingfu Qiu, School of Public Health, Chongqing Medical University, Yixueyuan Road, Yuzhong District, Chongqing, 400016, People’s Republic of China, Email [email protected]
Background: In 2016, an innovative medical pricing reform called zero-markup drug policy (ZMDP) was implemented in selected pilot cities in China, which focuses on curbing the unreasonable growth of medical expenses. This study aimed to evaluate the impacts of ZMDP on medical expenditure of stroke in western China.
Methods: The quantitative data of inpatients diagnosed with stroke was extracted from the medical insurance system in 7 tertiary public hospitals. An interrupted time series (ITS) was used to analyze the instantaneous level and long-term trend changes of hospitalization expenses per visit from January 2015 to November 2018.
Results: A total of 22,407 stroke inpatients were extracted. The total hospitalization expense per visit had the highest proportion of 20,000 CNY and above (33.66%). After the ZMDP, the median total hospitalization expense and western medicine expense per visit decreased by 631.74 CNY and 966.35 CNY, respectively (P < 0.001). Before the policy, the total hospitalization expense, traditional Chinese medicine (TCM) expense, examination expense, treatment expense, laboratory expense and surgical expense per visit showed upward trends (P< 0.05), while the anesthesia expense per visit showed a downward trend (P< 0.001). When the policy was implemented, the anesthesia expense per visit instantaneously increased by 91.70% (P< 0.001). After the policy, the total hospitalization expense, western medicine expense, TCM expense, treatment expense and surgical expense per visit changed from upward trends to downward trends (P< 0.05). The anesthesia expense per visit changed from a downward trend to an upward trend (P< 0.001), and the examination expense per visit maintained an upward trend (P=0.005).
Conclusion: The economic burden of stroke inpatients decreased significantly with the implementation of the ZMDP, especially for the drug expenses. The medical service expenses increased significantly, reflecting the improvement in the value of medical staff’s technical labor. However, the unexpected increase in the examination expenses was likely to be associated with the unreasonable medical compensation mechanism.
Keywords: zero-markup drug policy, stroke, interrupted time series, hospitalization expenses, drug expenses
Introduction
Public hospitals are the main component of China’s healthcare system, occupying an absolutely dominant position in the healthcare services market. The Chinese government introduced the drug markup policy during a historical period of low socio-economic level and limited government financial resources, allowing public hospitals to sell drugs with a 15% markup on the purchase price, with the aim of maintaining the basic operation of public hospitals and promoting their own development.1 The policy has played a positive role in improving the operation of public hospitals in the course of their development. However, with the transformation of China’s economic system after the reform and opening up, the drug markup gradually evolved into a profit-seeking behavior, and the income from the drug markup became an important part of the income of public hospitals.2 In the two decades before the policy, China’s pharmaceutical expenditures accounted for 45.7% of the total expenditures on health care.3 Meanwhile, it is also worth noting that the medical staffs’ incomes are linked to drug profits, and problems such as abuse of high-priced drugs and over-prescribing are becoming more frequent.4 Health services have the special nature of being supply-led and demand-led, and health insurance funds are used irrationally, leading to a rapid increase in patients’ medical expenses. At the same time, doctors, stimulated by the profit-seeking mechanism, generate provider-induced demand and prescribe large quantities of unnecessary antibiotics, injections and hormone drugs for patients, which has become a major public health problem in China at this stage.5–7
In view of this, in 2009, China initiated a reform of medical and health-care system, whereby drugs are uniformly purchased and distributed through government tenders and sold at the tendered price, with a 15% mark-up on the original price abolished. The zero-markup drug policy (ZMDP) is aimed at separating drug sales from hospital revenue, regulating the profit-making tendency and unreasonable medical behaviors of medical staffs, focusing on the public welfare of public medical institutions, and effectively decreasing the economic burden for patients. Since then, China has carried out pilot reforms in tertiary public hospitals in various provinces and cities to gradually implement the ZMDP. In September 2017, the Chinese government abolished the 15% mark-up on medicines (except for decoction pieces of Chinese medicine) in public hospitals.8,9 As one of the pilot areas for the ZMDP, seven tertiary public hospitals implemented the ZMDP starting from December 19, 2016 in Luzhou. The local government has compensated the reduced revenue after the ZMDP, promoting hospitals to actively reduce the purchase price of drugs.
Stroke is currently the second leading cause of death and the third leading cause of disability globally, and one of the chronic non-communicable diseases (NCDs) that threaten human life and health. In 2019, stroke accounted for 11.6% of all deaths worldwide.10 Similarly, stroke is the leading cause of death among Chinese residents, with an estimated number of deaths accounting for approximately one-third of global stroke deaths.11 Stroke is characterized by high morbidity, high mortality, and complex etiology, and may be accompanied by various comorbidities, such as hypertension and diabetes mellitus.12 In addition, stroke recurrence and related complications generate significant healthcare expenses. One study found that stroke patients with lacunar cerebral infarction had a low early mortality rate but a significantly increased risk of mortality, stroke recurrence, and subcortical dementia in the medium and long term.13 Meanwhile, cardiogenic stroke is accompanied by severe adverse cardiovascular co-morbidities and higher mortality, for which patients require long-term drug therapy.14 It is worth noting that the average annual medical expense of stroke patients in urban areas of China is 10,637 CNY, of which drug expenses account for more than 50%. The huge economic burden of medicines has pushed some families into poverty.15
Previous studies have found significant short-term reductions in drug expenses of chronic diseases after the implementation of ZMDP,16,17 but have not assessed the changes in the various expenses and component structure. Meanwhile, most studies on the policy effects of ZMDP have used short-term data before and after the reform, making it difficult to assess future changes in long-term trends, and there are differences in the unintended policy impacts and substitution effects of ZMDP. Therefore, it is necessary to conduct a comprehensive and detailed assessment of the economic burden of ZMDP on stroke inpatients and to analyze the long-term effects of ZMDP on expense structure. This study analyzed the instantaneous level changes and long-term trend changes of hospitalization expenses of stroke patients before and after the implementation of the ZMDP by using the ITS model, and provided the evidence-based experience and policy recommendations for further improvement of medical and health care policies and effective control of excessive growth of medical expenses.
Methods
Study Setting
The study was conducted at Luzhou in Sichuan province, which is located in western China and in the upper reaches of the Yangtze River, with 3 districts and 4 counties under its jurisdiction. Owing to Luzhou’s unique location on the border of four provinces (Sichuan, Chongqing, Yunnan and Guizhou), the city’s tertiary public hospitals provide medical services covering the city and adjacent regions. The prevalence of chronic diseases and risk factors among residents of the city are maintained at a high level, and the main chronic diseases threatening the residents are stroke, chronic obstructive pulmonary disease and other chronic diseases. As one of the pilot cities, Luzhou implemented the ZMDP of abolishing 15% mark-up of drug sales (except for decoction pieces of Chinese medicine) in 7 tertiary public hospitals since December 19, 2016. The relevant financial departments made price compensation for the reduced income after the ZMDP, and promoted medical institutions to reduce the purchase price of related drugs.
Data Sources and Outcome Indicators
The data were obtained from the medical insurance system of Luzhou’s medical security bureau, from which the settlement data of inpatients in 7 tertiary public hospitals were obtained from 2015 to 2018. Based on the International Classification of Diseases, 10th version (ICD-10), this study screened inpatients with stroke (ICD-10 coded as I60-I64) from January 1, 2015 to November 20, 2018 in 7 tertiary public hospitals.
The data collected included: 1) socio-demographic information: gender, age, ethnicity, and type of health insurance. 2) hospital information: ICD-10 codes, date of visit, date of discharge, and length of stay. 3) expense information: total expenses, western medicine expenses, examination expenses, treatment expenses, materials expenses, surgery expenses, anesthesia expenses, traditional Chinese medicine (TCM) expenses, and laboratory expenses, and other expenses.
Quality Control
Due to the impact of inflation and price changes, and the long-time span of data involved in this study, discounting adjustments were conducted for the 2015–2017 hospitalization expenses based on the Consumer Price Index (CPI) for healthcare published by the China National Bureau of Statistics, using the 2018 hospitalization expenses as the baseline (Table 1).
 |
Table 1 Adjustment of Hospitalization Expenses Based on the CPI |
Statistical Analysis
The categorical variables were described in counts and percentages, and continuous variables with normal distributions were described in means and standard deviations. Normality of continuous variables was tested by the Kolmogorov–Smirnov (K-S) test, and non-normally distributed variables were described in medians and interquartile range (IQR). The Mann–Whitney U test was used to compare the continuous variables, and the chi-squared test was applied to compare the categorical variables.
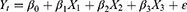
The ITS analysis, regarded as the strongest quasi-experimental research design, has been widely applied in the field of policy evaluation to evaluate the group-level instantaneous level and long-term trend changes triggered by interventions over a specific period of time.18,19 Segmented regression model is commonly used in an ITS analysis, which is proven effective for assessing intervention effects and requires fewer time points.20,21 In this study, the intervention point was December 18, 2016, when the ZDMP was officially implemented. The pre-ZDMP period was defined as January 1, 2015 to December 18, 2016, while the post-ZDMP period was defined as December 19, 2016 to November 20, 2018. The time variable was selected as the independent variable and counted in months. The ITS regression model was specified as follows:
where Yt is the outcome indicator representing the expenses in month t; X1 is a continuous variable representing each month during the observation period, coded “1, 2, 3...n”; X2 is a binary dummy variable, which is coded 0 before the policy was implemented, and is coded 1 after the policy was implemented; X3 is a continuous variable, which is coded 0 before the policy was implemented, and increases monthly after the policy implementation, coded “0, 1, 2, 3...n”.
In the regression model, β0 represents the constant term, which reflects the baseline level at t=0; β1 represents the monthly changes in the trend before the policy implementation, that is, the estimation of the slope of the baseline; β2 represents the estimation of the instantaneous level changes due to the implementation of the policy; β3 represents the estimation of the monthly changes in the trend after the policy; and β1+β3 represents the monthly trends after the policy.
The Durbin–Watson (D-W) test was applied to test the existence of first order autocorrelation in the error terms, and the Paris-Winsten estimation method was used to correct the D-W value.22 Moreover, the natural logarithmic transformations were performed on all outcome variables to adjust the non-normality data, and log-line transformations were applied to adjust the expense variables by converting them into percentage changes that directly reflect the relationship between X and Yt.23 The data analysis was performed in R software (version 4.0.5). The level of significance was set at 0.05.
Results
Characteristics of Study Population with Stroke
A total of 22,407 inpatients were included in this study, of which 10,075 were included before the implementation of the policy and 12,332 were included after the implementation of the policy. The sociodemographic characteristics of inpatients with stroke by gender, age, ethnic, and types of basic medical insurance before and after the implementation of the policy are displayed in Table 2. The proportion of males before and after the policy was higher than that of females, accounting for 57.56% and 58.29%, respectively. The average age of inpatients was 67.05 years. The proportion of inpatients in the age group of 60 years old and above before and after the implementation of the policy was the highest, accounting for 74.36% and 74.92%, respectively, and the proportion of inpatients aged 50–59 years old and 60 years old and above increased slightly after the implementation of the policy (P=0.026). The Han ethnic populations accounted for 99.9%. The proportion of inpatients who participated in urban and rural resident’s basic medical insurance before and after the policy was higher than the proportion of inpatients who participated in urban employee’s basic medical insurance, accounting for 65.30% and 64.23%, respectively.
 |
Table 2 Basic Characteristics of Inpatients Included Before and After the Policy |
Comparative Analysis of Hospitalization Expenses
The proportion of stroke patients with total hospitalization expense per visit of 20,000 CNY and above was the highest, accounting for 33.66%, while the proportion of stroke patients with total hospitalization expense per visit of less than 2,000 CNY was the lowest, accounting for 0.74%. After the implementation of the policy, the proportion of stroke patients with total hospitalization expense per visit of 20,000 CNY and above decreased from 35.79% to 31.92%, while the proportion of stroke patients with total hospitalization expense per visit of 10,000–15,000 and 15,000–20,000 CNY both increased (Table 3).
 |
Table 3 Frequency Distribution of Total Hospitalization Expense per Visit Before and After the Policy |
After the K–S test, the hospitalization expenses per visit were non-normally distributed (P < 0.001), and expenses variables were presented as a median and interquartile range. According to the results in Table 4, after the implementation of the ZMDP, the median value of total hospitalization expense per visit decreased by 631.74 CNY, the median value of western medicine expense per visit decreased by 966.35 CNY, the median value of TCM expense per visit decreased by 117.04 CNY, the median value of examination expense per visit increased by 394.27 CNY, the median value of treatment expense per visit increased by 368.33 CNY, the median value of laboratory expense per visit increased by 150.72 CNY, and the median value of materials expense per visit increased by 79.14 CNY (P < 0.001).
 |
Table 4 Comparative Analysis of the Hospitalization Expenses per Visit Before and After the Policy |
The ITS Analysis of Monthly Hospitalization Expenses
In order to visualize the changes before and after the implementation of the policy, this study converted the data to the original scale based on the linear regression results, and the fitted graph of the monthly changes in the hospitalization expenses per visit is shown in Figure 1. The model parameters are shown in Table 5. The D-W value or adjusted D-W value was from 1.794 to 2.036, indicating that the data met the autocorrelation test requirements.24 Before the implementation of the policy, the total hospitalization expense, TCM expense, examination expense, treatment expense, laboratory expense, surgical expense and other expenses per visit showed significant upward trends, with increasing by 0.70% per month (β1=0.007, P < 0.001), 3.05% per month (β1=0.03, P=0.007), 2.02% per month (β1=0.02, P < 0.001), 3.25% per month (β1=0.032, P < 0.001), 1.01% per month (β1=0.01, P=0.006), 2.02% per month (β1=0.02, P=0.005) and 8.00% per month (β1=0.077, P < 0.001), respectively. On the contrary, the anesthesia expense per visit showed a significant downward trend, with decreasing by 3.54% per month (β1=−0.36, P < 0.001). However, the trend changes in western medicine expense and materials expense per visit were statistically insignificant (P > 0.05). When the policy was implemented, the anesthesia expense per visit increased by 91.70% instantaneously (β2=0.651, P < 0.001). After the implementation of the policy, the total hospitalization expense, western medicine expense, TCM expense, treatment expense, surgical expense, and other expenses per visit changed from upward trends to downward trends, with decreasing by 1.09% per month (β1 + β3=−0.011, P < 0.001), 2.37% per month (β1 + β3=−0.024, P < 0.001), 1.39% per month (β1 + β3=−0.014, P=0.011), 2.37% per month (β1 + β3=−0.024, P < 0.001), 0.50% (β1 + β3=−0.005, P=0.017) and 1.98% per month (β1 + β3=−0.02, P < 0.001), respectively. On the contrary, the anesthesia expense per visit changed from a downward trend to an upward trend, increasing by 0.90% per month (β1 + β3=0.009, P < 0.001). The examination expense per visit maintained an upward trend with a monthly increase of 0.40% (β1 + β3=0.004, P=0.005). However, the trend changes in laboratory expense and materials expense per visit were statistically insignificant (P > 0.05).
 |
Table 5 ITS Regression Results of Hospitalization Expenses per Visit Before and After the Policy |
Discussion
Based on current studies, this study is the first to assess changes in the instantaneous levels and long-term trends of various hospitalization expenses for stroke patients before and after a policy intervention, with an additional focus on changes in cost structure.
The results showed that the median total hospitalization expense per visit of stroke patients decreased after the implementation of the ZMDP, in which the median western medicine expense per visit decreased significantly. The implementation of the ZMDP effectively controlled the rapid growth of total hospitalization expense and western medicine expense of stroke patients, and alleviated the economic burden of patients. As a kind of delayed disease, the incidence rate of stroke in the elderly population is significantly higher than that of other age groups, and it is usually accompanied by comorbidities such as hypertension, diabetes mellitus and coronary heart disease, and the recurrence rate after the onset of the disease is high.12,25 Pharmacological treatment is currently the main treatment modality, and lipid-lowering drugs are widely used in clinical practice, combined with antiplatelet and antihypertensive drugs, mainly clopidogrel hydrogen carbonate and aspirin, to inhibit thrombogenesis and reduce recurrent ischemic events.26–28 In addition, stroke patients need to take neuroprotective drugs such as piracetam to promote the recovery of cerebral neural function, and use the Shuxuetong injection, a purified extract of TCM for adjuvant treatment to relieve symptoms of vasospasm.29,30 After the implementation of the ZMDP, the TCM expense per visit in stroke patients showed a downward trend. Although the scope of ZDMP does not cover the decoction pieces of Chinese medicine, some TCMs not on the list have been affected by the policy, resulting in a reduction of selling prices. It is worth noting that stroke inpatients had the highest proportion of drug expenses, despite ischemic stroke, as one of the subtypes of stroke, is primarily treated by surgical interventions, but still accounts for a high proportion of drug expenses. There are several reasons for the high proportion of drug expenses for stroke. Firstly, Chinese hospitals calculate expenses incurred during surgical treatment, such as medical consumables expenses, drug expenses, and anesthesia expenses, separately, whereas surgical expenses include only the technical operation expenses of medical staff. Secondly, Chinese hospitals implement the strict medical technology charging standards, and most of the charging standards have not been adjusted for a long time, while the prices of drugs and medical consumables are widely influenced by the regulation of the market, and have been on a rising trend in recent years.31,32 As a result, the surgery expenses in Chinese hospitals are underestimated, while the drug expenses usually account for a relatively high proportion.
The total hospitalization expense and drug expenses of stroke patients did not change significantly at the instantaneous level when the policy was implemented, but thereafter showed a month-by-month decreasing trend, which may be due to the lagged effect of the policy interventions, consistent with the findings of Zhu et al.33 One possible explanation is that continuous interventions such as ZMDP usually require a period of time as a transition period for adjustment from implementation to effect, resulting in the effects being delayed until after the transition period. The examination expense showed a month-to-month increase after the implementation of the policy. Consistent with the previous studies, hospitals may not have rationalized the reform policy when the ZMDP was implemented, and the government’s financial compensation to public hospitals was not in place in a timely manner, and the economic loss formed in the short term will have an impact on the operation of the hospitals.7,34 Some hospitals may increase their revenues by increasing the number of consumable materials and checkups in order to mark up for the economic loss caused by ZMDP.35 In the long term, it seems that the growth rate of inpatients’ examination expense per visit narrowed significantly after the policy implementation compared with that before the policy implementation, and the reason may be related to China’s policy of abolishing the markup on medical consumables and the reform of clinical pathway in public hospitals.7 Thus, although the overall level of consumables and examination expenses is still at a high level, the reform of China’s healthcare system in recent years has had a significant effect, and the structure of patients’ healthcare expenses has been optimized in a sustained and long-term process.
Clinical treatment, surgery, anesthesia, and other medical service programs are closely related to the total hospitalization expense. The higher the price of medical services, the higher the technical labor value of medical staffs.34 The results of the ITS analysis showed that the instantaneous level of anesthesia expense for stroke inpatients increased at the time of policy implementation, reflecting the improvement in the value of medical staff’s technical labor. Although the Chinese government explicitly requires medical service providers to further increase the price of medical services and mobilize the medical staffs’ motivation, the problems of a low-price base for medical service programs, and the imperfection of the ZMDP related supporting policies and compensation mechanisms still exist in the current stage.36 In addition, there is a certain degree of difficulty in promoting and charging for medical service programs due to the price control imposed by the health insurance sector on the reimbursement of some medical service programs and the difficulty in pricing new medical technologies.37 When the contributions of medical staff cannot be acknowledged, their work motivation will decline, and some of them will be driven by interests to generate induced demand, and unreasonable behaviors such as over-diagnosis and treatment and repeated examinations will occur.38 Therefore, it is recommended to continuously optimize the structure of hospitalization expenses, strengthen internal supervision of hospitals, and deepen clinical path management.
This study has several limitations. Firstly, due to the availability of data, this study was not able to assess the changes in indirect expenses, intangible expenses, financial burden on uninsured stroke inpatients, and the expenses and mortality for patients with recurrent stroke and related complications. Secondly, the hospitals involved in this study were all tertiary public hospitals, and there was no cross-sectional comparison of hospitalization expenses for stroke inpatients at different levels of hospitals. Thirdly, although this study controlled the impact of long-term trend changes triggered by historical factors on outcome indicators before the intervention by setting multiple observation time points, it was not able to fully control the confounding factors, which affected the comparability of hospitalization expenses. In the future, more relevant data need be collected to assess the effects of the ZMDP on the economic burden of inpatients with stroke.
Conclusion
ZMDP is an effective attempt to reduce the financial burden of stroke inpatients and optimize the structure of medical expenses, with a significant decrease in patients’ drug expenses. The expenses of medical service programs have increased, reflecting the improvement in the value of medical staff’s technical labor. However, patients’ examination expenses increased unexpectedly after the implementation of ZMDP, which may be related to the unreasonable medical compensation mechanism. The results of this study have a certain reference value for low- and middle-income countries to carry out medical reform. Further studies will be conducted by increasing the evaluation index and sample size for the assessment of different subtypes of stroke, stroke recurrence and associated complications to evaluate related health policies’ long-term impact in a broader range.
Data Sharing Statement
The datasets used and analyzed in the current study are available from the corresponding author, upon reasonable request.
Ethics Approval and Informed Consent
The study has been granted exemption by the Biomedical Ethics Committee of Southwest Medical University (No. SWMUIRB-MCSC-20240226-0001). This study was conducted using anonymized informational data, and the patients’ right to informed consent was ensured. All methods were performed in accordance with the Declaration of Helsinki and the Measures for the Ethical Review of Biomedical Research Involving Human Subjects issued by China.
Acknowledgments
The authors sincerely thank the healthcare security administration of Luzhou City for the contribution of data sources.
Funding
The study was supported by the Key Project of Chongqing Science and Technology Bureau (No. CSTB2022TIAD-YJX0008).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yip WC, Hsiao W, Meng Q, Chen W, Sun X. Realignment of incentives for health-care providers in China. Lancet. 2010;375(9720):1120–1130. doi:10.1016/s0140-6736(10)60063-3
2. Wagstaff A, Yip W, Lindelow M, Hsiao WC. China’s health system and its reform: a review of recent studies. Health Econ. 2009;18(Suppl 2):S7–S23. doi:10.1002/hec.1518
3. Shi L, Yang HY, Cheng G, Meng Q. Time trends and determinants of pharmaceutical expenditure in China (1990–2009). Pharmacoeconomics. 2014;32(3):257–264. doi:10.1007/s40273-013-0072-3
4. Jiang Q, Yu BN, Ying G, et al. Outpatient prescription practices in rural township health centers in Sichuan Province, China. BMC Health Serv Res. 2012;12:324. doi:10.1186/1472-6963-12-324
5. Currie J, Lin W, Meng J. Addressing antibiotic abuse in China: an Experimental Audit Study. J Dev Econ. 2014;110:39–51. doi:10.1016/j.jdeveco.2014.05.006
6. Li Y, Xu J, Wang F, et al. Overprescribing in China, driven by financial incentives, results in very high use of antibiotics, injections, and corticosteroids. Health Aff. 2012;31(5):1075–1082. doi:10.1377/hlthaff.2010.0965
7. Liu M, Jia M, Lin Q, Zhu J, Wang D. Effects of Chinese medical pricing reform on the structure of hospital revenue and healthcare expenditure in county hospital: an interrupted time series analysis. BMC Health Serv Res. 2021;21(1):385. doi:10.1186/s12913-021-06388-2
8. Gao L, Shi L, Meng Q, Kong X, Guo M, Lu F. Effect of healthcare system reforms on public hospitals’ revenue structures: evidence from Beijing, China. Soc Sci Med. 2021;283:114210. doi:10.1016/j.socscimed.2021.114210
9. Shi X, Zhu D, Man X, et al. The biggest reform to China’s health system”: did the zero-markup drug policy achieve its goal at traditional Chinese medicines county hospitals? Health Policy Plan. 2019;34(7):483–491. doi:10.1093/heapol/czz053
10. Collaborators. GS. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. doi:10.1016/s1474-4422(21)00252-0
11. Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi:10.1016/s0140-6736(19)30427-1
12. Ergul A, Hafez S, Fouda A, Fagan SC. Impact of comorbidities on acute injury and recovery in preclinical stroke research: focus on hypertension and diabetes. Transl Stroke Res. 2016;7(4):248–260. doi:10.1007/s12975-016-0464-8
13. Arboix A, Massons J, García-Eroles L, et al. Nineteen-year trends in risk factors, clinical characteristics and prognosis in lacunar infarcts. Neuroepidemiology. 2010;35(3):231–236. doi:10.1159/000319460
14. Arboix A, Oliveres M, Massons J, Pujades R, Garcia-Eroles L. Early differentiation of cardioembolic from atherothrombotic cerebral infarction: a multivariate analysis. Eur J Neurol. 1999;6(6):677–683. doi:10.1046/j.1468-1331.1999.660677.x
15. Zhu D, Shi X, Nicholas S, et al. Medical service utilization and direct medical cost of stroke in Urban China. Int J Health Policy Manag. 2022;11(3):277–286. doi:10.34172/ijhpm.2020.111
16. Liu L, Xu Y, Jiang Y, et al. Impact of Beijing healthcare reform on the curative care expenditure of outpatients with noncommunicable diseases based on SHA2011 and interrupted time series analysis. BMC Health Serv Res. 2021;21(1):1045. doi:10.1186/s12913-021-07059-y
17. Du J, Xie J, Qian Y, et al. Impact of China’s zero mark-up drug policy on drug cost of NCDs’ outpatients: an interrupted time series analysis. BMC Health Serv Res. 2021;21(1):404. doi:10.1186/s12913-021-06414-3
18. Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17(6):1231–1238. doi:10.1111/j.1365-2753.2010.01504.x
19. Li L, Cuerden MS, Liu B, Shariff S, Jain AK, Mazumdar M. Three statistical approaches for assessment of intervention effects: a primer for practitioners. Risk Manag Healthc Policy. 2021;14:757–770. doi:10.2147/rmhp.S275831
20. Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13(6 Suppl):S38–S44. doi:10.1016/j.acap.2013.08.002
21. Nistal-Nuño B. Segmented regression analysis of interrupted time series data to assess outcomes of a South American road traffic alcohol policy change. Public Health. 2017;150:51–59. doi:10.1016/j.puhe.2017.04.025
22. Turner SL, Forbes AB, Karahalios A, Taljaard M, McKenzie JE. Evaluation of statistical methods used in the analysis of interrupted time series studies: a simulation study. BMC Med Res Methodol. 2021;21(1):181. doi:10.1186/s12874-021-01364-0
23. Yu SC, Wang QQ, Long XJ, et al. 变量自然对数转换的多重线性回归 [Multiple linear regression models with natural logarithmic transformations of variables]. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(4):451–456. Chinese. doi:10.3760/cma.j.cn112150-20191030-00824
24. Chen Y. Spatial autocorrelation approaches to testing residuals from least squares regression. PLoS One. 2016;11(1):e0146865. doi:10.1371/journal.pone.0146865
25. Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health. 2019;4(3):e159–e167. doi:10.1016/s2468-2667(19)30019-2
26. Alpérovitch A, Kurth T, Bertrand M, et al. Primary prevention with lipid lowering drugs and long term risk of vascular events in older people: population based cohort study. BMJ. 2015;350:h2335. doi:10.1136/bmj.h2335
27. Schulz UG. Drug treatments in the secondary prevention of ischaemic stroke. Maturitas. 2013;76(3):267–271. doi:10.1016/j.maturitas.2013.05.009
28. Hackam DG, Spence JD. Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke. 2007;38(6):1881–1885. doi:10.1161/strokeaha.106.475525
29. Ricci S, Celani MG, Cantisani TA, Righetti E. Piracetam for acute ischaemic stroke. Cochrane Database Syst Rev. 2012;2012(9):Cd000419. doi:10.1002/14651858.CD000419.pub3
30. Gu HQ, Xie XW, Jing J, et al. Shuxuetong for Prevention of recurrence in Acute Cerebrovascular events with Embolism (SPACE) trial: rationale and design. Stroke Vasc Neurol. 2020;5(3):311–314. doi:10.1136/svn-2019-000293
31. Blumenthal D, Hsiao W. Privatization and its discontents--the evolving Chinese health care system. N Engl J Med. 2005;353(11):1165–1170. doi:10.1056/NEJMhpr051133
32. Shang L, Lin Y, Fang W, et al. How national health insurance coverage policy affected the use of trastuzumab and rituximab in China: a Bicentric Retrospective Study. Risk Manag Healthc Policy. 2023;16:1739–1753. doi:10.2147/rmhp.S420899
33. Zhu Z, Wang J, Sun Y, Zhang J, Han P, Yang L. The impact of zero markup drug policy on patients’ healthcare utilization and expense: an interrupted time series study. Front Med. 2022;9:928690. doi:10.3389/fmed.2022.928690
34. Zeng J, Chen X, Fu H, Lu M, Jian W. Short-term and long-term unintended impacts of a pilot reform on Beijing’s zero markup drug policy: a propensity score-matched study. BMC Health Serv Res. 2019;19(1):916. doi:10.1186/s12913-019-4764-z
35. Liu X, Xu J, Yuan B, Ma X, Fang H, Meng Q. Containing medical expenditure: lessons from reform of Beijing public hospitals. BMJ. 2019;365:l2369. doi:10.1136/bmj.l2369
36. Liu S, Xu H, Cui X, Qian Y. How the implementation of drug zero markup policy will affect health care expenditure in hospitals: observation and prediction based on Zhejiang Model. Value Health. 2014;17(7):A790. doi:10.1016/j.jval.2014.08.432
37. Tang X, Zhang X, Chen Y, Yan J, Qian M, Ying X. Variations in the impact of the new case-based payment reform on medical costs, length of stay, and quality across different hospitals in China: an interrupted time series analysis. BMC Health Serv Res. 2023;23(1):568. doi:10.1186/s12913-023-09553-x
38. Yi H, Miller G, Zhang L, Li S, Rozelle S. Intended and unintended consequences of China’s zero markup drug policy. Health Aff. 2015;34(8):1391–1398. doi:10.1377/hlthaff.2014.1114
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.