Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Impact of Prone Jackknife Position on Intraoperative Hypotension During Percutaneous Nephroscopy: A Retrospective Matched Analysis
Received 16 August 2023
Accepted for publication 25 October 2023
Published 2 November 2023 Volume 2023:19 Pages 865—873
DOI https://doi.org/10.2147/TCRM.S430523
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Deyun Wang
Song Lyu,1 Guobin Wu,2 Yingfen Wu1
1Department of Anesthesiology, The Second Affiliated Hospital of Hainan Medical University, Haikou, People’s Republic of China; 2Medical Record Management Department, The Second Affiliated Hospital of Hainan Medical University, Haikou, People’s Republic of China
Correspondence: Song Lyu, Department of Anesthesiology, The Second Affiliated Hospital of Hainan Medical University, Haikou, People’s Republic of China, Fax +8689866808208, Email [email protected]
Objective: To investigate the potential relationship between the prone jackknife position during percutaneous nephroscopy and the occurrence of intraoperative hypotension.
Methods: A retrospective analysis was conducted on 651 patients who underwent percutaneous nephroscopy at the Second Affiliated Hospital of Hainan Medical University. The primary focus was to investigate the occurrence of hypotension during the surgical procedure and assess the duration of hypotensive episodes. Patients were categorized into the prone jackknife position group and the lateral position group. To compare the incidence of intraoperative hypotension between the two groups, a 1:1 propensity match was performed. Following the matching process, intraoperative hypotension was assessed and compared between the two groups before and after the match. The binary logistic regression analysis determined the probability of intraoperative hypotension occurred in each group. Furthermore, linear regression analysis was used to analyze the duration of hypotensive episodes experienced by patients in both groups.
Results: After propensity score matching, a total of 272 patients with similar characteristics were obtained (136 in each group). The prone jackknife group had a significantly higher incidence of intraoperative hypotension than the lateral group after the match, with an odds ratio of 2.71 (95% confidence interval: 1.595– 4.605). Binary logistic regression analysis showed that age and body position exhibited statistical significance as risk factors. Linear regression analysis before and after the match indicated that the duration of hypotension was associated with age, surgical time, and a history of hypertension.
Conclusion: The prone jackknife position syndrome after general anesthesia could occur in surgeries. The position could contribute to the development of hypotension during the percutaneous nephroscopy procedure.
Keywords: prone, jackknife position, percutaneous nephroscopy, intraoperative hypotension
Introduction
Almost one-third of the surgical workload in urology is related to the treatment of stone patients,1 with approximately 14% receiving percutaneous nephrolithotomy (PCNL) treatment.2 The incidence rate of complications of PCNL is as high as 15%.3,4 Intraoperative hypotension (IOH) is associated with various adverse events. Specifically, IOH during noncardiac surgeries has been associated with an increased risk of major adverse cardiac or cerebrovascular events within 30 days after the procedure. Furthermore, the severity of hypotension is correlated with an increased likelihood of experiencing cardiovascular and cerebrovascular complications.5
The occurrence of IOH during PCNL is usually believed to be caused by bleeding or infection. However, changes in posture may also be an undeniable cause. As in anesthesiology, when a pregnant woman changes from a lateral position to a supine position, the inferior vena cava is compressed, a condition known as “supine hypotension syndrome”.6,7 When choosing the position of PCNL, surgeons not only need to consider factors such as the size, location, and diameter of the stones8 but also need to pay attention to the impact of the position on the patient.
The prone and lateral positions are commonly used during PCNL. The prone position offers the advantage of better stabilization of the kidneys and, when combined with the jackknife position, raises the 12th rib, providing a larger operating space for puncture.9 But this usually safe prone position10 may lead to hemodynamic instability.11 We observed an increase in the occurrence of IOH when patients were placed in a combination of prone and jackknife positions. Consequently, we hypothesized that this specific position could lead to IOH and coined the term “prone jackknife position hypotension syndrome after general anesthesia” to describe this phenomenon.
There is a lack of comprehensive analysis in the literature on the impact of a prone jackknife position on hypotension during PCNL surgery. This study investigated factors associated with hypotension syndrome in patients placed in prone-jackknife positions after general anesthesia.
Methods
Study Design and Setting
This retrospective propensity score matching study was conducted at the Second Affiliated Hospital of Hainan Medical University from October 2019 to January 2023. The study included patients who met the following inclusion criteria: 1) underwent elective percutaneous nephrolithotomy, 2) had complete height and weight data, 3) had no missing blood pressure records (with intervals not exceeding 5 minutes), 4) had an American Society of Anesthesiologists (ASA) Physical Status classification II–III, and 5) were over 18 years old. Exclusion criteria were 1) surgery termination after needle insertion due to the discovery of infected hydronephrosis, 2) pre-existing nephrostomy tube in the patient, and 3) documented drug allergy to the anesthetic administered during the surgery.
All data were anonymized to maintain confidentiality. This study involves no harm to human bodies, no sensitive personal information, and no commercial interests. It followed the guidelines of the Helsinki Declaration and was reviewed by the Ethics Committee of the Second Affiliated Hospital of Hainan Medical University (LW2003083), obtaining an informed consent exemption.
Surgery and Anesthesia
All included patients underwent anesthesia in the supine position, followed by insertion of ureteral catheters in the lithotomy position, and subsequently underwent percutaneous nephroscopy surgery in the prone jackknife position (PJ Group) or lateral position (LL Group). After surgery, the patients were returned to the supine position.
The anesthesia protocol was consistent for the PJ and LL groups. All patients received general anesthesia and underwent tracheal intubation. Anesthesia induction involved the administration of midazolam (0.03–0.05 mg/kg), etomidate (0.2 mg/kg), sufentanil (0.5 μg/kg), and cisatracurium (0.2 mg/kg). Maintenance of anesthesia was achieved using propofol (4–8 mg·kg−1·h−1), sevoflurane (0.7–1.3 MAC), remifentanil (20–40 μg·kg−1·h−1), or cisatracurium (0.04–0.1 mg·kg−1·h−1).
Data Collection and Processing
The following demographic and clinical information was extracted from medical records: age, sex, history of hypertension and diabetes, and body mass index (BMI). Anesthesiologists reviewed anesthesia records to obtain additional data, including ASA physical status scores, surgical duration, patient position during surgery (prone jackknife or lateral), the occurrence of IOH, intraoperative blood loss, and blood pressure measurements after returning the patient to the supine position in cases of IOH.
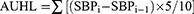
Baseline blood pressure was the lowest measured before anesthesia when the patient entered the operating room. Hypotension was defined as a systolic blood pressure (SBP) of 80 mmHg or less or a decrease in SBP to 80% or less of the baseline value.12 The duration of hypotension is known to be associated with its harmful effects. Hypotension criteria served as a reference point for each patient, forming a line in a coordinate plane with blood pressure and time as axes over time. This line represents the hypotension trend. The actual blood pressure measurements and the hypotension line create an irregular figure The area under this irregular figure is called the area under the hypotension line (AUHL).13,14 AUHL is a continuous variable measured in units of a 10 mmHg decrease in SBP per 5 minutes, representing the integral of the magnitude and duration of the reduction in blood pressure. The calculation of AUHL adopts the trapezoidal rule, which is a numerical integration method. The trapezoidal rule estimates the total area under a curve by approximating the area under the curve to the sum of a series of small trapezoidal areas. The calculation formula for AUHL is as follows:
Among them, SBPi and SBPi-1 represent the systolic blood pressure at the end of the i-th and i-1st 5-minute intervals, respectively.
Early intervention in malignant events during anesthesia is common. The increase in blood pressure after medication can mask hypotension, which can lead to bias if it is considered not present. Therefore, patients who received more than 10ug of norepinephrine but did not experience an increase in blood pressure (higher than previous measurements) are considered to have developed hypotension. This does not affect the judgment of hypotension, but it will affect the calculation of AUHL. We used an estimation method, assuming that 5 micrograms of norepinephrine can increase blood pressure by about 10 millimeters of mercury and maintain it for 5 minutes. This method can provide an approximate value for considering this group of patients when calculating AUHL. This estimation method may have errors as different patients may have different reactions to norepinephrine.
Sample Size Calculation
Based on our preliminary research, the incidence of hypotension is 60% and 47%, respectively. Use a formula to compare two independent proportions. A minimum sample size of 343 participants was established based on a desired statistical power of 0.8, a significance level of 0.05 (α), and a participant ratio in the two groups (κ) set at 0.5.
Statistical Analysis
Data were divided into the PJ and LL groups based on the body position during surgery. Continuous variables are presented as mean and standard deviation and analyzed using t-tests. Categorical variables are presented as percentages and analyzed using chi-square tests. Baseline demographics and risk factors were compared between the two groups. In case of existing differences, a 1:1 matching algorithm with a caliper size of 0.05 was applied to create matched pairs based on propensity scores.15,16 Subsequently, another test was conducted to assess any remaining differences between the groups. Propensity matching categorized data into unmatched (original) and matched (balanced concerning risk factors other than body position), which can be beneficial in clarifying causal relationships.
Data were analyzed using univariate analysis before and after matching to identify risk factors associated with IOH. Subsequently, a binomial logistic regression model was used to analyze the unmatched and matched data sets to identify risk factors and calculate the corresponding odds ratios (OR).
AUHL is a significant indicator that reflects the severity of hypotension and is considered a continuous variable. AUHL was designated as the dependent variable to identify relevant risk factors. Independent variables included age, sex, history of hypertension, presence of diabetes, BMI, ASA physical status score, duration of surgery, patient position, and intraoperative blood loss. Linear regression analysis assessed the relationship between these independent variables and the time of hypotension before and after the match.17 P < 0.05 was considered statistically significant. All statistical analyses were performed with SPSS (version 22, SPSS, Chicago, IL).
Results
Patient Baseline Characteristics and Propensity Match
Of the 812 patients screened, 670 met the study inclusion criteria, and 19 were excluded (18 with infected hydronephrosis and an existing renal fistula and 1 with drug allergy). The final analysis was conducted on 651 cases, comprising 515 patients in the PJ group and 136 in the LL group (Figure 1). The baseline characteristics of the two groups of patients were compared, revealing significant differences in the sex ratio and intraoperative blood loss between the groups. A propensity score matching was performed to address these differences, resulting in a matched data set of 272 patients (136 per group) in which the two groups of patients had similar characteristics (Table 1).
 |
Table 1 Patient Baseline Characteristics |
 |
Figure 1 The flow of patients. |
Univariate Analysis of Risk Factors Associated with Intraoperative Hypotension
Univariate analysis was performed before and after the matching between the two groups to identify risk factors associated with IOH. The results of the unmatched analysis revealed that age, operation time, surgical positions, ASA physical status score, and preoperative hypertension were identified as risk factors for IOH. However, after matching the propensity score, the matched results indicated that operating time no longer significantly impacted the occurrence of hypotension (Table 2).
 |
Table 2 Univariate Analysis of Influencing Factors for Intraoperative Hypotension Before and After Propensity Score Matching |
Logistic Regression Analysis
A binary logistic regression model was used to determine the predictive risk factors for the occurrence of IOH, with IOH as the dependent variable and the other variables as independent variables. The results showed that, before matching, age, position, ASA physical status score, and hypertension were statistically significant as risk factors for IOH (Table 3). However, after performing propensity score matching, the results showed that age and position remained statistically significant. In contrast, the ASA physical status score and the history of hypertension did not show statistical significance. After the match, the odds ratio (OR) of experiencing hypotension in the PJ group was 2.71, higher than the OR observed before the match (1.541). To identify factors influencing the severity of IOH, AUHL was considered the dependent variable, while the other variables were treated as independent variables. Linear regression analysis was conducted on both unmatched and matched patient data sets. The results of the linear regression analysis, both before and after matching, were consistent. AUHL was significantly associated with age, duration of surgery, and history of hypertension (Table 4). All patients with IOH had their blood pressure restored before leaving the surgical room.
 |
Table 3 Regression Analysis of Predictive Factors for Intraoperative Hypotension Before and After Propensity Score Matching |
 |
Table 4 Linear Regression Analysis Results Before and After Matching the Duration of Hypotension |
Discussion
Intraoperative hypotension occurred after the prone jackknife position due to changes in body position and improved after returning to the original position. There was a clear time correlation, but the influence of other factors could not be ruled out. After performing propensity score matching, the odds ratio for IOH in the prone jackknife position group increased to 2.71, compared to 1.541 before the match. This suggests that confounders may have obscured the true impact of body position on the occurrence of IOH. Consequently, the significance of posture in contributing to hypotension might have been overlooked for a considerable period. Typically, during the post-anesthesia onset period, anesthesiologists focus primarily on monitoring surgical progress and assessing the effects of varying levels of stimuli, inadvertently disregarding the potential influence of body position on the patient’s blood pressure.
Unmatched regression analysis revealed that age, body position, ASA grade, and history of hypertension were associated with IOH before matching. After matching the propensity score, the results showed that age and body position remained significant factors influencing intraoperative hypotension. This suggests a plausible causal relationship between body position and hypotension, with age acting as a confounder. It is important to note that age can contribute to cardiovascular fragility.18 However, there was no temporal correlation between these factors and IOH in this study. In particular, after matching, the statistical significance of the ASA grading and a history of hypertension were no longer observed for the occurrence of IOH. This indicates that physiological changes determine the relationship between body position and hypotension and do not depend on the severity of the patient’s preoperative condition.
In the analysis of the severity of hypotension, AUHL was associated with age, duration of surgery, and a history of hypertension. It is well-established that age and hypertension can contribute to cardiovascular fragility.18,19 On the other hand, body posture was related to hypotension but not its severity. This suggests that body posture was an initial factor in the development of hypotension. At the same time, the duration of the position (the duration of surgery) was associated with the severity of hypotension experienced by the patient.
The phenomenon of prone position causing IOH has been discussed in various studies. When an individual assumes a prone position, it can decrease cardiac output per stroke by 20 mL, increase heart rate, and increase total peripheral vascular resistance.20 Experimental results suggest that prone posture may contribute to uncontrolled orthostatic hypotension.18 During spinal surgery under anesthesia, hypotension has been observed, and there have even been reports linking postoperative blindness to hypotension.14,21,22 The impact of a prone position on hemodynamics can potentially result in cardiac arrest.23 Furthermore, the prone position has been associated with sudden infant death syndrome.24
The pathophysiological mechanism underlying the prone position can be explained by chest compression and the consequent increase in intrathoracic pressure, reducing venous reflux and stroke volume.20 Additionally, the prone position decreases stroke volume due to the activation of the sympathetic nervous system reflex.18 In awake individuals, compensatory tachycardia counter-balances these effects.18,20 However, under general anesthesia, this compensatory response is suppressed. Mechanical ventilation during general anesthesia further increases intrathoracic pressure, exacerbating these pathological and physiological changes. Abdominal compression in the prone position can reduce the diameter of the inferior vena cava, affecting the venous return from the lower extremities and potentially leading to deep vein thrombosis.23 This further reduces the amount of blood returning to the heart, particularly when the prone position is combined with the jackknife position.
Similarly to supine hypotensive syndrome observed in late pregnancy, hypotension associated with the jackknife position can be alleviated by rapid infusion of the upper limb extremities. However, there is a distinction between the two scenarios. In the case of late pregnancy, the obstruction is relieved once the baby is delivered. In contrast, percutaneous nephroscopy in the prone jackknife position cannot quickly correct the compression. Returning the prone jackknife position after a puncture to the prone position is recommended to reduce compaction in the inferior vena cava. However, more research is necessary to determine the feasibility and effectiveness of this approach.
So, after the patient’s position changes, anesthesiologists should pay attention to the changes in blood pressure, use medication as needed, and assist surgeons in reducing the angle of the knife position when possible. Surgeons should be informed that prone folding position can cause IOH and try to use other positions to reduce this impact. When lying prone, the duration should be minimized as much as possible. Devices should be used to promote lower limb blood circulation. When in a prone position, elderly and patients with a history of hypertension should be given attention.
Although the incidence of hypotension was lower in the lateral position compared to the prone jackknife position, almost 40% of the individuals still experienced hypotension in the lateral position. More research is necessary to investigate possible causes, such as infection, anesthesia techniques, or other surgical factors that may contribute to hypotension.
This study has several limitations. First, it is a retrospective study that could not control the anesthesia procedures. The impact of static water pressure on blood pressure measurements at different body positions could not be assessed. Second, this study did not observe indicators of renal function or long-term outcome measures. Many of the factors that were associated with intraoperative hypotension were not controlled for. Blood pressure data were intermittent and hence the duration of hypotension is imprecise. The assumption made on the duration of hypotension based on the administration of norepinephrine is also not precise. Future studies should address these limitations to provide a more comprehensive understanding. We propose a prospective study of real-time blood pressure monitoring to provide more accurate data on the duration and severity of hypotension.
Conclusions
The prone jackknife position was associated with intraoperative hypotension and increased challenges in anesthesia management. Avoiding or minimizing the prone jackknife position whenever possible is advisable.
Key Points
Question: [Is there a causal relationship between Hypotension during percutaneous nephroscopy with prone jackknife position?]
Findings: [The prone jackknife group had a significantly higher incidence of intraoperative hypotension than the lateral group, with an odds ratio of 2.71.]
Meaning: [It is recommended to use the lateral position or restore the prone jackknife position to the prone position after a puncture to reduce the compression of the inferior vena cava.]
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Project supported by Hainan Province Clinical Medical Center.
Disclosure
The authors report no conflicts of interest in this work.
References
1. de la Rosette J, Assimos D, Desai M, et al. The clinical research office of the endourological society percutaneous nephrolithotomy global study: indications, complications, and outcomes in 5803 patients. J Endourol. 2011;25:11–17. doi:10.1089/end.2010.0424
2. Monga M, Murphy M, Paranjpe R, et al. Prevalence of stone disease and procedure trends in the United States. Urology. 2023;176:63–68. doi:10.1016/j.urology.2023.03.040
3. Leow J, Meyer C, Wang Y, et al. Contemporary trends in utilization and perioperative outcomes of percutaneous nephrolithotomy in the united states from 2003 to 2014. J Endourol. 2017;31:742–750. doi:10.1089/end.2017.0225
4. Alsyouf M, Abourbih S, West B, et al. Elevated renal pelvic pressures during percutaneous nephrolithotomy risk higher postoperative pain and longer hospital stay. J Urol. 2018;199:193–199. doi:10.1016/j.juro.2017.08.039
5. Gregory A, Stapelfeldt WH, Khanna AK, et al. Intraoperative hypotension is associated with adverse clinical outcomes after noncardiac surgery. Anesth Analg. 2021;132:1654–1665. doi:10.1213/ANE.0000000000005250
6. Wright L. Postural hypotension in late pregnancy. “The supine hypotensive syndrome”. Br Med J. 1962;1:760–762. doi:10.1136/bmj.1.5280.760
7. Sherman C, Gauthier M, David M. Supine Hypotensive Syndrome of Pregnancy. In: Freeman BS, Berger JS, editors. Anesthesiology Core Review: Part Two Advanced Exam. New York, NY: McGraw-Hill Education; 2016.
8. Wang F, Hong Y, Yang Z, et al. Comparison of retrograde intrarenal surgery and standard percutaneous nephrolithotomy for management of stones at ureteropelvic junction with high-grade hydronephrosis. Sci Rep. 2021;11:14050. doi:10.1038/s41598-021-93551-8
9. Zhao Z, Fan J, Liu Y, et al. Percutaneous nephrolithotomy: position, position, position! Urolithiasis. 2018;46(79–86):79–86. doi:10.1007/s00240-017-1019-5
10. Feix B, Sturgess J. Anaesthesia in the prone position. Cont Educ Anaesth Crit Care Pain Med. 2014;14:291–297. doi:10.1093/bjaceaccp/mku001
11. Roodneshin F, Poor Zamany Nejat Kermany M, Rostami P, et al. Comparison of hemodynamic stability and pain control in lateral and prone positions in patients undergoing percutaneous nephrolithotomy: a randomized controlled trial. Urol J. 2020;17:124–128. doi:10.22037/uj.v0i0.4915
12. Awad H, Alcodray G, Raza A, et al. Intraoperative hypotension-physiologic basis and future directions. J Cardiothorac Vasc Anesth. 2022;36:2154–2163. doi:10.1053/j.jvca.2021.05.057
13. Salmasi V, Maheshwari K, Yang D, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017;126:47–65. doi:10.1097/ALN.0000000000001432
14. Postoperative Visual Loss Study Group. Risk factors associated with ischemic optic neuropathy after spinal fusion surgery. Anesthesiology. 2012;116:15–24. doi:10.1097/ALN.0b013e31823d012a
15. Mao C, Xiao M, Chen J, et al. Propensity score matching comparisons of postoperative complications and morbidity between digestive tract reconstruction methods after gastrectomy in gastric cancer patients with visceral obesity. Front Oncol. 2022;12:1072127. doi:10.3389/fonc.2022.1072127
16. Schmidt MT, Paredes S, Rössler J, et al. Postoperative risk of transfusion after reversal of residual neuromuscular block with sugammadex versus neostigmine: a retrospective cohort study. Anesth Analg. 2023;136:745–752. doi:10.1213/ANE.0000000000006275
17. Edelman ER, van Kuijk SMJ, Hamaekers AEW, et al. Improving the prediction of total surgical procedure time using linear regression modeling. Frontiers in Medicine. 2017;4:85. doi:10.3389/fmed.2017.00085
18. Tabara Y, Tachibana-Iimori R, Yamamoto M, et al. Hypotension associated with prone body position: a possible overlooked postural hypotension. Hypertens Res. 2005;28:741–746. doi:10.1291/hypres.28.741
19. Gu F, Randall EB, Whitesall S, et al. Potential role of intermittent functioning of baroreflexes in the etiology of hypertension in spontaneously hypertensive rats. JCI Insight. 2020;2020:5.
20. Pump B, Talleruphuus U, Christensen NJ, et al. Effects of supine, prone, and lateral positions on cardiovascular and renal variables in humans. Am J Physiol Regul Integr Comp Physiol. 2002;283:R174–80. doi:10.1152/ajpregu.00619.2001
21. Wada K, Kumagai G, Kudo H, et al. Association between intra-operative hemodynamic changes and corrective procedures during posterior spinal fusion in adolescent patients with scoliosis: a case-control study. Medicine. 2021;100:e28324. doi:10.1097/MD.0000000000028324
22. Peng Z, Xia J, Yin N, et al. The effects of volume-controlled ventilation versus pressure-controlled ventilation on hemodynamic and respiratory parameters in patients undergoing lumbar spine fusion surgery: a randomized controlled trial. Ann Palliat Med. 2021;10:9553–9563. doi:10.21037/apm-21-1932
23. Khouri DB, Delgado MA, Lemes JL, et al. Differential diagnosis of intraoperative cardiac arrest after spine surgery in prone position. Saudi J Anaesth. 2022;16:485–487. doi:10.4103/sja.sja_893_21
24. Carpenter RG, Irgens LM, Blair PS, et al. Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004;363:185–191. doi:10.1016/S0140-6736(03)15323-8
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.