Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
Impact of Implementing Key Performance Indicators on Catheter-Associated Urinary Tract Infection (CAUTI) Rates Among Adult ICU Patients in Saudi Arabia
Authors Alhabdan N, Alyaemni A, Aljuaid MM , Baydoun A , Hamidi S
Received 16 November 2022
Accepted for publication 12 January 2023
Published 19 January 2023 Volume 2023:15 Pages 41—49
DOI https://doi.org/10.2147/CEOR.S396160
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Nouf Alhabdan,1 Asma Alyaemni,1 Mohammed M Aljuaid,1 Ali Baydoun,2 Samer Hamidi3
1Department of Health Administration, College of Business Administration, King Saud University, Riyadh, Saudi Arabia; 2School of Medicine, St. George’s University, Grenada, West Indies; 3School of Health and Environmental Studies, Hamdan Bin Mohammed Smart University, Dubai, United Arab Emirates
Correspondence: Samer Hamidi, School of Health and Environmental Studies, Hamdan Bin Mohammed Smart University, Dubai Academic City, P.O.Box 71400, Dubai, United Arab Emirates, Tel +971-4-424-1089, Email [email protected]
Background: The prevalence of catheter-associated urinary tract infections (CAUTIs) in hospitals characterizes one of the most significant problems in healthcare. This study aims to assess whether the implementation of impact of key performance indicators (KPIs) checklist reduces the number of CAUTI in adults present in intensive care unit (ICU) with indwelling catheters.
Methods: This is a retrospective analytical study conducted in a tertiary hospital in Riyadh, Saudi Arabia, from June 2020 to June 2021. One hundred and thirty-four patients with CAUTIs met the criteria and were included in the study. Socio-demographic data was collected to enable informed analysis based on personal information (age, gender, marital status, monthly income, level of education, and department) and medical history (duration of catheterization, types of organisms, history of chronic illness, and duration of hospitalization). The research also used a prevention of CAUTI checklist containing 26 items. The outcome measures were 1) the rate of CAUTIs measured pre- and post-implementing performance measurement indicators (KPI) of CAUTIs prevention practice and 2) the prevention of catheter-associated urinary tract infection in three areas: general information recording, insertion practices, and maintenance practices.
Results: The study found that there was compliance with the prevention of CAUTIs in terms of recording the general patient’s information (72%), insertion practices (52%), and maintenance practices (50%). However, most safety practices, including poor hygiene and safety standards, patient handling, and audited protocol programs, were not strictly followed, resulting in increased risk factors for CAUTIs.
Conclusion: Compliance with the prevention of CAUTIs in terms of recording the general patient’s information, insertion practices, and maintenance practices lies within the range of 50– 75%, and the recommended practices are usually followed. A targeted education on CAUTI-prevention practices curtailing the most aggravating risk factors and adopting a safety culture driven by a patient handling and audited protocol program should be explored to reduce hospital CAUTIs.
Keywords: catheter-associated urinary tract infections, CAUTIs, intensive care unit, ICU, urinary catheter, key performance indicator, KPI, checklist
Introduction
Globally, healthcare-associated infections (HAIs) are the leading cause of morbidity and mortality, and the most frequent adverse event in healthcare delivery.1 HAIs include catheter-associated urinary tract infections, ventilator-associated pneumonia, and central line-associated bloodstream infections.2 Catheter-associated urinary tract infections (CAUTIs) are the most common type of HAIs.3 Approximately 75% of hospitals-acquired urinary tract infections (UTIs) are associated with urinary catheters.4 The indwelling urinary catheter is usually used in hospitalized patients for various purposes such as monitoring clinical parameters. When preventive procedures are not implemented, CAUTIs occur with high incidence.
CAUTIs constitute about 4–50% of the HAIs in the United States, where approximately five million patients are put on catheters annually, which increases the average length of stay, use of antibiotics, and the overall cost.1 In developing countries, ICU-acquired infection is at least two to three-fold higher than in high-income countries. In Saudi Arabia, a recent study shows that the prevalence of HAIs was 6.8% among inpatients in six hospitals.5 Another study conducted over 5 years in Saudi Arabia found that CAUTIs constitute about 31% HAIs, and about 42% of HAIs were detected in ICUs.6 Another study in six hospitals from Saudi Arabia, Oman, and Bahrain, which used the National Healthcare Safety Network (NHSN) methodology pooled from, showed that the overall CAUTI rate is 3.2 per 1000 catheter days, 32% higher than the United States.7
Risk Factors
Lengthy use of urinary catheters is the most critical risk factor for developing CAUTIs.4,8 Several studies have shown that females are at higher risk of CAUTIs due to pregnancies, poor nutrition, fecal incontinence, compromised immunity, and illness severity.8 Other patient-related factors that can increase the risk of developing CAUTI include age, patient condition type (surgical vs medical), and patient comorbidities.9 Other system-related factors include lapses in catheter care protocols, insufficient observance of infection control protocols for hand hygiene and aseptic technique for catheter insertion, and lack of knowledge of and adherence to infection control guidelines.10,11
Prevention Strategies and Key Performance Indicators (KPIs)
Key Performance Indicators (KPIs) aim to understand the actual performance of a process and compare it with the best performance (benchmark). In addition, it helps to ascertain and prove the deviation in performance and suggest the necessary improvement. The measurement does not mean the presence of a performance problem, yet it is an opportunity to monitor the actual performance. Therefore, the culture of monitoring and continuous measurement is the core of continuous improvement of the performance of processes and systems. Healthcare organizations must work hard to create and promote a positive culture that strengthens the cohesiveness of teamwork and improve productivity and efficiency in the workplace.
Sterile insertion, locked drainage systems, and appropriate maintenance are recommended to prevent CAUTIs.12,13 The World Health Organization (WHO) suggests specific guidelines to prevent CAUTIs. These include using a locked drainage system, inserting a catheter aseptically, and evaluating the patient on a daily basis. It is not recommended to give patients with indwelling urinary catheters any antibiotics, unless they have a documented infection.14,15
Understanding the culture of safety is crucial to deliver good-quality healthcare and improve patient safety.16 Positive culture of safety contributes to success of interventions, improvement of processes, and prevention of HAIs. It is based on providing support to health workforce, confidence in the effectiveness of preventive measures, and shared perceptions of the importance of safety.17 This study aims to assess whether the implementation of key performance indicators (KPIs) checklist reduces the number of CAUTI among adult patients admitted to intensive care units (ICUs).18
Methodology
This is a retrospective before-and-after study that took place between June 2020 and June 2021, reviewed medical and laboratory records. The eligible study population during the period of the study included 25,517 adult patients admitted to six medical/surgical intensive care units (ICUs) with indwelling catheters from June 2020-June 2021. Only patients with CAUTI presented during their stay in the hospital and were in the ICU units during the data collection period were included in the study. The data were collected using socio-demographic and clinical data sheets. The socio-demographic data sheet included age, gender, marital status, monthly income, level of education, department, and medical history. The clinical data sheet included the duration of catheterization, types of organisms, history of chronic illness, and duration of hospitalization. These were all extracted from the patient’s medical records in these units and daily observations of the nurses. The researcher collected data from baseline records of the medical/surgical intensive care unit (ICU) and compiled data based on the Urinary Tract Infection (UTI) Checklist of the Prevention of Catheter-Associated Urinary.
Study Design
A retrospective analytical study was used in the current study to assess the impact of using KPI measurements on minimizing catheter-associated urinary tract infection (CAUTI) among adult ICU patients. The study population included all adult medical/surgical intensive care unit (ICU) patients available during the study period with indwelling catheters (134 patients). Patients with CAUTI present on admission and other infections of the urinary tract were excluded.
Pre-KPI data were collected from medical records. Post-KPI data were collected using the Urinary Tract Infection (UTI) Checklist, which takes 10–15 min to fill for each patient found with CAUTI. This checklist was initially designed by the US Centers for Disease Control and Prevention (CDC) (2009) to assess preventive measures for catheter-associated urinary tract infections. CDC measured the validity and content reliability of the checklist and indicated its validity and reliability. This checklist contains 26 items on three themes: general information (5 questions), insertion practices (8 questions), and maintenance practices (13 questions).18 According to the checklist, the researcher carried out observations concerning preventing CAUTI in the adult ICU for 3 weeks. Each question on the checklist is coded as zero or one. Assessment total is the sum of points for all marked responses. Possible total is the sum of all possible points for the question. The possible total points for clinical areas general information, insertion practices, and maintenance practices are 10, 16, and 19, respectively. As per the checklist, the total possible points for the three clinical areas are 45. The percentage score (rating) is calculated by dividing the assessment total by the possible total multiplied by 100.18
The percentage score (rating) falls into one of the following three categories:
- Category A: Recommended practices are followed constantly and carefully (>75% of the possible points).
- Category B: Recommended practices are usually followed (50–75% of the possible points).
- Category C: Training and follow-up needed on recommended practices (<50% of the possible points).
Ethical Considerations
Ethical approval was obtained from Humanities Research Ethical Committee at King Saud University, including the aim of the study and confirmation that all data collected, will be kept confidential and used for scientific research only. Informed consent was obtained from the study participants. The Study complies with the Declaration of Helsinki.
Results
Data entry and statistical analysis were done using SPSS 25 statistical software package. Data were presented using descriptive statistics in the form of frequencies and percentages. The mean age of the study participants was 38.4± 16.8 years. The majority of the participants were married females, between the age of 50–60 years old, with low income and primary education, as shown in Table 1. About 94% of study participants had a history of chronic illness. The duration of hospitalization, with the two most frequent being 14 days and 20 days (16%). About 63% of participants indicated that they have a previous history of chronic illness.
 |
Table 1 Socio-Demographic Data for Patients with CAUTI in Adult ICU |
General Information
Results showed that the 100% of indwelling urinary catheters were not reprocessed or reused, and they were bundled in a kit, ready to use. Results also showed that the facility provided continuous education sessions on indwelling urinary catheter insertion. However, results show that about 94% of clinicians did not have access to checklists for practices related to CAUTI prevention. Regarding the items provided by the facility to support prevention of CAUTI, results showed that guidelines for or indwelling urinary catheters were provided in 22% of the cases; a system for documenting insertions of indwelling urinary catheters was provided in 72% of the cases. And a system for documenting removals of indwelling urinary catheters was provided in 6% of the cases. Overall the percentage score of the general information of post-KPI is 72% as shown in Table 2.
 |
Table 2 Assessment Total, Possible Total, and Percent Score for Three Clinical Areas |
Insertion Practices
Main uses of indwelling urinary catheters included acute urinary retention or bladder outlet obstruction, monitoring urine output, urine drainage during surgery, substituting for nursing care in incontinent patients, and obtaining urine specimens. About 97% of patients stated that hand hygiene performed before insertion happens 50% of the time, while 3% of patients stated that hand hygiene is always performed. Results show that indwelling urinary catheters can be inserted by trained personnel in aseptic insertion practices. Overall, percentage score of the insertion practices of post-KPI is 52% post-KPI as shown in Table 2.
Maintenance Practices
About 93% of respondents stated that daily audits to assess the continuous patient need for indwelling catheters were not conducted. About 97% of patients agree that health workers wash their hands when handling an indwelling urinary catheter or collection system. However, 94% of patients agree that the aseptic technique is not followed while removing the indwelling catheter and collection system. All patients stated that the persons who handled their indwelling catheters were trained in aseptic handling practices. All patients stated that the persons who drained their collecting bags were trained in aseptic technique. Most patients (85%) stated that only one practice, having the collecting bag not resting on the floor, was confirmed daily. Only 3% of patients stated that aseptic technique is always followed when removing the indwelling catheter and collection system. Overall, 97% of respondents stated that there is no fixed routine for removing the indwelling catheter and its respective collection system. Only 9% of respondents stated systemic antimicrobials were administered to prevent CAUTI. All the respondents stated that the periurethral area was cleaned with antiseptics while the catheter was in place. All the respondents stated that the bladder was routinely irrigated, regardless of antimicrobial use. Routine bladder irrigation is an applied technique in the organization’s protocol. All the respondents stated that antiseptic or antimicrobial solutions were instilled into the urine collection bags, an applied technique in the organization’s protocol. However, all respondents stated that if urine specimens are needed, then large volumes are aseptically obtained from the drainage bag. However, only 3% of respondents stated that small volumes were obtained aseptically from a needless sampling port. Overall, percentage score of the maintenance practices of post-KPI is 50% as shown in Table 2
Overall, percentage score of the general information improved from 67% pre-KPI to 72% post-KPI, percentage score of the insertion practices improved from 45% pre-KPI to 52% post-KPI, and percentage score of the maintenance practices improved from 40% pre-KPI to 50% post-KPI. Figure 1 presents pre-KPI and post-KPI percentage scores for the three clinical areas.
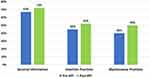 |
Figure 1 Pre-KPI and post-KPI percent score rating. |
These metrics mean that the recommended practices are usually followed, but there needs to be a consolidated effort to address the shortcomings emanating from the shortcomings observed.
Discussion
This paper focused on KPI measurements that impact Catheter-Associated Urinary Tract Infection (CAUTI) among adult ICU patients in the region of Riyadh, Saudi Arabia. KPI measurements are considered an effective tool to assist healthcare organizations in identifying various areas that need to be improved.8 Therefore, the use of KPI measurement may assist healthcare organizations to constantly monitor their operational and systems performance whether there is a need to intervene for quality of services. Hsu et al 2020 observed in their study that the healthcare associated infection (HAI) rate of patient demographic characteristics impact of CAUTI on gender has a higher incidence rate 65% as compared to Mutair et al 2019 findings that indicated (57% rate) in the same similar context.6,19 However, the descriptive statistical analysis indicated that mean age of participants was 38.4± 16.8 years and the baseline stages compose 50–60 years (26%) and 30–40 years (20%), which are consistent with previous study conducted by Letica-Kriegel et al9 The findings of their study indicated risk development of CAUTI increasing with age. The study highlighted the importance of culture of patient safety, which is considered an effective tool to discover areas of improvement. Enhancing culture of safety helps health institutions to identify their area of improvement and continually monitor the performance of their operations and systems regardless of whether there is an urgent need for measurement.
Concerning socio-demographic factors, the study was divided into the following sections: personal information and the patient’s medical history. Concerning personal history, the current study concurs with previous literature that females are at higher risk of developing CAUTI and constitutes a higher percentage of patients with HAI infections than males. The results of the study show that 65% of the CAUTI participants were females, slightly higher than rate 57% rate provided by Mutair et al6 However, findings by Mutair et al 2019 regarding the age prevalence (38.4± 16.8 years) correspond to the findings of this study Mutair et al6 In particular, the research notes that the most prevalent ages are 50–60 years (26%) and 30–40 years (20%), which concurs with findings of Letica-Kriegel et al 2019 on the development risk of CAUTI increasing with age. According to the results of the study show that the prevalence of patients with CAUTI composes 96% of married individuals and 4% of divorced persons.9
The study shows that there is a negative correlation between the education level of participants and CAUTI prevalence in the ICU. This indicates that less educated individuals, such as primary education and basic literate individuals, have a higher affinity to HAI infections than higher academic study individuals. This information consolidates missing literature data on socio-demographic metrics to consolidate existing literature and enhance knowledge on CAUTI prevalence in the ICU. Regarding the prevailing financial situation, there is a noticeable correlation between macro- and micro-economic situations.
Some variables examined compose unexplored, novel research areas in previous literature, expanding the topic’s understanding. The findings of this study indicate that there is a higher prevalence of married individuals than divorced individuals. Also, less educated persons, such as primary education and basic literate individuals, have a higher affinity to HAI infections than individuals with higher academic studies. Concerning a patient’s earning ability, the WHO (2014) notes a significant correlation between a country’s GDP and the incidence, with the instances trickling down to individual earnings as exhibited by the higher incidence amongst persons earning between 5000 and 10,000 SR in comparison with higher earners (10,000–15,000 SR). While the scope of the study does not examine the relationship between macro (country) - and micro (individual) - economic effects on HAI infections, it can be inferred that this corresponds to the level of care given to high-end earners.
Regarding medical history, the current study examines metrics concerned with the duration of catheterization, history of chronic illness, and the duration of hospitalization. Concerning departmental prevalence, the research findings differ from findings of Alshamrani et al on 30% of the cases in developing countries happening in the ICU, with the current study finding a 15.7% and 13.4% in respiratory ICU and step-down ICU.5 While the generalization in the former study may have contributed to the significant difference with the current research, it necessitates further investigation to consolidate the findings. Another crucial factor characterizes the history of chronic illness and the duration of hospitalization. The assertion of a history of chronic illness being a contributing factor by Anggi, Wijaya & Ramayani (2019) holds in the study, with 94% of infections happening to individuals with a prior illness.8
Additionally, the study shows that the average length of stay is about 14.6 days, with 14, 15, and 20 days being the duration time with the highest frequency. Duration of hospitalization is positively correlated with the rate of chronic-illness UTI infection. This corresponds to findings of Anggi, Wijaya & Ramayani (2019) on time-related risk factors being a major contributing factor.8 Anggi, Wijaya, and Ramayani (2019) and Letica-Kriegel et al identify gender as a significant contributing factor, and the effect of these variables on persons with prior chronic illness history shows a very high affinity for both genders, albeit more for females.8,9
Additionally, while hospitals follow best practices in ensuring that indwelling urinary catheters are not reused or reprocessed, they do not come in a buddle kit available for use. Hence, the latter contributes to an increase in the risk of urinary catheter infections by 75%, considering that 15–25% of hospitalized patients receive urinary catheters during their hospital stays.2 Hence, multiple handlings (100% lack of consolidation of catheter insertion kit) correspond to observation of Meddings et al 2013 of lapses of catheter care protocols significantly contributing to UTI.10
The study’s finding on 94% of clinicians lacking access to checklists for practices related to CAUTI prevention also confounds the UTI infection rate, as noted by Atkins et al11 While the facility provides reoccurring education sessions on UTI insertions, it lags in providing guidelines for (21.6%) and removals (6%) of indwelling or insertion urinary catheters, which corresponds to Atkins et al and Fuchs et al findings as a significant contributor to hospital-related infections. Hence, the study corresponds to other literature on the need for best practices such as education, preventive measures, and protocol adherence as necessary for CAUTI prevention efforts.11,20
Insertion practices also contribute significantly to increased CAUTI infections. The study notes 94% usage of indwelling urinary catheters in critically ill and surgery patients, with a 97% hand hygiene rate during the operation, which corresponds to an increase in CAUTI due to lack of hygiene.11 In addition, there is a lack of preventive strategies (Taha et al, 2017), and lapses in catheter care protocols (Meddings et al, 2013), especially while surgical procedures compose a higher risk factor (Letica-Kriegel et al, 2019) in the ICU, especially in developing countries (Alshamrani et al, 2019).5,9,10,12 While all insertion instances consisted of a urinary catheter-trained individual, most insertions (91%) were performed using only lubricating gel. In addition, only 3% of instances used all recommended items (one sterile glove, drape, and sponge, one antiseptic solution for periurethral cleaning, and one single-use packet of lubricant jelly). Additionally, a 94% rate of indwelling catheter securing and an antiseptic supply 50% of the time contravenes the culture of safety associated with CAUTI handling (Braun et al, 2020) in significant risk (Meddings et al, 2013; Atkins et al, 2020; Anggi, Wijaya and Ramayani, 2019).8,10,11,17 Therefore, it necessitates a hospital’s culture of safety change, intervention implementation, and targeted education.16,21
Maintenance practices suffered significant deficiencies in the study, with most practices increasing the risk factors associated with CAUTI. In line with findings of Meddings et al 2013, the risk factor in the study increases given their lack of hand hygiene (97%), daily audit assessment for patients (93.3%), use of sterile gloves in manipulating the collection system or the catheter (94%), following the recommended aseptic technique (97%), change of catheter collection systems (97%), good urine-collection practices, and administering antimicrobial to prevent CAUTI (91%).10 Considering the 50.7% score in maintenance practices lies at the threshold of training and follow-up needed on recommended practices (“CAUTI checklist”, n.d), there needs to be a consolidated effort at decreasing the probability of CAUTI through following catheter care protocols (Meddings et al 2013) and teaching best practices (Atkins et al, 2020; CDC, 2015).10,11
The study exposed harmful practices regarding CAUTI handling in adult ICU instances. While some key preventive measures performed exceptionally well, there was a significant contrariety where there was an utter disregard for other primary practices. Hence, this necessitates a consolidated effort to address key performance indexes that performed poorly. The institution must also insist on a checklist-based treatment plan, with caregivers required to fulfill all preventive measures while handling patients in adult ICU to reduce CAUTI-related instances, with constant practice reviews performed constantly. The study will enhance the widespread implementation of intervention programs, foster CAUTI-related practices, and curtail bad practices from creeping into healthcare institutions. The study also composes objective data that can guide future studies and enable best practice implementation at a local, regional, and national level.
Conclusion
The prevalence of CAUTIs in hospitals is one of the most significant problems and accelerating the cost of healthcare. Hence, this necessitates the examination of key performance indicators in a hospital setting to ascertain the effectuality of CAUTI-related processes. The low percentage score reported for insertion and maintenance practices in this study needs to be of significant concern, considering that the hospital characterizes many bad practices in handling the insertion and maintenance practices of UTIs. Regarding the general information, the study found a 72% score rating showing that the recommended practices are usually followed with proper documentation practices. Regarding insertion practices, the research records a 52% score with notable bad practices observed in hand hygiene practices, lack of safe handling materials, and unsecured catheters. However, some good practices include the use of closed system and qualified personnel to perform the insertion of the catheter. Finally, the maintenance practices score 50, which, although very low, corresponds to the recommended practices usually followed category. Some areas of concern include poor hand hygiene, use of sterilizing procedures in urine collection, administering CAUTI-prevention medication, and changing catheter schedules.
In summary, the pre- and post-KPI score rating for general information, insertion practices, and maintenance practices falls in the recommended practices usually followed rating. However, the study results show good practices in routinely irrigating the bladder, using antiseptics in urine bags, and cleaning the periurethral area with antiseptics to prevent CAUTI while the catheter is in place. The study shows the necessity of training the personnel in good CAUTI-prevention practices and adopting a handling and maintenance protocol to be used in all patient catheter-handling instances to prevent harmful practices from creeping in and increasing patients’ instances.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors declare that they have no conflicts of interest in relation to this work.
References
1. Mukhit Kazi M. Catheter Associated Urinary Tract Infections (CAUTI) and antibiotic sensitivity pattern from confirmed cases of CAUTI in a tertiary care hospital: a prospective study. Clin Microbiol. 2015;4(2). doi:10.4172/2327-5073.1000193
2. Centers for disease control and prevention, Healthcare Associated Infections (HAI); 2015. Available from: https://www.cdc.gov/hai/infectiontypes.html#:~:text=Infections%20can%20be%20associated%20with,%2C%20and%20ventilator%2Dassociated%20pneumonia.
3. Werneburg GT. Catheter-associated urinary tract infections: current challenges and future prospects. Res Rep Urol. 2022;14:109–133. doi:10.2147/RRU.S273663
4. Catheter-associated Urinary Tract Infections (CAUTI), HAI, CDC; 2015. Available from: https://www.cdc.gov/hai/ca_uti/uti.html.
5. Alshamrani MM, El-Saed A, Alsaedi A, et al. Burden of healthcare-associated infections at six tertiary-care hospitals in Saudi Arabia: a point prevalence survey. Infect Control Hosp Epidemiol. 2019;40(3):355–357. doi:10.1017/ice.2018.338
6. Mutair AA, Alhumaid S, Alawi ZA, et al. Five-year resistance trends in pathogens causing healthcare-associated infections at a multi-hospital healthcare system in Saudi Arabia, 2015–2019. J Glob Antimicrob Resist. 2021;25:142–150. doi:10.1016/j.jgar.2021.03.009
7. Al Nasser W, El-Saed A, Al-Jardani A, et al. Rates of catheter-associated urinary tract infection in tertiary care hospitals in 3 Arabian Gulf countries: a 6-year surveillance study. Am J Infect Control. 2016;44(12):1589–1594. doi:10.1016/j.ajic.2016.06.030
8. Anggi A, Wijaya DW, Ramayani OR. Risk factors for catheter-associated urinary tract infection and uropathogen bacterial profile in the intensive care unit in hospitals in Medan, Indonesia. Open Access Maced J Med Sci. 2019;7(20):3488–3492. doi:10.3889/oamjms.2019.684
9. Letica-Kriegel AS, Salmasian H, Vawdrey DK, et al. Identifying the risk factors for catheter-associated urinary tract infections: a large cross-sectional study of six hospitals. BMJ Open. 2019;9(2):e022137. doi:10.1136/bmjopen-2018-022137
10. Meddings J, Rogers MAM, Krein SL, Fakih MG, Olmsted RN, Saint S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: an integrative review. BMJ Qual Saf. 2014;23(4):277–289. doi:10.1136/bmjqs-2012-001774
11. Atkins L, Sallis A, Chadborn T, et al. Reducing catheter-associated urinary tract infections: a systematic review of barriers and facilitators and strategic behavioural analysis of interventions. Implement Sci. 2020;15(1):1–44. doi:10.1186/s13012-020-01001-2
12. Taha H, Raji SJ, Khallaf A, et al. Improving catheter associated urinary tract infection rates in the medical units. BMJ Qual Improv Rep. 2017;6(1):
13. Obaid NA. Preventive measures and management of catheter-associated urinary tract infection in adult intensive care units in Saudi Arabia. J Epidemiol Glob Health. 2021;11(2):164–168. doi:10.2991/jegh.k.210418.001
14. Köves B, Magyar A, Tenke P. Spectrum and antibiotic resistance of catheter-associated urinary tract infections. GMS Infect Dis. 2017;5:Doc06. doi:10.3205/id000032
15. Tenke P, Mezei T, Bőde I, Köves B. Catheter-associated urinary tract infections. Eur Urol Suppl. 2017;16(16):138–143. doi:10.1016/j.eursup.2016.10.001
16. Gammon J, Hunt J, Williams S, Daniel S, Rees S, Matthewson S. Infection prevention control and organisational patient safety culture within the context of isolation: study protocol. BMC Health Serv Res. 2019;19(1):296. doi:10.1186/s12913-019-4126-x
17. Braun BI, Chitavi SO, Suzuki H, Soyemi CA, Puig-Asensio M. Culture of safety: impact on improvement in infection prevention process and outcomes. Curr Infect Dis Rep. 2020;22(12):34. doi:10.1007/s11908-020-00741-y
18. Urinary Tract Infection (UTI) checklist; 2022. Available from: https://www.cdc.gov/nhsn/pdfs/checklists/uti-checklist-508.pdf.
19. Hsu HE, Wang R, Broadwell C, et al. Association between federal value-based incentive programs and health care–associated infection rates in safety-net and non–safety-net hospitals. JAMA Netw Open. 2020;3(7):e209700. doi:10.1001/jamanetworkopen.2020.9700
20. Fuchs MA, Sexton DJ, Thornlow DK, Champagne MT. Evaluation of an evidence-based, nurse-driven checklist to prevent hospital-acquired catheter-associated urinary tract infections in intensive care units. J Nurs Care Qual. 2011;26(2):101–109. doi:10.1097/NCQ.0b013e3181fb7847
21. Encourage II. Does improving safety culture affect patient outcomes?; 2011; Available from: https://www.health.org.uk/sites/default/files/DoesImprovingSafetyCultureAffectPatientOutcomes.pdf.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
