Back to Journals » Psychology Research and Behavior Management » Volume 16
Impact of Easing COVID-19 Restrictions on Fear of COVID-19 and Social Support Among Chinese Students: A Longitudinal Analysis
Authors Zhao Y, Wang R, Li H , Chen C, Zhou B, Weng X , Hua Y, Jia Y, Wu Y, Li Y
Received 10 August 2023
Accepted for publication 13 November 2023
Published 20 November 2023 Volume 2023:16 Pages 4685—4696
DOI https://doi.org/10.2147/PRBM.S434765
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Yang Zhao,1 Ruizhe Wang,2 Hebin Li,3 Chong Chen,4 Bowen Zhou,5 Xinying Weng,3 Yidi Hua,6 Yaqi Jia,7 Yajun Wu,8 Ying Li9
1Faculty of Law, Qingdao University, Qingdao, People’s Republic of China; 2HeXie Management Research Center, Xi’an Jiaotong-Liverpool University, Suzhou, People’s Republic of China; 3Department of Social and Behavioural Sciences, City University of Hong Kong, Hong Kong, People’s Republic of China; 4CAS Key Laboratory of Behavioral Science, Institute of Psychology, Chinese Academy of Sciences, Beijing, People’s Republic of China; 5Department of Social Work, Hong Kong Baptist University, Hong Kong, People’s Republic of China; 6School of Humanities and Social Science, The Hong Kong University of Science and Technology, Hong Kong, People’s Republic of China; 7Entrepreneurs College, Xi’an Jiaotong-Liverpool University, Suzhou, People’s Republic of China; 8Department of Applied Psychology, Guangdong University of Foreign Studies, Guangzhou, People’s Republic of China; 9School of Urban Governance and Public Affairs, Suzhou City University, Suzhou, People’s Republic of China
Correspondence: Ying Li, Email [email protected]
Introduction: This longitudinal study aims to investigate the relationship between fear of COVID-19, support-seeking behaviors, and perceived social support among Chinese college students during two distinct periods of the COVID-19 pandemic: the period of strict control (time 1) and the period following a relaxation of restrictions (time 2).
Methods: A total of 408 Chinese college students participated in this study. Data collection included demographic information, measures of fear of COVID-19, support-seeking behaviors, and perceived social support.
Results: Fear of COVID-19 at time 1 showed a significant positive association with fear of COVID-19 at time 2. The relationship between support-seeking behavior at time 1 and fear of COVID-19 at time 2 was significantly mediated through a chain mediation effect of support-seeking behavior at time 1 and perceived social support at time 2.
Discussion: This study contributes to the growing body of evidence on the psychological impacts of the COVID-19 pandemic and underscores the significance of social support in mitigating fear of COVID-19. It calls for a re-evaluation of public health policies considering their potential psychological effects and introduces new opportunities for developing psychosocial interventions.
Keywords: fear of COVID-19, social support, Chinese students, COVID-19 policy, longitudinal study
Introduction
The COVID-19 pandemic, which surfaced in December 2019, has left a deep global impact, severely affecting both public health and economic sectors.1,2 By January 2023, the pandemic had led to nearly 664 million confirmed cases and over seven million fatalities across 223 countries.3 Despite the widespread distribution of vaccines and the relaxation of control measures in various regions, the pandemic consequences persist on a global scale. In the face of a crisis of this magnitude, effective crisis management is vital to mitigate further public health challenges.4,5 The Chinese government’s implementation of a strict zero-tolerance strategy, in effect until December 2022, played a pivotal role in curbing the virus’s spread. However, as the virus became less lethal, the government adjusted its approach, signaling a diminishing public health concern.6
The unpredictability brought by the pandemic disrupted the innate human desire for stability, resulting in a surge in mental health issues, including depression, trauma-induced stress, and anxiety.7,8 Nonetheless, the Chinese government’s rigorous policies fostered a sense of stability, distinguishing it from countries like the United States and Italy.9 However, this prolonged stability might have inadvertently reduced the overall awareness and perceived immediacy of COVID-19 among the Chinese population.10
As control measures were eased and a prolonged sense of safety prevailed, mainland China witnessed a renewed sense of apprehension and anxiety regarding COVID-19.11,12 This heightened concern manifested in a rush for anti-epidemic medications, reduced travel, and a scarcity of medical resources.13 Prior traumatic events, such as the initial outbreak in Wuhan, may have exacerbated vigilance and stress surrounding COVID-19 for the Chinese populace.14 Furthermore, the psychological challenges of transitioning from stringent restrictions to a more open society became apparent.15 Specifically, Chinese college students, a demographic highly attuned to societal shifts and expectations, experienced pronounced effects.16 Their narratives provide insight into the wide-ranging societal challenges encountered during this transition.
This study investigates the psychological and societal consequences of relaxing COVID-19 measures in China, with a focus on the experiences of Chinese college students. By examining their fear of COVID-19, support-seeking behaviors, and perceptions of social support, we aim to shed light on the broader implications of policy changes during global health emergencies.
Literature Review
Fear of COVID-19
Fear, a fundamental adaptive emotion, arises when individuals perceive threats or potential harm.8,17 The COVID-19 pandemic, with its extensive impact and persistent unpredictability, has triggered this emotion on an unprecedented global scale. Factors contributing to this fear include concerns about personal health, the well-being of loved ones, experiences of social isolation, economic volatility, and uncertainties regarding career prospects. Taken together, these concerns can heighten the risk of mental health disorders and, in some cases, lead to thoughts of suicide.18
College students, in particular, are vulnerable to the tumultuous changes brought about by the pandemic. The closure of academic institutions has confined many to their family homes, while necessary social distancing measures have limited their interactions with peers and faculty.19 Adding to these challenges, the economic consequences of the pandemic have resulted in widespread job losses, leading to significant career-related anxieties among this demographic.8,20 While navigating this critical phase of life, these students, who are already prone to mental health challenges during major life transitions, are confronted with heightened stressors arising from academic obligations and uncertainty about their professional paths.21–23
Social Support Under the COVID-19 Pandemic
Lazarus and Folkman’s seminal stress coping theory24–26 provides a valuable framework for understanding the psychological impact of the pandemic. This theory emphasizes coping mechanisms as transactional, categorizing them into problem-focused and emotion-focused strategies. The former, which includes resource mobilization and seeking social support, is crucial during sudden crises like disease outbreaks.27 Existing literature suggests that individuals with strong coping abilities are better at navigating and recovering from stress-inducing events.28,29 Effective problem-focused coping, when combined with appropriate cognitive and emotional processing, can significantly reduce vulnerabilities to stress-related mental health issues. Leveraging social support as a coping mechanism is considered a problem-focused strategy,30 and its effectiveness in alleviating stress is well-documented. Furthermore, perceiving social support from colleagues, family, and friends is essential for maintaining emotional stability during times of adversity and tension.31
Fear of COVID-19 and Social Support
The COVID-19 pandemic has given rise to a pervasive atmosphere of fear. Paradoxically, this environment can also strengthen a sense of unity and interdependence among individuals. Shared adversities and objectives, especially in crises, can foster cooperation, altruism, and group cohesion. This idea aligns with a combination of evolutionary models and social psychological perspectives.32–35
In China, collective efforts, exemplified by community-wide nucleic acid testing, have showcased the power of working together to maintain low infection rates. The visible successes of these collaborative endeavors have reinforced individuals’ belief in their collective resilience, a concept known as collective self-efficacy.36,37 Such a united response to a widespread health threat underscores the vital role of societal bonds and mutual support in navigating crises.
Studies have suggested that fear can motivate individuals to engage in collective efforts that enhance the well-being of the community, ranging from following health advisories to participating in mutual aid.38 Active participation in task-oriented community groups during crises can alleviate feelings of despair and increase optimism.3,39 However, the relationship between the fear induced by COVID-19 and the perception of social support remains relatively unexplored. While previous research during different health outbreaks offers initial insights,40 the complex dynamics unique to the COVID-19 pandemic warrant further investigations. Social support, stemming from various sources, whether it’s family, peers, or institutions, has the potential to modulate fear responses, positively affecting both psychological and physiological well-being.41–45
For the student cohort during the pandemic, the effects of social support remain somewhat unclear. While some studies suggest that social support can alleviate fears related to job security and COVID-19 in specific demographics,46,47 the unique challenges students face, such as the shift to virtual education, may limit the applicability of these findings. Furthermore, the long-term consequences of social support during pandemic events are yet to be definitively determined. Robust social support has been linked to reductions in depression, anxiety, and overarching psychological distress post-crisis, but its impact on post-traumatic stress manifestations remains uncertain.48–50
Given the emergence of COVID-19 variants with varying virulence, like Omicron, the continuous assessment of evolving fear dynamics and associated social response is essential. Amid fluctuating infection patterns and the diverse spectrum of fear experienced by university students, exam ining the role of perceived social support in mitigating fear becomes crucial, especially through longitudinal research methods. Such an investigative trajectory promises to elucidate the temporal shifts in fear intensity alongside the pandemic’s progression and the evolution of policy responses.
Support Seeking and Perceived Social Support
Support-seeking behavior is a widely recognized coping strategy that individuals frequently employ in response to challenges.51 This adaptive, problem-focused approach involves actively seeking information, guidance, and emotional reassurance as a means to address and navigate the perceived challenge.24,52,53 Contemporary research outlines three fundamental phases inherent in support-seeking behavior: (1) Recognizing the problem; (2) Deciding to seek help; and (3) Choosing a source of assistance.54,55
Amid the COVID-19, the psychological upheavals induced by the virus—manifested as heightened anxiety, panic episodes, sleep disruptions, and irritability—may enhance support-seeking tendencies. Especially when individuals perceive limited personal coping resources in the face of this unprecedented threat, they are inclined to seek external assistance to alleviate their concerns and refine their coping strategies.
The Protection Motivation Theory (PMT) provides a robust framework for understanding this behavior.56 PMT elucidates the mechanisms through which individuals interpret and respond to fear-inducing stimuli, such as severe health threats like COVID-19. The theory posits that an individual’s assessment of a threat, including its severity and their vulnerability to it, can trigger fear, which subsequently catalyzes tendencies to seek help. Simultaneously, an assessment of coping strategies, which evaluates the available tools and their perceived effectiveness, can influence the inclination to seek assistance. This depends on the individual’s belief that such behavior will effectively mitigate the threat and enhance well-being. Recent empirical evidence supports an increase in help-seeking tendencies in regions dealing with the pandemic, reinforcing this aspect of PMT.57
Furthermore, when individuals actively engage in support-seeking, they emphasize the importance of social connection and their faith in the reservoir of support within their networks.58 Such a deliberate quest for support signifies confidence in one’s social fabric and enhances the perception of existing social support—a critical indicator of an individual’s perceived worth and integration within their social environment, founded on mutual communication and reciprocity.59–61 Notably, the mere perception of such support often has a more significant impact on mental and physical health improvements than tangible support received. It serves as a protective barrier against psychological challenges (eg, Li et al, 2015; McDowell and Serovich, 2007).62,63
Current Study
Despite the plethora of research on online social interactions and their implications in the digital age, the dynamics of face-to-face interactions, particularly in crisis contexts, have remained relatively underexplored. The COVID-19 pandemic introduced an unprecedented context, impacting both online and offline social behaviors. For instance, although studies have discovered positive correlations between help-seeking behaviors and perceived social support among online communities,64 it remains unclear whether these findings can be extended to face-to-face interactions during the pandemic. Addressing this gap is essential for comprehending how individuals navigate their social worlds in times of global crises. This study aims to contribute to this body of knowledge by exploring the relationship between fear of COVID-19, support-seeking behaviors, and perceived social support in offline contexts.
Based on the aforementioned rationale, the following hypotheses are proposed (as shown in the conceptual framework in Figure 1):
Hypothesis 1 (H1): Fear of COVID-19 at time 1 will be positively associated with fear of COVID-19 at time 2. Hypothesis 2 (H2): Support-seeking behavior at time 1 will mediate the relationship between fear of COVID-19 at time 1 and perceived social support at time 2. Hypothesis 3 (H3): Support-seeking behavior at time 1 will mediate the relationship between fear of COVID-19 at time 1 and fear of COVID-19 at time 2. Hypothesis 4 (H4): The relationship between support-seeking behavior at time 1 and fear of COVID-19 at time 2 will be mediated through a chain mediation effect of support-seeking behavior at time 1 and perceived social support at time 2.
 |
Figure 1 Conceptual model. Notes: T1= at Time 1; T2 = at Time 2. |
Method
Participants and Procedures
To address safety and social distancing requirements during the COVID-19 outbreak period, we conducted a longitudinal study using two-wave online self-administered surveys to collect data for this study. The first wave of data collection took place in November 2022 (Time 1), during a period when the Chinese government implemented strict control measures. The second wave of data collection occurred from the end of December 2022 to January 2023 (Time 2; about two months after Time 1), following the relaxation of control measures in the COVID-19 policy.
We used online posters to disseminate invitations to participate in the study, providing details about the survey link, the study’s objectives, confidentiality policies, and contact information for the researchers. Participation in this study was voluntary and anonymous.
The initial criterion for participation in this study was being a currently enrolled undergraduate student in a Chinese university, and consent provided through a consent form. Exclusion criteria involved not being an undergraduate student or not being enrolled in a Chinese university during the specified time frame. All valid participants were undergraduate students currently studying at Chinese universities. In total, 408 participants (mean age = 20.67 ± 5.59 years), including 141 males (34.6%) and 267 females (65.4%), from five universities in three Chinese cities, took part in the study. The dataset contained no missing entries, as participants were required to complete all survey components before submission. All participants in the research were adults, for whom the requirement for parental informed consent was waived. Informed consent was obtained directly from each participant prior to their participation, ensuring compliance with the Declaration of Helsinki.
Measures
Demographic Information
Participants provided information on their age, gender (coded as 0 for male and 1 for female), and region of study.
Fear of COVID-19
In this study, we employed the Fear of the COVID-19 Scale (FCV-19S)65 to measure fear of COVID-19. The FCV-19S comprises seven items that assess two factors: physical fear response and fear thinking. Participants rated each item on a five-point scale (1 = disagree; 5 = completely agree), for example: “It makes me uncomfortable to think about coronavirus-19”. Higher mean scores on this scale indicate greater levels of fear of COVID-19. The FCV-19S demonstrated good internal consistency with a Cronbach’s alpha of 0.89.
Support Seeking
Support seeking was assessed using the eleven items Seeking Social Support of Coping Strategy Indicator (CSI).66,67 The CSI was rated on a three-point scale (1 = not at all; 3 = a lot), for example: “Sought friends for advice”. Higher mean scores on this scale indicate a greater level of support seeking. The CSI was translated into Chinese by,68 and showed a Cronbach’s alpha of 0.85.
Perceived Social Support
Perceived social support was assessed using six items COVID-19 Version Perceived Social Support Questionnaire (F-SozU), developed by69 and adapted from the Perceived Social Support Questionnaire70 to measure perceived social support during the COVID-19 pandemic. Participants rated each item on a 5-point scale, ranging from 1 = not at all true to 5 = very true). For example, “If I get sick, I have friends and family who will take care of me”. A higher mean score on this scale indicate a greater level of perceived social support. The F-SozU was validated in Chinese populations by71 and demonstrated good internal consistency, with a Cronbach’s alpha coefficient of 0.83.
Statistical Analysis
We performed data analysis using SPSS 27.0 software. Descriptive analyses were conducted to examine the demographic variables. Bivariate correlations among fear of COVID-19, support seeking, and perceived social support were explored using Pearson’s correlation coefficient. We examined the mediating roles of fear of COVID-19 at Time 1 and Time 2 using Model 6 in the SPSS PROCESS macro version 3.5.3.72 Bootstrap estimates were resampled 5000 times to calculate 95% confidence intervals of the indirect effects. A mediating effect was considered significant at p < 0.05 if the confidence interval did not include zero.
Results
The current study yielded insights into the relationships among fear of COVID-19, seeking social support, and perceived social support at two different time points.
Descriptive Statistics and Correlations
As illustrated in Table 1, fear of COVID-19 at time 1 exhibited significant positive correlations with fear of COVID-19 at time 2, perceived social support at time 2, and seeking social support at time 1. Conversely, seeking social support at time 1 showed a negative correlation with fear of COVID-19 at time 2.
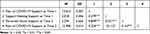 |
Table 1 Correlations Among Variables |
The study evidenced that fear of COVID-19 at time 1 was positively correlated with fear of COVID-19 at time 2 (r = 0.324, p < 0.01), as well as with perceived social support at time 2 (r = 0.849, p < 0.01) and seeking social support at time 1 (r = 0.279, p < 0.01). Seeking social support at time 1 was negatively correlated with fear of COVID-19 at time 2 (r = −0.112, p < 0.01), while perceived social support at time 2 was positively correlated with fear of COVID-19 at time 2 (r = 0.167, p < 0.01). Moreover, the correlation between seeking social support at time 1 and perceived social support at time 2 was in the expected direction (r = 0.521, p < 0.01).
Chain Mediation Model Analysis
Table 2 presents the results of the chain mediation model analysis, which examined the mediating effect of seeking social support at time 1 and perceived social support at time 2 in the relationship between fear of COVID-19 at time 1 and fear of COVID-19 at time 2. The findings revealed several key relationships. Fear of COVID-19 at time 1 was a significant positive predictor of fear of COVID-19 at time 2 (β =0.23, p < 0.001), supporting H1. Fear of COVID-19 at time 1 emerged as a significant predictor of its level at time 2. Meanwhile, both seeking social support at time 1 (β = −0.15, p < 0.05) and perceived social support at time 2 (β = −0.24, p < 0.05) were significant negative predictors of fear of COVID-19 at time 2. And the direct path from fear of COVID-19 at time 1 to fear of COVID-19 at time 2 (β = 0.56, p < 0.001) was significant. Additionally, the direct effect of fear of COVID-19 at time 1 on seeking social support at time 1 (β = 0.28, p < 0.001) and perceived social support at time 2 (β = 0.76, p < 0.001) was significant. In line with H2 and H3, both seeking social support at time 1 and perceived social support at time 2 were significant negative predictors of fear of COVID-19 at time 2.
 |
Table 2 Regression Analysis of Relationship Between Fear of COVID-19 at Time 1 and Fear of COVID-19 at Time 2 with Mediation Analyses |
Mediation Effects
The results presented in Table 3 demonstrate a significant cascading mediating effect between fear of COVID-19 at time 1 and fear of COVID-19 at time 2. Specifically, seeking social support at time 1 and perceived social support at time 2 acted as significant mediators between fear of COVID-19 at time 1 and fear of COVID-19 at time 2 (β = −0.24, SE = 0.08, 95% CI = −0.4034 to −0.0848). Furthermore, all predicted indirect paths in the mediation model were significant: (1) Path 1 (H2): fear of COVID-19 at time 1→ seeking social support at time 1→ fear of COVID-19 at time 2 (β = −0.04, SE = 0.08, 95% CI = −0.0788 to. −0.0094); (2) path 2 (H3): fear of COVID-19 at time 1 → perceived social support at time 2 → fear of COVID-19 at time 2 (β = −0.18, SE = 0.08, 95% CI = −0.3337 to. −0.0312). (3) path 3 (H4): fear of COVID-19 at time 1 → seeking social support at time 1 → perceived social support at time 2 → fear of COVID-19 at time 2 (β = −0.02, SE = 0.01, 95% CI = −0.0420 to −0.0034). Since the 95% confidence intervals for all of these paths did not include a value of 0, the results confirmed that H4 was supported. Specifically, seeking social support at time 1 and perceived social support at time 2 significantly mediated the relationship between fear levels of COVID-19 at the two-time points.
 |
Table 3 Fear of COVID-19 at Time 1 and Fear of COVID-19 at Time 2 in the Mediation Effect Analysis |
Discussion
This longitudinal study, grounded in the framework of social support theory,73 aimed to elucidate the complex interplay between social support and the dynamic fear associated with COVID-19 among college students. Our findings robustly validated our hypotheses, shedding light on a significant increase in fear levels following the government’s shift toward more lenient pandemic control measures. Importantly, the results emphasize the critical role of social support and support-seeking behavior in mitigating the apprehension and anxiety induced by COVID-19.
The observed escalation in fear levels related to COVID-19 after the relaxation of preventive measures aligns with previous research. Prior studies have suggested that fear and anxiety levels fluctuate over the course of an epidemic and are significantly influenced by public health interventions.74 For example, during the Severe Acute Respiratory Syndrome (SARS) outbreak in Taiwan, anxiety levels peaked during the initial phase but declined as containment strategies were implemented.75 This study expands on this understanding, highlighting how shifts in public health directives and policy changes can influence fear and anxiety levels. These insights hold significant implications for future policy development.76
Role of Social Support in Mitigating Fear of COVID-19
Social support theory posits that strong social relationships and networks act as protective buffers, shielding individuals from the adverse consequences of stressors, including fear, anxiety, and depression.73 This investigation elucidated the multifaceted ways in which social support can mitigate fears associated with COVID-19, encompassing emotional, informational, tangible, and appraisal dimensions of support.77–79
The fear surrounding COVID-19 characterized as a multidimensional construct, encompasses both the physiological and psychological aspects of apprehension and anxiety related to virus.80 This fear can motivate individuals to seek social support from their connections. Grounded in the concept of collective efficacy, this act of seeking support can enhance individuals’ abilities to protect themselves and their communities from the virus.81,82 This theoretical perspective provides a compelling rationale for the observed positive correlation between the fear of COVID-19 and perceived social support.
Perceived Social Support and Collective Efficacy
Empirical studies consistently indicate a positive correlation between fear of COVID-19 and perceived social support. This suggests that individuals experiencing heightened fear tend to perceive stronger affiliations and support from their social circles.57,83 This correlation may be attributed to an increased awareness of vulnerability and potential hazards associated with the pandemic, compelling individuals to seek and perceive higher levels of social support to navigate prevailing uncertainties.71 Furthermore, research has suggested that perceived social support can serve as a protective buffer, attenuating the adverse psychological consequences of fear and anxiety.84
A pronounced sense of collective efficacy, rooted in robust social networks and mutual trust, also influences the intensity of individuals’ fear responses. For instance, individuals residing in regions characterized by abundant social capital exhibited lower fear levels concerning COVID-19.85 These observations suggest that strengthening social ties and support networks can play a crucial role in reducing fear levels and fostering a stronger sense of collective efficacy. Consequently, collective efficacy and perceived social support are interconnected, serving as valuable assets in reducing fear and anxiety, thereby enhancing individual and communal resilience.86
Support Seeking: Opportunities and Challenges
During the COVID-19 pandemic, support-seeking has emerged as a vital mechanism for nurturing resilience. Such support can manifest in various forms, including interpersonal, professional, and community-based support.87 However, inherent challenges, such as societal stigmatization and limited access to support, need acknowledgment and remediation.88 Throughout the pandemic, community and professional support paradigms have risen as indispensable pillars, correlating with increased resilience and better mental health outcomes in crisis situations.49,89,90
Theoretical and Practical Implications
This study’s findings offer insights of both theoretical and practical significance. The research contributes to our understanding of post-COVID-19 mental well-being by providing a framework for interpreting the fluctuations in fear and anxiety witnessed throughout the pandemic, emphasizing the interplay of uncertainty and social support.91
Practically, the results underscore the importance of evaluating the psychological impact of public health interventions. Policymakers must recognize the potential consequences of policy shifts on the fluctuations of fear and anxiety related to COVID-19 to prevent a resurgence of infection surges.92 In clinical practice, it is crucial to acknowledge the potential psychological burden of the pandemic. Initiatives promoting social support can serve as powerful tools in mitigating associated fear and anxiety.76
Policy and Public Health Interventions
The fluctuations in fear levels in response to changes in public health measures align with prior research suggesting that public sentiment, specifically fear and anxiety, can be significantly influenced by the stringency of public health interventions.93 Policy shifts, especially those affecting public health, often have a profound psychological impact on the population. The nature and immediacy of these policies can either alleviate or exacerbate existing anxieties. Chinese experience during the SARS outbreak manifested a similar trajectory where initial heightened anxiety tapered with stringent control measures.94,95 This study emphasizes the need for policymakers to be aware of these psychological consequences when designing and implementing public health strategies. A comprehensive approach that combines epidemiological strategies with psychological insights may lead to more effective and well-received public health interventions.
Limitations and Future Directions
While this study provides valuable insights into the relationship between social support and the fear of COVID-19 among college students, several limitations should be acknowledged. Firstly, the longitudinal design, while offering temporal depth, may be vulnerable to participant attrition, potentially affecting the results or reducing statistical power.96 Additionally, relying on self-reported data may introduce social desirability or recall biases. The use of an online survey platform, though convenient, might inadvertently exclude individuals with limited internet access or technological proficiency, resulting in a selection bias. Moreover, the relatively small sample size, limited to college students from a singular Chinese city, may impact the study’s statistical robustness and generalizability of its findings.97 Future research should aim to diversify participant demographics across various locations, employ mixed-method approaches for a more nuanced understanding, increase sample sizes, and explore alternative data collection techniques. These refinements will contribute to a more comprehensive understanding of the complex relationship between social support and the psychological repercussions of global health disruptions.
Conclusion
In summary, this longitudinal study investigated the fear of COVID-19 among Chinese college students during two distinct periods of the pandemic–while strict control measures were in place and after their relaxation. The findings revealed a significant increase in fear levels following the government’s policy changes, underscoring the potential psychological impact of public health measures. Additionally, the study emphasized the crucial role of support-seeking behaviors and perceived social support in alleviating the fear of COVID-19. This study is significant because it underscores the value of collective efficacy and social support systems in reducing crisis-related fear, which can subsequently enhance individual and community resilience during health crises. By providing empirical evidence of the association between social support and fear of COVID-19, it opens new avenues for the development of psychosocial interventions and calls for a re-evaluation of public health policies to consider their potential psychological impacts.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
This study has been approved by the Survey and Behavioural Research Ethics Committee of the Qingdao University.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
2. Acter T, Uddin N, Das J, Akhter A, Choudhury TR, Kim S. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency. Sci Total Environ. 2020;730:138996. doi:10.1016/j.scitotenv.2020.138996
3. Ghebreyesus TA. The WHO special initiative for mental health (2019–2023): universal health coverage for mental health [Internet]. JSTOR; 2019. Available from: https://www.jstor.org/stable/resrep28223.
4. Panneer S, Kantamaneni K, Akkayasamy VS, et al. The great lockdown in the wake of COVID-19 and its implications: lessons for low and middle-income countries. Int J Environ Res Public Health. 2022;19(1):610. doi:10.3390/ijerph19010610
5. Crow DA, DeLeo RA, Albright EA, et al. Policy learning and change during crisis: COVID‐19 policy responses across six states. Rev Policy Res. 2023;40(1):10–35. doi:10.1111/ropr.12511
6. Nordin J. China’s Pandemic Shift: The End of Dynamic Zero-COVID. Institute for Security and Development Policy; 2023.
7. Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J Psychiatr. 2020;51:101990. doi:10.1016/j.ajp.2020.101990
8. Zhou T, Bao Y, Guo D, et al. Intolerance of uncertainty and future career anxiety among Chinese undergraduate students during COVID-19 period: fear of COVID-19 and depression as mediators. Front Public Health. 2022;10:1015446. doi:10.3389/fpubh.2022.1015446
9. Wong JY, Wai AK, Wang MP, et al. Impact of COVID-19 on child maltreatment: income instability and parenting issues. Int J Environ Res Public Health. 2021;18(4):1501. doi:10.3390/ijerph18041501
10. Lu Q, Atadil HA. Do you dare to travel to China? An examination of China’s destination image amid the COVID-19. Tour Manag Perspect. 2021;40:100881. doi:10.1016/j.tmp.2021.100881
11. Sun R, Ye X, Tang J, Yang J, Scott N. The impact of the intensity of media use on potential tourists’ risk perception and travel protective behavioral intentions in COVID-19. Front Psychol. 2023;14. doi:10.3389/fpsyg.2023.1201481
12. Zhao S, Sha T, Xue Y, Chen H. Flattening the curve: imperative when China eases the severe COVID-19 control policy. J Infect. 2023;86(3):e75–e77. doi:10.1016/j.jinf.2022.12.022
13. Tu K, Reith A. Changes in urban planning in response to pandemics: a comparative review from H1N1 to COVID-19 (2009–2022). Sustainability. 2023;15(12):9770. doi:10.3390/su15129770
14. Ye Z, Yang X, Zeng C, et al. Resilience, social support, and coping as mediators between COVID‐19‐related stressful experiences and acute stress disorder among college students in China. Appl Psychol. 2020;12(4):1074–1094. doi:10.1111/aphw.12211
15. Shevlin M, Butter S, McBride O, et al. Refuting the myth of a ‘tsunami’of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol Med. 2023;53(2):429–437. doi:10.1017/S0033291721001665
16. Yu T, Dai J, Wang C. Adoption of blended learning: Chinese university students’ perspectives. Humanit Soc sci. 2023;10(1):1–6. doi:10.1057/s41599-023-01904-7
17. Shahnawaz M, Nabi W, Nabi S, et al. Relationship between intolerance of uncertainty and symptom severity in Covid-19 patients: the mediating role of illness perception and Covid-19 fear. Curr Psychol. 2022;2022;1–8.
18. Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(6):468–471. doi:10.1016/S2215-0366(20)30171-1
19. Wang H, Paulson KR, Pease SA, et al. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet. 2022;399(10334):1513–1536. doi:10.1016/S0140-6736(21)02796-3
20. Schleicher A. The Impact of COVID-19 on Education: Insights From” Education at a Glance 2020”. OECD Publishing; 2020.
21. Cvetkovski S, Reavley NJ, Jorm AF. The prevalence and correlates of psychological distress in Australian tertiary students compared to their community peers. Aust N Z J Psychiatry. 2012;46(5):457–467. doi:10.1177/0004867411435290
22. Barnett P, Mackay E, Matthews H, et al. Ethnic variations in compulsory detention under the mental health act: a systematic review and meta-analysis of international data. Lancet Psychiatry. 2019;6(4):305–317. doi:10.1016/S2215-0366(19)30027-6
23. Blanco C, Okuda M, Wright C, et al. Mental health of college students and their non–college-attending peers: results from the national epidemiologic study on alcohol and related conditions. Arch Gen Psychiatry. 2008;65(12):1429–1437. doi:10.1001/archpsyc.65.12.1429
24. Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer publishing company; 1984.
25. Folkman S, Lazarus RS. If it changes it must be a process: study of emotion and coping during three stages of a college examination. J Pers Soc Psychol. 1985;48(1):150. doi:10.1037/0022-3514.48.1.150
26. Lazarus RS, Folkman S. The concept of coping. In: Stress and Coping: An Anthology. Columbia University Press; 1991:189–206.
27. Bhattacharjee A, Ghosh T. COVID-19 pandemic and stress: coping with the new normal. J Prev Health Promot. 2022;3(1):30–52. doi:10.1177/26320770211050058
28. Duncan DL. What the COVID-19 pandemic tells us about the need to develop resilience in the nursing workforce. Nurs Manage. 2020;27(3):1.
29. Labrague LJ, McEnroe‐Petitte DM, Leocadio MC, Van Bogaert P, Cummings GG. Stress and ways of coping among nurse managers: an integrative review. J Clin Nurs. 2018;27(7–8):1346–1359. doi:10.1111/jocn.14165
30. Samios C, Catania J, Newton K, Fulton T, Breadman A. Stress, savouring, and coping: the role of savouring in psychological adjustment following a stressful life event. Stress Health. 2020;36(2):119–130. doi:10.1002/smi.2914
31. Nowicki GJ, Ślusarska B, Tucholska K, Naylor K, Chrzan-Rodak A, Niedorys B. The severity of traumatic stress associated with COVID-19 pandemic, perception of support, sense of security, and sense of meaning in life among nurses: research protocol and preliminary results from Poland. Int J Environ Res Public Health. 2020;17(18):6491. doi:10.3390/ijerph17186491
32. Hammond RA, Axelrod R. The evolution of ethnocentrism. J Conflict Resol. 2006;50(6):926–936. doi:10.1177/0022002706293470
33. Riolo RL, Cohen MD, Axelrod R. Evolution of cooperation without reciprocity. Nature. 2001;414(6862):441–443. doi:10.1038/35106555
34. Ip M, Lui SL, Poon VK, Lung I, Burd A. Antimicrobial activities of silver dressings: an in vitro comparison. J Med Microbiol. 2006;55(1):59–63. doi:10.1099/jmm.0.46124-0
35. Kurzban R, Leary MR. Evolutionary origins of stigmatization: the functions of social exclusion. Psychol Bull. 2001;127(2):187. doi:10.1037/0033-2909.127.2.187
36. Cocking C, Vestergren S, Ntontis E, Luzynska K. ‘All together now’: facilitators and barriers to mutual aid during the first UK COVID-19 lockdown, and implications for community resilience. PsyArXiv. 2022;2022:1.
37. Burrows B, Abellera C, Markowitz EM. COVID‐19 and climate change: the social‐psychological roots of conflict and conflict interventions during global crises. Wiley Interdiscip Rev. 2023;2023:e837.
38. Fernandes-Jesus M, Mao G, Ntontis E, et al. More than a COVID-19 response: sustaining mutual aid groups during and beyond the pandemic. Front Psychol. 2021;12:716202. doi:10.3389/fpsyg.2021.716202
39. Canfield J. Secondary traumatization, burnout, and vicarious traumatization: a review of the literature as it relates to therapists who treat trauma. Smith Coll Stud Soc Work. 2005;75(2):81–101. doi:10.1300/J497v75n02_06
40. Sim A, Bowes L, Gardner F. Modeling the effects of war exposure and daily stressors on maternal mental health, parenting, and child psychosocial adjustment: a cross-sectional study with Syrian refugees in Lebanon. Glob Ment Health. 2018;5:e40. doi:10.1017/gmh.2018.33
41. Hornstein EA, Eisenberger NI, Brown KW. Unpacking the buffering effect of social support figures: social support attenuates fear acquisition. PLoS One. 2017;12(5):e0175891. doi:10.1371/journal.pone.0175891
42. Fenlason KJ, Beehr TA. Social support and occupational stress: effects of talking to others. J Organ Behav. 1994;15(2):157–175. doi:10.1002/job.4030150205
43. Gülaçtı F. The effect of perceived social support on subjective well-being. Procedia Soc Behav Sci. 2010;2(2):3844–3849. doi:10.1016/j.sbspro.2010.03.602
44. Hupcey JE. Social support: assessing conceptual coherence. Qual Health Res. 1998;8(3):304–318. doi:10.1177/104973239800800302
45. Poudel A, Gurung B, Khanal GP. Perceived social support and psychological wellbeing among Nepalese adolescents: the mediating role of self-esteem. BMC Psychol. 2020;8(1):1–8. doi:10.1186/s40359-020-00409-1
46. Abbas J, Mubeen R, Iorember PT, Raza S, Mamirkulova G. Exploring the impact of COVID-19 on tourism: transformational potential and implications for a sustainable recovery of the travel and leisure industry. Curr Res Behav Sci. 2021;2:100033. doi:10.1016/j.crbeha.2021.100033
47. Chen X, Zou Y, Gao H. Role of neighborhood social support in stress coping and psychological wellbeing during the COVID-19 pandemic: evidence from Hubei, China. Health Place. 2021;69:102532. doi:10.1016/j.healthplace.2021.102532
48. Cook JD, Bickman L. Social support and psychological symptomatology following a natural disaster. J Trauma Stress. 1990;3(4):541–556. doi:10.1002/jts.2490030406
49. Chan SM, Wong H, Chen Y, Tang MY. Determinants of depression and anxiety in homeless people: a population survey of homeless people in Hong Kong. Int J Soc Psychiatry. 2023;2023:00207640231152208.
50. Bromet EJ, Atwoli L, Kawakami N, et al. Post-traumatic stress disorder associated with natural and human-made disasters in the World Mental Health Surveys. Psychol Med. 2017;47(2):227–241. doi:10.1017/S0033291716002026
51. Ashton WA, Fuehrer A. Effects of gender and gender role identification of participant and type of social support resource on support seeking. Sex Roles. 1993;28(7–8):461–476. doi:10.1007/BF00289608
52. Aldwin CM, Revenson TA. Does coping help? A reexamination of the relation between coping and mental health. J Pers Soc Psychol. 1987;53(2):337. doi:10.1037/0022-3514.53.2.337
53. Rickwood DJ. The effectiveness of seeking help for coping with personal problems in late adolescence. J Youth Adolesc. 1995;24(6):685–703. doi:10.1007/BF01536951
54. Cauce AM, Hannan K, Sargeant M. Life stress, social support, and locus of control during early adolescence: interactive effects. Am J Community Psychol. 1992;20(6):787–798. doi:10.1007/BF01312608
55. Rickwood D, Thomas K. Conceptual measurement framework for help-seeking for mental health problems. Psychol Res Behav Manag. 2012;173–183. doi:10.2147/PRBM.S38707
56. Vance A, Siponen M, Pahnila S. Motivating IS security compliance: insights from habit and protection motivation theory. Inf Manag. 2012;49(3–4):190–198. doi:10.1016/j.im.2012.04.002
57. Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–48. doi:10.1016/j.bbi.2020.04.028
58. Thoits PA. Social support as coping assistance. J Consult Clin Psychol. 1986;54(4):416. doi:10.1037/0022-006X.54.4.416
59. Cobb S. Social support as a moderator of life stress. Psychosom Med. 1976;38(5):300–314. doi:10.1097/00006842-197609000-00003
60. Heaney CA, Israel BA. Social networks and social support. Health Behavi Health Educ. 2008;4:189–210.
61. House JS. Social support and social structure. In: Sociological Forum. Vol. 2. Dordrecht: Kluwer Academic Publishers; 1987:135–146.
62. Li Y, Wei F, Ren S, Di Y. Locus of control, psychological empowerment and intrinsic motivation relation to performance. J Manag Psychol. 2015;30(4):422–438. doi:10.1108/JMP-10-2012-0318
63. McDowell TL, Serovich JM. The effect of perceived and actual social support on the mental health of HIV-positive persons. AIDS Care. 2007;19(10):1223–1229. doi:10.1080/09540120701402830
64. Oh HJ, Lauckner C, Boehmer J, Fewins-Bliss R, Li K. Facebooking for health: an examination into the solicitation and effects of health-related social support on social networking sites. Comput Human Behav. 2013;29(5):2072–2080. doi:10.1016/j.chb.2013.04.017
65. Chi X, Chen S, Chen Y, et al. Psychometric evaluation of the fear of COVID-19 scale among Chinese population. Int J Ment Health Addict. 2021;2021:1–6.CSI.
66. Amirkhan JH. A factor analytically derived measure of coping: the coping strategy indicator. J Pers Soc Psychol. 1990;59(5):1066. doi:10.1037/0022-3514.59.5.1066
67. Lo CF. Stress and coping strategies among University freshmen in Hong Kong: validation of the coping strategy indicator. Psychology. 2017;8(08):1254. doi:10.4236/psych.2017.88081
68. Hou ZJ, Zhou X, Chen JL, Zhu L, Ni J, Chen SF. The influencing factors of PTSD and PTG among teachers after Wenchuan earthquake: perspectives from before, during and after disaster. Psychol Dev Educ. 2014;30(1):82–89.
69. Sommerlad A, Marston L, Huntley J, et al. Social relationships and depression during the COVID-19 lockdown: longitudinal analysis of the COVID-19 Social Study. Psychol Med. 2022;52(15):3381–3390. doi:10.1017/S0033291721000039
70. Kliem S, Mößle T, Rehbein F, Hellmann DF, Zenger M, Brähler E. A brief form of the Perceived Social Support Questionnaire (F-SozU) was developed, validated, and standardized. J Clin Epidemiol. 2015;68(5):551–562. doi:10.1016/j.jclinepi.2014.11.003
71. Chen Y, Liu Y, Zhang Y, Li Z, Zhou T. The effect of fear of the COVID-19 on depression among Chinese outbound students studying online in China amid the COVID-19 pandemic period: the Role of resilience and social support. Front Psychol. 2021;12:750011. doi:10.3389/fpsyg.2021.750011
72. Hayes AF. PROCESS: a versatile computational tool for observed variable mediation, moderation, and conditional process modeling; 2012
73. Lakey B, Cohen S. Social support and theory. In: Social Support Measurement and Intervention: A Guide for Health and Social Scientists. Oxford University Press; 2000:29–49.
74. Al-Dmour H, Masa’deh RE, Salman A, Abuhashesh M, Al-Dmour R. Influence of social media platforms on public health protection against the COVID-19 pandemic via the mediating effects of public health awareness and behavioral changes: integrated model. J Med Internet Res. 2020;22(8):e19996. doi:10.2196/19996
75. Hsieh YH, Lee JY, Chang HL. SARS epidemiology modeling. Emerg Infect Dis. 2004;10(6):1165–1167. doi:10.3201/eid1006.031023
76. Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1). doi:10.1192/j.eurpsy.2020.35
77. Labrague LJ, Santos JAA. COVID‐19 anxiety among front‐line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653–1661. doi:10.1111/jonm.13121
78. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288(0165–1781):112954. doi:10.1016/j.psychres.2020.112954
79. Torous J, Jän Myrick K, Rauseo-Ricupero N, Firth J. Digital mental health and COVID-19: using technology today to accelerate the curve on access and quality tomorrow. JMIR Mental Health. 2020;7(3):e18848. doi:10.2196/18848
80. Martínez-Lorca M, Martínez-Lorca A, Criado-álvarez JJ, Armesilla MD, Latorre JM. The fear of COVID-19 scale: validation in Spanish university students. Psychiatry Res. 2020;293:113350. doi:10.1016/j.psychres.2020.113350
81. Goddard RD, Hoy WK, Hoy AW. Collective efficacy beliefs: theoretical developments, empirical evidence, and future directions. Educ Res. 2004;33(3):3–13. doi:10.3102/0013189X033003003
82. Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS One. 2021;16(3):e0247679. doi:10.1371/journal.pone.0247679
83. Yenen ET, Carkit E. Fear of COVID-19 and general self-efficacy among Turkish teachers: mediating role of perceived social support. Curr Psychol. 2023;42(3):2529–2537. doi:10.1007/s12144-021-02306-1
84. Muflih S, Abuhammad S, Karasneh R, Al-Azzam S, Alzoubi KH, Muflih M. Online education for undergraduate health professional education during the COVID-19 pandemic: attitudes, barriers, and ethical issues. Res Sq. 2020. doi:10.21203/rs.3.rs-42336/v1
85. Pakpour AH, Griffiths MD, Chang KC, Chen YP, Kuo YJ, Lin CY. Assessing the fear of COVID-19 among different populations: a response to Ransing et al. Brain Behav Immun. 2020;89:524–525. doi:10.1016/j.bbi.2020.06.006
86. Hyde LW, Gorka A, Manuck SB, Hariri AR. Perceived social support moderates the link between threat-related amygdala reactivity and trait anxiety. Neuropsychologia. 2011;49(4):651–656. doi:10.1016/j.neuropsychologia.2010.08.025
87. Islam AN, Mäntymäki M, Laato S, Turel O. Adverse consequences of emotional support seeking through social network sites in coping with stress from a global pandemic. Int J Inf Manage. 2022;62:102431. doi:10.1016/j.ijinfomgt.2021.102431
88. Williams SL, Mickelson KD. A paradox of support seeking and rejection among the stigmatized. Pers Relatsh. 2008;15(4):493–509. doi:10.1111/j.1475-6811.2008.00212.x
89. Jia Z, Xu S, Zhang Z, et al. Association between mental health and community support in lockdown communities during the COVID-19 pandemic: evidence from rural China. J Rural Stud. 2021;82:87–97. doi:10.1016/j.jrurstud.2021.01.015
90. Baker F. The interface between professional and natural support systems. Clin Soc Work J. 1977;5(2):139–148. doi:10.1007/BF02144239
91. Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019‐nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74(4):281. doi:10.1111/pcn.12988
92. Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2021;19:1875–1888. doi:10.1007/s11469-020-00281-5
93. Kaushal A, Mandal A, Khanna D, Acharjee A. Analysis of the opinions of individuals on the COVID-19 vaccination on social media. Digit Health. 2023;9:20552076231186246. doi:10.1177/20552076231186246
94. Matus K, Sharif N, Li A, Cai Z, Lee WH, Song M. From SARS to COVID-19: the role of experience and experts in Hong Kong’s initial policy response to an emerging pandemic. Humanit Soc sci. 2023;10(1):1–6. doi:10.1057/s41599-022-01467-z
95. Zhang W, Huang L, Xu F, Liu H, Wang G. Impact of campus living conditions on Chinese medical school students’ mental health during the COVID-19 campus lockdown: the chain mediating role of cognitive reappraisal and expression suppression. Front Psychiatry. 2023;14:1171425. doi:10.3389/fpsyt.2023.1171425
96. Rajulton F. The fundamentals of longitudinal research: an overview. Can Stud Popul. 2001;28(2):169–185. doi:10.25336/P6W897
97. Hackshaw A. Small studies: strengths and limitations. Eur Respir J. 2008;32(5):1141–1143. doi:10.1183/09031936.00136408
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
