Back to Journals » Clinical Ophthalmology » Volume 17
Impact of Donor, Recipient, and Graft Characteristics on Corneal Transplantation Outcomes
Authors Shah PP , Hasan A, Winokur J, Braunstein R, Ritterband DC, Seedor JA, Cheela I
Received 2 December 2022
Accepted for publication 9 January 2023
Published 23 February 2023 Volume 2023:17 Pages 633—640
DOI https://doi.org/10.2147/OPTH.S399847
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Paras P Shah,1 Aisha Hasan,2 Jules Winokur,1,2 Richard Braunstein,1,2 David C Ritterband,1,2 John A Seedor,1,2 Isha Cheela1,2
1Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, USA; 2Department of Ophthalmology, Northwell Health/Manhattan Eye, Ear & Throat Hospital, New York, NY, USA
Correspondence: Paras P Shah, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, 500 Hofstra Blvd, Hempstead, NY, 11549, USA, Email [email protected]
Purpose: Although several donor, recipient, and graft characteristics have been studied in relation to corneal transplantation outcomes, no study to our knowledge has assessed the impact of donor cooling times on postoperative outcomes longitudinally. With only one corneal graft available for every 70 needed worldwide, this study seeks to identify any factors that could alleviate this shortage.
Methods: Patients undergoing corneal transplantation at the Manhattan Eye, Ear & Throat Hospital over a 2-year period were retrospectively studied. Study metrics included age, diabetic history, hypertensive history, endothelial cell density, death-to-preservation time (DTP), death-to-cooling time (DTC), and time-in-preservation (TIP). Postoperative transplantation outcomes, including best corrected visual acuity (BCVA) at 6- and 12-month follow-up visits, need for re-bubbling, and need for re-grafting, were assessed. Unadjusted univariate and adjusted multivariate binary logistic regressions were performed to determine the association of cooling and preservation parameters with corneal transplantation outcomes.
Results: Among 111 transplants, our adjusted model found that DTC ≥ 4 hours was associated with significantly worse BCVA, but only at 6-month postoperative follow-up (odds ratio [OR]: 0.234; 95% confidence interval [CI]: 0.073– 0.747; p = 0.014). By 12-month follow-up, DTC > 4 hours was no longer associated with BCVA in a statistically significant manner (OR: 0.472; 95% CI: 0.135– 1.653; p = 0.240). A similar trend was found at a DTC cutoff of ≥ 3 hours. None of the other studied parameters, including DTP, TIP, donor age, or medical history were significantly correlated with transplantation outcomes.
Conclusion: Longer DTC or DTP did not have a statistically significant effect on corneal graft outcomes after one year, though short-term outcomes were improved in donor tissues with DTC below four hours. None of the other studied variables correlated with transplantation outcomes. Given the global shortage of corneal tissue, these findings should be considered when determining suitability for transplantation.
Keywords: corneal transplant, donor, recipient, outcome, cooling, refrigeration
Introduction
Corneal donor characteristics and preservation methods have been extensively studied to assess outcomes in patients. Currently, three forms of preservation of corneal grafts are used – organ culture solution (28–37°C), hypothermia (2–8°C), and cryopreservation (4°C).1 Of these, hypothermia is most frequently used in the United States, while European eye banks more frequently use organ culture. Organ culture, in which tissue is incubated in a medium supplemented with fetal calf serum, antibiotics, and antimycotics, has been associated with longer viable storage times than hypothermia.1 However, surgeons and eye banks have become judicious with the number of days a corneal graft can be used after preservation, with many preferring not to exceed seven days when stored via hypothermia.2 Despite this, many recent studies have found few significant associations between the preservation characteristics of the graft and corneal transplantation outcomes.3–7 One of these reports, which analyzed 857 DMEK transplants, further suggested no significant relationship between donor age, diabetic history, or endothelial cell density (ECD) with regard to rebubble rates, calling in to question common surgeon preferences for younger, nondiabetic grafts.4
The premise behind hypothermic storage of tissue stems from the concept that the rate constant of cellular reactions is exponentially proportional to temperature.8 Therefore, at a reduced temperature, cells decrease their metabolism and oxygen consumption, preventing mitochondrial stress and hypoxia-induced apoptosis. Most corneal transplants depend largely on preservation of a viable endothelium.2 Along with hypothermic preservation, media such as Optisol-GS (Bausch and Lomb) have been found to lengthen endothelial cell viability to up to two weeks.9 This solution contains nutrients including ATP precursors, vitamins, dextran, and chondroitin sulfate, which further support the endothelial cells during preservation.
Cooling during the death to preservation window has also been explored as a possible factor affecting corneal graft viability. Arguably, donor refrigeration is crucial to prevent early endothelial damage by decelerating cellular metabolism and ensuing cell death in a state of cooling prior to preservation. One analysis of nearly 43,000 donor eyes found that refrigeration during this interval was related to significantly higher odds of suitability for transplantation, though the amount of time in refrigeration was not investigated.10 Others found that donor refrigeration had a beneficial effect on ECD only when the death to preservation time exceeded 12 hours.11
The purpose of this study is to further examine the effect of donor, recipient, and graft characteristics, namely donor age, diabetic and hypertensive history, recipient sex, history of prior transplant, endothelial cell density (ECD), death-to-cooling time (DTC), death-to-preservation time (DTP), and time-in-preservation (TIP), on corneal transplantation outcomes, including rebubble rates, regraft rates, and best corrected visual acuity (BCVA) improvement.
Materials and Methods
A retrospective analysis of patients who underwent corneal transplantation at the Manhattan Eye, Ear & Throat Hospital between September 2018 and June 2020 was performed. All transplants were performed by one of three surgeons with similar years of experience. Three types of transplants, Descemet stripping automated endothelial keratoplasty (DSAEK), penetrating keratoplasty (PKP), and Descemet membrane endothelial keratoplasty (DMEK), were included in the study, while patients who received Boston keratoprosthesis (KPro), anterior lamellar keratoplasty, or deep anterior lamellar keratoplasty (DALK) were excluded. The patient’s sex, preoperative best corrected visual acuity (BCVA) in the affected eye, date of surgery, and whether the patient had received a prior transplant were also noted.
Each patient’s donor report was obtained from the respective eye bank and data was recorded about each donor graft, including date and time of death, ECD, donor age, and donor history of diabetes mellitus or hypertension. Death to cooling (DTC) and death to preservation (DTP) times, as well as time in preservation (TIP), were recorded.
Postoperative transplantation outcomes that were assessed included best spectacle corrected visual acuity (BSCVA) at 6- and 12-month follow-up visits, as well as need for rebubbling or regrafting. BSCVA was defined as Snellen visual acuity measured in length adjusted lanes. In cases involving DSAEK and DMEK, the determination to rebubble was made by the treating physician and was largely based on the extent of a graft detachment and duration of time since surgery. In general, a decision was made that the patient would receive an eventual regraft if the graft failed to clear after approximately one month of intensive topical steroid therapy and/or rebubbling. In addition, a patient was considered to have BSCVA improvement if they improved by >1 line from the preoperative to postoperative interval. In patients with very poor vision, any improvement during this period was sufficient to meet criteria (ie: hand motion to counting fingers).
Graft success was compared to graft failure with regard to the characteristics of the donor and recipient (Tables 1–3). Graft tissue was further characterized based on ECD, DTC, DTP, and TIP. The two groups (ie, outcome achieved or not) were compared using chi-square tests for categorical characteristics and independent samples t-tests for continuous variables. Binary logistic regression was performed to determine the association of cooling and preservation parameters with corneal transplantation outcomes. Both crude and adjusted multivariate models were reported. Additional models were run with DTC, a binary variable, with DTC cutoffs of > 3 hours and > 4 hours. All models were adjusted for donor age, ECD, history of DM, history of HTN, and recipient sex and history of prior transplantation. Covariates were chosen based on literature review and clinical knowledge. Given that all outcomes were binary, the results were expressed as odds ratios, with accompanying 95% confidence intervals and P-values. Statistical Package for the Social Sciences (SPSS), Version 26 (IBM Inc.), was utilized and a P-value ≤0.05 was considered statistically significant for all analyses. The Institutional Review Board (IRB) of Northwell Health reviewed and approved the study protocol. The study complies with the Declaration of Helsinki. All corneas were donated voluntarily with written informed consent, and this was conducted in accordance with the Declaration of Istanbul.
Results
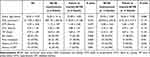
One hundred and twenty-six patients were considered for inclusion in this study, of which 15 patients were excluded due to either lack of data (ie, preservation time could not be assessed) or unsuitable surgery type (ie, KPro). The final analysis included 111 patients (61% male), whose full transplantation characteristics are described in Table 1. Reported with one standard deviation, the average ECD given on the donor reports was 3114 ± 303 cells/mm,2 while the average DTC, DTP, and TIP were 3.43 ± 1.96 hours, 10.75 ± 4.04 hours, and 4.50 ± 1.68 days, respectively. Furthermore, the average donor was 52.05 ± 14.07 years old, with a 45% prevalence of hypertension and 27% diabetes mellitus. The percentage of patients who underwent DSAEK, PK, and DMEK, was 62%, 30%, and 8%, respectively.
A significant difference was found between the DTC of the donors for recipients who achieved BCVA improvement at 6-month follow-up versus those who did not (3.00 hours versus 3.88 hours, respectively, p = 0.017; Table 1). A comparison of other donor, recipient, and graft characteristics did not reveal any significant differences. Notably, a difference between the DTC times of the donors for recipients with or without BCVA improvement was still noted at 12-month follow-up, though it was no longer statistically significant (3.25 hours versus 3.79 hours, respectively; p = 0.119). Similarly, the remaining donor, recipient, and graft characteristics remained statistically insignificant at the 12-month follow-up.
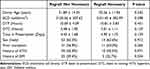
Of all the factors studied, none were statistically significant to explain differences in need for rebubble in DSAEK or DMEK patients (Table 2). DTC was most closely related to the need for rebubble, though significance was not achieved (3.24 hours versus 3.72 hours, respectively; p = 0.215). A similar difference was also seen with longer DTP (10.79 hours versus 11.55 hours, p = 0.290). Likewise, need to regraft was not statistically significant with any of the studied parameters (Table 3). It has been reported that patients with prior failed transplants are at higher risk of requiring regrafting with subsequent corneal transplants.12,13 Although not statistically significant, our findings are in line with this finding; patients for whom a regraft was necessary were more likely to have already had a history of prior transplant when compared to those patients who did not need a regraft (50% versus 36.9%, respectively; p = 0.264). Time in preservation and DTC seemed to be most related to the need to regraft, though neither achieved statistical significance.
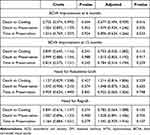
Binary logistic regression, adjusted for donor age, ECD, history of DM, history of HTN, and recipient sex and history of prior transplantation revealed that an increased DTC time of a corneal graft was associated with significantly lower odds of BCVA improvement at 6-month postoperative follow-up (OR: 0.677; 95% CI: 0.494–0.929; p = 0.016; Table 4). Notably, this significance is lost by the 12-month postoperative follow-up (OR: 0.753; 95% CI: 0.525–1.082; p = 0.110). The adjusted multivariate model largely corroborates the crude, unadjusted model, which similarly found that a longer DTC of a corneal graft is associated with significantly worse 6-month BCVA (OR: 0.755; 95% CI: 0.574–0.993; p = 0.044). The adjusted and crude models did not detect any significant associations between cooling and preservation characteristics, and the need for a rebubbled graft or complete regraft.
Furthermore, our adjusted multivariate model found that treating DTC as a binary variable with specific cutoffs of 3 hours as well as 4 hours yielded similar results to when DTC was a linear variable. A DTC time > 4 hours was associated with significantly worse BCVA, but only at 6-month postoperative follow-up (OR: 0.234; 95% CI: 0.073–0.747; p = 0.014; Table 5). By 12-month follow-up, DTC > 4 hours was no longer significantly associated with BCVA (OR: 0.472; 95% CI: 0.135–1.653; p = 0.240). A similar trend was found at a DTC cutoff of 3 hours (6 months: OR 0.282, 95% CI 0.103–0.773, p = 0.014; 12 months: OR 0.414, 95% CI 0.127–1.356, p = 0.145).
Discussion
Our study set out to re-evaluate previously studied variables with regard to donor tissue, as well as to look at the impact of cooling characteristics on graft outcomes over time. Numerous studies have looked at the importance of factors including ECD, corneal thickness, DTP time, and donor age, among others, to predict graft survival, and many have shown little association of these criteria with graft survival.3–7 Munir et al found that the presence of cooling post-mortem showed a statistically significant improvement in the suitability of donor tissue for implantation per eye bank criteria but did not find a significant difference on ECD.10 However, their study did not assess clinical outcomes after the donor tissue had been transplanted, and cooling was treated as a binary variable irrespective of the amount of time cooled. Our study further examined the interval from DTC as a binary variable at specific cutoffs of three hours and four hours, and we found that in either case, DTC beyond these cutoffs was associated with worse BCVA at 6-month follow-up but not at 12-month follow-up. We also ran additional models with DTC as a continuous variable, which is a more powerful analysis, which corroborated our finding that longer DTC times were not associated with BCVA at 12-months. Importantly, significance was retained in both univariate unadjusted models, and multivariate adjusted models, further indicating consistency of the data. It should be noted that the univariate models in Tables 1–3 are included for descriptive purposes and to identify potential biases in the dataset only, while the adjusted multivariate models in Tables 4–5 adjust for confounding variables and should be used for final interpretation.
The postulated decrease in the rate constant of cellular reactions that is theorized to occur with reduction of temperature may lead to better corneal donor preservation.8 Even a one-hour delay in cooling results in lower glucose levels in the stroma and aqueous, harming endothelial integrity.14,15 For corneal transplant surgery, the viability of the endothelium is largely predictive of successful transplants and some studies have assessed whether hypothermia can act to preserve the endothelium, with many either finding no correlation or a correlation only with a longer DTP time (>12hr).11 Other studies have found that the DTP interval has no influence on endothelial cell loss, with exceptions only for certain situations such as patients with keratoconus.16–18 These findings have been replicated in a study of split corneal transplantation.19 By extension, rapid postmortem donor refrigeration may be the more important factor in preventing early endothelial damage, via the mechanism described earlier, because cellular metabolism and ensuing cell death has already been somewhat decelerated in a state of cooling prior to preservation. This could explain why extended DTP times have not previously been found to affect outcomes, whereas DTC times have been found to affect outcomes in cases of prolonged preservation. One study suggests a maximum death-to-enucleation of 24 hours only in circumstances where the donor body has been refrigerated at 2–8°C within 6 hours of death, highlighting the importance of rapid cooling.20 In contrast, European studies which utilize organ culture have demonstrated that DTP times of up to 72 hours have no influence on the quality of transplanted corneas or transplantation outcomes, irrespective of DTC.21 The influence of DTC times may be impacted by the local climate and environmental factors and could therefore vary by region.
A statistically significant difference was seen in the DTC time in those who had a BCVA improvement at 6 months versus those who did not. This indicates that there may be a benefit in early graft outcomes related to cooling times. A hypothesis for this finding is that it is secondary to the previously mentioned concept of rate constant and the exponential impact of temperature on cellular reactions. Therefore, in donor corneas that were cooled more quickly, this allowed for improved endothelial integrity, which is critical to successful grafting. This difference was not replicated with any other variable such as DTP, ECD, or donor age to indicate a confounding result. This statistical significance was lost in those who had BCVA improvement at 12 months. These findings may suggest that there is little evidence that long-term graft survival is affected by comparatively longer DTC or DTP times. The acceptance of tissues with longer cooling times may lead to more tissue utilization, helping to overcome tissue shortages; one report estimates that only 1 cornea is available for every 70 needed worldwide.22 While many surgeons make every effort to use tissues with expedited procurement times, these factors seem to have little effect on transplantation outcomes. We have found that the outcomes from donors with extended cooling/preservation times may be initially worse but are likely to improve over one year to the point at which there is little to no difference in the outcome. Corneal blindness is a leading contributor to reversible blindness worldwide and an increase in the supply of viable corneal grafts could reduce this burden.23
One possible limitation of this study arises from the fact that rehabilitation times from PK may vary from that of DMEK and DSAEK. Our rationale to include PK with DMEK and DSAEK was because of our hypothesis that endothelial survival is crucial during the cooling window. To ensure that the inclusion of PK did not introduce a bias into our dataset, we ran one additional model excluding PK, using the same covariates, and discovered that with longer DTC times, BCVA continued to worsen only at 6-months postoperative follow-up (OR: 0.616, 95% CI: 0.422–0.899, p = 0.012) and remained unchanged by 12-months postoperative follow-up (OR: 0.731, 95% CI: 0.486–1.098, p = 0.131). While this does point to the consistency of our data, this limitation should still be considered. Additional limitations of this study include a small sample size and single center of study especially when compared to some of the larger corneal donor studies. There may also be a selection bias in the tissue selection criteria that are used by the surgeons in this study, limiting the variability of the criteria studied. The study participants were also not masked during the study leading to another implicit bias. Moreover, there is a possibility that recipient age and indication for transplantation may influence graft outcomes and these variables should be included in future analyses. Another limitation of this study is the absence of postoperative ECDs immediately postoperatively or even at other postoperative visits, which limits the assessment of any loss of endothelial cells during or following the procedure.
Overall, our study found the association of cooling to be linked to early visual improvement, and while that trend continued, it was not statistically significant one year post surgery. Further studies could assess outcomes at longer intervals than one year and in a larger cohort. Another factor that would be useful to assess with an increase in data could be whether our findings can be replicated with DTC times > 5 hours and beyond, which we could not model due to sample limitations. This could help determine whether a certain threshold of cooling exists beyond which even long-term outcomes suffer. Additionally, ECD post transplantation could also be assessed in future studies. This could give more insight into endothelial cell loss during the various surgical techniques and whether cooling plays a role in endothelial cell preservation. We did not find other tissue factors to be statistically significant with regard to graft survival within the range of tissues that were transplanted. This may lead to greater acceptance by transplanting surgeons of tissues that have factors outside of their preferred use and lead to greater usage of donor corneas.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Funding
No funding was received for this work.
Disclosure
None of the authors declare any conflicts of interest or proprietary interest in relation to the submitted work.
References
1. Xi L, Kozlov AV. Research progress of the application of hypothermia in the eye. Oxid Med Cell Longev. 2020;2020:3897168. doi:10.1155/2020/3897168
2. Armitage WJ. Preservation of human cornea. Transfus Med Hemother. 2011;38(2):143–147. doi:10.1159/000326632
3. Madzak A, Hjortdal J. Outcome of human donor corneas stored for more than 4 weeks. Cornea. 2018;37(10):1232–1236. doi:10.1097/ico.0000000000001676
4. Straiko MD, Bauer AJ, Straiko MMW, et al. Donor DMEK tissue characteristics: association with rebubble rate and 6-month endothelial cell loss. Cornea. 2020;39(10):1267–1273. doi:10.1097/ico.0000000000002398
5. Maguire MG, Stark WJ, Gottsch JD, et al. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative Corneal Transplantation Studies Research Group. Ophthalmology. 1994;101(9):1536–1547. doi:10.1016/s0161-6420(94)31138-9
6. Lass JH, Benetz BA, Verdier DD, et al. Corneal endothelial cell loss 3 years after successful descemet stripping automated endothelial keratoplasty in the cornea preservation time study: a randomized clinical trial. JAMA Ophthalmol. 2017;135(12):1394–1400. doi:10.1001/jamaophthalmol.2017.4970
7. Gal RL, Dontchev M, Beck RW, et al. The effect of donor age on corneal transplantation outcome results of the cornea donor study. Ophthalmology. 2008;115(4):620–626.e6. doi:10.1016/j.ophtha.2008.01.003
8. Liavitskaya T, Vyazovkin S. All you need to know about the kinetics of thermally stimulated reactions occurring on cooling. Molecules. 2019;24(10):1918. doi:10.3390/molecules24101918
9. Lindstrom RL, Kaufman HE, Skelnik DL, et al. Optisol corneal storage medium. Am J Ophthalmol. 1992;114(3):345–356. doi:10.1016/s0002-9394(14)71803-3
10. Munir WM, Brown CH, Munir SZ, Hoover CK. Effect of body refrigeration time on cornea donor tissue. Cornea. 2021;40(12):1590–1593. doi:10.1097/ico.0000000000002665
11. Patel D, Tandon R, Ganger A, Vij A, Lalwani S, Kumar A. Study of death to preservation time and its impact on utilisation of donor corneas. Trop Doct. 2017;47(4):365–370. doi:10.1177/0049475517713406
12. Son HS, Lum F, Li C, Schein O, Pramanik S, Srikumaran D. Risk factors for repeat keratoplasty after endothelial keratoplasty-an iris registry analysis. Am J Ophthalmol. 2022;242:77–87. doi:10.1016/j.ajo.2022.05.026
13. Muijzer MB, Hoven CMW, Frank LE, Vink G, Wisse RPL. A machine learning approach to explore predictors of graft detachment following posterior lamellar keratoplasty: a nationwide registry study. Sci Rep. 2022;12(1):17705. doi:10.1038/s41598-022-22223-y
14. Thoft RA, Friend J, Freedman H, Dohlman CH. Corneal epithelial preservation. Arch Ophthalmol. 1975;93(5):357–361. doi:10.1001/archopht.1975.01010020369011
15. Sperling S. A simple apparatus for controlled rate corneal freezing. Acta Ophthalmol. 1977;55(1):1–8. doi:10.1111/j.1755-3768.1977.tb06090.x
16. Parekh M, Salvalaio G, Ferrari S, et al. Effect of postmortem interval on the graft endothelium during preservation and after transplantation for keratoconus. Cornea. 2013;32(6):842–846. doi:10.1097/ICO.0b013e318283c873
17. Mohamed A, Chaurasia S, Garg P. Outcome of transplanted donor corneas with more than 6 h of death-to-preservation time. Indian J Ophthalmol. 2016;64(9):635–638. doi:10.4103/0301-4738.194338
18. Sun MJ, Duong AT, Tran KD, Straiko MMW, Stoeger CG, Sales CS. Primary graft failure, infection, and endothelial cell density in corneal transplants with increased death-to-preservation time. Cornea. 2021;40(11):1462–1465. doi:10.1097/ico.0000000000002697
19. Kandemir B, Tutaş Günaydın N, Göktaş E, Tanyıldız B. Does storage time affect the outcomes of split corneal transplantation to reduce corneal donor shortage? A retrospective study. Inquiry. 2021;58:469580211045846. doi:10.1177/00469580211045846
20. Sampaio TL, Rodrigues IP, Cresta MBL, et al. Factors influencing endothelial cell density of corneas for transplantation. Cell Tissue Bank. 2021;22(2):263–275. doi:10.1007/s10561-020-09875-8
21. Hofmann N, Wittmershaus I, Salz AK, Börgel M. Cornea procurement and processing up to 72 hours: no risk for cornea transplant quality. Transfus Med Hemother. 2021;48(1):3–11. doi:10.1159/000510588
22. Gain P, Jullienne R, He Z, et al. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol. 2016;134(2):167–173. doi:10.1001/jamaophthalmol.2015.4776
23. Singh R, Gupta N, Vanathi M, Tandon R. Corneal transplantation in the modern era. Indian J Med Res. 2019;150(1):7–22. doi:10.4103/ijmr.IJMR_141_19
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.