Back to Journals » Risk Management and Healthcare Policy » Volume 15
Impact of COVID-19 on Health Seeking Behavior of Patients with Chronic Disease at Public Hospitals in Jimma Zone, South West Ethiopia
Authors Awel S , Ahmed I , Tilahun D , Tegenu K
Received 31 March 2022
Accepted for publication 23 July 2022
Published 1 August 2022 Volume 2022:15 Pages 1491—1500
DOI https://doi.org/10.2147/RMHP.S367730
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Samira Awel, Ismael Ahmed, Desalew Tilahun, Kenenisa Tegenu
School of Nursing, College of Health Science, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Samira Awel, School of Nursing, College of Health Science, Institute of Health, Jimma University, P.O. Box 378, Jimma, Ethiopia, Tel +251 921918489, Email [email protected]
Background: COVID-19 is a global pandemic with unprecedented medical, economic and social consequences affecting nations across the world. This epidemic arises while chronic diseases are continued to be a public health concern. Though evidence is generated on its impact on the health care system, little is known about the Impact of COVID − 19 on the care-seeking behavior of chronic patients.
Objective: To assess the Impact of COVID-19 on healthcare-seeking behavior of patients with chronic diseases attending follow-up at public hospitals in Jimma zone, South West Ethiopia.
Methods: Facility-based cross-sectional study design was employed. The sample was calculated using the single population proportion formula. Hospitals were selected by using simple random sampling. Then, the final calculated sample size for the study was proportionally allocated to each selected hospital. Data were collected from 400 participants through face-to-face interviews and card reviews. Data were entered into Epi-Data version 3.1 and then exported to SPSS version 23 for analysis. Binary and multivariable logistic regression analyses with 95% CI for odds ratio (OR) were used to identify significant factors.
Results: Of the total respondents 156 (39.0%) of them had poor health-seeking behavior. Contact history with COVID − 19 patient (AOR = 2.8; 95% CI = 1.1– 7.0), perceived moderate depression (AOR = 2.3; 95% CI = 1.2– 4.2), perceived extreme depression (AOR = 4.3; 95% CI = 1.8– 10.5), shortage of medication (AOR = 2.4; 95% CI = 1.0– 6.2) increases the odds of poor health-seeking behavior. In addition, the odds of poor health-seeking in patients with no formal education were higher compared to patients with higher educational status (AOR = 2.7; 95% CI = 1.0– 9.0).
Conclusion: COVID − 19 outbreaks affected the health-seeking behavior of patients with chronic diseases. The impact was found to be more significant among patients who had a contact history with COVID − 19 patients. Moreover, perceived depression, shortage of medication, and low educational status were significant predictors of poor health-seeking behavior. Therefore, working on the barriers to the health-seeking behavior of chronic patients may reduce the effect of COVID-19.
Keywords: COVID-19, health-seeking behavior, chronic disease, Ethiopia
Introduction
Coronavirus disease-19 (COVID-19) is a global pandemic with unprecedented medical, economic and social consequences affecting nations across the world.1,2 In the past few years, the COVID-19 outbreak has largely changed the rhythm of human life and overwhelmed the healthcare systems of both developing and developed countries.3 The outbreak of the COVID-19 has caused enormous stress among the public in China initially and then after the whole world.4 Amidst to current pandemic, the WHO has issued several guidelines and also started online courses and training sessions to raise awareness and preparedness regarding the prevention and control of COVID-19.5
This epidemic arises while chronic diseases are continued to be a public health concern. According to the WHO report, non-communicable diseases cause 41 million deaths each year, which is equivalent to 71% of all deaths globally.6 Though chronic diseases are not curable, they are controllable. Pre-existing co-morbidities such as hypertension, diabetes, and cardiovascular disease are associated with greater severity and a higher fatality rate of COVID-19.7 Currently, most global healthcare resources are focused on COVID-19 which disrupts the continuum of care for patients with chronic diseases. A global survey shows that chronic disease is highly impacted by the reduction in healthcare resources due to COVID-19.8
Poor health care seeking among patients has been linked to worse health outcomes and may also lead to mortality.9
Several factors may influence the health care seeking of the population.10,23 A study conducted in Singapore shows that about 40% of respondents reported missing their healthcare appointment during the COVID-19 outbreak.1 The outbreak has the potential to indirectly impact people with pre-existing chronic medical conditions if they are not able to access routine health care for managing their chronic conditions.1,9 In addition, greater worry may influence their health-care-seeking behavior for chronic medical conditions which may result in morbidity and mortality.9,11,12,15
Evidence shows that the number of patients attending essential health care services declined during the COVID-19 in Ethiopia.9,24,25 The Government of Ethiopia has taken numerous significant actions including lockdown during an initial six-month-long State of Emergency to mitigate the pandemic’s overspread, which was implemented throughout the country.2,25
Unlike developed countries, patients with chronic diseases in developing countries including Ethiopia lack follow-up through phone (telemedicine) and home-setting care.10 As chronic diseases are one of the major causes of mortality and morbidity, controlling them needs good follow-up and health-seeking behavior among the nation. Even though COVID-19 has affected the health care system, little is known about the Impact of COVID-19 on care-seeking behavior among chronic patients in Ethiopia, especially in the study area. Therefore, this study aimed at assessing the impact of COVID-19 on health-seeking behavior among patients with chronic disease at Jimma zone public hospitals.
Methods
Description of Approaches/Methods
Study Area and Period
The study was conducted in public hospitals in Jimma zone, Oromia region state South West Ethiopia. Jimma zone is located 350 km away from Addis Ababa. The zone is divided into 18 districts and one town administration. There are eight hospitals (one referral and teaching hospital, one general hospital, and six primary hospitals), 115 health centers, and 520 health posts in the Jimma zone. The populations being served by the public health facilities are estimated to be more than 15 million annually including people from border zones and South Sudan, while the Jimma University Medical Center has a lion’s share. The study was conducted from April 1 to 30 2021 G.c.
Study Design
Facility-based cross-sectional study design was employed.
Source of Population
All patients in chronic follow-up at public hospitals in Jimma zone, South West Ethiopia, were considered.
Study Population
All patients in chronic follow-up at the selected public hospitals of Jimma zone during the study period.
Study Unit
All sampled patients attended a chronic follow-up unit at the selected public hospitals in Jimma zone during the study period.
Eligibility Criteria
Adult outpatients attending chronic follow-up at the selected public hospitals in Jimma zone during the study period and giving consent to participate were included. Severely sick patients, who cannot respond and were admitted to the ward since the COVID-19 pandemic, were excluded.
Sample Size Determination and Sampling Technique
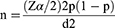
The sample size was determined by using the single population proportion formula by considering a 50%. The formula for calculating the sample size (n) is
where n = Minimum sample size
p = an estimate of the prevalence rate for the population
d = the margin of the sampling error
Zα/2 = standard normal variance (1.96) 2 is mostly 5%, ie, with 95% confidence level
n = 384
By adding a 10% non-response rate the final sample size is 422.
Sampling Procedures
There are eight public hospitals in the Jimma Zone, from eight hospitals four hospitals were selected by using simple random sampling. Then, the final calculated sample size for the study was proportionally allocated to each selected hospital. Individual study participants were selected using systematic random sampling techniques from the chronic follow-up registration book of each selected hospital by K-value (N/n=total population/total sample size). Proportional allocation for each selected hospital was done as the following accordingly (Table 1).
 |
Table 1 Proportional Allocation for Each Selected Hospital |
Data Collection Tools
Pre-tested, structured interviewer-administered questionnaires were used, which was adapted from different literature.3,7,8,13,17 The independent variables were as follows: Socio-demographic characteristics (residence, age, sex, ethnicity, educational status, and occupation), clinical and treatment-related characteristics (types of diagnosis, respiratory symptoms, travel history, contact history with a known COVID-19 case, source of medication, and presence of comorbid illness), and quality of life-related variables which includes mobility, self-care, usual activities, pain/discomfort, and perceived anxiety/depression.
The dependent variables were health care seeking behavior: participants were asked to claim a health facility in case of health problems, health care appointment, willing to spend time on health care, willing to spend money on health care, and take medications as prescribed by health care provider after the COVID −19 pandemic. To identify barriers, those participants who mentioned canceling their health care appointment were asked about the reason and the alternative measures they took for the missed follow-up.
Data Collection Procedure
Interviewer-administered structured questionnaires and card reviews were used to collect data. 14 BSc nurses and 4 MSc nurses were recruited as data collectors and supervisors, respectively. Data were collected through face-to-face interviews and card reviews.
Data Quality Control
Both data collectors and a supervisor were trained for three days on the objective of the study and techniques of data collection. A supervisor was checking the completeness and consistencies of the questionnaires. The principal investigator evaluated the data before the data analysis to verify the completeness of the collected data. A pretest was done on 5% of the sample size in Limmu hospital to ensure the internal consistency of the instrument.
Data Processing and Analysis
The data were entered and coded into the EpiData version 3.1 and then exported to SPSS version 23 for analysis. Descriptive statistics and logistic regression were computed. Variables with a p-value less than ≤0.25 were candidates for multivariate logistic regression. Binary logistic regression was done accordingly, and multivariable logistic regression analysis was adjusted for potential confounders. Educational status, self-care, income, activity, contact history with COVID-19 patients, mobility, pain, perceived depression, health care service since the outbreak and shortage of medication were variable candidates for multivariable logistic regression analysis. Multivariable logistic regression was done after identifying those candidate variables with a P-value of ≤0.25. Variables with a p-value <0.05 were declared statistically significant.
Operational Definition
In this study, the health-seeking behavior was determined based on the following five components: claiming to visit a health facility in case of health problems, do not miss/canceled a health-care appointment, willing to spend time on health care, willing to spend money on health care, and take medications as prescribed by health care provider after the COVID −19 pandemic.2,9
Good health-seeking behavior was considered if participants adhered to all the five components listed above.2,9
Poor health-seeking behavior: was considered if participants did not adhere to one or more components of the health-seeking behavior listed above.2,9
Ethical Considerations
Ethical clearance was obtained from the Institutional Review Board of Jimma University, Institute of Health. A formal letter from the Institute of Health Science was submitted to selected public hospitals to acquire their cooperation. Ethical issues within the study were taken into consideration when carrying out the study. At the initial stage of data collection, informed oral and written consent was taken from respondents, and the participants were assured that their participation was recorded anonymously. Participants were informed of the purpose, merit, and demerits of the study, and their participation was voluntary. The obtained data were used only for research purposes and kept confidentially. This study complies with the Declaration of Helsinki.
Results
Socio-Demographic Characteristics of the Study
A total of 400 chronic patients participated, yielding a response rate of 94.8%. The majority of respondents or 53.0% were residing in urban. 198 (49.05%) of them were in the age range of 40–59, and the mean age was 48.3 (Table 2).
 |
Table 2 Socio-Demographic Characteristics of Respondents at Jimma Public Health Hospitals, Ethiopia, 2021 (N = 400) |
Clinical Characteristics of Study Participants
The majority 366 (91.5) of participants reported as they have no travel history. Of all chronic patients who participated in this study 284 (71.0%), 260 (65.0%) of them reported as they got medication with payment after the pandemic and had no comorbidity, respectively, and hypertension was mentioned more frequently among other chronic illnesses (Table 3).
 |
Table 3 Clinical and Treatment-Related Characteristics of Respondents at Jimma Public Health Hospitals, Ethiopia, 2021 (N = 400) |
Health-Seeking Behavior of Study Participants
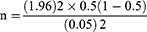
Of the total respondents, 156 (39.0%) of them had poor health-seeking behavior (Figure 1). Among patients who missed health care appointments (had poor health-seeking), fear of COVID-19 was frequently mentioned as a reason 76 (48.7%) followed by economic and transportation problems (Figure 2). Of all respondents who canceled health care appointments, 60 (39%) of them use self-refill as an alternative treatment and the rest use traditional healers and holy water, respectively (Figure 3).
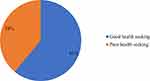 |
Figure 1 Health-seeking behavior of respondents at Jimma Public Health Hospitals, Ethiopia, 2021 (N = 400). |
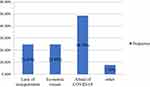 |
Figure 2 Reasons of respondents for missed health care appointments at Jimma Public Health Hospitals, Ethiopia, 2021 (N = 156). |
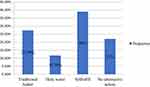 |
Figure 3 The alternative way used by respondents for the missed follow-up at Jimma Public Health Hospitals, Ethiopia, 2021 (N = 156). |
Factors Associated with Care-Seeking Behavior of Patients with Chronic Diseases
The likelihood of poor health-seeking behavior was about 3 times higher among patients who have a contact history with COVID-19 patients than those who have no contact (AOR = 2.8; 95% CI = 1.1–7.0). Patients who perceive moderate depression had about 2 times as poor health-seeking behavior as compared to patients with no depression (AOR = 2.3; 95% CI = 1.2–4.2). Moreover, the odds of patients with perceived extreme depression were 4.3 higher compared to those with no perceived depression (AOR = 4.3; 95% CI = 1.8–10.5). The likelihood to have poor health-seeking behavior was 2 times higher among patients who always encountered a shortage of medication (AOR = 2.4; 95% CI = 1.0–6.2). In addition, the odds of patients with no formal education were about 3 times higher compared to patients with higher educational status (AOR = 2.7; 95% CI = 1.0–9.0) (Table 4).
 |
Table 4 Factors Associated with Care-Seeking Behavior of Patients with Chronic Diseases at Public Hospitals in Jimma Zone, South West Ethiopia During COVID-19. Ethiopia, 2021 (N = 400) |
Discussion
This study assessed the impact of COVID-19 on the health-seeking behavior of chronic patients. This work makes a vital contribution to the limited pool of studies addressing the health-seeking behavior of chronic patients during COVID-19, particularly in Ethiopia. Non-communicable diseases are highly increasing from time to time while the COVID pandemic becomes a burden for the health system.3,6 The current study revealed that COVID −19 has made a significant impact on health-seeking behavior: 39% of patients had poor health-seeking behavior. Health care seeking disruption happened in similar studies in Singapore during COVID-19 as stated 40% of chronic patients missed follow-up during the COVID-19 outbreak.1 It is known that chronic disease may lead to severe morbidity or mortality unless a good follow-up and care are made.11,16 Moreover, this pandemic has also raised concerns about safely accessing health care and has reduced the ability to prevent or control chronic diseases.12,14,21 The major reason mentioned for poor follow-up was fear of being infected. Fear of being infected was shown as one of the major causes which disrupted the health-seeking behavior of patients with chronic illness in the Ebola outbreak that occurred in West Africa, the same happened in Ethiopia’s health care utilization due to the COVID-19 pandemic.22–24 The main alternative method for missed appointments reported was self-refill. This finding was in line with a cross-sectional telephone survey conducted elsewhere.2
Moreover, the study indicated that contact history with COVID −19 patients has significantly impacted the health-seeking behavior of follow-up to the chronic unit. This might be due to patients who have contact may isolate themselves even when they got common cold symptoms.18 Patients who perceive moderate and severe depression were found more likely to have poor health-seeking behavior compared to patients with no depression. Perceived depression has been increased during COVID-19 due to different reasons including lockdown,19 this result was proven by one of the studies indicating that depression-related impaired self-management may lead to poor health-seeking behavior in patients with chronic illness.20
Unlike studies conducted in tertiary hospitals elsewhere in Ethiopia, the current study indicated that age has no association with the care-seeking behavior of chronic patients.2 In this study, those who reported as they always face a shortage of medication since the start of the COVID-19 pandemic had poor health-seeking behavior than their counterparts. Poor health-seeking behavior among chronic patients was observed in Sierra Leone during the Ebola outbreak, indicating increased self-refill of medications with old prescriptions instead of seeking care at a health facility.22
In addition, the odds of poor health-seeking behavior were higher among patients with no formal education than in patients with higher education. Evidence from a cross-sectional study in Turkey indicated higher education has to be a positive predictor of health-seeking behaviors.23
Implications
These current findings may contribute several insightful implications for scientific information sources regarding the impact of COVID-19 on the health-seeking behavior of chronic patients. The study would give insight and enable healthcare administrators to strengthen the capacity of the hospitals to improve their readiness to care for future infectious diseases and to overcome barriers to health-seeking behavior by preparing an alternative way to address patients who canceled their follow-up from health care. Moreover, it could be used as an input for further research in a related area.
Limitations
Given the study was facility-based, it lacks evidence from the community. A community-based study would have been ideal to address patients who avoid follow-up at health facilities while they are diagnosed as chronic patients, and thus, we recommend further research.
Conclusion
This study indicated the COVID-19 outbreak affected the health-seeking behavior of patients with chronic diseases in the study area. The impact was found more significant among patients who had a contact history with COVID-19 patients and perceived depression. Moreover, patients who faced a shortage of medication and with low educational status are prone to have poor health-seeking behavior. As perceived depression and contact history with COVID 19 patients were predictors, a good council and education on precautionary measures of COVID 19 may enhance the health-seeking behavior of patients. Hospitals should solve problems regarding the shortage of medication as it hinders the motivation of chronic patients for health care follow-up. Furthermore, education should be promoted as the low educational status may affect health-seeking behavior across the nation.
Abbreviations
AOR, adjusted odds ratio; COVID-19; coronavirus disease-19, COR, crude odds ratio; OR, odds ratio; SPSS, Statistical Package for Social Sciences.
Acknowledgments
We are grateful to the administrative officials of Jimma zone public hospitals for giving us information, respective data collectors, and study participants for their valuable contribution to the realization of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Malhotra C, Chaudhry I, Ozdemir S, Finkelstein EA. Reduced health-care utilization among people with chronic medical conditions during coronavirus disease 2019. Proc Singapore Healthc. 2021;30(3):254–257. doi:10.1177/2010105820964533
2. Aklilu TM, Abebe W, Worku A, et al. The impact of COVID-19 on care seeking behavior of patients at tertiary care follow-up clinics: a cross-sectional telephone survey. Addis Ababa, Ethiopia. medRxiv. 2020. doi: 10.1101/2020.11.25.20236224.
3. Guo D, Han B, Lu Y, et al. Influence of the COVID-19 pandemic on quality of life of patients with Parkinson’s disease. Parkinson’s Dis. 2020;2020:1–6. doi:10.1155/2020/1216568
4. Johnson M. Wuhan 2019 novel coronavirus-2019-nCoV. Mater Methods. 2020;10:1–5. doi:10.13070/mm.en.10.2867
5. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(3):105924. doi:10.1016/j.ijantimicag.2020.105924
6. Reeve E, Thow AM, Huse O, Bell C, Peeters A, Sacks G. Policy-makers’ perspectives on the implementation of cross-sectoral nutrition policies, Western Pacific Region. Bull World Health Organ. 2021;99(12):865. doi:10.2471/BLT.20.283366
7. Lim SL, Woo KL, Lim E, Ng F, Chan MY, Gandhi M. Impact of COVID-19 on health-related quality of life in patients with cardiovascular disease: a multi-ethnic Asian study. Health Qual Life Outcomes. 2020;18(1):1–7. doi:10.1186/s12955-020-01640-5
8. Teixeira L, de Freitas RL, Abad A, et al. Anxiety-related psychological impacts in the COVID-19 pandemic on cardiovascular diseases and diabetes; 2020.
9. Latunji OO, Akinyemi OO. Factors influencing health-seeking behaviour among civil servants in Ibadan, Nigeria. Ann Ib Postgrad Med. 2018;16(1):52–60.
10. Combi C, Pozzani G, Pozzi G. Telemedicine for developing countries. Appl Clin Inform. 2016;7(04):1025–1050. doi:10.4338/ACI-2016-06-R-0089
11. Chakraborty K, Chatterjee M. Psychological impact of COVID-19 pandemic on general population in West Bengal: a cross-sectional study. Indian J Psychiatry. 2020;62(3):266. doi:10.4103/psychiatry.IndianJPsychiatry_276_20
12. Kazan Kizilkurt O, Dilbaz N, Noyan CO. Psychological impact of COVID-19 pandemic on general population in Turkey: risk factors. Asia Pac J Public Health. 2020;32(8):519. doi:10.1177/1010539520964276
13. EuroQolresearch Foundation. EQ5Duserguide; 2018. Available from: http://www.euroqol.org/publications/user.guide.
14. Shuka Z, Mebratie A, Alemu G, Rieger M, Bedi AS. Use of healthcare services during the COVID-19 pandemic in urban Ethiopia: evidence from retrospective health facility survey data. BMJ open. 2022;12(2):e056745. doi:10.1136/bmjopen-2021-056745
15. Malinauskienė V, Bernotaitė L. The impact of event scale–revised: psychometric properties of the Lithuanian version in a sample of employees exposed to workplace bullying. Acta medica Lituanica. 2016;23(3):185. doi:10.6001/actamedica.v23i3.3384
16. Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale—revised. Behav Res Ther. 2003;41(12):1489–1496. doi:10.1016/j.brat.2003.07.010
17. Samlani Z, Lemfadli Y, Oubaha S, Krati K. The impact of the COVID-19 pandemic on quality of life and well-being in Morocco. Archives Commun Med Public Health. 2020;6(2):130–134. doi:10.17352/2455-5479.000091
18. Agusto FB, Erovenko IV, Fulk A, et al. To isolate or not to isolate: the impact of changing behavior on COVID-19 transmission. BMC Public Health. 2022;22(1):1–20. doi:10.1186/s12889-021-12275-6
19. Parvar SY, Ghamari N, Pezeshkian F, Shahriarirad R. Prevalence of anxiety, depression, stress, and perceived stress and their relation with resilience during the COVID‐19 pandemic, a cross‐sectional study. Health Sci Report. 2022;5(1):e460. doi:10.1002/hsr2.460
20. Li H, Ge S, Greene B, Dunbar-Jacob J. Depression in the context of chronic diseases in the United States and China. Int J Nurs Sci. 2019;6:117e122. doi:10.1016/j.ijnss.2018.11.007
21. Hacker KA, Briss PA, Richardson L, Wright J, Petersen R. Peer reviewed: COVID-19 and chronic disease: the impact now and in the future. Prev Chronic Dis. 2021;18.
22. Vygen S, Tiffany A, Rull M, et al. Changes in health-seeking behavior did not result in increased all-cause mortality during the Ebola outbreak in Western Area, Sierra Leone. Am J Trop Med Hyg. 2016;95(4):897. doi:10.4269/ajtmh.16-0295
23. Abuduxike G, Aşut Ö, Vaizoğlu SA, Cali S. Health-seeking behaviors and its determinants: a facility-based cross-sectional study in the Turkish Republic of Northern Cyprus. Int J Health Policy Manag. 2020;9(6):240. doi:10.15171/ijhpm.2019.106
24. Romano F. The Impact of COVID-19 in Ethiopia: Policy Brief; 2021.
25. Dandena F, Teklewold B, Anteneh D. Impact of COVID-19 and mitigation plans on essential health services: institutional experience of a hospital in Ethiopia. BMC Health Serv Res. 2021;21(1):1–9. doi:10.1186/s12913-021-07106-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.