Back to Journals » Patient Preference and Adherence » Volume 17
Impact of COVID-19 Lockdown on Glycemic, Weight, Blood Pressure Control and Medication Adherence in Patients with Type 2 Diabetes
Authors Sim R , Chong CW, Loganadan NK , Hussein Z , Adam NL, Lee SWH
Received 1 June 2023
Accepted for publication 18 August 2023
Published 24 August 2023 Volume 2023:17 Pages 2109—2117
DOI https://doi.org/10.2147/PPA.S420545
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Ruth Sim,1 Chun Wie Chong,1 Navin Kumar Loganadan,2 Zanariah Hussein,3 Noor Lita Adam,4 Shaun Wen Huey Lee1,5– 7
1School of Pharmacy, Monash University Malaysia, Subang Jaya, Selangor, Malaysia; 2Department of Pharmacy, Putrajaya Hospital, Ministry of Health Malaysia, Putrajaya, Malaysia; 3Department of Medicine, Putrajaya Hospital, Ministry of Health Malaysia, Putrajaya, Malaysia; 4Department of Medicine, Hospital Tuanku Jaafar, Ministry of Health Malaysia, Seremban, Negeri Sembilan, Malaysia; 5School of Pharmacy, Faculty of Health and Medical Sciences, Taylor’s University, Subang Jaya, Selangor, Malaysia; 6Asian Centre for Evidence Synthesis in Population, Implementation and Clinical Outcomes (PICO), Monash University Malaysia, Bandar Sunway, Selangor, Malaysia; 7Center for Global Health, University of Pennsylvania, Philadelphia, PA, USA
Correspondence: Shaun Wen Huey Lee, School of Pharmacy, Monash University Malaysia, Subang Jaya, Selangor, Malaysia, Tel +60 3 5514 5890, Email [email protected]
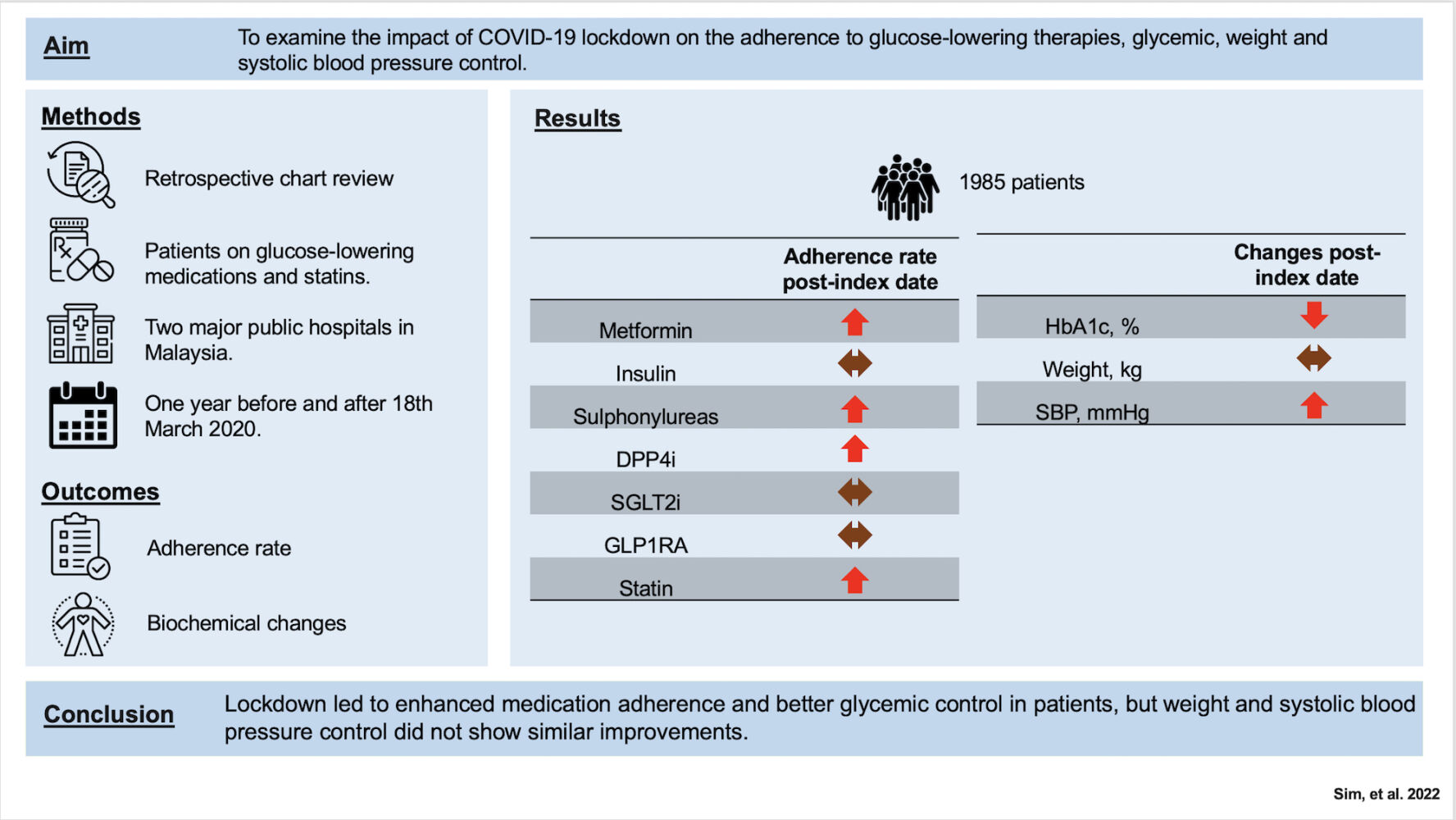
Abstract: Medication adherence profoundly affects blood glucose management in patients with type 2 diabetes. Measures to contain the COVID-19 pandemic have affected disease management and medication adherence, owing to limited access to healthcare facilities. This study aimed to examine the impact of the COVID-19 lockdown on adherence to glucose-lowering and lipid-lowering therapies (statins), and glycemic, weight, and systolic blood pressure control measures. A retrospective chart review was conducted one year pre- and post- March 18, 2020, for patients receiving glucose-lowering medications and lipid-lowering therapies (statins) in two major public hospitals in Malaysia. We compared the proportion of days covered by medication, HbA1c level, weight, and systolic blood pressure (SBP) values pre- and after the index date. A total of 1985 patients were included in this study. The adherence rate significantly increased for metformin, sulfonylureas dipeptidyl peptidase 4 inhibitors (DPP4i) and statin after the index date (metformin (PDC: 0.985 vs 0.978, p < 0.001), sulfonylureas (PDC: 0.988 vs 0.979, p < 0.01), DPP4i (PDC: 0.987 vs 0.98, p < 0.001), and statins (PDC: 0.983 vs 0.978, p < 0.05)). HbA1c levels were significantly reduced after the index follow-up (Mean difference: − 0.43%, p < 0.001), while there was a 2.5 mmHg (p = 0.03) significant increase in SBP post-index follow-up. No significant changes in weight were observed during the post-index follow-up period. In this study, we observed better medication adherence and glycemic control among patients during the lockdown, but not for weight and systolic blood pressure control.
Keywords: diabetes, covid-19, SARS-CoV 2, adherence, weight, glycemic
Graphical Abstract:
Introduction
Type 2 diabetes is a chronic and progressive condition marked by elevated blood glucose levels. The number of individuals with diabetes was estimated to be 537 million in 2021, and its prevalence is growing at a faster rate in low- and middle-income countries.1 Medication adherence is associated with better clinical outcomes including intermediate risk factors and long-term outcomes.2,3 People with type 2 diabetes are at a higher risk of SARS-CoV-2 virus (COVID-19) complications, especially among those with multimorbidity such as cardiovascular disease and obesity, making them very vulnerable to the infection.4 Malaysia implemented various movement restrictions totaling more than 500 days to curb the spread of COVID-19 infection since March 2020.5 This has caused considerable repercussions for people with type 2 diabetes, such as access to healthcare facilities, clinical visits, and physical exercise. Previous studies have shown mixed results regarding the impact of the COVID-19 lockdown on glycemic control and medication adherence in people with type 2 diabetes.6,7 Eberle et al 2021 found that lockdown was associated with worsening in glycemic control, while Patel et al 2021 did not find any difference in medication fills or glycemic control pre-pandemic and during pandemic period.6,7 In patients hospitalized with COVID-19 and experiencing severe clinical outcomes, diabetes, obesity, and hypertension have emerged as some of the most common risk factor.8–10 We aimed to examine the impact of the COVID-19 lockdown on glycemic control, weight, blood pressure control, and medication adherence in patients with type 2 diabetes. Additionally, we also examined the relationship between time interval of pre- and post-index follow-up and the difference in HbA1c, SBP and weight post follow-up studied as part of the secondary objective.
Materials and Methods
This retrospective study was conducted at two tertiary government hospitals. These hospitals are located in major cities in the state of Putrajaya and Negeri Sembilan and run weekly diabetes clinics with endocrinologists available to people with diabetes. During the COVID-19 period, these hospitals in Malaysia have implemented virtual clinics with telemedicine services and mail-delivery of medicines.11,12 Data, including sociodemographic details, drug prescriptions, and laboratory results, were manually extracted from the hospital medical records. The index date was set to be March 18, 2020, and the first day Movement Control Order (Movement Control Order March 18, 2020) was implemented in Malaysia. The study period was one year pre- and after the index date (Figure 1a). We identified people with type 2 diabetes aged >18 years who were receiving glucose-lowering therapies (metformin, insulin, sulfonylureas, dipeptidyl peptidase 4 inhibitors DPP4i, sodium-glucose co-transporter 2 inhibitors SGLT2i) and statins between January 2012 and December 2020. In 2012, both hospitals successfully implemented comprehensive medical record systems, enabling efficient tracking of medication records. We have excluded patient younger than 18 years, had missing baseline characteristics such as comorbidities and medical history or diagnosed as type 1 diabetes. The outcomes of interest included adherence to glucose-lowering therapies and statins, changes in glycated hemoglobin (Hba1c); weight and systolic blood pressure (SBP) pre- and post-index dates. Adherence to medication was measured as the proportion of days covered (PDC) by medication one year pre- and after the index date. PDC was calculated as number of days patients has access to treatment in the specified time interval divided by number of days in a specified time interval (one year pre- and post-index date).13 An adherence threshold of ≥0.8 was set to classify individuals as adherent, while those with a value <0.8 were categorized as nonadherent. As eligible patients were required to have pre- and post-laboratory values, we created separate cohorts for changes in Hba1c, weight, and SBP. We reported a difference in HbA1c, SBP and weight stratified by the time interval between pre- and post-index follow-up. The data collected closest to the laboratory test pre- and post-index follow-up were utilized. An analysis of variance (ANOVA) was conducted to compare the differences in the means of the outcomes at pre- and after the index date. Statistical significance was set at p < 0.05. All analyses were performed using R software (version 4.1.1).
 |
Figure 1 (a) Study period. (b) Flow chart of patient selection. |
Ethics Statement
The study was in conformance with the Declaration of Helsinki and was approved by the National Medical Research Register (Ministry of Health Malaysia) (NMRR-20-662-52570) and Monash Human Research Ethics Committee (Monash University) (2020-24900-45575). As patient consent to review their medical records was not required by the ethics committees, due to the retrospective design of this study and full data anonymization, informed consent for participation was waived by National Medical Research Register (Ministry of Health Malaysia) and Monash Human Research Ethics Committee (Monash University) in accordance to Declaration of Helsinki.
Results
A total of 1985 patients who met the inclusion criteria were included in the study (Figure 1b). The patient characteristics are shown in Table 1. The cohort included both males and females, with a mean age of 56.9 years and mean HbA1c of 8.09% (65 mmol/mol). The majority of patients were taking metformin (74.8%), followed by insulin (61%), DPP4i (56.3%), sulfonylureas (29.2%), SGLT2i (20.9%), and GLP1-RA (0.9%). Compared to the pre-index period, the adherence (PDC) post-index date increased for metformin, sulfonylureas, DPP4i and statins (Figure 2). We observed an increase in adherence to metformin post-index date compared to pre-index date (PDC: 0.985 vs 0.978, p < 0.001), sulfonylureas (PDC: 0.988 vs 0.979, p < 0.01), DPP4i (PDC: 0.987 vs 0.98, p < 0.001), and statins (PDC: 0.983 vs 0.978, p < 0.05). HbA1c levels were significantly reduced after the index follow-up (Mean difference: −0.43%, p < 0.001), while there was a 2.5 mmHg increase (p = 0.03) in SBP post-index follow-up (Table 2). No significant changes in weight were observed during the post-index follow-up period. The reduction in HbA1c and weight show a non-linear downward trend post-index follow-up as the time interval between follow-ups increased, except for days 60 and 90 post-index follow-up (Figure 3).
 |
Table 1 Characteristics of the Included Patients on Index Date |
 |
Table 2 Difference in HbA1c, Weight and Systolic Blood Pressure Values Pre- and Post-Index Date |
Discussion
In this retrospective study, we observed higher adherence to glucose-lowering medications and a reduction in HbA1c levels among people with type 2 diabetes during the COVID-19 pandemic, despite fewer outpatient visits. One possible explanation for these patterns could be the larger quantity of medications being supplied to patients due to the COVID lockdown, where the usual restriction on medication prescriptions was relaxed in some hospitals.7,14 Thong et al 2021 has reported an increase in quantity of medication supply during the COVID-19 pandemic in Malaysia.15 This could have prevented any medication disruption during the pandemic and reduced detrimental effects on glycemic control.
Second, telemedicine and mail-order pharmacies could have been highly utilized during the pandemic period, thereby providing uninterrupted healthcare services for patients. Studies by Patel et al 2021 and Nguyen et al 2021 have shown similar findings, whereby HbA1c level, HbA1c testing, and medication adherence rate were not substantially affected during the COVID-19 pandemic.7,16 Furthermore, our study findings could be attributed to tertiary hospital settings, where telemedicine and pharmacy delivery services were more established and more readily provided. Taken together, it is likely that patient care was not compromised during the pandemic period, although on-site HbA1c testing reduced during this period. However, our study had to consider that the PDC calculation was based on medication prescription, which might not correlate directly with patients’ medication-taking behavior.
Our study also found interesting results indicating a non-significant decrease in bodyweight among patients during the COVID-19 pandemic period. We hypothesized that these individuals with high average BMI were likely at an advanced stage of the diabetes, with already low levels of physical activity. The imposed lockdown restrictions prevented them from engaging in excessive food consumption and encouraged healthier eating habits through increased home cooking. Furthermore, the introduction of newer glucose-lowering therapies, known for their weight-reducing effects, likely played a role in the observed weight loss. It is worth noting that contrasting findings were reported in other studies, where notable changes in bodyweight were not observed in people with diabetes.17–19
This report presents the first comprehensive analysis of COVID-19’s impact on glycemic, weight, and blood pressure control in a large patient population in Malaysia, aiming to fill knowledge gaps and provide insights for targeted interventions and management strategies. Nevertheless, our study had some limitations. First, owing to the retrospective nature of the study, unmeasured confounding bias may exist. Second, when measuring adherence, we assumed that medication consumption corresponded to medication prescriptions. Third, this study was conducted in tertiary hospitals; thus, the findings may not be generalizable to primary care settings or the entire Malaysian population. A notable number of patients in this study had a longer history of diabetes, pre-existing cardiovascular disease and microvascular disease. These observations could be attributed to the fact that the study took place in tertiary hospital settings, where patients were typically in an advanced stage of the disease. They were referred from primary care settings due to poorly controlled diabetes. In fact, the average HbA1c (8.6%) and BMI level (33.72 kg/m2) of the patients in our study, was considerably higher than the national average HbA1c (7.9%) and BMI (27.9 kg/m2).20 Fourth, the difference in number of patients on medication pre- and post-index follow-up may have been influenced by the change of medications in the follow-up such as introduction of novel glucose-lowering therapies (DPP4i, SGLT2i) in recent years. Fifth, the retrospective nature of the study lost some data on clinical parameters. As the primary objective of this manuscript was to serve as a concise report to inform readers, we did not include additional statistical tests to adjust for confounders. Hence, the results have to be interpreted cautiously.
In this study, we found that those with a longer interval between pre- and post- index follow-up had a smaller reduction in HbA1c levels and weight. This further established the fact that better adherence to HbA1c test was beneficial for patients’ glycemic control.21 Our study also suggested a need to look into the prescribing pattern of antihypertensives during the pandemic period, as there was a small but significant increase in systolic blood pressure among people with type 2 diabetes.
Conclusion
In conclusion, we observed better adherence for metformin, sulfonylureas, DPP4i and statins, and glycemic control among people with type 2 diabetes during the COVID-19 lockdown period. It is essential for policymakers, clinicians, and patients to work collaboratively to sustain the positive changes observed during the pandemic, ensuring continued medication adherence, glycemic control, and overall management of type 2 diabetes.
Acknowledgments
We would like to thank the Director General of Health Malaysia for their permission to publish this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Federation ID. IDF Diabetes Atlas.
2. Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27(12):2800–2805. doi:10.2337/diacare.27.12.2800
3. Hong JS, Kang HC. Relationship between oral antihyperglycemic medication adherence and hospitalization, mortality, and healthcare costs in adult ambulatory care patients with type 2 diabetes in South Korea. Med Care. 2011;49(4):378–384. doi:10.1097/MLR.0b013e31820292d1
4. Hartmann-Boyce J, Morris E, Goyder C, et al. Diabetes and COVID-19: risks, management, and learnings from other national disasters. Diabetes Care. 2020;43(8):1695–1703. doi:10.2337/dc20-1192
5. Expatriate Services Division. Covid-19 (latest announcement) [press release]. Immigration Department of Malaysia; 2020. Available from: https://esd.imi.gov.my/portal/latest-news/announcement/announcement-convid19-latest/.
6. Eberle C, Stichling S. Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: a systematic review. Diabetol Metab Syndr. 2021;13(1):95. doi:10.1186/s13098-021-00705-9
7. Patel SY, McCoy RG, Barnett ML, Shah ND, Mehrotra A. Diabetes care and glycemic control during the COVID-19 pandemic in the United States. JAMA Intern Med. 2021;181(10):1412–1414. doi:10.1001/jamainternmed.2021.3047
8. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5
9. Parra-Bracamonte GM, Lopez-Villalobos N, Parra-Bracamonte FE. Clinical characteristics and risk factors for mortality of patients with COVID-19 in a large data set from Mexico. Ann Epidemiol. 2020;52:93–98.e92. doi:10.1016/j.annepidem.2020.08.005
10. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
11. Thong HK, Wong DKC, Gendeh HS, Saim L, Athar P, Saim A. Perception of telemedicine among medical practitioners in Malaysia during COVID-19. J Med Life. 2021;14(4):468–480. doi:10.25122/jml-2020-0119
12. Pharmaceutical Services Programme MoHM. COVID-19 pandemic in Malaysia: the Journey. A report by the Pharmaceutical Services Programme, Ministry of Health Malaysia; 2020.
13. Canfield SL, Zuckerman A, Anguiano RH, et al. Navigating the wild west of medication adherence reporting in specialty pharmacy. J Manag Care Spec Pharm. 2019;25(10):1073–1077. doi:10.18553/jmcp.2019.25.10.1073
14. Di Novi C, Leporatti L, Levaggi R, Montefiori M. Adherence during COVID-19: the role of aging and socio-economics status in shaping drug utilization. J Econ Behav Organ. 2022;204:1–14. doi:10.1016/j.jebo.2022.10.012
15. Thong KS, Selvaratanam M, Tan CP, et al. Pharmacy preparedness in handling COVID-19 pandemic: a sharing experience from a Malaysian tertiary hospital. J Pharm Policy Pract. 2021;14(1):61. doi:10.1186/s40545-021-00343-6
16. Nguyen A, Williams T, Kangethe A, Polson M. Impacts of COVID-19 on the Adherence to Oral Anti-Diabetic Medications in Commercially Insured Adult Patients with Type 2 Diabetes Mellitus. Magellan Medicaid Administration, Inc.; 2021.
17. Pla B, Arranz A, Knott C, et al. Impact of COVID-19 lockdown on glycemic control in adults with type 1 diabetes mellitus. J Endocrinol. 2020;4(12). doi:10.1210/jendso/bvaa149
18. Hosomi Y, Munekawa C, Hashimoto Y, et al. The effect of COVID-19 pandemic on the lifestyle and glycemic control in patients with type 1 diabetes: a retrospective cohort study. Diabetol Int. 2022;13(1):85–90. doi:10.1007/s13340-021-00507-4
19. Ke HT, Hsieh CL, Cheng WJ. Physical activity, dietary behavior, and body weight changes during the COVID-19 nationwide level 3 alert in Taiwan: RESULTS of a Taiwanese online survey. Nutrients. 2022;14(22):4941. doi:10.3390/nu14224941
20. Ministry of Health Malaysia. National Diabetes Registry Report 2013–2019; 2020. Available from: https://www.moh.gov.my/moh/resources/Penerbitan/Rujukan/NCD/Diabetes/National_Diabetes_Registry_Report_2013-2019_26082021.pdf.
21. Imai C, Li L, Hardie RA, Georgiou A. Adherence to guideline-recommended HbA1c testing frequency and better outcomes in patients with type 2 diabetes: a 5-year retrospective cohort study in Australian general practice. BMJ Qual Saf. 2021;30(9):706–714. doi:10.1136/bmjqs-2020-012026
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


