Back to Journals » Journal of Asthma and Allergy » Volume 15
Impact of Baseline Lung Function on Future Exacerbations in Patients with Moderate-to-Severe Asthma
Authors Khan AH , Gray C, Eckert L, Amand C, Maroni J, Wang Z, Jones B , Berni T, Morgan CL, Rowe PJ
Received 20 May 2022
Accepted for publication 30 September 2022
Published 11 November 2022 Volume 2022:15 Pages 1639—1644
DOI https://doi.org/10.2147/JAA.S375134
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Amrita Dosanjh
Asif H Khan1 *, Cori Gray2 *, Laurent Eckert,1 Caroline Amand,1 Jaman Maroni,3 Zhixiao Wang,3 Bethan Jones,4 Thomas Berni,4 Christopher Ll Morgan,4 Paul J Rowe5
1Sanofi, Chilly-Mazarin, France; 2Sanofi, Cambridge, MA, USA; 3Regeneron Pharmaceuticals Inc, Tarrytown, NY, USA; 4Pharmatelligence, Cardiff, UK; 5Sanofi, Bridgewater, NJ, USA
*These authors contributed equally to this work
Correspondence: Asif H Khan, Sanofi, 1 Avenue Pierre Brossolette, Chilly-Mazarin, France, 91385, Tel +33160495076, Email [email protected]
Introduction
Asthma is a chronic inflammatory disease characterized by reversible and variable expiratory airflow obstruction.1 It is well known that abnormalities of airway structure and hyperresponsiveness contribute to impaired lung function.2 Airway remodeling and hyperinflation are also associated with accelerated decline in lung function.3 In addition, severe asthma exacerbations are correlated with a rapid decline in lung function and reduction in airway reversibility, leading to the progression of irreversible airflow limitation over time.4 Although reduced lung function is associated with worsened outcomes and increased mortality risk,5,6 limited real-world evidence exists on the effect of forced expiratory volume in 1 second percent predicted (FEV1pp) on exacerbations in patients with moderate-to-severe asthma.7,8 In this retrospective database study, we aimed to determine the baseline distribution of FEV1pp in patients with moderate-to-severe asthma and the association between baseline FEV1pp and risk of severe asthma exacerbations in a large UK dataset.
Methods
Study Design
This retrospective cohort study was performed using the Clinical Practice Research Datalink (CPRD) database linked to Hospital Episode Statistics inpatient, outpatient and accident and emergency data. The CPRD is an anonymized, longitudinal research database that derived data from nearly 700 primary-care practices in the UK when this study was conducted and provided healthcare data of 60 million patients.9 Patients were identified from 1st January 2010 to 31st December 2012 and followed up for 36 months from the index date. The index date was defined as the date of the first asthma medication prescription during the study period. A variable-length period from the registration date of patients (from up-to-standard CPRD practices) in the database to the index date was identified as a pre-index baseline period and was used to capture comorbidities.
Patients
Patients aged ≥18 years at the index date, with ICD-1010 clinical diagnosis and Read codes for asthma were identified. Patients with a diagnosis of COPD were excluded. Asthma severity (moderate-to-severe) was determined using the prescription criteria consistent with the British Thoracic Society (BTS) 2011 guideline Steps 3–5 (medium-high dose inhaled corticosteroid [ICS] and long-acting β-agonist plus additional controller medications or oral corticosteroids [OCS], as needed for asthma control).11
Outcomes
Baseline FEV1 values were taken as the observation nearest to the index date within ±180 days. Observed FEV1 values were compared with the normal range accounting for age, gender and height and were categorized as Group 1: FEV1pp ≥ 80%; Group 2: FEV1pp 50–79%; Group 3: FEV1pp < 50%. The FEV1pp values could be either pre- or post-bronchodilator FEV1. Exacerbations in the year prior to the index date were considered as baseline. Severe asthma exacerbations during the follow-up period were identified by an acute course of OCS for <7 days or an asthma-related emergency hospital contact (A&E diagnosis code 251) or inpatient admission with a primary diagnosis (ICD10 J45, J45.0, J45.1, J45.8, and J45.9) in non-OCS-dependent patients. For OCS-dependent patients (BTS step 5), a severe exacerbation was defined as above but without the criteria for an acute course of OCS use.
Statistical Analysis
Descriptive statistics were used to analyze baseline demographics and clinical characteristics. Univariate analyses were compared using t-test and chi-squared tests for continuous data and categorical variables, respectively. Multivariable regression models were used to estimate the risk of severe asthma exacerbations after adjusting for covariates, including age at the index date, smoking, body mass index, gender, rhinitis, presence of chronic sinusitis, nasal polyps, atopic dermatitis, diabetes, anaphylaxis, ischemic heart disease, heart failure, food allergy, anxiety, depression, and psoriasis. The incident rate ratio (IRR) for severe asthma exacerbation was calculated over the 12 months using the Poisson regression. The Cox proportional hazard model was used to determine hazard ratios (HR) for the risk of severe exacerbation (time-to-first exacerbation) over the 3-year follow-up. Additional sensitivity analyses were performed by adjusting for severe baseline exacerbations as a covariate in addition to the covariates listed above.
Results
Baseline Demographics and Patient Characteristics
Of 36,164 patients identified, 1865 had baseline FEV1pp values reported and were included in this analysis. Mean (SD) age was 47.5 (16.5) years in the overall population and 1130 (60.6%) were women. Based on the FEV1pp values, 1106 (59.3%) patients were categorized in Group 1 (FEV1pp ≥ 80%), 644 (34.5%) in Group 2 (FEV1pp 50–79%) and 115 (6.2%) in Group 3 (FEV1pp < 50%). Baseline FEV1pp measurements occurred within approximately 50 days of the index date. The average pre-index date baseline period, when comorbidities were captured, was 8 years. The number of patients on BTS Step 5 were 83 (7.5%) in Group 1, 58 (9.0%) in Group 2, and 22 (19.1%) in Group 3. Baseline demographics and patient characteristics are described in Table 1.
 |
Table 1 Baseline Demographics and Patient Characteristics |
Exacerbations
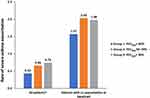
Rates of severe asthma exacerbations over 12 months in patients in Groups 1–3, and in patients with ≥1 severe asthma exacerbation at baseline in these groups are presented in Figure 1.
The annual IRR of severe exacerbations was significantly higher for Group 2 (1.46 [1.27 to 1.68]; P < 0.0001) and 3 (2.03 [1.59 to 2.54]; P < 0.0001) versus Group 1 (Figure 2) over 12 months following index date. The risk of severe asthma exacerbation was significantly greater in patients in Group 2 (P = 0.0018) and 3 (P < 0.0001), compared with those in Group 1 during the 36-month follow-up period (Figure 2). In sensitivity analysis, similar results were observed after adjusting for baseline severe exacerbations. The annual IRR of severe exacerbation was significantly higher for Group 2 (1.61 [1.27 to 2.05]; P < 0.0001) and 3 (1.78 [1.22 to 2.54]; P = 0.0029) versus Group 1; however the risk of severe exacerbation was significantly greater for Group 3 versus Group 1 (1.45 [1.04 to 2.03]; P = 0.0308) but not for Group 2 (1.11 [0.91 to 1.34]; P = 0.3011).
Discussion
In asthma, permanent structural changes in the airway can lead to a progressive loss of lung function, increasing airflow obstruction.12 These structural changes can include subepithelial fibrosis (thickening of the membrane), airway smooth muscle hypertrophy and hyperplasia. Clinically, decreased lung function can result in reduced treatment efficacy, is associated with poor asthma control, and lower health-related quality of life, and is a more reliable indicator of exacerbation severity13–15 than symptoms.1
We report the prevalence of impaired lung function in a population cohort representative of patients with moderate-to-severe asthma treated in the UK. Although lung function assessment is recommended for diagnosis1 and periodically after that in asthma, we found that only about 5% of the patients in this cohort had FEV1 recorded, showing low utilization at the primary health care level. Indeed, in a discussion on the national review of asthma deaths,16 one of the recommendations to reduce the mortality rate due to asthma was a routine measurement of lung function.17
FEV1pp allows for the comparison of the functional measure of lung function with a population. In the current analysis, ~40% of patients had impaired lung function with FEV1pp <80% (FEV1pp 50–79%, 34.5%; FEV1pp < 50%, 6.2%), while the remaining patients experienced mild airflow obstruction (FEV1pp ≥ 80%). Although asthma severity cannot be described by FEV1pp alone, it is a marker of disease severity that can be measured objectively and is reproducible.1,18 In this analysis, 6.2% of the patients had severely impaired lung function with FEV1pp < 50% despite treatment with a standard-of-care therapy. We did not assess specialist referrals for these patients; however, this highlights the unmet needs in some patients with moderate-to-severe asthma.
Further, during the follow-up period, we observed that the patients with low FEV1pp had increased exacerbation rates and a higher risk of severe exacerbations over the 36-month follow-up, which were about 20% and 60% greater, respectively, in patients in Group 2 (FEV1pp 50–79%) and Group 3 (FEV1pp <50%), compared with Group 1 (FEV1pp ≥80%), respectively. Data from this analysis were in line with previous findings, wherein lower FEV1pp values were associated with an increased risk of severe asthma exacerbations.5,19–21 Assessment of the risk of future exacerbations is an important aspect in the clinical management of asthma, and FEV1pp values at baseline can be a reliable predictor of future risks and guide treatment.
In Groups 1–3, severe exacerbations were even higher in patients with ≥1 severe asthma exacerbation at baseline than in the overall population; a formal statistical analysis was not performed to evaluate these differences. This is consistent with published evidence suggesting prior severe exacerbation as a predictor of future severe exacerbations.22 Exacerbations represent a change in lung function or asthma symptoms. Severe exacerbations can occur in patients with well-controlled or mild asthma symptoms23 and can be life-threatening.
There are a few limitations that should be considered. Lung function measurement (FEV1pp) could be biased as only patients with moderate-to-severe asthma were assessed. The current analysis compares the rate and risk of exacerbations in patients with impaired lung function versus those with mild airflow limitation to evaluate the impact of FEV1pp values on exacerbations. Accordingly, a comparison between Group 2 and 3 was out of the scope of this analysis. Further, severe exacerbations were identified by either an acute course of OCS use or asthma-related emergency room or hospital admission in this analysis. For OCS-dependent patients (BTS step 5), an acute course of OCS was not one of the criteria. However, given the low proportion (8.7%) of patients in BTS step 5, this might not impact the overall findings from this analysis. In addition, an analysis combining spirometry and biomarkers at baseline could provide additional predictive value in identifying patients with a greater exacerbation risk.
Conclusion
Lung function is an important parameter in asthma control; however, as reported in this analysis, only a few patients have this assessed in clinical practice. The data from this analysis showed that low FEV1pp is a significant predictor of increased rate and greater risk of severe asthma exacerbations. Lung function in asthma typically declines over time, contributing to an increased risk of exacerbations and further impairment of asthma control. Therefore, it is important to assess lung function in patients with asthma to optimize treatment options in patients with low lung function to improve patient outcomes, including asthma control.
Data Sharing Statement
The datasets used and/or analysed during the current analysis are available from the corresponding author on reasonable request.
Ethics Approval
This study is based in part on data from the Clinical Practice Research Datalink (CPRD) obtained under license from the UK Medicines and Healthcare products Regulatory Agency. The anonymized data are provided by patients and collected by the NHS as part of their care and support. The interpretation and conclusions contained in this study are those of the author/s alone. The CPRD has ethics approval from the Health Research Authority to support research using anonymized patient data. This study received protocol approval (ISAC 17_077) from the CPRD Independent Scientific Advisory Committee. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Acknowledgments
The research was sponsored by Sanofi and Regeneron Pharmaceuticals, Inc. Medical writing/editorial assistance was provided by Vatsal Vithlani (M.Pharm) and Amit Garg (M.Pharm) of Sanofi, according to the Good Publication Practice guideline.
Author Contributions
All authors contributed to data analysis, drafting, or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
The study was funded by Sanofi and Regeneron Pharmaceuticals Inc.
Disclosure
Khan AH, Gray C, Eckert L, Amand C and Rowe PJ are employees of Sanofi, may hold stock and/or stock options in the company. Maroni J and Wang Z are employees of Regeneron Pharmaceuticals Inc, may hold stock and/or stock options in the company. Jones B, Berni T and Morgan CL are employees of Pharmatelligence, which was funded by Sanofi to conduct the study. The authors report no other conflicts of interest.
References
1. Global Initiative for Asthma. Global strategy for asthma management and prevention; 2021. Available from: http://www.ginasthma.org/.
2. James AL, Palmer LJ, Kicic E, et al. Decline in lung function in the Busselton Health Study: the effects of asthma and cigarette smoking. Am J Respir Crit Care Med. 2005;171(2):109–114. doi:10.1164/rccm.200402-230OC
3. Krings JG, Goss CW, Lew D, et al. Quantitative CT metrics are associated with longitudinal lung function decline and future asthma exacerbations: results from SARP-3. J Allergy Clin Immunol. 2021;148(3):752–762. doi:10.1016/j.jaci.2021.01.029
4. Matsunaga K, Hirano T, Oka A, et al. Progression of irreversible airflow limitation in asthma: correlation with severe exacerbations. J Allergy Clin Immunol Pract. 2015;3(5):759–764 e1. doi:10.1016/j.jaip.2015.05.005
5. Tupper OD, Ulrik CS. Long-term predictors of severe exacerbations and mortality in a cohort of well-characterised adults with asthma. Respir Res. 2021;22(1):269. doi:10.1186/s12931-021-01864-z
6. Knuiman MW, James AL, Divitni ML, et al. Lung function, respiratory symptoms, and mortality: results from the Busselton Health Study. Ann Epidemiol. 1999;9(5):297–306. doi:10.1016/S1047-2797(98)00066-0
7. Kitch BT, Paltiel AD, Kuntz KM, et al. A single measure of FEV1 is associated with risk of asthma attacks in long-term follow-up. Chest. 2004;126(6):1875–1882. doi:10.1378/chest.126.6.1875
8. Hansen EF, Vestbo J, Phanareth K, Kok-Jensen A, Dirksen A. Peak flow as predictor of overall mortality in asthma and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163(3 Pt 1):690–693. doi:10.1164/ajrccm.163.3.2006120
9. Clinical Practice Research Datalink (CPRD) | UK data driving real-world evidence; 2019. Available from: https://www.cprd.com/.
10. World Health Organization. International statistical classification of diseases and related health problems 10th revision; 2010. Availabe from: https://icd.who.int/browse10/2010/en#/X.
11. British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma (101): a national clinical guideline; 2011. Available from: http://globalasthmanetwork.org/management/guides/bosnia_and_herzegovina/British%20guideline%20for%20asthma.pdf.
12. Education National Asthma and Prevention Program. Expert Panel Report 3 (EPR-3): guidelines for the diagnosis and management of asthma-summary report 2007. J Allergy Clin Immunol. 2007;120(5 Suppl):S94–S138. doi:10.1016/j.jaci.2007.09.029
13. Fleming L, Murray C, Bansal AT, et al. The burden of severe asthma in childhood and adolescence: results from the paediatric U-BIOPRED cohorts. Eur Respir J. 2015;46(5):1322–1333. doi:10.1183/13993003.00780-2015
14. Shaw DE, Sousa AR, Fowler SJ, et al. Clinical and inflammatory characteristics of the European U-BIOPRED adult severe asthma cohort. Eur Respir J. 2015;46(5):1308–1321. doi:10.1183/13993003.00779-2015
15. Ilmarinen P, Juboori H, Tuomisto LE, Niemela O, Sintonen H, Kankaanranta H. Effect of asthma control on general health-related quality of life in patients diagnosed with adult-onset asthma. Sci Rep. 2019;9(1):16107. doi:10.1038/s41598-019-52361-9
16. Why asthma still kills: the National Review of Asthma Deaths (NRAD) confidential enquiry report. London: Royal College of Physicians; 2014. Available from: http://www.rcplondon.ac.uk/sites/default/files/why-asthma-still-kills-full-report.pdf.
17. Levy ML. The national review of asthma deaths: what did we learn and what needs to change? Breathe. 2015;11(1):14–24. doi:10.1183/20734735.008914
18. Enright PL, Lebowitz MD, Cockroft DW. Physiologic measures: pulmonary function tests. Asthma outcome. Am J Respir Crit Care Med. 1994;149(2 Pt 2):S9–S18; discussion S19–S20. doi:10.1164/ajrccm/149.2_Pt_2.S9
19. Zeiger RS, Yegin A, Simons FE, et al. Evaluation of the National Heart, Lung, and Blood Institute guidelines impairment domain for classifying asthma control and predicting asthma exacerbations. Ann Allergy Asthma Immunol. 2012;108(2):81–87. doi:10.1016/j.anai.2011.12.001
20. Patel M, Pilcher J, Reddel HK, et al. Predictors of severe exacerbations, poor asthma control, and beta-agonist overuse for patients with asthma. J Allergy Clin Immunol Pract. 2014;2(6):751–758. doi:10.1016/j.jaip.2014.06.001
21. Papaioannou AI, Kostikas K, Bakakos P, et al. Predictors of future exacerbation risk in patients with asthma. Postgrad Med. 2016;128(7):687–692. doi:10.1080/00325481.2016.1220807
22. Chipps BE, Zeiger RS, Borish L, et al. Key findings and clinical implications from The Epidemiology and Natural History of Asthma: outcomes and Treatment Regimens (TENOR) study. J Allergy Clin Immunol. 2012;130(2):332–342 e310. doi:10.1016/j.jaci.2012.04.014
23. Reddel H, Ware S, Marks G, Salome C, Jenkins C, Woolcock A. Differences between asthma exacerbations and poor asthma control. Lancet. 1999;353(9150):364–369. doi:10.1016/S0140-6736(98)06128-5
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.