Back to Journals » Patient Preference and Adherence » Volume 16
Immediate Postnatal Care Satisfaction and Associated Factors Among Postnatal Women in Public Health Facilities at Debre Markos Town, Northwest Ethiopia, 2021
Authors Bekele SB , Yirdaw BW , Abuhay M, Gebremichael MA
Received 15 November 2021
Accepted for publication 24 December 2021
Published 18 January 2022 Volume 2022:16 Pages 137—147
DOI https://doi.org/10.2147/PPA.S348597
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Sintayehu Bezabih Bekele,1 Birhanu Wubale Yirdaw,2 Mulunesh Abuhay,2 Mathewos Alemu Gebremichael3
1Department of Midwifery, Mizan Aman College of Health Sciences, Mizan Aman, Ethiopia; 2School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia; 3Department of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia
Correspondence: Sintayehu Bezabih Bekele Email [email protected]
Background: Immediate postnatal care (PNC) satisfaction is considered as the desired outcome of the health care system and determines the use of subsequent health care services. There is a paucity of evidence on the level of immediate PNC satisfaction in the study setting. Therefore, the aim of this study was to assess the level of immediate PNC satisfaction and associated factors among women who gave birth in Debre Markos town public health institutions, northwest Ethiopia.
Methods: An institution-based cross-sectional study was conducted from January 1 to February 28, 2021, and a systematic sampling technique was used to select the postnatal women. An interviewer-administered pretested structured tool was used. The level of immediate PNC satisfaction was measured by Jipi’s postnatal satisfaction with the nursing care questionnaire (JPSNQ). The collected data were entered into EpiData version 4.6.0 and exported to SPSS version 23 for management and analysis. Both bivariable and multivariable binary logistic regression analysis were applied. Adjusted odds ratios (AORs) with corresponding 95% confidence intervals (CIs) were calculated and statistical significance was declared at P-value < 0.05.
Results: A total of 389 postnatal mothers participated in this study with a response rate of 98.73%. Immediate PNC satisfaction was 60.90% (95%CI: 56.50– 65.60). Postnatal women having multiparity (AOR=7.31, 95%CI: 4.40– 12.17), four and more antenatal care (ANC) visits (AOR=1.90, 95%CI: 1.08– 3.36), satisfied by delivery care (AOR=2.05, 95%CI: 1.24– 3.40), received friendly care (AOR=7.72, 95%CI: 2.42– 13.52) and having companion (AOR=2.48, 95%CI: 1.37– 4.50) had higher likelihood of immediate PNC satisfaction.
Conclusion: Women’s satisfaction with immediate PNC was higher than the national achievements of targets for the client satisfaction. Therefore, health-care providers should encourage frequent ANC visits, friendly care, and companionship to increase the level of immediate PNC satisfaction.
Keywords: immediate postnatal care, women’s satisfaction, Debre Markos town, northwest, Ethiopia
Background
The immediate postnatal period refers to the time just after childbirth to the first 24 h, during which the infant’s physiology adapts, and the risks to the mother and other significant morbidities are highest.1,2
Immediate postnatal care (PNC) satisfaction has been defined as the level at which mothers’ immediate postnatal health care needs are met, in regard to their expectations, giving them a sense of happiness and it is considered one of the desired outcomes of health care.1,3
Despite being a very important time for the provision of interventions that are vital to the health of the mother and the newborn, the immediate PNC is among the weakest of all reproductive and child health programs and more than half of maternal deaths and about 40% newborn deaths occur in the first 24 h after birth.4–6
Understanding the experience of a client concerning health care is important to obtain valid information about the care and to identify problem areas that could be improved and enable measurable improvements in user satisfaction with the care they received.7 Evidence had indicated that satisfaction affects health service utilization; mothers’ satisfactory experiences in immediate PNC enhances their compliance with subsequent postnatal care visits and uptake of health-care services such as family planning services, immunizations, and recommendation of services to others.1,8,9
In contrast to this, when immediate PNC is unsatisfactory; dissatisfied mothers do not follow the recommendations offered by the health-care providers. And also dissatisfied mothers end treatment prematurely, do not cooperate in the implementation of the care and treatment plans, and seek help elsewhere, treatment refusal even in emergency conditions, which could result in severe maternal and/or neonatal morbidity or mortality.1,3,10,11
Ethiopia has been implementing a maternal health quality improvement initiative that encompasses satisfaction of clients with the care they received and working to achieve an increased proportion of clients satisfied during their last health-care visit to 75% by 2024/25 in Health sector Transformation Plan II (HSTP).9,12
An institution-based cross-sectional study done in Awi zone13 and West Shewa,14 Ethiopia showed that about 63% and 55.6% were satisfied with the postnatal care they received, respectively.
Women’s satisfaction with immediate PNC is significantly influenced by provider-interaction during episodes of care, surrounding physical environment, interpersonal skills in terms of courtesy, respect by health-care providers, communication skills, explanation, and clear information, technical skills like clinical competency, and hospital equipment.15,16
Even though immediate postnatal care satisfaction determines the use of subsequent health care services, there is a scarcity of evidence which shows the level and factors that affects immediate PNC satisfaction in the study setting. Hence, the aim of this study was to assess the level of immediate postnatal care satisfaction and associated factors among women who gave birth in Debre Markos town public health institutions, East Gojjam zone, northwest Ethiopia Figure 1).
Methods
Study Design, Setting, and Period
An institution-based cross-sectional study was conducted in Debre Markos town public health institutions from January 1 to February 28, 2021. Debre Markos town is the administrative town of East Gojjam Zone, which is located 276 km away from Bahir Dar, the capital city of Amhara Regional state and 300 km away from Addis Ababa (capital city of Ethiopia); it has a latitude and longitude of 10°20′N 37°43′E and an elevation of 2446 m. According to the population projection of Ethiopia for all regions at woreda level from 2014–2017, the total population of the town is estimated to be 92,470. Among these 46,738 are females.17 Currently, it has seven kebeles (the smallest administrative unit in Ethiopia). Debre Markos town has one Comprehensive Specialized hospital and three public health centers. All four public health institutions in the town are providing immediate postnatal care services.
Population
All women who gave birth in the Debre Markos town public health institutions in the study period were included and taken as a study population. However, those postnatal women critically ill (unable to communicate) were excluded.
Sample Size Determination
The sample size was determined by using single population proportion formula through StatCalc Epi Info™ version 7.2.4.0 considering the following assumptions: 95% level of confidence, 5% margin of error, and taking 63% hypothesized proportion of women satisfied by the postnatal care from previous study done in Awi zone, Amhara region, Ethiopia.13 By adding 10% non-response rate, the final sample was 394.
Sampling Technique
Systematic random sampling technique was used to select study participants. Before the actual data collection, the average two months delivery report was taken from each health institution’s PNC registration book. Samples were proportionally allocated to each public health institution based on their average two-month cases. Skipping interval was calculated by dividing a total population for the sample size (k=N/n). Finally, study subjects were selected by skipping the skipping interval “k” Figure 2).
Study Variables
The dependent variable was an immediate PNC satisfaction level (satisfied or unsatisfied). The independent variables were sociodemographic characteristics such as age, religion, ethnicity, place of residence, maternal occupation, maternal educational status, marital status, husband’s educational status, husband’s occupation, and average monthly income, an obstetrics-related characteristics like gravidity/parity, number of live children, pregnancy status, faced complication, mode of delivery, baby’s condition, gestational age, and sex of the baby. Furthermore, previous ANC follow-up/ANC follow-up, number of ANC, place of previous delivery, place of current delivery, satisfaction with delivery services, previous PNC follow-up were other dependent variables. Health care provider-related variables such as gender, advising about maternal postnatal danger signs/advised about neonatal danger signs, friendly care, and health facility related variables like reaching time, having companion and also women’s perspective to health facility and health-care provider related factors such as perceived privacy, perceived support, and perceived facility cleanness were taken as independent variables.
Operational Definitions
Immediate PNC Satisfaction
This was measured by a five-point Likert scale which was adapted from Jipi’s postnatal satisfaction with nursing care questionnaire (JPSNQ)18 and determined by summing up scores and divided by the number of items in each subscales which gives an overall mean that could be attained as a general measure of the mother’s satisfaction with immediate PNC.1 Based on an overall mean score, who scored mean and above (≥154.95) were categorized as satisfied and respondents who scored below mean were categorized as unsatisfied.
Friendly Care
Friendly care was measured by seven “yes or no” questions and considered as having received friendly care if the women answered “yes” for seven questions, otherwise it was considered as not having received friendly care.19
Satisfaction with Delivery Services
Satistaction was assessed by 14 satisfaction assessment questions on a five-point Likert scale (1=very dissatisfied, 2=dissatisfied, 3=neutral, 4=satisfied, 5=very satisfied). For the overall satisfaction level, those women who were satisfied in greater or equal to the mean score of the items were categorized under “satisfied” and those who were satisfied in less than the mean score of the items were categorized as “unsatisfied”.20
Having Companion
Having a support person for laboring women to provide support and stay with her during labor in the health facilities and was validated by a “yes or no” question. If the woman answered “yes” for the question, she was considered as having a companion.21
Maternal Condition After Delivery
The presence of at least one of the maternal morbidity conditions (hemorrhagic, hypertensive, uterine rupture, genital tract tear, and severe management—blood transfusion, hysterectomy) is considered as facing complication, otherwise considered as normal maternal condition after delivery.22,23
Advised About Postnatal Danger Signs
Advised if the women mention at least one maternal and or neonatal danger sign during the postpartum period, otherwise they were considered not advised about postnatal danger signs.
Data Collection Instrument and Procedure
Data were collected using a pretested and structured interviewer-administered standardized questionnaire, which was developed through reviewing various literature. Four BSc nurses who were not working in that health facility collected the data under the supervision of two final year MSc clinical midwifery students.
The immediate PNC satisfaction was measured by a tool adapted from JPSNQ presented by five-point Likert scales (1=dissatisfied, 2=satisfied, 3=minimally satisfied, 4=moderately satisfied, and 5=fully satisfied).18 The internal consistency of the tool of immediate PNC satisfaction was also checked in present study with (Cronbach’s alpha=0.987) and for the components of Jipi’s PNC assessment tool, it ranges from 0.908 and 0.974.
Data Quality Assurance
To ensure its consistency, the English version questionnaire was translated into the local language (Amharic version) and translated back to English version by language experts during analysis. Two days training was given to the data collectors and supervisors on the objective, the relevance of the study, and confidentiality of information, respondent’s rights, informed consent, and techniques of interview. A week before actual data collection, the questionnaire was pretested among postnatal mothers in Amanuel health center which has similar sociocultural and economic characteristics with the study population on 5% (n=20) of the total sample size, and necessary modification was done for the questionnaire according to the gaps which were identified. The supervisors made frequent checks on the data collection process to ensure the completeness and consistency of the gathered information and errors found during the process were corrected. The collected data were reviewed and checked for completeness before data entry. A data entry format template was produced and programmed on the Epi Data™ version 4.6.0.
Data Processing and Statistical Analysis
After data collection, filled questionnaires were coded, checked for consistency and completeness, and entered into Epi Data™ version 4.6.0 statistical software and then entered data were exported to Statistical Package for Social Sciences (SPSS) version 23 for further management and analysis. Before analysis, data cleaning and cross-checking were done. Both descriptive and analytical statistical procedures were performed. The descriptive analysis such as frequencies, percentages, means, and medians were computed.
Bivariable binary logistic regression analysis was used to assess the association of each independent variable with the level of immediate PNC satisfaction and variables with a P-value of <0.25 in the bivariable analysis were included in the multivariable logistic regression model for controlling confounders. The variables were entered into the multivariable binary logistic model using the backward variable selection method.
In multivariable binary logistic regression analysis, AORs with corresponding 95%CIs were calculated and statistical significance was declared at P-value <0.05. The model fitness was checked by Hosmer and Lemeshow goodness of fit test and it was a good fit and multicollinearity was checked by using variable inflation factor (VIF). Finally, the results were presented in the form of texts, tables, and graphs.
Ethical Considerations
Ethical approval was obtained from the Institutional Review Committee of School of Midwifery, College of Medicine and Health Sciences, University of Gondar with the reference number SMIDW/18/2013. An official letter of cooperation was written to respective health institutions from Debre Markos town health office. After a detailed explanation of the purpose, risks, and benefits of the study to the study participants, an informed verbal consent was taken from each study participant, because a total of 106 (27.20%) of the study participants had no formal education (illiterate). The informed verbal consent was approved by the Institutional Review Committee of School of Midwifery. To secure confidentiality and privacy of participants anonymity of patient information was implemented by avoiding personal identifiers, coding, locking the data, the data were not exposed to the third party and names were not recorded, and the interview was done in a private room. The study was also conducted in accordance with the Declaration of Helsinki.
For the prevention of COVID-19 pandemic transmission, data collectors and supervisors wore face masks, used hand sanitizers, and taught the mothers to apply COVID-19 prevention techniques while interviewing.
Results
Sociodemographic Characteristics
A total of 389 postnatal mothers were involved in the study with a response rate of 98.73%. The median age of the participants was 26 years (interquartile range, IQR=23–30) with a range of 18–40 years. A majority 327 (84.10%) of the study participants were in the age group of 20–34 years. A total of 282 (72.50%) of the participants were urban residents Table 1).
 |
Table 1 Sociodemographic Characteristics of Postnatal Mothers in Public Health Institutions of Debre Markos Town, northwest Ethiopia, 2021 |
Obstetric Characteristics of the Study Participant
More than half (54.80%) of the respondents were multiparous. Nearly one third (32.39%) faced obstetrics complications Table 2).
 |
Table 2 Obstetric Characteristics of Postnatal Mothers in Public Health Institutions of Debre Markos Town, northwest Ethiopia, 2021 |
Overall Level of Women Satisfaction with Immediate Postnatal Care
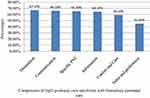
This study finding revealed that the level of women’s satisfaction with the immediate postnatal care was 60.90% with 95%CI (56.50–65.60). The study also showed that the majority of women (67.10%) were satisfied with orientation and 45% of women were satisfied by value and preferences components in Jipi’s nursing care satisfaction assessment framework Figure 3).
Factors Associated with Immediate Postnatal Care Satisfaction
Both bivariable and multivariable binary logistic regression analyses were computed. In bivariable binary logistic regression analysis, age of the mother, parity, ANC visits, friendly care, maternal educational level, advised about postnatal maternal danger signs, delivery care satisfaction, place of current delivery, mode of delivery, having companion, had a P-value <0.25 and were considered for multivariable binary logistic regression analysis to control the possible effects of confounders.
In multivariable analysis, multiparity (AOR=7.31, 95%CI: 4.40–12.17), four and more ANC visits (AOR=1.90, 95%CI: 1.08–3.36), satisfied by delivery care (AOR=2.05, 95%CI: 1.24–3.40), received friendly care (AOR=7.72, 95%CI: 2.42–13.52) and having companion (AOR=2.48, 95%CI: 1.37–4.50) were found to be significantly associated factors with immediate postnatal care satisfaction Table 3).
Discussion
This study assessed the level of immediate postnatal care satisfaction among women who give birth in public health institutions of Debre Markos town. It showed that the level of immediate PNC satisfaction was 60.90% (95%CI: 56.50–65.60).
This finding was in line with the studies done in Awi zone (63%)13 and West Shewa zone (55.8%)14 (Ethiopia), Czech (61%),24 and India (60%).25 The possible justification for this consistency of finding could be similarity in the characteristics of study population and study setting.
However, the study finding was lower when compared to studies conducted in UK (71.8%),26 Sweden (66%),27 Poland (68%),3 Nepal (78.6%),28 Saudi Arabia (79.4%),29 Ibadan (82.5%),30 and Ogun state, Nigeria (83%).31 The possible justification for this variation may be the clear difference in the health-care delivery system, timing of the survey, sociocultural differences in the study populations, and study population.
In contrast, this study finding was higher compared to studies done in Iran (52.60%),32 Nepal (45.10%),28 and Egypt (28.9%).33 This variation may be explained by the differences in the timing of the survey, the subjective nature of satisfaction, and the health institutions included in the study. During the immediate postnatal period, the view of women about their care may be overwhelmed by their happiness of having a baby and relief of pain7,34 and may be affected by the fact that women may not be feeling comfortable reporting a negative experience while still at the facility.35
In multivariable binary logistic regression analysis, multiparity, four and more ANC visits, satisfaction by delivery care, friendly care and having companion were statistically associated factors with the immediate PNC satisfaction. Multiparous women were 7.31 times more likely to be satisfied in immediate PNC compared with the primiparous women. This finding was consistent with studies done in Nepal28 and Malaysia.22 This may be explained by multiparous women who may reflect their expectations based on prior experiences compared to primiparous women. Conversely, primiparous women may have a higher expectation and perceive that transition to motherhood was fearful and they need more time to be with the health-care provider to get more information, support, care, and assistance with baby care, breastfeeding, and their postnatal care,33 which may lead them to be less satisfied with immediate PNC than multiparous women in immediate PNC.
Women who had four and above ANC follow-ups during their index pregnancy were 1.90 times more likely to be satisfied in immediate PNC when compared to the women who had less than four ANC follow-ups. The possible explanation for this finding could be attending more ANC follow-ups may help women to get more information about birth preparedness plans and complication readiness, to acquire more knowledge, and to develop a better attitude about maternal health services, which may lead them to be satisfied with immediate PNC. Thus, attending at least four regular ANC visits improves immediate PNC satisfaction.13
Delivery care satisfaction was found to be statistically significantly associated with the immediate postnatal care satisfaction. Women who were satisfied with delivery care services were 2.05 times more likely to be satisfied with immediate PNC than women who were not satisfied with delivery care services. This study finding was supported by the studies done in West Shewa, Ethiopia14 and Malaysia22 The possible explanation for this finding could be that satisfaction is influenced by previous experiences. Thus, a good experience contributes to building confidence and trust toward health services in general.22 Satisfaction during labor and delivery enhances a good perception and a positive attitude,36 which may affect women’s immediate postnatal care satisfaction. Once women are satisfied with their delivery care services, they become confident to take up all the challenges of motherhood in the immediate postpartum,37 which may lead them to be satisfied in immediate PNC.
In this study, women who received friendly care were 7.72 times more likely to be satisfied with immediate PNC than women who did not receive friendly care. This finding was in agreement with the studies done in Tigray, Ethiopia38 and Sweden.27 The possible justification for this finding could be if the women were treated with politeness, courtesy, and respect, their satisfaction level regarding the care they received became higher. In contrast to this, if the health-care providers give whatever qualified services to mothers without respecting mothers and being polite to them, they could never satisfy them.27
Another important factor in this study was having a companion during labor. Women who had a companion were 2.48 times more likely to be satisfied with immediate PNC than those who had no companion. This finding was supported by a study done in Tanzania.39 This could be explained by the presence of a companion makes women very happy, which may improve their labor, delivery, and immediate postpartum experiences and fill the gap when the health-care professionals were busy,39,40 which in turn may make them satisfied with the immediate PNC they received.
A limitation in the present study, due to the social desirability bias, study subjects might face difficulty in reporting dissatisfaction in the presence of data collectors, and this might overestimate the satisfaction level of immediate PNC. However, to minimize the bias the data were collected by BSc nurses who were working at another health facility in Debre Markos town, and the interview was done in a private room. Due to the cross-sectional nature of the study, temporal relations of cause-effect might not be inferred.
Conclusions
The result of this study showed that immediate PNC satisfaction was higher than national achievements of targets for the proportion of client satisfaction during their last health-care visit in the HSTP-I period which was 46%. Multiparous women, four and more ANC visits, satisfied in delivery care services, experienced friendly care, and had companions during labor were more likely to be satisfied with immediate PNC. Therefore, health-care providers and policy makers should encourage frequent ANC visits, give friendly care, and encourage companionship to increase the level of immediate PNC satisfaction.
Abbreviations
AOR, adjusted odds ratio; ANC, antenatal care; CS, cesarean section; CI, confidence interval; COR, crude odds ratio; DHS, demographic and health survey; ETB, Ethiopian birr; HSTP, health sector transformation plan; JPSNQ, Jipi’s postnatal satisfaction with nursing care questionnaire; PNC, postnatal care; SPSS, Statistical Package for Social Sciences; SVD, spontaneous vaginal delivery; UK, WHO, World Health Organization.
Data Sharing Statement
All relevant data are available from the corresponding author upon reasonable request.
Acknowledgments
The authors acknowledge the Mizan Aman College of Health Sciences for funding and respondents in Debre Markos town for providing data. We also would like to acknowledge data collectors and supervisors for accomplishing their tasks.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Funding was obtained from Mizan Aman College of Health Sciences.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Zulu MDC. Mothers’ Satisfaction with immediate postnatal care provided at Ndola Central Hospital, Zambia. Int J Nurs Stud. 2017;03(4):145–153.
2. World Health Organization. WHO technical consultation on postpartum and postnatal care. Geneva; [
3. Kowalewska B, Kamińska A, Rolka H, Ortman E, Krajewska–Kułak E. Satisfaction with obstetric care in the early postnatal period. Progress Health Sci. 2014;4(1):95–101.
4. Berhe A, Araya T, Tesfay K, et al. Assessment of quality of postnatal care services offered to mothers in hospitals, of Tigray Ethiopia 2016. Res Rev. 2017;6(1):11–19.
5. Jillian A, Al-Battawi SK. Evaluation of postnatal mother’s satisfaction with nursing care in El-Shatby Maternity University Hospital. IOSR J Nurs Healt Sci. 2017;6(6):69–80.
6. World health Organization. WHO recommendations on postnatal care of the mother and newborn; [
7. Matejić B, Milićević MŠ, Vasić V, Djikanović B. Maternal satisfaction with organized perinatal care in Serbian public hospitals. BMC Pregnancy Childbirth. 2014;14(1):1–9. doi:10.1186/1471-2393-14-14
8. Maha M, El Habashy AA, Hables RM, Safaa HM. Women satisfaction regarding utilization of post natal care in alexandria government. Int j Novel Res Healthc Nurs. 2020;7(3):625–635.
9. FMOH. Health sector transformation plan II 2020/21-2024/25 (2013 EFY - 2017 EFY). Addis Ababa, Ethiopia: FMOH; 2021.
10. Crecious MM, Lonia M, Patricia K-M, Margaret M. Postnatal care within six hours following delivery at two selected general hospitals of Zambia—mothers’ experiences. Open J Nurs. 2018;8(06):355. doi:10.4236/ojn.2018.86029
11. Enabudoso EI, Alphonsus R. Determinants of patient satisfaction after cesarean delivery at a university teaching hospital in Nigeria. Int J Gynecol Obstet. 2011;114(3):251–254. doi:10.1016/j.ijgo.2011.03.010
12. FMOH. National reproductive health strategy 2016–2020. Directorate MaCH, editor. Addis Ababa: FMOH; 2016.
13. Adane D, Wassihun B. Client satisfaction with existing postnatal care and associated factors: a study among mothers in Awi Zone, Amhara region, Ethiopia. Women’s Health. 2020;16:1745506520976017. doi:10.1177/1745506520976017
14. Ejara B. Assessment of mothers’ satisfaction on postnatal care given and its associated factors among mothers admitted to postnatal ward at public health centers and hospital setting west Shoa Zone, Oromia. Ethiopia: Addis Ababa University; 2014.
15. Srivastava A, Avan BI, Rajbangshi P, Bhattacharyya S. Determinants of women’s satisfaction with maternal health care: a review of literature from developing countries. BMC Pregnancy Childbirth. 2015;15(1):1–12. doi:10.1186/s12884-015-0525-0
16. Malouf RH, Henderson J, Alderdice F. Expectations and experiences of hospital postnatal care in the UK: a systematic review of quantitative and qualitative studies. BMJ Open. 2019;9(7):e022212. doi:10.1136/bmjopen-2018-022212
17. Agency CS. Population projection of Ethiopia for all regions at wereda level from 2014–2017. Addis Ababa; 2013.
18. Varghese J. Development of a new tool for evaluating postnatal mother’s satisfaction following nursing care: in India. Development. 2013;3(9):45.
19. Sheferaw ED, Mengesha TZ, Wase SB. Development of a tool to measure women’s perception of respectful maternity care in public health facilities. BMC Pregnancy Childbirth. 2016;16(1):67. doi:10.1186/s12884-016-0848-5
20. Dewana Z, Fikadu T, Abdulahi M. Client perspective assessment of women’s satisfaction towards labour and delivery care service in public health facilities at Arba Minch town and the surrounding district, Gamo Gofa zone, south Ethiopia. Reprod Health. 2016;13(1):11. doi:10.1186/s12978-016-0125-0
21. Beyene Getahun K, Ukke GG, Alemu BW. Utilization of companionship during delivery and associated factors among women who gave birth at Arba Minch town public health facilities, southern Ethiopia. PLoS One. 2020;15(10):e0240239. doi:10.1371/journal.pone.0240239
22. Imtithal Adnan F, Noor NM, Mat Junoh NA. Associated factors of labor satisfaction and predictor of postnatal satisfaction in the north-east of Peninsular Malaysia. PLoS One. 2020;15(8):e0238310. doi:10.1371/journal.pone.0238310
23. Bazant ES, Koenig MA. Women’s satisfaction with delivery care in Nairobi’s informal settlements. Int J Qual Health Care. 2009;21(2):79–86. doi:10.1093/intqhc/mzn058
24. Takács L, Seidlerová JM, Šulová L, Hoskovcová SH. Social psychological predictors of satisfaction with intrapartum and postpartum care–what matters to women in Czech maternity hospitals? Open Med. 2015;10(1). doi:10.1515/med-2015-0022
25. Varghese J, Rajagopal K. A study to evaluate the level of satisfaction perceived by postnatal mothers following nursing care in postnatal wards as expressed by themselves: pilot study. J Biol Agric Healthc. 2012;2(6):101–111.
26. McLellan J, Laidlaw A. Perceptions of postnatal care: factors associated with primiparous mothers perceptions of postnatal communication and care. BMC Pregnancy Childbirth. 2013;13(1):227. doi:10.1186/1471-2393-13-227
27. Hildingsson IM. New parents’ experiences of postnatal care in Sweden. Women Birth. 2007;20(3):105–113. doi:10.1016/j.wombi.2007.06.001
28. Regmi S, Kaphle HP, Gupta N. Maternal satisfaction regarding perinatal care and ınfluencing factors in tertiary hospitals of western, Nepal. Medicine. 2017;6(3):471–475.
29. Tehsin F, Mohammed AO, Lassoued L, Ali SI, al-Kishi AM. Parturient satisfaction with intrapartum and postpartum care in A maternity referral hospital at Al Ahsa, Saudi Arabia. J Soc Obstet Gynaecol Pak. 2018;8(3):169–175.
30. Ilesanmi RE, Akinmeye JA. Evaluation of the quality of postnatal care and mothers’ satisfaction at the university college hospital Ibadan, Nigeria; 2018.
31. Umahi EN, Atinge S, Agbede C, Muhammad KU. Knowledge, perception, and satisfaction of mothers regarding antenatal and postnatal care services in Ikenne Local Government Area, Ogun State. Niger Health J. 2020;19(2):70–84.
32. Mirzaei K, Oladi GS, Mousavi BM, Ziaee M. Mother’s satisfaction of postpartum care and its relationship with midwifery care at Urban Health Centers, Mashhad, Iran; 2016.
33. Mansour Lamadah S, El–Nagger N. Mothers’ satisfaction regarding quality of postpartum nursing care and discharge teaching plan at ain shams maternity and gynecological hospital. Int J Curr Res. 2014;6(7):7545–7551.
34. Waldenström U. Why do some women change their opinion about childbirth over time? Birth. 2004;31(2):102–107. doi:10.1111/j.0730-7659.2004.00287.x
35. Sando D, Ratcliffe H, McDonald K, et al. The prevalence of disrespect and abuse during facility-based childbirth in urban Tanzania. BMC Pregnancy Childbirth. 2016;16(1):1–10. doi:10.1186/s12884-016-1019-4
36. Dzomeku M. Maternal satisfaction with care during labour: a case study of the Mampong-Ashanti district hospital maternity unit in Ghana. Int J Nurs Midwifery. 2011;3(3):30–34.
37. Eti M, Sunitha C, Sarojamma C, Sai LM. Satisfaction and maternal postnatal adjustments following different modes of delivery. Int J Reprod Contracept Obstet Gynecol. 2020;9(2):640–646. doi:10.18203/2320-1770.ijrcog20200351
38. Fisseha G, Berhane Y, Worku A. Quality of intrapartum and newborn care in Tigray, Northern Ethiopia. BMC Pregnancy Childbirth. 2019;19(1):1–8. doi:10.1186/s12884-019-2184-z
39. Chaote P, Mwakatundu N, Dominico S, et al. Birth companionship in a government health system: a pilot study in Kigoma, Tanzania. BMC Pregnancy Childbirth. 2021;21(1):1–17. doi:10.1186/s12884-021-03746-0
40. World Health Organization. Companion of choice during labour and childbirth for improved quality of care: evidence-to-action brief; [
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.