Back to Journals » Therapeutics and Clinical Risk Management » Volume 15
Idiopathic pulmonary fibrosis and GERD: links and risks
Authors Ghisa M , Marinelli C , Savarino V , Savarino E
Received 8 May 2019
Accepted for publication 11 August 2019
Published 5 September 2019 Volume 2019:15 Pages 1081—1093
DOI https://doi.org/10.2147/TCRM.S184291
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Matteo Ghisa1, Carla Marinelli1, Vincenzo Savarino2, Edoardo Savarino1
1Gastrointestinal Unit, Department of Surgery, Oncology and Gastroenterology, University of Padua, Padua, Italy; 2Gastrointestinal Unit, Department of Internal Medicine and Medical Specialties, University of Genoa, Genoa, Italy
Correspondence: Edoardo Savarino
Gastrointerology Unit, Department of Surgery, Oncology and Gastroenterology, University of Padua, Via Giustiniani 2, Padova 351258, Italy
Tel +39 049 821 7749
Fax +39 049 876 0820
Email [email protected]
Abstract: Gastroesophageal reflux disease (GERD) and idiopathic pulmonary fibrosis (IPF) are two pathological conditions often strictly related, even if a clear relationship of causality has not been demonstrated. GERD is a frequent comorbidity in IPF patients, as demonstrated using combined multichannel intraluminal impedance-pH, despite being mostly clinically silent. According to that, it has been hypothesized that microaspiration of gastric material may play a fundamental role in the fibrotic transformation of pulmonary parenchyma. In contrast, it cannot be excluded that IPF may favor GERD by increasing the negative intrathoracic pressure. Therefore, this relationship is uncertain as well as not univocal. Nevertheless, the latest international guidelines recommend the use of proton pump inhibitors (PPIs) in IPF based on several data showing that PPIs can stabilize lung function, reduce disease flares and hospitalizations. On the contrary, recent studies not only question the relevance of these results, but also associate the use of PPIs with an increased risk of lung infections and a negative prognostic outcome. The aim of this review is to analyze the possible links between GERD and IPF and their possible therapeutic implications, trying to translate this scientific evidence into useful information for clinical practice.
Keywords: idiopathic pulmonary fibrosis, microaspiration, chronic cough, GERD, reflux disease, motility
Introduction
Pulmonary fibrosis
Idiopathic pulmonary fibrosis (IPF) is a chronic and progressive respiratory disease of unknown cause, limited to the lungs and affecting adults. It is associated with the radiological and/or histological pattern of “Usual Interstitial Pneumonia” (UIP) and is characterized by fibrotic alterations of the pulmonary interstitium.1 This leads to a progressive functional deficit, ending up to death, due to respiratory failure, on average within 3 years from diagnosis.
The incidence of the disease appears to be increasing in the last decades. It is more frequently diagnosed in the industrialized world, such as Northern America and Europe (up to 9 cases per 100,000 persons-year).1 It is a heterogeneous disease, with an unpredictable clinical course. While most of the patients have a stable clinical-functional course, part of them (10–15%) show rapid deterioration of lung function and high mortality.2
IPF is characterized by the deposition of fibrous tissue in the pulmonary interstitium, with not completely clear pathophysiological mechanisms. According to the latest evidence, IPF can be considered as the result of the interaction between genetic factors and tissue damage caused by various agents, such as smoking, some viruses, gastroesophageal reflux (GER) or environmental and occupational exposure to harmful substances. Also, epigenetic mutations are involved. In particular, the shortening of telomeres and cellular senescence causes genomic instability, reducing the response to repeated stimuli and resulting in fibrotic parenchymal damage.1 Clinically, the suspicion of the disease occurs in the presence of chronic cough and dyspnea, more often present for some years and initially labeled as heart failure or COPD. Spirometry and diffusing capacity of the lung for carbon monoxide (DLCO) should be performed in the suspicion of interstitial lung disease (ILD) and they may show a reduction of vital capacity, total lung capacity and DLCO.1 For the diagnosis, a high-resolution computed tomography (HRCT) is necessary, showing the typical pattern of UIP (i.e., honeycomb changes in the periphery and bases of the lungs). The investigation of other known causes of ILD (for e.g., pneumoconiosis, drug-induced ILDs, connective tissue disorders) is mandatory. If these are excluded, a diagnosis of IPF can be made. In case of typical patterns, lung biopsy may not be indicated. However, if performed, it shows heterogeneous paraseptal fibrosis with architectural distortion, defined as UIP.1
Gastroesophageal reflux disease
Gastroesophageal reflux disease (GERD) is a condition which develops when the reflux of the stomach contents causes troublesome symptoms and/or complications.3 It is one of the most prevalent conditions in Western Countries, with the highest rates reported from Europe (23.7%) and the US (28.8%).4 Mechanisms behind GERD have been summarized in Figure 1. Classical manifestations of GERD are heartburn and regurgitation defined as “esophageal syndrome” or “typical GERD”.3 In the last decades, it has been found that GER can involve other organs such as the lungs or the throat, determining a series of extra-esophageal symptoms so-called “atypical” (extraesophageal GERD, EE-GERD). According to Montreal Classification, among these extraesophageal manifestations, there are some with an established association such as chronic cough, laryngitis, asthma and dental erosions.3,5 However, for other conditions (such as pharyngitis, sinusitis, recurrent otitis media), the GER causal role has been only speculated. IPF belongs to the latter category.3,5
 |
Figure 1 Mechanisms behind GERD. The imbalance between triggering and defensive factors causes GERD.6–13 Abbreviations: GERD, gastroesophageal reflux disease; GER, gastroesophageal reflux. |
In clinical practice, in order to make a certain diagnosis of GERD, a typical symptomatic pattern must be associated with response to proton pump inhibitors (PPIs) or endoscopic finding of reflux esophagitis. After exclusion of other causes, also in case of EE symptoms, the response to PPIs is used to define if the symptom in question is GERD-related or not. Nevertheless, particularly in case of EE symptoms, lack of response to PPIs does not exclude GER as a causative agent, particularly considering the existence of weakly acidic and biliary reflux.14 Thus, reflux monitoring by means of pH-metry, Bravo pH capsule or 24-hr multichannel impedance-pH monitoring (MII-pH) is suggested to determine the amount of refluxate, its proximal extent and/or the presence of both acid and weakly acidic reflux.15–20 To reach a diagnosis of GERD according to the latter technology (i.e., MII-pH), the first element to analyze is the total number of refluxes (i.e., normal when lower than 40/24 hrs, considered normal, pathological when higher than 80/24 hrs) and, the esophageal acid exposure time (AET) as the percentage of time with pH <4.0 in the distal esophagus.17 Symptom index scoreand symptom association probability (SAP) represent two scores elaborated in order to temporally correlate symptoms to GER. For a positive association, they have to occur within 2 mins from the reflux episodes.21–23 The use of these parameters is well established in typical GERD, whereas in atypical GERD represents a matter of debate. Only in the last years researchers have started to use MII-pH evaluation to correlate GERD with EE manifestations and putative extraesophageal associations like IPF. However, some studies showed that the accuracy of MII-pH, unfortunately, decreases. For example, considering the ability to predict the effectiveness of anti-reflux surgery on EE symptom resolution, co-presence of typical GERD is more effective than a positive MII-pH.24 Also, the application of SI and SAP for EE esophageal symptoms is challenging. Considering dental erosions or laryngitis, the calculation of these scores is not possible. In the same way, the relationship between GERD and asthma attacks cannot be routinely evaluated during a 24-hr monitoring. Moreover, both indexes are hampered by intrinsic limitations (i.e., day-to-day variability of reflux occurrence and therefore limited probability to associate it with symptoms, lack or uncorrect symptom reporting during the testing day, etc.), which finally questioned their adoption in clinical practice.
Relationship between GERD and IPF
General and epidemiological consideration
Despite IPF is labeled as idiopathic, several factors play a role in its pathogenesis. Previous studies have shown that GERD is more common in patients with IPF than in general population.25,26 Similarly, in a study of over 100,000 people with erosive esophagitis, the prevalence of pulmonary fibrosis was significantly higher than in healthy controls.27 Also, the incidence of newly diagnosed GERD is continuously increasing in IPF patients.28 Moreover, the evidence of hiatal hernia at thorax-CT scan appears to be more frequent in these patients, compared to both healthy controls and patients with other respiratory problems, such as COPD or asthma.29 However, evidences are not all in agreement. Although apparently the two pathologies seemed to be associated in 18 case-control studies, a subsequent meta-regression analysis controlling for smoking revealed no correlation between GERD and IPF.30 Possible biases, not constantly ruled out, are the presence of risk factors and comorbidities, such as aging and male gender.31 Further studies are required to evaluate the impact of common comorbidities and risk factors both on IPF and GERD, beyond their epidemiological association.
Pathophysiological mechanisms and biological rationale of the relationship
Despite epidemiological data seem to be significant, many pathophysiological aspects are still uncertain. The strict interactions between the two entities are depicted in Figure 2.
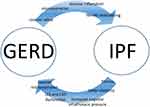 |
Figure 2 Mutual mechanisms behind GERD and IPF.Abbreviations: GERD, gastroesophageal reflux disease; IPF, idiopathic pulmonary fibrosis. |
On the one hand, chronic microaspiration may lead to fibrotic remodeling of the pulmonary parenchyma; on the other hand, lower pulmonary elasticity increases negative intrathoracic pressure. This latter event could favor GER by decreasing the pressure of the upper esophageal sphincter, thus predisposing to multiple episodes of micro-aspiration that determine/aggravate the course of the lung disease.
Beyond the epidemiological data, evidences from cell culture and animal models make this relationship stronger.32 Studies in mice have shown how the presence of gastric content in lungs can induce pulmonary fibrosis. Histologically, it results in thickening of the alveolar walls, deposition of collagen at the interstitial level, epithelial-mesenchymal transition and expression of fibrogenic factors, such as TGF-beta, NFκB and Farnesoid X receptor.32–35 Both acidic reflux and bile acids might contribute to induce TGF-beta production and fibroblast proliferation in cultured tissue.36 Also in humans, several studies confirm that pepsin and acid are frequently present in the bronchoalveolar lavage fluid (BALF) of patients with IPF,37–40 thus influencing fibroproliferative response in lungs parenchyma.38,41,42 In particular, children with GERD have more frequently pepsin in tracheal fluid than healthy controls, particularly when both GERD and respiratory problems are present, as confirmed in pediatric patients with cough and proximal reflux.43,44 Moreover, pepsin is not found in tracheal fluid of children without GERD.45 Other studies evaluated the presence of GERD in patients undergoing or who have already undergone lungs transplantation. Davis et al analyzed BALF in 100 patients after lung transplantation for chronic lung diseases (including IPF). BALF pepsin levels were higher in IPF patients than in other end-stage pulmonary disease.39 Furthermore, it has been demonstrated a lower pH in peripheral branches of bronchi (p<0.001) and higher inflammatory markers (like lactate dehydrogenase and C-reactive protein and TNF-alfa) in BALF of IPF patients compared to GERD population.46 Interesting data come from a report of 32 cases of asymmetric IPF cases (asymmetry was defined by quantitative HRCT fibrosis score). GERD was increased in patients with asymmetric IPF compared to those with symmetric IPF (63% vs 31%, p=0.009). Patients with asymmetric IPF usually reported sleeping on the more affected side.32
A completely different hypothesis suggests that the presence of Helicobacter pylori (H. pylori) in the reflux may induce pulmonary fibrosis by determining parenchymal inflammatory changes. In one study, H. pylori seroprevalence correlated with a more severe functional impairment in patients with IPF, but other studies failed to identify H. pylori DNA in lung biopsies from patients with IPF.42 In contrast with these conflicting considerations, a negative association between the prevalence of H. pylori and the severity of GERD, including Barrett’s esophagus, has been demonstrated in epidemiological studies and moreover, eradication therapy was related to a higher risk of developing de novo GERD in Asian studies. These considerations make H. pylori–IPF putative relationship even more controversial.47
On the other hand, it is known that respiratory disease can determine or exacerbate GER. Altered respiratory movements, cough and low lung compliance can enhance trans-diaphragmatic pressure gradient during respiration inducing esophagogastric junction (EGJ) dysfunction and, subsequently, microaspiration.48 Reduced pulmonary compliance could determine distortion of mediastinal structures and traction on the esophagus, causing weakening of lower esophageal sphincter (LES).42 Low pulmonary volumes in ILD-like IPF can explain an anatomical disruption of EGJ with a loss of overlap between LES and CD, thus explaining an increased prevalence of hiatal hernia in these patients.48 IPF lung parenchyma is stiffer and less compliant, determining greater negative inspiratory pressures to expand itself. GER is indeed eased, especially during transient lower esophageal sphincter relaxation (TLESR)R, for a higher gastro-esophageal pressure gradient that causes greater negative intrathoracic pressures during inspiration, probably due to poor lung compliance. Moreover, values of inspiratory thoracic pressures inversely correlate with the number of proximal refluxes in esophagus.48 All these speculations support the hypothesis that GERD is a factor involved in the natural history of IPF.
Clinical presentation of GERD in IPF patients
In IPF patients, GERD is usually clinically silent.25,49 Heartburn prevalence is significantly lower in IPF-GERD population than in GERD (59 vs 84%, p=0.028).50 Typical GERD has low sensitivity (65%) and specificity (71%) compared to 24-hr pH monitoring for diagnosing GERD,42 and then it seems to be unable to identify GERD in IPF patients. Anyway, the Hull Airway Reflux Questionnaire (HARQ) has been validated to identify GERD in these patients. A prospective cross-sectional study including 40 patients reported that 68% of IPF patients had pathological HARQ scores than healthy controls.51 Gao et al obtained the same results in a study evaluating 69 patients with IPF, in whom GERD prevalence was 62.3% and typical symptoms were present only in 58.1% of them.52 For these reasons, symptoms did not reliably predict the presence of GERD, subsequently confirmed by pH-metry reporting acid reflux.53 In another study, pH-metry-assessed GER prevalence in IPF patients was significantly increased (87–94%) compared with both the general population (10–19%) and patients suffering from other chronic pneumopathies, such as asthma (58–69%), cystic fibrosis (35–81%) and COPD (19–28%).54
Briefly, severity and frequency of reflux episodes can modify the course of the disease and trigger IPF exacerbation. To confirm this, pepsin concentrations in BALF positively correlate with the frequency of exacerbations,36 even though a small cohort study did not show any difference in the rate of clinical exacerbations between GERD and non-GERD IPF patients.36 Otherwise, it could also occur the opposite, i.e., that during clinical exacerbations the alteration of respiratory dynamics and the increased chest negative pressure exacerbate GER. However, there is currently no evidence correlating the severity of IPF with that of GER.42
Esophageal manometric findings in IPF
Considering manometric alterations, LES pressure was normal in most studies, while an increased number/duration of TLESRs has been found supporting the role of GER in IPF pathogenesis. On the contrary, the upper esophageal sphincter (UES) pressure is often reduced and this might be associated with an increased risk of aspiration. Few studies showed that IPF patients had a significantly lower mean basal LES pressure than healthy controls (14.1 mmHg vs 22 mmHg, p=0.001).42 Besides, Gao et al showed that IPF patients had significantly decreased LES and UES pressure, compared with healthy volunteers.52 Manometric patterns of esophageal body peristalsis were mostly normal, although some studies observed increased frequency of ineffective peristalsis.55,56 Finally, a recent meta-analysis confirmed a higher prevalence of GERD and⁄or esophageal dysmotility in ILD compared with controls.57
Esophageal impedance-pH monitoring in IPF
Esophageal pH-metry and impedance-pH analysis represent a key element in the evaluation of the presence and characteristics of GER in IPF patients. Since the early 1990s, pulmonary symptoms (cough, dizziness, history of pneumonia) have been related to GER due to the introduction of the pH-metry measurement also at the level of the proximal esophagus. A lot of evidences showed that from one-third up to two-thirds of IPF patients have frequent proximal reflux and then abnormal proximal esophageal acid exposure.25,50,53,58 In a study of 65 consecutive IPF patients with 24-hr pH monitoring, the overall prevalence of pathological reflux was 87%, and 53% of these patients were completely asymptomatic.25 In another study among IPF patients, 67–76% of them had abnormal AET at pH-metry, performed off-PPI treatment.57 A recent meta-analysis did not show a causal link or a clear relationship between the severity of GERD and gravity of fibrosis.30 Similarly, data are inconclusive regarding outcome studies evaluating anti-reflux treatments in patients with IPF.57 A study published in 2014 evaluating 28 IPF patients with 24 hrs hypopharyngeal multichannel intraluminal impedance showed that 15 patients had abnormal proximal reflux exposure with 25% of them of non-acidic nature. In these patients, an abnormal rate of esophageal mucosal injury, a longer acid clearance and a high number of reflux events were reported.59 Another study by Borges et al demonstrated that patients with increased bolus exposure time (BET) had a 1-year poor pulmonary outcome (hospitalization for respiratory exacerbation or death) compared with those with normal BET (45.7% vs 15.2%, p=0.006). Moreover, this higher BET was predictive for an early onset of poor pulmonary outcome (hazard ratio 4.88; p=0.007).60
Other studies investigated reflux patterns of IPF patients using MII-pH, confirming that non-acidic refluxate also occurs and that it may be involved in the pathogenesis of IPF.38,61,62 For instance, Savarino et al compared IPF patients with non-IPF pulmonary fibrosis and healthy volunteers and found that in IPF population there was a significantly higher (p<0.01) AET as well as a greater number of weakly acidic and proximal reflux events compared to both controls. Pulmonary fibrosis HRCT scores were significantly correlated with reflux episodes in both distal and proximal esophagus. Patients with IPF had more bile acids and pepsin (p<0.03) in BALF (62% and 67%, respectively) and saliva (61% and 68%, respectively) than non-IPF patients (25% and 25% in BALF, and 33% and 36%, respectively, in saliva) and healthy controls (0% and 0% in BALF and saliva, respectively.38 Microaspiration has also been studied as a pathogenic factor of pulmonary fibrosis in patients with scleroderma (SSc) by Savarino et al, as lungs and gastrointestinal tract are the most frequently involved internal organs in this disease.63 The comparison of SSc patients with and without pulmonary fibrosis showed that the former had higher esophageal acid exposure, greater number of both acid and non-acidic reflux episodes and major number of proximal refluxes than the latter group (p<0.01). Moreover, the number of reflux episodes in both distal and proximal esophagus was significantly correlated with HRCT scores of PF and this confirms that patients with pulmonary involvement have more severe reflux.63 Another study was carried out in patients awaiting for lung transplantation because of an end-stage pulmonary disease.64 Typical symptoms of GERD had low sensitivity (67%) and specificity (26%), and they could not distinguish between patients with and without abnormal reflux, having positive predictive and negative predictive values of 64% and 28%, respectively.64 Compared with COPD patients, IPF subjects had greater reflux episodes and increased bolus reflux exposure time on MII-pH. Moreover, a high proportion of them had an increase of non-acid reflux.61 More recently, Gavini et al assessed the correlation between MII-pH parameters and pulmonary function scores and found that both the number of total reflux episodes (OR=4.70 p=0.04) and the prolonged bolus clearance (OR=1,21 p=0.05), but not the refluxate pH values, were significantly associated with the severity of pulmonary dysfunction.62 A study of patients who underwent lung transplantation showed that a pre-operative abnormal proximal acid reflux evaluated by MII-pH testing was associated with early hospital readmission after lung transplantation.65
Role of proton pump inhibitors
General considerations on PPI use in IPF
Last few years have seen a growing interest in the research of new therapeutic strategies in IPF. Remarkable advances have been made with the introduction of nintedanib and pirfenidone, two approved antifibrotic medications. Despite these advances, however, no significant changes in the natural history of the disease have been obtained. Probably this is due to the lack of knowledge of the real pathophysiological mechanisms of the disease and the absence of a real target/process to treat. All treatments explicate their action in the latest steps of the pathogenetic process and therefore they are not able to be decisive.
Pathophysiological background of PPI use in IPF
Starting with the hypothesis that GER plays an important role in the natural history of IPF, the latest guidelines on IPF management suggest a conditional indication in favor of PPI use. An increasing number of studies show that PPIs are able to stabilize lung function, reduce hospitalizations for respiratory problems and episodes of exacerbation and can have a positive prognostic role in terms of increased survival.25,28,66 Until few years ago, the supposed mechanism of action of these drugs was thought to be linked only to acid suppression. Last evidences seem to indicate a role of PPIs in the modulation of multiple systemic processes, including inhibition of pro-inflammatory and tissue remodeling mechanisms.54 In addition to systemic effects, they have also local effects, such as the reduction of apoptosis of pneumocytes expressing SP-C (surfactant).41
Evidences from in vitro and in vivo studies
Evidences from in vitro studies showed that PPIs can regulate the oxidant–antioxidant balance.54 Primary lung fibroblasts, endothelial and epithelial cells cultures, exposed to ionizing radiation, showed lower expression of matrix metalloproteinase enzymes, inflammatory cytokines and adhesion molecules when in presence of esomeprazole. This macromolecule is also able to inhibit, in a dose-depend way, the proliferation of lung fibroblasts.41 Moreover, in rat models of bleomycin-induced lung injury, esomeprazole has positive effects in reducing both inflammatory and fibrotic responses. This suggests that PPIs have pleiotropic effects.54
Evidences in human studies
The role of PPIs in influencing the natural course of IPF has been investigated in retrospective and prospective studies (Table 1). First evidences, in small case series, showed stabilization of functional lung capacity (FVC and DLCO) in IPF patients affected by GERD and treated with antisecretory therapy.29,67 These medications have also a positive action on transplant-free survival of patients with GERD/IPF by inducing a slower decline in FVC and a reduction of acute exacerbation events. Most patients in these studies were on PPIs (85%) compared with H2RAs.41,49,68 Moreover, some studies showed a significant reduction of the frequency of disease exacerbations and in pulmonary-related mortality.28,68,69 On the other hand, in 2016, data from a post hoc analysis study from three placebo-controlled trials of pirfenidone (CAPACITY 004, CAPACITY 006 and ASCEND) showed that there was no difference in disease progression, IPF-related mortality and hospital admission in patients treated or not with PPIs.70 Moreover, a post hoc analysis in patients treated with nintedanib (INPULSIS) showed that acute exacerbations occurred in a higher proportion of those patients who were on antisecretory medications (PPIs or H2RAs) than in those not taking this therapy.71 Several studies explained how PPIs are able to increase pH of gastric juice, but anyway unable to suppress other components of the refluxate, like pepsin and bile salts and to modulate the volume of gastric secretion in toto.17 Accordingly, PPI use may negatively influence disease course due to a higher intra-gastric pH and, consequently, an increased risk of infective respiratory events. In keeping with this consideration, pneumonia occur more frequently in IPF patients receiving PPIs compared with those who were not treated with them.71
 |
Table 1 Data from studies investigating the role of PPIs or antireflux surgery in IPF |
Role of surgery
The role of anti-reflux surgery in controlling reflux events and preventing micro-aspiration has also been studied in IPF patients (Table 1). First evidences derive from a case series presented by Raghu et al in 2006, in which antireflux surgery for treating GERD induced the stabilization of pulmonary function.67 Data from patients in waiting list for lung transplantation demonstrated stabilization in oxygen needs and improvement in the FVC.72,73 Laparoscopic anti-reflux surgery (LARS) efficacy in preventing GER in lung transplanted patients was evaluated by dosing the presence of pepsin in BALF. Transplant recipients undergoing LARS had significantly lower pepsin levels than unoperated patients. The absence of pepsin in BALF of GERD-free controls got these data stronger. Moreover, high pepsin levels correlated with a quicker progression to bronchiolitis obliterans syndrome (BOS) and more acute rejection episodes.74
The hypotheses for explaining the high rate prevalence of GERD after transplantation involve the secondary disruption of protective mechanisms against reflux and aspiration, like mucociliary clearance and cough reflexes, and the negative effects of immunosuppressant drugs, like tacrolimus and cyclosporine, on gastrointestinal motility.74 A pulmonary functional evaluation after LARS showed improvement of FEV1 and lower rate of onset of BOS.75 Moreover, Patti et al confirmed the safety of this surgery due to its ability to significantly reduce GERD-related damage on allograft injury.76 On the contrary, a multicenter, randomized, controlled Phase II trial (WRAP-IPF), in which patients with IPF and GERD and concomitant therapy with nintedanib and pirfenidone were randomized to undergo LARS or medical treatment, did not show any difference of FVC between those treated and untreated with LARS. However, acute exacerbation, respiratory-related hospitalization and death were less common in patients who underwent LARS, but the result was not statistically significant.77 New prospective and adequate powered studies are mandatory in order to enhance the significance of these results.
Discussion
The proposal of a possible etiologic role of reflux in pulmonary fibrosis has been advanced on the basis of the results of epidemiological studies and the high frequency of objectively demonstrated GERD in the IPF population. Furthermore, patients with erosive esophagitis present more frequently pulmonary fibrosis. From a clinical point of view, reflux is frequently asymptomatic, and a diagnosis based on typical symptoms is often not accurate.
The first doubt to work out is whether GERD is really the cause of IPF or a simple consequence, probably due to a decreased pulmonary compliance during respiratory acts secondary to fibrosis. Manometric study of esophageal motor function in IPF patients did not show particular patterns of body dysmotility, with only few studies showing a higher frequency of ineffective peristalsis.55,56 Regarding the two esophageal sphincters, LES has almost always a normal tone, while UES is more frequently hypotonic.50
Until now, various studies used different criteria for the diagnosis of GERD, but its prevalence can be really estimated only by means of MII-pH. Impedance studies showed that refluxes can frequently reach the proximal esophagus, explaining how this can subsequently involve the pulmonary tree. This proximal extension of GER is often coupled with a slower acid clearance. Another aspect issued from MII-pH analysis, but not fully clarified, is the possible role of non-acid reflux and other components such as pepsin and biliary salts, repeatedly found in the BALF of patients with IPF and GER. These elements are present only in patients with GERD detected by means of objective measurements and could play an important role in the pathogenesis of IPF.
From a therapeutic point of view, the role of PPIs in GERD was studied particularly in the last decade. The latest international guidelines for IPF, updated in 2015, recommended antisecretory therapy in these patients. Several studies have shown that PPIs can be of help in improving lung function, reducing the decline of pulmonary functional tests, diminishing the rate of exacerbation of the disease and improving the disease prognosis. Another important aspect of these drugs is their safety because of their rare adverse events78 and the low cost of therapy. These evidences, unfortunately, are mostly of low quality, based on observational and retrospective studies. Even more, some of the latest publications questioned the fragile recommendation of PPIs in IPF. PPIs not only do not improve pulmonary function, but also may increase the risk of lung infections in those patients who have advanced disease.1 Studies have shown that PPIs are able to increase gastric pH, but do not affect weakly alkaline reflux or other components of the refluxate. These substances have already been assessed in IPF, but their role is still unclear. However, there is the possibility that PPIs may play a role in IPF beyond controlling GER pH itself or micro-aspiration. An alternative and biologically plausible mechanism involves the downregulation of fibroinflammatory molecules, the inhibition of fibroblast proliferation and the upregulation of cytoprotective mechanisms.
Surgery represents the other way of treatment of GERD in IPF. LARS is almost always safe and, in selected patients, represents a good therapeutic option. Unfortunately, latest evidences do not seem to confirm a better patients’ outcome when surgery is used in the management of IPF-GERD.77
Unfortunately, more questions than answers emerge from international medical literature about the relationship between GERD and IPF and a great research work needs to be done in this field.
Five years of prospective view
Taking into account the increase of IPF incidence, an early intervention is mandatory for a better management of the disease. From a therapeutic point of view, great expectation is conferred to new antifibrotic medications, which are used in ongoing clinical trials. About GERD-IPF relationship, the Lyon consensus clarifies that esophageal MII-pH is the current gold standard for the diagnosis of GERD and the classic parameters, such as AET and the number of refluxes, detected by the traditional pH-metry, are no more sufficient to distinguish normal from abnormal reflux patterns, especially in EE-manifestations. In clinical practice, there is a “gray area” including unclear physiological conditions and, in these cases, some recently developed parameters, like post-reflux swallow-induced peristaltic wave (PSPW) index and mean nocturnal baseline impedance (MNBI), can be of help in discriminating normal from abnormal findings.79–83 Further studies should be carried out to assess the usefulness of these novel two parameters in GERD patients with pulmonary problems. Two abstracts were recently presented at DDW 2017 by Borges et al, showing the correlation between MNBI and PSPW values and changes in pulmonary function testing parameters over 1 year in IPF patient. Low proximal and distal MNBI were positively correlated with 1-year decline in FEV1 (r=0.50, p=0.03) and FVC. The authors concluded that low distal and proximal MNBI and also an abnormal PSPW are predictors of more severe decline in lung function over 1 year on pulmonary function tests among pre-lung transplant IPF patients.84,85
In addition to PSPW and MNBI, mucosal integrity Testing can represent a promising approach to detect esophageal epithelial changes as previously demonstrated.86
Another tool emerging in the field of esophageal pathophysiology is functional lumen imaging probe (FLIP), and its endoscopic subtype EndoFLIP (Crospon Ltd, Galway, Ireland), for the mechanical properties assessing of the esophageal wall and both LES and UES compliance.87 Another possible application of EndoFLIP could be the identification of those patients presenting EGJ dysfunction that could have benefit from surgery.
All these new diagnostic tools, in addition to a more diffuse and frequent use of MII-pH, should improve our ability to establish a more accurate cause-effect relationship between IPF and GERD and to assess the real effectiveness of both medical and surgical anti-reflux therapies.
Conclusion
The hypothesis of GERD as prominent etiological factor of IPF and, moreover, the idea that its treatment, either medical or surgical, may slow disease progression and improve patients’ survival are extremely intriguing issues. We know that GERD is frequently asymptomatic and typical symptoms often do not allow us to make a certain diagnosis in IPF patients. For this reason, despite the above-mentioned limitations, all IPF patients should be screened for GERD by pathophysiological studies, mainly using HRM and MII-pH. Also, bronchoscopy with analysis of BALF by dosing pepsin and/or bile acids could increase the diagnostic accuracy. Furthermore, the efficacy of PPI therapy should be evaluated in prospective and randomized clinical trials aimed to assess lung function parameters and clinical response of respiratory symptoms and to improve esophageal pH and impedance values. Anti-reflux surgery, particularly LARS, appears to be an effective and safe option for these patients. Similarly, in patients waiting for or who have undergone lung transplantation, a careful evaluation of GER and its adequate management (both medical or surgical) can reduce the appearance of BOS and change the clinical course of the disease.
In conclusion, all this uncertainty about GER-IPF relationship and, consequently, about its therapeutic management, is due to the scant knowledge of the real pathogenic mechanisms of the pulmonary damage in IPF. Unfortunately, IPF is still an idiopathic condition, as its name suggests, despite our research and clinical efforts. Several questions need to be addressed, particularly in relation to the role of micro-aspiration in lung injury, remodeling and progression to IPF. Pathophysiological studies of the esophagus with HRM and MII-pH are therefore suggested in order to strengthen the value of previous data and, in clinical practice, to detect safely IPF patients with GERD and define better those who can benefit from PPI therapy or anti-reflux surgery. Moreover, there is a prominent need for high-quality, randomized, controlled clinical studies in order to prospectively evaluate the efficacy and safety of both PPIs and anti-reflux surgery in the treatment of IPF, also taking into account that all the new anti-fibrotic and immune-suppressive therapies have relevant limitations.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclosure
Edoardo Savarino received lecture and consultancy honoraria from Takeda, Janssen, MSD, Abbvie, Sofar, Malesci, Reckitt Benckiser, and Medtronic. Matteo Ghisa, Carla Marinelli, and Vincenzo Savarino had no conflicts of interests to report in this work.
References
1. Lederer DJ, Martinez FJ. Idiopathic pulmonary fibrosis. Longo DL, ed. N Engl J Med. 2018;378(19):1811–1823. doi:10.1056/NEJMra1705751
2. Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. doi:10.1164/rccm.2009-040GL
3. Vakil N, Van Zanten SV, Kahrilas P, Dent J, Jones R. The montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus CME. Am J Gastroenterol. 2006;101:1900–1920. doi:10.1111/j.1572-0241.2006.00630.x
4. Ronkainen J, Agréus L. Epidemiology of reflux symptoms and GORD. Best Pract Res Clin Gastroenterol. 2013;27(3):325–337. doi:10.1016/j.bpg.2013.06.008
5. de Bortoli N, Nacci A, Savarino E, et al. How many cases of laryngopharyngeal reflux suspected by laryngoscopy are gastroesophageal reflux disease-related? World J Gastroenterol. 2012;18(32):4363. doi:10.3748/wjg.v18.i32.4363
6. Boeckxstaens G, El-Serag HB, Smout AJPM, Kahrilas PJ. Symptomatic reflux disease: the present, the past and the future. Gut. 2014;63(7):1185–1193. doi:10.1136/gutjnl-2013-306393
7. Roman S, Holloway R, Keller J, et al. Validation of criteria for the definition of transient lower esophageal sphincter relaxations using high-resolution manometry. Neurogastroenterology Motil. 2017;29(2):e12920. doi:10.1111/nmo.12920
8. Scarpellini E, Boecxstaens V, Broers C, Vos R, Pauwels A, Tack J. Effect of baclofen on gastric acid pocket in subjects with gastroesophageal reflux disease symptoms. Dis Esophagus. 2016;29(8):1054–1063. doi:10.1111/dote.12443
9. Mello M, Gyawali CP. Esophageal manometry in gastroesophageal reflux disease. Gastroenterol Clin North Am. 2014;43(1):69–87. doi:10.1016/j.gtc.2013.11.005
10. Savarino E, Giacchino M, Savarino V. Dysmotility and reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2013;21(6):1. doi:10.1097/MOO.0b013e3283658edf
11. Tolone S, De Bortoli N, Marabotto E, et al. Esophagogastric junction contractility for clinical assessment in patients with GERD: a real added value? Neurogastroenterology Motil. 2015;27(10):1423–1431. doi:10.1111/nmo.12638
12. Tolone S, de Cassan C, de Bortoli N, et al. Esophagogastric junction morphology is associated with a positive impedance-pH monitoring in patients with GERD. Neurogastroenterology Motil. 2015;27(8):1175–1182. doi:10.1111/nmo.12606
13. Tolone S, Savarino E, Zaninotto G, et al. High-resolution manometry is superior to endoscopy and radiology in assessing and grading sliding hiatal hernia: a comparison with surgical in vivo evaluation. United Eur Gastroenterol J. 2018;6(7):981–989. doi:10.1177/2050640618769160
14. Ribolsi M, Savarino E, De Bortoli N, et al. Reflux pattern and role of impedance-pH variables in predicting PPI response in patients with suspected GERD-related chronic cough. Aliment Pharmacol Ther. 2014;40(8):966–973. doi:10.1111/apt.12919
15. Savarino E, Bredenoord AJ, Fox M, Pandolfino JE, Roman S, Gyawali CP. Expert consensus document: advances in the physiological assessment and diagnosis of GERD. Nat Rev Gastroenterol Hepatol. 2017;14(11):665–676. doi:10.1038/nrgastro.2017.130
16. Roman S, Gyawali CP, Savarino E, et al. Ambulatory reflux monitoring for diagnosis of gastro-esophageal reflux disease: update of the porto consensus and recommendations from an international consensus group. Neurogastroenterol Motil. 2017;29(10):1–15. doi:10.1111/nmo.13067
17. Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67(7):1351–1362. doi:10.1136/gutjnl-2017-314722
18. Zentilin P, Dulbecco P, Savarino E, Giannini E, Savarino V. Combined multichannel intraluminal impedance and pH-metry: a novel technique to improve detection of gastro-oesophageal reflux. Dig Liver Dis. 2004;36(9):565–569. doi:10.1016/j.dld.2004.03.019
19. Savarino E, Zentilin P, Frazzoni M, et al. Characteristics of gastro-esophageal reflux episodes in Barrett’s esophagus, erosive esophagitis and healthy volunteers. Neurogastroenterology Motil. 2010;22(10):1061–e280. doi:10.1111/j.1365-2982.2010.01536.x
20. Savarino E, Zentilin P, Savarino V. NERD: an umbrella term including heterogeneous subpopulations. Nat Rev Gastroenterol Hepatol. 2013;10(6):371–380. doi:10.1038/nrgastro.2013.50
21. Savarino E, Tutuian R, Zentilin P, et al. Characteristics of reflux episodes and symptom association in patients with Erosive Esophagitis and nonerosive reflux disease: study using combined impedance–pH off therapy. Am J Gastroenterol. 2010;105(5):1053–1061. doi:10.1038/ajg.2009.670
22. Savarino E, Zentilin P, Tutuian R, et al. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103(11):2685–2693. doi:10.1111/j.1572-0241.2008.02119.x
23. Savarino E, Marabotto E, Zentilin P, et al. The added value of impedance-pH monitoring to Rome III criteria in distinguishing functional heartburn from non-erosive reflux disease. Dig Liver Dis. 2011;43(7):542–547. doi:10.1016/j.dld.2011.01.016
24. Francis DO, Goutte M, Slaughter JC, et al. Traditional reflux parameters and not impedance monitoring predict outcome after fundoplication in extraesophageal reflux. Laryngoscope. 2011;121(9):
25. Raghu G, Freudenberger TD, Yang S, et al. High prevalence of abnormal acid gastro-oesophageal reflux in idiopathic pulmonary fibrosis. Eur Respir J. 2006;27(1):136–142. doi:10.1183/09031936.06.00037005
26. Raghu G, Amatto VC, Behr J, Stowasser S. Comorbidities in idiopathic pulmonary fibrosis patients: a systematic literature review. Eur Respir J. 2015;46(4):1113–1130. doi:10.1183/13993003.02316-2014
27. el-Serag HB, Sonnenberg A. Comorbid occurrence of laryngeal or pulmonary disease with esophagitis in United States military veterans. Gastroenterology. 1997;113(3):755–760. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9287965.
28. Lee CM, Lee DH, Ahn BK, et al. Protective effect of proton pump inhibitor for survival in patients with gastroesophageal reflux disease and idiopathic pulmonary fibrosis. J Neurogastroenterol Motil. 2016;22(3):444–451. doi:10.5056/jnm15192
29. Noth I, Zangan SM, Soares RV, et al. Prevalence of hiatal hernia by blinded multidetector CT in patients with idiopathic pulmonary fibrosis. Eur Respir J. 2012;39(2):344–351. doi:10.1183/09031936.00099910
30. Bédard Méthot D, Leblanc É, Lacasse Y. Meta-analysis of gastroesophageal reflux disease and idiopathic pulmonary fibrosis. Chest. 2018. doi:10.1016/j.chest.2018.07.038
31. Puglisi S, Torrisi SE, Vindigni V, et al. New perspectives on management of idiopathic pulmonary fibrosis. Ther Adv Chronic Dis. 2016;7(2):108–120. doi:10.1177/2040622315624276
32. Lee JS. The role of gastroesophageal reflux and microaspiration in idiopathic pulmonary fibrosis. Clin Pulm Med. 2014;21(2):81–85. http://www.ncbi.nlm.nih.gov/pubmed/24729673.
33. Chen B, You WJ, Liu XQ, Xue S, Qin H, Jiang HD. Chronic microaspiration of bile acids induces lung fibrosis through multiple mechanisms in rats. Clin Sci. 2017;131(10):951–963. doi:10.1042/CS20160926
34. Downing TE, Sporn TA, Bollinger RR, Davis RD, Parker W, Lin SS. Pulmonary histopathology in an experimental model of chronic aspiration is independent of acidity. Exp Biol Med. 2008;233(10):1202–1212. doi:10.3181/0801-RM-17.
35. Appel JZ, Lee SM, Hartwig MG, et al. Characterization of the innate immune response to chronic aspiration in a novel rodent model. Respir Res. 2007;8(1):87. doi:10.1186/1465-9921-8-87
36. Wang Z, Bonella F, Li W, et al. Gastroesophageal reflux disease in idiopathic pulmonary fibrosis: uncertainties and controversies. Respiration. 2018;96(6):571–587. doi:10.1159/000492336
37. Mise J, Lozo M, Mise K, et al. Bronchoalveolar pH and inflammatory biomarkers in newly diagnosed IPF and GERD patients: a case-control study. Med Sci Monit. 2014;20:255–261. doi:10.12659/MSM.889800
38. Savarino E, Carbone R, Marabotto E, et al. Gastro-oesophageal reflux and gastric aspiration in idiopathic pulmonary fibrosis patients. Eur Respir J. 2013;42(5):1322–1331. doi:10.1183/09031936.00101212
39. Davis CS, Mendez BM, Flint DV, et al. Pepsin concentrations are elevated in the bronchoalveolar lavage fluid of patients with idiopathic pulmonary fibrosis after lung transplantation. J Surg Res. 2013;185(2):e101–e108. doi:10.1016/j.jss.2013.06.011
40. Lee JS, Song JW, Wolters PJ, et al. Bronchoalveolar lavage pepsin in acute exacerbation of idiopathic pulmonary fibrosis. Eur Respir J. 2012;39(2):352–358. doi:10.1183/09031936.00050911
41. Ghebremariam YT, Cooke JP, Gerhart W, et al. Pleiotropic effect of the proton pump inhibitor esomeprazole leading to suppression of lung inflammation and fibrosis. J Transl Med. 2015;13(1):249. doi:10.1186/s12967-015-0614-x
42. Johannson KA, Strâmbu I, Ravaglia C, et al. Antacid therapy in idiopathic pulmonary fibrosis: more questions than answers? Lancet Respir Med. 2017;5(7):591–598. doi:10.1016/S2213-2600(17)30219-9
43. Farrell S, McMaster C, Gibson D, Shields MD, McCallion WA. Pepsin in bronchoalveolar lavage fluid: a specific and sensitive method of diagnosing gastro-oesophageal reflux–related pulmonary aspiration. J Pediatr Surg. 2006;41(2):289–293. doi:10.1016/j.jpedsurg.2005.11.002
44. Starosta V, Kitz R, Hartl D, Marcos V, Reinhardt D, Griese M. Bronchoalveolar pepsin, bile acids, oxidation, and inflammation in children with gastroesophageal reflux disease. Chest. 2007;132(5):1557–1564. doi:10.1378/chest.07-0316
45. Krishnan U, Mitchell JD, Messina I, Day AS, Bohane TD. Assay of tracheal pepsin as a marker of reflux aspiration. J Pediatr Gastroenterol Nutr. 2002;35(3):303–308. doi:10.1097/00005176-200209000-00012
46. Lozo Vukovac E, Lozo M, Mise K, et al. Bronchoalveolar pH and inflammatory biomarkers in newly diagnosed IPF and GERD patients: a case-control study. Med Sci Monit. 2014;20:255–261. doi:10.12659/MSM.889800
47. Hong SJ, Kim SW. Helicobacter pylori infection in gastroesophageal reflux disease in the Asian countries. Gastroenterol Res Pract. 2015;2015:985249. doi:10.1155/2015/985249
48. Houghton LA, Lee AS, Badri H, DeVault KR, Smith JA. Respiratory disease and the oesophagus: reflux, reflexes and microaspiration. Nat Rev Gastroenterol Hepatol. 2016;13(8):445–460. doi:10.1038/nrgastro.2016.91
49. Lee JS, Ryu JH, Elicker BM, et al. Gastroesophageal reflux therapy is associated with longer survival in patients with idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;184(12):1390–1394. doi:10.1164/rccm.201101-0138OC
50. Allaix ME, Fisichella PM, Noth I, Herbella FA, Borraez Segura B, Patti MG. Idiopathic pulmonary fibrosis and gastroesophageal reflux. Implications for treatment. J Gastrointest Surg. 2014;18(1):100–105. doi:10.1007/s11605-013-2333-z
51. Fahim A, Dettmar P, Morice A, et al. Gastroesophageal reflux and idiopathic pulmonary fibrosis: a prospective study. Medicina. 2011;47(4):28. doi:10.3390/medicina47040028
52. Gao F, Hobson AR, Shang ZM, et al. The prevalence of gastro-esophageal reflux disease and esophageal dysmotility in Chinese patients with idiopathic pulmonary fibrosis. BMC Gastroenterol. 2015;15:26. doi:10.1186/s12876-015-0253-y
53. Sweet MP, Patti MG, Leard LE, et al. Gastroesophageal reflux in patients with idiopathic pulmonary fibrosis referred for lung transplantation. J Thorac Cardiovasc Surg. 2007;133(4):1078–1084. doi:10.1016/j.jtcvs.2006.09.085
54. Ghebre YT, Raghu G. Idiopathic pulmonary fibrosis: novel concepts of proton pump inhibitors as antifibrotic drugs. Am J Respir Crit Care Med. 2016;193(12):1345–1352. doi:10.1164/rccm.201512-2316PP
55. Fouad YM, Katz PO, Hatlebakk JG, Castell DO. Ineffective esophageal motility: the most common motility abnormality in patients with GERD-associated respiratory symptoms. Am J Gastroenterol. 1999;94(6):1464–1467. doi:10.1111/j.1572-0241.1999.1127_e.x
56. Allaix ME, Rebecchi F, Morino M, Schlottmann F, Patti MG. Gastroesophageal reflux and idiopathic pulmonary fibrosis. World J Surg. 2017;41(7):1691–1697. doi:10.1007/s00268-017-3956-0
57. Hershcovici T, Jha LK, Johnson T, et al. Systematic review: the relationship between interstitial lung diseases and gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;34(11–12):1295–1305. doi:10.1111/j.1365-2036.2011.04870.x
58. D’Ovidio F, Singer LG, Hadjiliadis D, et al. Prevalence of gastroesophageal reflux in end-stage lung disease candidates for lung transplant. Ann Thorac Surg. 2005;80(4):1254–1260. doi:10.1016/j.athoracsur.2005.03.106
59. Hoppo T, Komatsu Y, Jobe BA. Gastroesophageal reflux disease and patterns of reflux in patients with idiopathic pulmonary fibrosis using hypopharyngeal multichannel intraluminal impedance. Dis Esophagus. 2014;27(6):530–537. doi:10.1111/j.1442-2050.2012.01446.x
60. Borges LF, Jagadeesan V, Goldberg H, et al. Abnormal bolus reflux is associated with poor pulmonary outcome in patients with idiopathic pulmonary fibrosis. J Neurogastroenterol Motil. 2018;24(3):395–402. doi:10.5056/jnm18023
61. Gavini S, Finn RT, Lo W-K, et al. Idiopathic pulmonary fibrosis is associated with increased impedance measures of reflux compared to non-fibrotic disease among pre-lung transplant patients. Neurogastroenterology Motil. 2015;27(9):1326–1332. doi:10.1111/nmo.12627
62. Gavini S, Borges LF, Finn RT, et al. Lung disease severity in idiopathic pulmonary fibrosis is more strongly associated with impedance measures of bolus reflux than pH parameters of acid reflux alone. Neurogastroenterology Motil. 2017;29(5):e13001. doi:10.1111/nmo.13001
63. Savarino E, Bazzica M, Zentilin P, et al. Gastroesophageal reflux and pulmonary fibrosis in scleroderma. Am J Respir Crit Care Med. 2009;179(5):408–413. doi:10.1164/rccm.200808-1359OC
64. Sweet MP, Herbella FAM, Leard L, et al. The prevalence of distal and proximal gastroesophageal reflux in patients awaiting lung transplantation. Ann Surg. 2006;244(4):491–497. doi:10.1097/01.sla.0000237757.49687.03
65. Lo W-K, Goldberg HJ, Burakoff R, Feldman N, Chan WW. Increased proximal acid reflux is associated with early readmission following lung transplantation. Neurogastroenterology Motil. 2016;28(2):251–259. doi:10.1111/nmo.12720
66. Raghu G, Rochwerg B, Zhang Y, et al. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis. an update of the 2011 clinical practice guideline. Am J Respir Crit Care Med. 2015;192(2):e3–e19. doi:10.1164/rccm.201506-1063ST
67. Raghu G, Yang ST-Y, Spada C, Hayes J, Pellegrini CA. Sole treatment of acid gastroesophageal reflux in idiopathic pulmonary fibrosis. Chest. 2006;129(3):794–800. doi:10.1378/chest.129.3.794
68. Lee JS, Collard HR, Anstrom KJ, et al. Anti-acid treatment and disease progression in idiopathic pulmonary fibrosis: an analysis of data from three randomised controlled trials. Lancet Respir Med. 2013;1(5):369–376. doi:10.1016/S2213-2600(13)70105-X
69. Fidler L, Sitzer N, Shapera S, Shah PS. Treatment of gastroesophageal reflux in patients with idiopathic pulmonary fibrosis. Chest. 2018;153(6):1405–1415. doi:10.1016/j.chest.2018.03.008
70. Kreuter M, Wuyts W, Renzoni E, et al. Antacid therapy and disease outcomes in idiopathic pulmonary fibrosis: a pooled analysis. Lancet Respir Med. 2016;4(5):381–389. doi:10.1016/S2213-2600(16)00067-9
71. Costabel U, Behr J, Crestani B, et al. Anti-acid therapy in idiopathic pulmonary fibrosis: insights from the INPULSIS® trials. Respir Res. 2018;19(1):167. doi:10.1186/s12931-018-0866-0
72. Linden PA, Gilbert RJ, Yeap BY, et al. Laparoscopic fundoplication in patients with end-stage lung disease awaiting transplantation. J Thorac Cardiovasc Surg. 2006;131(2):438–446. doi:10.1016/j.jtcvs.2005.10.014
73. Raghu G, Mart D, Anstrom KJ, et al. Treatment of Idiopathic Pulmonary Fibrosis (IPF) with Laparoscopic Anti-Reflux Surgery (LARS) Is Associated With Improvement In Forced Vital Capacity (FVC). In:
74. Fisichella PM, Davis CS, Lundberg PW, et al. The protective role of laparoscopic antireflux surgery against aspiration of pepsin after lung transplantation. Surgery. 2011;150(4):598–606. doi:10.1016/j.surg.2011.07.053
75. Cantu E
76. Patti MG, Vela MF, Odell DD, Richter JE, Fisichella PM, Vaezi MF. The intersection of GERD, aspiration, and lung transplantation. J Laparoendosc Adv Surg Tech A. 2016;26(7):501–505. doi:10.1089/lap.2016.0170
77. Raghu G, Pellegrini CA, Yow E, et al. Laparoscopic anti-reflux surgery for the treatment of idiopathic pulmonary fibrosis (WRAP-IPF): a multicentre, randomised, controlled phase 2 trial. Lancet Respir Med. 2018;6(9):707–714. doi:10.1016/S2213-2600(18)30301-1
78. Savarino V, Dulbecco P, Savarino E. Are proton pump inhibitors really so dangerous? Dig Liver Dis. 2016;48(8):851–859. doi:10.1016/j.dld.2016.05.018
79. Frazzoni L, Frazzoni M, de Bortoli N, et al. Postreflux swallow-induced peristaltic wave index and nocturnal baseline impedance can link PPI-responsive heartburn to reflux better than acid exposure time. Neurogastroenterology Motil. 2017;29(11):e13116. doi:10.1111/nmo.13116
80. Frazzoni M, de Bortoli N, Frazzoni L, et al. Impairment of chemical clearance and mucosal integrity distinguishes hypersensitive esophagus from functional heartburn. J Gastroenterol. 2017;52(4):444–451. doi:10.1007/s00535-016-1226-9
81. Frazzoni M, Savarino E, de Bortoli N, et al. Analyses of the post-reflux swallow-induced peristaltic wave index and nocturnal baseline impedance parameters increase the diagnostic yield of impedance-pH monitoring of patients with reflux disease. Clin Gastroenterol Hepatol. 2016;14(1):40–46. doi:10.1016/j.cgh.2015.06.026
82. de Bortoli N, Martinucci I, Savarino E, et al. Association between baseline impedance values and response proton pump inhibitors in patients with heartburn. Clin Gastroenterol Hepatol. 2015;13(6):1082–1088.e1. doi:10.1016/j.cgh.2014.11.035
83. Frazzoni M, Frazzoni L, Tolone S, De Bortoli N, Savarino V, Savarino E. Lack of improvement of impaired chemical clearance characterizes PPI-refractory reflux-related heartburn. Am J Gastroenterol. 2018;113(5):670–676. doi:10.1038/s41395-018-0044-5
84. Borges LF, Rangan V, Hathorn K, et al. 253 - Postreflux Swallow-Induced Peristaltic Wave (PSPW) index and Mean Nocturnal Baseline Impedance (MNBI) on impedance-ph testing predict lung function decline at 1 year in pulmonary fibrosis. Gastroenterology. 2018;154(6):S–61. doi:10.1016/S0016-5085(18)30660-7
85. Borges LF, Hathorn K, Gavini S, et al. Mean nocturnal baseline impedance on multichannel intraluminal impedance monitoring predicts one-year pulmonary function decline in patients with idiopathic pulmonary fibrosis. Gastroenterology. 2017;152(5):S131. doi:10.1016/S0016-5085(17)30771-0
86. Naik RD, Barrett C, Ferguson S, et al. Mucosal integrity testing can detect changes in esophageal and extraesophageal gerd. Gastroenterology. 2019;156(6):
87. Hirano I, Pandolfino JE, Boeckxstaens GE. Functional lumen imaging probe for the management of esophageal disorders: expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15(3):325–334. doi:10.1016/j.cgh.2016.10.022
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
