Back to Journals » International Medical Case Reports Journal » Volume 15
Hypotony Maculopathy Related to Anti-VEGF Intravitreal Injection
Authors Lima-Fontes M , Godinho G, Cunha AM , Madeira C, Falcão M , Falcão-Reis F, Carneiro Â
Received 21 July 2022
Accepted for publication 6 September 2022
Published 19 September 2022 Volume 2022:15 Pages 517—520
DOI https://doi.org/10.2147/IMCRJ.S382421
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mário Lima-Fontes,1 Gonçalo Godinho,2 Ana Maria Cunha,1 Carolina Madeira,3 Manuel Falcão,1,4 Fernando Falcão-Reis,1,4 Ângela Carneiro1,4
1Department of Ophthalmology, Centro Hospitalar Universitário São João, Porto, Portugal; 2Department of Ophthalmology, Centro Hospitalar de Leiria, Leiria, Portugal; 3Department of Ophthalmology, Centro Hospitalar Vila Nova de Gaia/Espinho, Vila Nova de Gaia, Portugal; 4Department of Surgery and Physiology, Faculty of Medicine, University of Porto, Porto, Portugal
Correspondence: Mário Lima-Fontes, Department of Ophthalmology, Centro Hospitalar Universitário São João, Alameda Professor Hernâni Monteiro, Porto, 4200-319, Portugal, Tel +351 918420563, Fax +351 225513669, Email [email protected]
Purpose: To describe a case of hypotony maculopathy following anti-VEGF intravitreal injection (IVI) in a patient with pseudoxanthoma elasticum (PE).
Methods: Clinical case report.
Results: A 52-year-old male complained of right eye (OD) vision loss 2 days after an uncomplicated anti-VEGF IVI for the treatment of choroidal neovascularization secondary to angioid streaks. Relevant medical history included PE, pathologic myopia, and a previous pars plana vitrectomy (PPV) due to a retinal detachment. OD best-corrected visual acuity (BCVA) dropped from 6/12 to 6/18 after the IVI. Intraocular pressure (IOP) was 3 mmHg and chorioretinal folds were evident in the posterior pole. Topical dexamethasone and atropine were prescribed, and full recovery was noticed after 3 days. Four months later, the patient developed a new episode of vision loss after another IVI. His BCVA was counting fingers, IOP was 2mmHg, and more noticeable chorioretinal folds were found. This time, an open scleral wound at the injection site was evident and a scleral suture was necessary. Once again, the patient recovered well.
Conclusion: Hypotony maculopathy following intravitreal injection is a rare condition. However, the described patient presented several conditions which could be related with poor scleral wound closure: intrinsic scleral fragility due to myopia and pseudoxanthoma elasticum; repeated IVI procedures; and absence of vitreous in the posterior segment due to prior vitrectomy. Despite the good outcome, hypotony maculopathy may be a sight-threatening condition, and special attention is necessary for specific patients with risk factors.
Keywords: hypotony maculopathy, intravitreal injection, anti-VEGF, pseudoxanthoma elasticum, angioid streaks
Introduction
Pseudoxanthoma elasticum (PE) is an autosomal recessive disease linked to a mutation in the ABCC6 gene. It causes fragmentation and calcification of the elastic fibers, generating dermatological, vascular, and ophthalmological malformations. The deterioration of the Bruch membrane’s elastic fibers creates angioid streaks, which can develop choroidal neovascularization (CNV).1
Anti-VEGF intravitreal injection (IVI) is commonly used to treat retinal conditions as CNV or diabetic macular edema. Despite being a safe procedure, several IVI are usually necessary to improve or preserve best-corrected visual acuity (BCVA) increasing the risk of adverse effects.
Hypotony maculopathy has been described as the eye globe low pressure that leads to anatomical and functional changes. The most common cause is glaucoma filtering surgery.2 Despite the previous descriptions of wound leaks due to IVI,3,4 the relation with hypotony maculopathy is not usual. We aim to report a case of a hypotony maculopathy following an anti-VEGF intravitreal injection.
Materials and Methods
Description of a clinical case of hypotony maculopathy following anti-VEGF IVI in a patient with pseudoxanthoma elasticum and CNV secondary to angioid streaks.
Written informed consent for publication of this clinical case report was obtained from the patient. Institutional approval was required to publish the case details.
Results
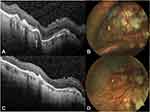
A 52-years-old male presented visual acuity loss of his right eye (OD) 2 days after an uncomplicated ranibizumab IVI with a 30G needle. The past medical history included PE, high myopia, and OD pars plana vitrectomy due to retinal detachment. He was being treated with monthly ranibizumab due to choroidal neovascularization secondary to angioid streaks, with 78 previous injections in the OD. At presentation, his BCVA was 6/18 and the intraocular pressure (IOP) was 3 mmHg. Slit-lamp examination of the anterior segment was unremarkable. Fundoscopy and OCT-scans revealed posterior pole chorioretinal folds (Figure 1A). Altogether, the low intraocular pressure and fundoscopic findings led to the diagnosis of hypotony maculopathy. Topical dexamethasone and atropine were prescribed to improve ciliary body function. The IOP normalized within 3 days with a recovery of visual acuity and resolution of the chorioretinal folds. Four months later, a new OD anti-VEGF IVI with a 30G needle was performed in the inferolateral quadrant and the patient reported decreased visual acuity in the day following the injection. BCVA was counting fingers and IOP was 2 mmHg. Chorioretinal folds in the posterior pole were present, even more prominently this time (Figure 1B). Slit-lamp examination revealed an open scleral wound at the injection site. The wound was sutured with 10–0 monofilament and topical dexamethasone and atropine were prescribed. The patient recovered well (Figure 1C and D) and presented BCVA of 6/12 and an IOP of 12mmHg.
Discussion
Despite being considered a safe procedure, IVI may damage the sclera, leading to some degree of scleral dehiscence.5 Prior cases of wound leak following IVI have been described. However, hypotony maculopathy has not been generally linked to the procedure, particularly with no evidence of wound leak, as described in the first episode of this clinical case. However, our patient presented special conditions that may have promoted the situation.
As so, the scleral thickness is thinner in older and myopic patients.6,7 Also, PE has been linked to “blue sclera”, a condition associated with a decreased scleral thickness,8 probably in the sequence of the fragmentation of the scleral elastic fibers. These were intrinsic characteristics of the patient.
Similarly, several IVI were given to the patient, which have been associated in the literature with localized scleral thinning in the site of the procedure.9 This finding may be caused by the scleral scar formation and hydration promoted by the anti-VEGF IVI.
Finally, a prior pars plana vitrectomy has been performed. The surgery results in a vitreous cavity filled with aqueous humor that is more fluid than vitreous humor and, probably, more prone to leak.
All the ocular conditions created a significant scleral fragility that promoted abnormal reflux, leading to a marked hypotony and consequent hypotony maculopathy and vision loss. Topical treatment is not always sufficient, with more severe cases needing a scleral suture to solve it.
Hypotony maculopathy should be taken into consideration when performing IVI. The need to continue anti-VEGF treatment imposes care with the procedure site, which should be alternated in each administration, to avoid more scleral damage. Also, a perpendicular needle entry in the sclera should be avoided in favor of a more oblique approach, reducing the incidence of blebs in the entry site, and consequent fluid reflux.10
Conclusion
Despite being a popular procedure with a good safety profile, care should be taken when performing an IVI, specially in eyes with thin scleras and previous vitrectomies. Hypotony maculopathy, a sight-threatening condition, is not an adverse effect commonly associated with this procedure. However, it should be considered and prevented in pathologic eyes.
Acknowledgments
No funding or grant support received for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Roach ES, Islam MP. Chapter 15 - Pseudoxanthoma elasticum. In: Islam MP, Roach ES, editors. Handbook of Clinical Neurology. Vol. 132. Elsevier; 2015:215–221.
2. Thomas M, Vajaranant TS, Aref AA. Hypotony Maculopathy: clinical Presentation and Therapeutic Methods. Ophthalmol Ther. 2015;4(2):79–88. doi:10.1007/s40123-015-0037-z
3. Wickremasinghe SS, Michalova K, Guymer RH, Harper CA. Wound leak after intravitreal injection of bevacizumab. Retin Cases Brief Rep. 2008;2(3):245–246. doi:10.1097/ICB.0b013e3181652477
4. Rodrigues EB, Meyer CH, Schmidt JC, Hoerle S, Kroll P. Unsealed sclerotomy after intravitreal injection with a 30-gauge needle. Retina. 2004;24(5):810–812. doi:10.1097/00006982-200410000-00025
5. Breazzano MP, Gangaputra S, Shieh C. Isolated Scleral Dehiscence After Repeated Intravitreal Aflibercept Injections. JAMA Ophthalmol. 2019;137(10):e185935. doi:10.1001/jamaophthalmol.2018.5935
6. Deng J, Jin J, Lv M, et al. Distribution of scleral thickness and associated factors in 810 Chinese children and adolescents: a swept-source optical coherence tomography study. Acta Ophthalmol. 2019;97(3):e410–e418. doi:10.1111/aos.13788
7. Park HY, Shin HY, Park CK. Imaging the posterior segment of the eye using swept-source optical coherence tomography in myopic glaucoma eyes: comparison with enhanced-depth imaging. Am J Ophthalmol. 2014;157(3):550–557. doi:10.1016/j.ajo.2013.11.008
8. Caravati CM
9. Zinkernagel MS, Schorno P, Ebneter A, Wolf S. Scleral thinning after repeated intravitreal injections of antivascular endothelial growth factor agents in the same quadrant. Invest Ophthalmol Vis Sci. 2015;56(3):1894–1900. doi:10.1167/iovs.14-16204
10. Rodrigues EB, Meyer CH, Grumann A
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.