Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Hypoglycemic Coma Caused by Methimazole-Induced Insulin Autoimmune Syndrome, a Case Study
Authors He Y , Xu A, Yu D, Lv S, Xu H
Received 29 January 2023
Accepted for publication 18 April 2023
Published 24 April 2023 Volume 2023:16 Pages 1149—1154
DOI https://doi.org/10.2147/DMSO.S406290
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Gian Paolo Fadini
Yinhui He, Aihua Xu, Danqing Yu, Suzhen Lv, Haiyan Xu
Department of Endocrinology, Lishui Municipal Central Hospital, The Fifth Affiliated Hospital of Wenzhou Medical University, Lishui, Zhejiang Province, 323000, People’s Republic of China
Correspondence: Yinhui He; Haiyan Xu, Email [email protected]; [email protected]
Abstract: Islet autoimmune syndrome (IAS) is an autoimmune disease caused by high concentrations of insulin autoantibodies (IAA) in the blood. It is characterized by hyperinsulinemia and spontaneous hypoglycemia. The incidence of IAS is low, and the hypoglycemia symptom is usually mild. Hence, the severe manifestations (up to seizures and coma) are rarely reported. Here, we reported two cases of Graves’ disease who developed insulin autoimmune syndrome after methimazole treatment. The patients exhibited sudden hypoglycemic coma after receiving methimazole treatment for approximately 2 or 6 months. The patients’ serum glucose levels were below 2.8 mmol/L, and laboratory tests showed high levels of serum insulin and high titers of insulin autoantibodies. Patient 1 discontinued methimazole treatment and the hypoglycemic symptoms disappeared after 7 days. However, patient 2 experienced severe hypoglycemia after discontinuation of methimazole, and the patient condition improved after glucocorticoid therapy. He developed thyroid storm during the treatment, and his condition improved after receiving standard treatment procedures for thyroid storm. To the best of our knowledge, this is the first case report of IAS in Graves’ disease with thyroid storm.
Keywords: hypoglycemia, insulin autoimmune syndrome, Graves’ disease, methimazole, thyroid storm
Introduction
Islet autoimmune syndrome (IAS) is an autoimmune disease caused by high concentrations of insulin autoantibodies (IAA) in the blood. It is characterized by hyperinsulinemia and spontaneous hypoglycemia.1 So far, there are more than 400 cases of IAS reported worldwide, and about 300 cases were reported in Japan. The first case of IAS in China was reported in 1985,2 and nearly 100 cases have been reported in China since then.3,4 Although there are many reported cases of IAS, its incidence is low,5 2.6 cases per year (73 cases over 28 years) in China.6 The hypoglycemia symptoms of IAS are often mild and tend to remit spontaneously. Thus, the mechanisms of IAS are less understood and it is often overlooked by clinicians.
Symptoms of IAS include, but are not limited to, hunger, palpitation, tremors, irritability, behavioral changes, seizures and loss of consciousness.7 The hypoglycemia caused by IAS is usually mild, and severe cases (up to seizures and coma) are rarely reported.8 IAS are mainly induced by drugs containing sulfhydryl (eg, methimazole, captopril) and exogenous insulin. Methimazole-induced IAS mainly occur during 1 to 3 months after taking methimazole, severe hypoglycemia often occurs in the early morning and at midnight. The main features of methimazole-induced IAS laboratory tests include insulin concentration≥100 mU/ L, IAA antibody positive and HLA mainly DRB1* 0406.3 In this article, we reported two cases of hypoglycemic coma caused by methimazole-induced IAS that have been treated in our hospital in the past two years. Both patients provided written informed consent for their case details to be published.
Case Reports
Case 1
Female patient, 51 years old. The patient was admitted to the Endocrinology Department of our hospital on June 21, 2021 due to “sudden unconsciousness for 9 days“. Nine days before admission, the patient had sudden unconsciousness and gibberish, with no limb twitching, no foaming in the mouth, no headache, and no vomiting. The patient went to the emergency department of the local hospital and the blood sugar test was “1.8 mmol/L”. The symptoms of the patient improved after glucose treatment, and she was admitted to hospital afterwards. Blood test showed fasting C-peptide of 6.73ng/mL and fasting insulin of 254.58 mU/L. Thus, the patient was diagnosed with “hypoglycemic coma, hyperthyroidism, and hypertension”. After blood sugar treatment, the hypoglycemic symptom still persisted. Thereby, the patient was transferred to our department for further diagnosis and treatment. The patient had a history of hypertension for 20 years. She had been taking Amlodipine tablets, Telmisartan tablets, Metoprolol sustained-release tablets for antihypertensive therapy, and her blood pressure was controlled. The patient underwent surgical removal of left breast cancer and chemotherapy 10 years ago. The patient was diagnosed with Graves’ disease half a year ago, and she irregularly took “Methimazole tablets” for antithyroid treatment. Physical examination results: T 36.7°C; P 75 beats/min; Bp 129/79 mmHg; mild exophthalmos; moderately enlarged thyroid, soft texture; regular heart rhythm. When the patient suffered from hypoglycemia, the emergency blood sugar was 2.78 mmol/L, the concurrent insulin was >300.00 uU/mL, and the C-peptide was 14.92 ng/mL. The patient fasting insulin was >300.0 uU/mL, fasting C-peptide was 10.73 ng/mL, and fasting blood glucose was 3.09 mmol/L. The 2-hour postprandial insulin was >300.0 uU/mL, 2-hour postprandial C-peptide was 17.78 ng/mL, and 2-hour postprandial blood glucose was 4.30 mmol/L. Results of diabetes autoantibody detection: tyrosine phosphatase antibody 58.2IU/mL (reference value <10), glutamate decarboxylase antibody 5.9 IU/mL (reference value <10), islet cell antibody 0.3COI (cutoff index) (reference value <1.1), IAA 199.0 COI (reference value <1.1). The HbA1c percentage was 6.0%. The patient’s blood ACTH and cortisol were not low. 24 h urinary cortisol was 42.08 μg/24 h (Ref. 4.3–176). The patient’s growth hormone, tumor markers, antinuclear antibody, and antineutrophil cytoplasmic antibody were normal. Thyroid function test results: triiodothyronine (T3) 1.93 ng/mL (reference value 0.58–1.59), thyroxine (T4) 8.04 μg/dL (reference value 4.87–11.72), free triiodothyronine (FT3) 5.74 pg/mL (reference value 1.71–3.71), free thyroxine (FT4) 1.33 ng/dL (reference value 0.7–1.48), thyroid stimulating hormone (TSH) <0.01 μIU/mL (reference value 0.34–5.6), thyroid peroxidase antibody (TPOAb) 952.60 IU/mL (reference value <9), thyroglobulin antibody (TGAb) 124.16 IU/mL (reference value <4), thyroid stimulating receptor antibody (TRab) >40.00 IU/ L (reference value < 1.75). Thyroid B-ultrasound results: the right thyroid lobe had nodule, classified as TI-RADS class 3; goiter, with echo changes and increased blood supply. Thyroid emission single photon computed tomography (ECT) results: both lobes of the thyroid had enlarged glands, with enhanced technetium function. Results of pancreatic CT plain scan and pancreatic MRI plain scan + enhancement: no abnormal signs were found. After the patient was admitted to our hospital, the methimazole tablets were discontinued, and there were still hypoglycemia episodes, most of which occurred at 0:00 in the morning, with the minimum blood glucose of 2.2 mmol/L. During the hypoglycemic period, the patient had no disturbance of consciousness, and the blood sugar increased after eating or high sugar supplementation. Seven days after discontinuation of methimazole tablets, no hypoglycemia occurred. On September 8, 2021, the patient received radioactive iodine 131 therapy (7mci). The patient developed hypothyroidism 3 months after iodine-131 treatment and is currently being treated with levothyroxine tablets. During the follow-up, the patient’s fasting blood glucose and glycosylated hemoglobin were normal.
Case 2
Male patient, 35 years old. The patient was admitted to the neurology department of our hospital on September 23, 2022 due to “unconsciousness for 1 day”. On the day before admission, the patient had a sudden disturbance of consciousness, accompanied by yelling and sweating; the patient waved his limbs irregularly and did not respond to other people’s call. After about 15 minutes, the patient became conscious, but he could not recall the previous incidents and still felt exhausted. Thus, the patient was rushed to the emergency room of our hospital. The emergency blood glucose was 1.9 mmol/L, and the patient’s symptoms improved after supplementation with sugar. Afterwards, he was admitted to the neurology department of our hospital. Under the maintenance of 10% glucose intravenous drip, the patient still had repeated episodes of hypoglycemia and disturbance of consciousness. Hence, he was transferred to the endocrinology department for further diagnosis and treatment of hypoglycemia. The patient had a history of ankylosing spondylitis for 8 years. He started taking sulfasalazine enteric-coated tablets for symptomatic treatment since last year and stopped voluntarily six months ago. The patient had Graves’ disease for 5 years and did not receive treatment. He started taking methimazole tablets (30 mg daily) from 2 months. The results of physical examination on admission: body temperature 36.7°C, pulse 109 beats/min, respiration 23 beats/min, blood pressure 144/83 mmHg; the patient was skinny, exophthalmos, with moderately enlarged thyroid, no palpable nodules, no tenderness, and heart rhythm was normal. When the patient suffered from hypoglycemia, the emergency blood glucose was 1.31 mmol/L, the synchronous insulin was >300.00 uU/mL, and the C-peptide was 26.54 ng/mL. The results of glucose tolerance test and C-peptide insulin release test are shown in Table 1. Results of diabetes autoantibody detection: tyrosine phosphatase antibody <0.7 IU/mL, glutamate decarboxylase antibody 1.4 IU/mL, islet cell antibody 0.1 COI, IAA 263 COI. HbA1c percentage was 5.5%. The patient’s blood ACTH and cortisol were not low. HLA-B27 genotyping was positive. The patient’s growth hormone, tumor markers, antinuclear antibody, and antineutrophil cytoplasmic antibody were normal. Results of thyroid function test on 2022.9.24: T3>6 ng/mL, T4>24 μg/dL, FT3>20 pg/mL, FT4>3.43 ng/dL, TSH<0.008 μIU/mL. TPOAb 544.83 IU/mL, TGAb 83.81 IU/mL, TRAb>31.32 IU/L. Thyroid B-ultrasound results: goiter with echo changes and abnormally rich blood supply, classified as C-TIRADS class 1. Pancreatic CT scan showed no abnormal signs. Cranial CT plain scan: the ventricular system was slightly enlarged, and the sulci were slightly widened. Chest CT scan: 1. Mild inflammation in the right lung, with limited pulmonary emphysema in both lungs. 2. Possibility of ankylosing spondylitis. 3. Thyroid enlargement and uneven density. After admission, the patient stopped taking methimazole tablets but still had hypoglycemia under the maintenance of 10% glucose intravenous infusion, accompanied by disturbance of consciousness, limb convulsions, epilepsy-like seizures, and profuse sweating. The hypoglycemia mostly occurred from 0:00 to 7:00 in the morning, with a minimum blood glucose of 1.31mmol/L, which required emergency treatment of high sugar. In the morning of September 27, 2022, the patient developed disturbance of consciousness, fever with 40.6°C body temperature, heart rate 147 beats/min, and normal blood sugar. Thyroid storm was considered, and he was immediately given PTU antithyroid treatment, ventricular rate control with propranolol tablets, intravenous glucocorticoids, anti-infection treatment with piperacillin-tazobactam sodium, and fluid replacement therapy. After the patient’s condition was gradually stabilized, the intravenous glucocorticoids was discontinued, and long-term prednisone tablets (20 mg) was given every 8 hours. Thirteen days after discontinuation of methimazole tablets, no hypoglycemia occurred. Results of thyroid function were reviewed on 2022.10.4: T3 1.36 ng/mL, T4 9.47 μg/dL, FT3 4.57 pg/mL, FT4 1.65 ng/dL, TSH <0.008 μIU/mL. On December 8, 2022, the patient received radioactive iodine 131 therapy (22mci). Prednisone was tapered gradually by 5mg every 1–2 weeks and discontinued in January 2023. No hypoglycemia occurred during follow-up. IAA changes were shown in Figure 1, the IAA titer decreased gradually. On March 7, 2023, the patient IAA was 12.6 COI, fasting insulin was 29.0 uU/mL, fasting C-peptide was 1.60 ng/mL, and fasting blood glucose was 5.07mmol/L.
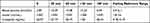 |
Table 1 The Results of a 75-g Oral Glucose Tolerance Test on Patient 2 |
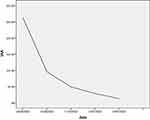 |
Figure 1 The follow-up IAA on Patient 2. |
Demographic characteristics, laboratory data and management of the 2 cases were summarized in Table 2.
 |
Table 2 Demographic Characteristics, Laboratory Data and Management of the 2 Cases |
Discussion
We report 2 cases with Graves’ disease who developed insulin autoimmune syndrome after methimazole treatment. Both patients had the following characteristics: 1. Graves’ disease was diagnosed before admission, and methimazole tablets were used for antithyroid treatment. 2. Severe hypoglycemia symptoms occurred after treatment with methimazole tablets, the blood sugar was low, the synchronous serum insulin level was significantly increased, and the C-peptide level was not obviously increased. 3. Hypoglycemia episodes repeatedly occurred, often occurring at night and requiring high-concentration glucose treatment. 4. Patients never used exogenous insulin and they were positive for insulin autoantibodies. 5. No obvious abnormality was found in pancreas imaging examination. 6. No hypoglycemia occurred after discontinuing methimazole tablets for a period of time. These features are consistent with the clinical characteristics of methimazole-induced insulin autoimmune syndrome in the Chinese population, as summarized by Wang et al through literature review.3 As a relatively rare disease, IAS currently has no accepted treatment guidelines, and it needs to be differentiated from insulinoma, type B insulin resistance syndrome, and non-insulinoma pancreatic hypoglycemia syndrome.9 The two cases in this report were also different in several aspects. Case 1 responded well to methimazole, while Case 2’s response to methimazole tablet treatment was poor, and FT3, FT4 did not decrease after 2 months of treatment. The underlying mechanism is not yet clear. Case 1 did not use glucocorticoids, and after 7 days of discontinuation of methimazole, hypoglycemia did not recur. Because FT3 and FT4 were mildly elevated in case 1 after discontinuation of methimazole, the radioactive iodine-131 was given for antithyroid therapy. On the contrary, severe hypoglycemia occurred in case 2 after discontinuation of methimazole, and the condition improved after glucocorticoid therapy. Case 2 also had ankylosing spondylitis. IAS often occurs in patients with autoimmune diseases such as Graves’ disease, rheumatoid arthritis, systemic lupus erythematosus, and psoriasis, and it is mostly drug-induced.10
Moreover, during the treatment, case 2 showed high fever (Burch-Wartofsky score:30), disturbance of consciousness (Burch-Wartofsky score:30), rapid heart rate (Burch-Wartofsky score:25), significantly increased FT3 and FT4, and presence of pulmonary infection predisposition (Burch-Wartofsky score:10); the Burch-Wartofsky total score was as high as 95. A score of 45 or greater is highly suggestive of thyroid storm.11 The patient condition stabilized after thyroid storm treatment.12 To the best of our knowledge, this is the first report of IAS in Graves’ disease with thyroid storm. The two patients understood the cause of their hypoglycemia and actively cooperated with the medical staff for treatment. There were no severe hypoglycemia episodes after discharge, and the prognosis of IAS was satisfactory.
IAS can be triggered by exposure to viruses or drugs, or it may occur spontaneously.13 Medications or drugs containing sulfhydryl groups are associated with IAS. It has been shown that sulfhydryl groups can bind to and reduce the sulfhydryl bonds connecting insulin chains A and B, making endogenous insulin more immunogenic.14 This result triggers an immune response and produces IAA, which has the characteristics of low affinity and high binding capacity,15 resulting in dramatic fluctuations in blood glucose in the body. Human leukocyte antigen (HLA) is closely related to the occurrence of IAS. Asian IAS patients express HLA-DR4, which is mainly DRB1*0406;3,16,17 and HLA-DRB1*0403 is more common in the Caucasian patients.18
There are still limitations of this study. For Case 1, no hypoglycemia occurred after discharge, but C-peptide, insulin and insulin autoantibodies were not re-examined during follow-up. There are plenty of follow-up data on Case 2. As the previous insulin titers were larger than the upper limit detected by the kit, the laboratory did not give specific values. We cannot graph the changes of serum insulin. Since the hospital and the genetic testing company did not develop IAS-related genetic testing, neither of the patient underwent genetic examination.
Conclusion
In conclusion, methimazole-induced insulin autoimmune syndrome has many common clinical features, such as hypoglycemia with high serum insulin concentrations and the presence of insulin autoantibodies in Graves’ patients with methimazole therapy. However, each patient also has its own unique clinical manifestations, such as thyroid storm. Therefore, for Graves’ patients who exhibit repeated severe hypoglycemia during antithyroid treatment, the possibility of methimazole-induced insulin autoimmune syndrome should be considered in order to make correct diagnosis, start treatment in time, and improve patient prognosis.
Ethics Statements
Ethical review and approval were not required because this is not a clinical study but a case study in accordance with the local legislation and institutional requirements. Both patients provided written informed consent for their case details to be published.
Acknowledgments
This work was supported by the Zhejiang Province Scientific Project of Health and Medicine (2021ZH015).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflict of interest.
References
1. Hirata Y, Ishizu H, Ouchi N, et al. Insulin autoimmunity in a case with spontaneous hypoglycemia. J Jpn Diabetes Soc. 1970;13:312–320.
2. Xiang D, Chen J, Xu M, et al. Insulin autoimmune syndrome - hypoglycemia caused by insulin autoantibodies. J Endocrinol Metab China. 1986;1:64.
3. Wang C, Sun W, Sun L. Clinical characteristics of insulin autoimmune syndrome caused by methimazole in Chinese population. Chin Clin Pharmacol Ther. 2020;25(02):209–213.
4. Hou S, Zheng W, Wang P, Meng Z, Tan J. A case of methimazole-related insulin autoimmune syndrome. China Clin Case Res Database. 2022;04(01):E00773.
5. Cappellani D, Macchia E, Falorni A, Marchetti P. Insulin autoimmune syndrome (Hirata Disease): a comprehensive review fifty years after its first description. Diabetes Metab Syndr Obes. 2020;1(13):963–978. doi:10.2147/DMSO.S219438
6. Wang YL, Yao PW, Zhang XT, Luo ZZ, Wu PQ, Xiao F. Insulin autoimmune syndrome: 73 cases of clinical analysis. Chin Med J. 2015;128(17):2408–2409. doi:10.4103/0366-6999.163376
7. Martens P, Tits J. Approach to the patient with spontaneous hypoglycemia. Eur J Intern Med. 2014;25(5):415–421. doi:10.1016/j.ejim.2014.02.011
8. Zhang Y, Zhao T. Hypoglycemic coma due to insulin autoimmune syndrome induced by methimazole: a rare case report. Exp Ther Med. 2014;8(5):1581–1584. doi:10.3892/etm.2014.1964
9. Censi S, Mian C, Betterle C. Insulin autoimmune syndrome: from diagnosis to clinical management. Ann Transl Med. 2018;6(17):335. doi:10.21037/atm.2018.07.32
10. Qin Y, Shen Y, Dai P, Chen Z, Lv Q, Ye Y. Literature analysis of 101 cases of drug-induced insulin autoimmune syndrome. Pharm Serv Res. 2020;20(03):213–216.
11. Burch HB, Wartofsky L. Life-threatening thyrotoxicosis. Thyroid storm. Endocrinol Metab Clin North Am. 1993;22(2):263–277. doi:10.1016/S0889-8529(18)30165-8
12. Endocrinology Branch of Chinese Medical Association, Endocrinology and Metabolism Branch of Chinese Medical Doctor Association, Nuclear Medicine Branch of Chinese Medical Association, Thyroid and Metabolic Surgery Group of Surgery Branch of Chinese Medical Association, Thyroid Surgeons Committee of Chinese Medical Doctor Association Surgeons Branch. Guidelines for the diagnosis and treatment of thyrotoxicosis caused by hyperthyroidism and other causes. Int J Endocrinol Metab. 2022;42(05):401–450.
13. Ismail AA. The insulin autoimmune syndrome (IAS) as a cause of hypoglycaemia: an update on the pathophysiology, biochemical investigations and diagnosis. Clin Chem Lab Med. 2016;54(11):1715–1724. doi:10.1515/cclm-2015-1255
14. Cryer PE, Axelrod L, Grossman AB, et al. Endocrine Society. Evaluation and management of adult hypoglycemic disorders: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2009;94(3):709–728. doi:10.1210/jc.2008-1410
15. Nasu T, Suzuki R, Okamoto Y, et al. Late postprandial hypoglycemia due to bioactive insulin dissociation from autoantibody leading to unconsciousness in a patient with insulin autoimmune syndrome. Intern Med. 2011;50(4):339–343. doi:10.2169/internalmedicine.50.4145
16. Uchigata Y, Kuwata S, Tokunaga K, et al. Strong association of insulin autoimmune syndrome with HLA-DR4. Lancet. 1992;339(8790):393–394. doi:10.1016/0140-6736(92)90080-M
17. Park MH, Park YJ, Song EY, et al. Association of HLA-DR and -DQ genes with Graves disease in Koreans. Hum Immunol. 2005;66(6):741–747. doi:10.1016/j.humimm.2005.03.001
18. Veltroni A, Zambon G, Cingarlini S, Davì MV. Autoimmune hypoglycaemia caused by alpha-lipoic acid: a rare condition in Caucasian patients. Endocrinol Diabetes Metab Case Rep. 2018;2018:18. doi:10.1530/EDM-18-0011
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
