Back to Journals » Risk Management and Healthcare Policy » Volume 13
Hypertension and Diabetes Management Practices Among Healthcare Workers in Imo and Kaduna States, Nigeria: An Exploratory Study
Authors Anyanti J , Akuiyibo S, Idogho O, Amoo B , Aizobu D
Received 20 July 2020
Accepted for publication 28 September 2020
Published 10 November 2020 Volume 2020:13 Pages 2535—2543
DOI https://doi.org/10.2147/RMHP.S271668
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Jennifer Anyanti, Selema Akuiyibo, Omokhudu Idogho, Babatunde Amoo, Dennis Aizobu
Society for Family Health, Abuja, Nigeria
Correspondence: Selema Akuiyibo Email [email protected]
Introduction: Effective management of hypertension and diabetes through accurate diagnosis and treatment can reduce the risk of complications and early deaths. This study was a descriptive cross-sectional study aimed at determining practices regarding hypertension and type 2 diabetes management among healthcare providers in Kaduna and Imo States, Nigeria. Data were collected using a semi-structured interviewer administered questionnaire consisting of questions across four major domains: 1) screening; 2) diagnosis; 3) pharmacological; and 4) non-pharmacological treatment of hypertension and diabetes.
Results: A total of 77 healthcare providers were interviewed and they included; 20 (26.5%) medical doctors, 25 (32.5%) nurses/midwives, 18 (23.4%) community health extension workers and 3 (3.9%) pharmacists. Almost half (46.8%) of the respondents indicated that they prioritize routine blood pressure (BP) checks among all adult patients while only 30 (39.0%) and 8 (10.4%) correctly identified the diagnostic criteria for hypertension and diabetes, respectively. Calcium chain blockers only were the most prescribed medication for treatment of hypertension across all stages of hypertension while metformin (glucophage) was stated as the preferred medication prescribed for controlling blood glucose levels among the respondents. Only 32.5% of the respondents stated that they have a means in place in their facilities to ensure that hypertension and diabetes patients adhere to follow-on visit recommendations.
Conclusion: A significant knowledge gap was identified in the diagnosis and treatment of hypertension and diabetes among the respondents due to unavailability of properly outlined management guidelines for these conditions for the different cadres of healthcare workers in Nigeria. There is a need for the development and wide distribution of guidelines highlighting cadre-specific roles for healthcare providers in hypertension and diabetes management and standard operating procedures based on such guidelines should be available at various points of care to ensure better treatment outcomes.
Keywords: hypertension, diabetes, management, healthcare workers, facilities
Introduction
Hypertension and diabetes are important medical conditions that are responsible for a significant number of deaths globally. Complications from hypertension are estimated to cause 9.4 million deaths every year and about 4 out of every 10 deaths among people with diabetes is as a result of raised blood pressure.1,2 While hypertension remains a major risk factor for deaths and disability globally, diabetes alone resulted in 1.4 million deaths in 2016.2 Over a billion people have hypertension while more than 400 million people are living with diabetes.3,4 It is estimated that two-thirds and four-fifths of adults living with hypertension and diabetes respectively are in low- and middle-income countries (LMICs).4,5
Being chronic conditions that often rarely present with symptoms at early stages, the majority of hypertension and diabetes cases are often left undiagnosed.6 For instance, around 46% of all diabetes cases worldwide are yet to be diagnosed.7 Inaccurate screening criteria also contributes to the burden of undiagnosed hypertension.8 Undiagnosed hypertension or diabetes increases the risk of complications among those affected as late detection affects prognosis and increases the burden as well as cost of treatment among those affected.6 The first step in reducing the risk of complications and effectively managing hypertension and diabetes is ensuring early and accurate diagnosis.9 In addition, about half of those diagnosed either remain untreated or are not adequately treated.6,8 Hence, treatment and control of blood pressure and blood glucose levels are equally essential for adequate management of hypertension and diabetes respectively.
Few recommendations for prevention, diagnosis and management of hypertension and cardiovascular risk factors in sub-Saharan Africa are available in the widely acceptable guidelines for the management of these conditions.10 Despite the availability of standard management guidelines globally, control of hypertension and diabetes in LMICs is still considered low compared to developed countries.11 Lack of awareness and general non-adherence to approved guidelines could be responsible for inadequate control being experienced in LMICs.12,13
The majority of healthcare services in Nigeria including hypertension and diabetes care are accessed through public and private hospitals14 and also from community pharmacies or patent proprietary medicine vendors (PPMVs).15–17 Community pharmacists are legally mandated to sell and dispense ethical drugs in Nigeria while PPMVs acquire health training through apprenticeship and can sell only patent medicines.15 In Nigeria, some primary level of care including hypertension and diabetes care, are often sought from these two groups.15 However, integrated guidelines for NCDs management in such resource-constrained settings are not available.10 Implementation of integrated non-communicable disease programs implemented through a primary healthcare approach are an affordable and sustainable way for countries to tackle hypertension. Thus, there is a need to ensure that best practices are being adopted by healthcare providers at this level in order to achieve acceptable levels of NCDs control. The WHO Package of Essential Non-communicable (PEN) Disease Interventions remains a preferred alternative integrated NCDs management guideline in low-resource settings such as Nigeria, as it is designed for primary healthcare and it highlights an integrated approach to NCDs care including hypertension and diabetes.18
In order to ensure desirable treatment outcomes are achieved in the management of hypertension and diabetes cases by healthcare providers in Nigeria, there is a need to assess current practices relating to the management of these conditions in comparison to established guidelines and evidence-based recommendations. This study attempts to evaluate the practices related to hypertension and diabetes management among healthcare workers across private and public sectors in Imo and Kaduna States. It aimed to understand screening and diagnostic practices according to relevant guidelines, pharmacological and non-pharmacological treatment recommendations among selected healthcare professionals in the country.
Materials and Methods
Approach
A descriptive cross-sectional study was conducted to assess the baseline status regarding hypertension and type 2 diabetes management among healthcare providers in participating facilities of the improving access to Non-communicable diseases (NCDs) management in Nigeria (ACCESS-N) project being implemented by Society for Family Health (SFH) in Imo and Kaduna States of Nigeria prior to the commencement of project interventions. Access-N is a 1-year health promotion project which focuses on two non-communicable diseases – hypertension and type 2 diabetes. The project aims to empower and train healthcare providers in private and public facilities across selected local governments (LGAs) in the implementing states to effectively diagnose, treat and educate clients on hypertension and type 2 diabetes.
Access-N adopts a hub and spoke facility model wherein hub facilities are empowered to provide comprehensive hypertension and type 2 diabetes management services while the spokes facilities provide basic services including screening and referral services to the hubs, for the two conditions. Each LGA selected for the project is made up of a cluster of five facilities; at least one hub and four spokes. Hubs include private hospitals with the capacity to provide secondary level of care and the spokes included primary health centers, faith-based clinics, community pharmacies (CPs), proprietary medicine vendors (PPMVs) and other smaller private hospitals (providing primary level of care). The project offers services through 35 health facilities in seven local government areas (LGAs) both rural and urban in each state: seven of the 27 and 23 LGAs in Imo and Kaduna States respectively. In Imo State, the urban LGAs included Owerri North, Obowo and Oguta while Aboh Mbaise, Oru West, Njaba and Ngor Okpala made up the rural LGAs. In Kaduna State, Kaduna North, Kaduna South, Zaria, Sabon Gari comprised of the urban LGAs while Igabi, Chikun and Kachia were the rural LGAs.
This study was a descriptive cross-sectional study aimed at determining the baseline status regarding hypertension and type 2 diabetes management among healthcare providers working in participating facilities (both hubs and spokes) of the project prior to the commencement of project interventions.
Study Population
The respondents were healthcare providers selected from Access-N participating facilities in Imo and Kaduna States. Only individuals who were responsible for actively managing and attending to hypertension and diabetes cases in these facilities were included in the study. In total, 77 healthcare providers in Imo and Kaduna states with different levels of medical qualifications participated in the study.
Data Collection and Analysis
Data was collected using a semi-structured interviewer administered questionnaire consisting of open and close ended questions across four major domains: 1) screening; 2) diagnosis; 3) pharmacological; and 4) non-pharmacological treatment of hypertension and diabetes.
Our study complied with the Declaration of Helsinki. Ethical approval for this study was obtained from the Institutional Review Board of the Nigeria Institute of Medical Research, Yaba, Lagos, Nigeria. An informed consent was obtained from each participant after the purpose of the study had been explained to them and their right to withdraw from the study at any point in time if they became unwilling to continue with the study. No identifying information of the participants was collected.
Data analysis was completed using Statistical Package for Social Sciences (SPSS), version 20.0. Descriptive statistics such as frequencies and proportions were used to summarize categorical variables while the continuous variable, “years of medical experience” was expressed as mean ± SD.
Results
The mean years of medical experience among the respondents was 20.1 ± 10.7 years. Out of the 77 healthcare providers interviewed, 40 (51.9%) were females while the rest (37, 48.1%) were males. Twenty-eight (36.4%) respondents were aged 35–44 years old, 18 (23.4%) were 55–64 years old, 16 (20.8%) were 45–54 years old, 11 (14.5%) were 25–34 years while only 4 (5.2%) were 65 years or older. Medical doctors made up 20 (26.0%) of the study population, 25 (32.5%) were nurses/midwives, 18 (23.4%) were community health extension workers (CHEWs) and 3 (3.9%) were pharmacists. Table 1 shows the socio-demographic characteristic of the respondents.
 |
Table 1 Socio-Demographic Characteristics of Respondents |
Facility Types and Hypertension/Diabetes Service Delivery
The respondents were drawn from different facility types including private hospitals, faith-based hospitals, primary health centers (PHCs), CPs and PPMVs. Thirty-eight (49.4%) of the respondents worked in a PHC, 28 (36.4%) worked in a private (or faith-based) hospital while 6 (7.8%) and 5 (6.5%) worked in a CP and PPMV outlet respectively as shown in Table 2. The majority (63, 81.8%) of the facilities where the respondents worked offered both hypertension and diabetes screening services, consultation sessions were maximized to educate clients on NCDs in 73 (94.8%) of the facilities but only 26 (33.8%) of the facilities had educational materials to guide patients on lifestyle modification. On average, 52 (67.5%) of the facilities saw between 1 and 25 hypertension and/or diabetes cases weekly (an average of 17 and 30 in Imo and Kaduna States respectively).
 |
Table 2 Facility Types and Hypertension/Diabetes Service Availability and Provision |
Screening and Diagnostic Criteria for Hypertension and Diabetes Among Respondents
Almost half of the respondents (36, 46.8%) indicated that they prioritized routine blood pressure (BP) checks among all adults (18 years and above) irrespective of their presenting signs and symptoms compared to individuals who were younger. Among the respondents that prioritized routine BP checks among all adults, 22 (61.1%) of them were medical doctors or nurses while the rest were non-medical doctors/nurses (which included CPs, PPMVs, laboratory assistants, and CHEWs). Similarly, more respondents stated that they prioritized routine blood glucose (BG) tests among all adults (18 years and above) than the other patient profiles indicated in Table 3. Also, Table 3 shows the correctness of the diagnoses (criteria based on recommendation of the WHO-PEN) used for hypertension and diabetes mellitus diagnosis as indicated by the respondents.
 |
Table 3 Screening and Diagnostic Criteria for Hypertension and Diabetes Among Respondents |
Pharmacological Treatment of Hypertension Among the Respondents
According to Figure 1, calcium chain blockers (CCB) were the most prescribed medication for treatment of hypertension across all stages of the condition. A combination of at least 2 or 3 antihypertensive drugs were also typically prescribed by the respondents for blood pressure control across the three blood pressure categories as shown in Figure 1.
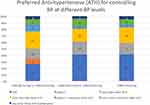 |
Figure 1 Medications prescribed for hypertension management by respondents across blood pressure levels. |
Pharmacological Treatment of Diabetes Among Respondents
Metformin (Glucophage) was stated as the preferred medication prescribed for controlling blood glucose levels among the respondents. Twenty-seven (60.0%) among 45 respondents stated they would prescribe only metformin (glucophage) for a patient with a blood glucose level between > 11.1 mmol/L (199.8 mg/dL) and < 11.7 mmol/L while 12 (26.7%) stated they would prescribe both metformin and glibenclamide for such a patient. Preferred diabetes medication prescription indicated by the respondents are shown in Table 4.
 |
Table 4 Preferred Diabetes Medication Among Respondents |
Hypertension and Diabetes Management Goals and Practices Among Respondents
The majority (70, 90.0%) of the respondents indicated that the goal of hypertension and diabetes management is to reduce blood pressure and glucose levels respectively while only 5 (5.5%) stated it is to encourage lifestyle changes. Only 25 (32.5%) of the respondents stated that they have a means in place in their facilities to ensure that hypertension and diabetes patients adhere to follow-on visit recommendations; the means stated by the respondents included phone calls19 and home visits.6 Table 5 shows data on the availability of means for ensuring adherence to follow-on visit recommendations in the respondents’ facilities, dietary recommendations and recommended frequency of follow-up for hypertension and diabetes patients of the respondents.
 |
Table 5 Hypertension and Diabetes Management Goals and Practices Among Respondents |
Discussion
The study examined the baseline hypertension and diabetes management practices among healthcare providers working in participating facilities of the Access-N project in Kaduna and Imo States of Nigeria. The result showed a significant non-uniform approach in the management of the two conditions among the respondents. More than half of the respondents in this study were either medical doctors or nurses (and midwives); most of whom are working in private hospitals and public primary healthcare centers respectively. More than a third of them had practiced their profession for between 11 and 20 years. Fewer of the respondents were owners of community pharmacies and patent medicine vendor stores. These informal healthcare providers are easily accessible to lower- and middle-class individuals which make up a larger proportion of the Nigerian population including in Imo and Kaduna States.14 This was also evident in the significant average weekly client flow of 1–50 clients for both hypertension and diabetes services observed in this study. A similar finding was made in a study among primary care physicians in Nigeria where, on average, four hypertension patients were seen daily.13
Due to increasing prevalence, availability of hypertension and diabetes management services have become important in health facilities at all levels6 The relative high availability of both hypertension and diabetes screening services in our respondents’ facilities (81.8%) indicate a high demand for these services. Community pharmacies (CPs) and proprietary medicine vendors (PPMVs) in Nigeria have been reported to provide basic health services such as STI management, Malaria and contraceptive education.15 It was observed in this study that they offer basic hypertension and diabetes services including screening, diagnosis, treatment for uncomplicated cases and referrals for complicated cases. However, the quality of such services provided by these entities are questionable as observed in this study. Considering the chronic nature of hypertension and diabetes, CPs and PPMVs could play a major role in offering health education on the two conditions and referral to hospitals for onward screening and diagnosis. Currently, the Pharmaceutical Council of Nigeria (PCN) Act approves only registered pharmacists to either dispense or replace hypertension and diabetes medication following diagnosis by a physician.
Most guidelines suggest adulthood, without specific preference to any age, as the preferred age for targeted hypertension screening.19 The WHO guideline for low resource settings suggests age 40 years for diabetes and blood pressure screening.20 Research has shown that based on recent hypertension guidelines, the magnitude of increase in hypertension prevalence in Nigeria is higher among individuals aged 20−39 years.21 In this study, it was observed that more than four out of every ten respondents screen all adults for diabetes and hypertension respectively. This is laudable as findings have shown that widening the criteria for preventive intervention and implementation of a population-based strategy are more effective than high-risk prevention strategies especially for chronic illnesses such as hypertension and diabetes.22
It was observed in this study that almost all the respondents maximize their consultation sessions to educate their clients about NCDs generally. This shows that healthcare providers consider NCDs to be a serious public health concern. However, despite the reported effectiveness of information, education and communication (IEC) materials in health communication,23 only a few of our respondents stated that they had IEC materials in their facilities to complement health education among their clients. IEC materials are effective tools in behavior change communication, which is an important part of NCDs (such as hypertension and diabetes) messaging. Health facilities should be provided which such tools to enhance NCD education in facilities.
According to ESH/ESC recommendations, hypertension is classified into three grades based on blood pressure levels. Diagnosis of hypertension in adults in based on an average of at least two systolic and diastolic blood pressure readings of ≥ 140 and 90 mmHg respectively.24 Only about four out of every ten of our respondents correctly identified that they should diagnose hypertension at these BP levels. Varying systolic and diastolic values were stated among the respondents in this study. In another study among primary care providers in Nigeria, a higher proportion (75%) of the respondents diagnosed hypertension using the correct BP threshold.13 The lower prevalence observed in this present study could be because non-physicians who have limited medical education were also included as respondents unlike the study by Ale and Braimoh13 wherein only medical doctors made up the study population. Similarly, it was observed that a much lower proportion (10.4%) of our respondents diagnosed diabetes mellitus using the WHO recommended blood glucose levels of ≥ 7.0 mmol/L (126 mg/dL) fasting plasma glucose test or ≥ 11.1 mmol/L (200 mg/dL) for random plasma glucose test. This finding identifies a huge gap in hypertension and diabetes management since accurate diagnosis remains the first step in achieving control. There is a need for continuing health education interventions among healthcare providers in order to address this problem.
Metformin is the most popular first level medication used in initial therapy for type 2 diabetes and used in combination with other diabetes drug classes in special cases.25 In this study, the majority of the respondents prescribed metformin as the first drug of choice and only prescribed it in addition to glibenclamide as second choice of therapy. This is consistent with guideline recommendations.4,26,27
Studies have shown that at the first stage (and even other stages) of hypertension, a calcium channel blocker (CCB) is the most prescribed medication among healthcare providers.12,28–30 CCB has been proven to achieve normotension (<140/90 mmg) compared to other monotherapy,31 although there are claims that diuretics could be an equally effective or better option.32 A prevalence of multitherapy preference was also observed among our respondents similar to findings by Odili et al.12 Although, several factors such as sex, age, and presenting symptoms are important in prescribing a therapy, guideline recommendations suggest that small doses of different classes of antihypertensive drugs are more beneficial than a high dose of one especially at higher blood pressure levels.33,34 Although this study could not ascertain the effectiveness of these medications in achieving blood pressure control, there is a need for a harmonized widely acceptable protocol for pharmacological treatment of hypertension in Nigeria.
The WHO, in addition to reduction of blood pressure and blood glucose levels as goals of hypertension and diabetes management or reducing risk of complications, also suggests that encouraging lifestyle changes is necessary to achieve hypertension and diabetes control.20 However, only a few of our respondents consider encouraging lifestyle changes among respondents as a goal of hypertension and diabetes management. This is worrisome as lifestyle changes has been found to be effective in maintaining healthy blood pressure and glucose levels and it is also cost-effective strategy for NCD management.20,35 Also, most of our respondents do not have a means of ensuring that their patients adhere to follow-on recommendation owing to unavailability of resources for such activities. Considering the chronic nature of NCDs, there is a need for relevant stakeholders (healthcare providers at all levels) to put means in places for ensuring adherence to follow-on visit among patients and also to encourage adoption of healthy lifestyle such as physical activity, tobacco use reduction, improved dietary intake and reduction of alcohol intake.20
There are a few limitations to note about this study. First, this study was conducted among healthcare workers in primary care settings in the study area and thus the findings from this study may not be applicable to healthcare workers working at a higher level of care. Also, the small sample size used in this study was as a result of the limited facilities covered by the Access-N project. Although this may affect the generalizability and external validity of the findings, it was ensured that the selection of study sites was randomly done and spread across the target LGA. It is recommended that future research includes other cadres of healthcare workers. Findings from this study will assist in identifying gaps and make recommendations for intervention activities targeting at improving hypertension and diabetes management among healthcare providers in Nigeria.
Conclusion
The study presents an overview of hypertension and diabetes management practices in primary healthcare settings in Imo and Kaduna States, Nigeria. Despite the availability of WHO guidelines for hypertension and diabetes management in low resource settings, adherence to guideline recommendations for screening, diagnosis and treatment of hypertension and diabetes cases vary widely among primary healthcare providers in Imo and Kaduna States. Significant inconsistencies in screening and diagnostic criteria, treatment recommendation and goals were observed. There is a need for the development and wide circulation of adopted or adapted government-approved guidelines for the management of the two conditions among healthcare providers in these locations. Also, continuous training of healthcare providers across all cadres involved in hypertension and diabetes management on recommended guideline provisions (including lifestyle and dietary modification recommendation to patients) should be prioritized in order to achieve commendable hypertension and diabetes control in the two states.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet. 2012;380(9859):2224–2260. doi:10.1016/S0140-6736(12)61766-8
2. WHO. Global Health Observatory (GHO) Data NCD Mortality and Morbidity. World Health Organization; 2018.
3. Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–450. doi:10.1161/CIRCULATIONAHA.115.018912
4. International Diabetes Federation. IDF Diabetes Atlas.
5. Campbell NRC, Lackland DT, Niebylski ML. High blood pressure: why prevention and control are urgent and important-a 2014 fact sheet from the world hypertension league and the international society of hypertension. J Clin Hypertens. 2014;16(8):551–553. doi:10.1111/jch.12372
6. Mohan V, Seedat YK, Pradeepa R. The rising burden of diabetes and hypertension in southeast Asian and African regions: need for effective strategies for prevention and control in primary health care settings. Int J Hypertens. 2013;2013:1–14. doi:10.1155/2013/409083
7. Beagley J, Guariguata L, Weil C, Motala AA. Global estimates of undiagnosed diabetes in adults. Diabetes Res Clin Pract. 2014;103(2):150–160. doi:10.1016/j.diabres.2013.11.001
8. Ataklte F, Erqou S, Kaptoge S, Taye B, Echouffo-Tcheugui JB, Kengne AP. Burden of undiagnosed hypertension in sub-saharan africa: a systematic review and meta-analysis. Hypertension. 2015;65(2):291–298. doi:10.1161/HYPERTENSIONAHA.114.04394
9. Schwartz CL, McManus RJ. What is the evidence base for diagnosing hypertension and for subsequent blood pressure treatment targets in the prevention of cardiovascular disease? BMC Med. 2015;13(1). doi:10.1186/s12916-015-0502-5
10. Owolabi M, Olowoyo P, Miranda JJ, et al. Gaps in hypertension guidelines in low- and middle-income versus high-income countries: a systematic review. Hypertension. 2016;68(6):1328–1337. doi:10.1161/HYPERTENSIONAHA.116.08290
11. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: national Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief. 2013.
12. Odili V, Oghagbon E, Ugwa N, Ochei U, Aghomo O. Adherence to international guidelines in the management of hypertension in a tertiary hospital in Nigeria. Trop J Pharm Res. 2008;7(2). doi:10.4314/tjpr.v7i2.14608
13. Ale OK, Braimoh RW. Awareness of hypertension guidelines and the diagnosis and evaluation of hypertension by primary care physicians in Nigeria. Cardiovasc J Afr. 2017;28(2):72–76. doi:10.5830/CVJA-2016-048
14. Asakitikpi E. A healthcare coverage and affordability in Nigeria: an alternative model to equitable healthcare delivery. In: Universal Healthcare. IntechOpen; 2019. Available from. https://www.intechopen.com/online-first/healthcare-coverage-and-affordability-in-nigeria-an-alternative-model-to-equitable-healthcare-delive.
15. Okonkwo AD, Okonkwo UP. Patent medicine vendors, community pharmacists and STI management in Abuja, Nigeria. Afr Health Sci. 2010.
16. Cremers AL, Alege A, Nelissen HE, et al. Patients’ and healthcare providers’ perceptions and practices regarding hypertension, pharmacy-based care, and mHealth in Lagos, Nigeria: a mixed methods study. J Hypertens. 2019;37(2):389–397. doi:10.1097/HJH.0000000000001877
17. Osamor P, BE O. Factors associated with treatment compliance in hypertensives in South West Nigeria. J Heal Popul Nat. 2011.
18. Dzudie A, Ojji D, Anisiuba BC, et al. Development of the roadmap and guidelines for the prevention and management of high blood pressure in Africa: proceedings of the PASCAR: hypertension task force meeting: nairobi, Kenya, 27 October 2014. Cardiovasc J Afr. 2014.
19. Piper MA, Evans CV, Burda BU, Smith N. Screening for high blood pressure in adults: a systematic evidence review for the U.S. preventive services task force. screen high blood press adults a system. Evid Rev US Prev Serv Task Force. 2014. 121. Available from. http://www.ncbi.nlm.nih.gov.proxy.med.sc.edu/books/NBK269495/%5Cnhttp://www.ncbi.nlm.nih.gov/pubmed/25632496.
20. World Health Organization. Prevention and Control of Noncommunicable Diseases: Guidelines for Primary Health Care in Low-Resource Settings. WHO Libr Cat Data; 2012.
21. Okubadejo NU, Ozoh OB, Ojo OO, et al. Prevalence of hypertension and blood pressure profile amongst urban-dwelling adults in Nigeria: a comparative analysis based on recent guideline recommendations. Clin Hypertens. 2019;25(1). doi:10.1186/s40885-019-0112-1.
22. Chiolero A, Paradis G, Paccaud F. The pseudo-high-risk prevention strategy. Int J Epidemiol. 2015;44(5):1469–1473. doi:10.1093/ije/dyv102
23. Cherie A, Mitkie G, Ismail S, Berhane Y. Perceived sufficiency and usefulness of IEC materials and methods related to HIV/AIDS among high school youth in Addis Ababa, Ethiopia. Afr J Reprod Health. 2005;9(1):66–77. doi:10.2307/3583161
24. World Health Organization International Society of Hypertension Writing Group. World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;2003.
25. Sanchez-Rangel E, Inzucchi SE. Metformin: clinical use in type 2 diabetes. Diabetologia. 2017;60(9):1586–1593. doi:10.1007/s00125-017-4336-x
26. Mosenzon O, Pollack R, Raz I. Treatment of Type. Vol. 2. Diabetes: From guidelines to position statements and back recommendations of the Israel National Diabetes Council. Diabetes Care; 2016.
27. Mancia G, Fagard R, Narkiewicz K, et al. ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;2013.
28. Olowofela A, Isah A. Antihypertensive medicines prescriptions before and after the Nigeria hypertension society guidelines and prescriber’s awareness of the guideline. Niger Med J. 2017;58(3):107. doi:10.4103/nmj.NMJ_131_16
29. Chou CC, Lee MS, Ke CH, Chung MH. Prescription patterns of hypertension - National Health Insurance in Taiwan. J Chinese Med Assoc. 2004;67(3):123–130.
30. Mori H, Ukai H, Yamamoto H, et al. Current status fo antihypertensive prescription and associated blood pressure control in Japan. Hypertens Res. 2006;29(3):143–151. doi:10.1291/hypres.29.143
31. Adigun AQ, Ishola DA, Akintomide AO, Ajayi AAL. Shifting trends in the pharmacologic treatment of hypertension in a Nigerian tertiary hospital: a real-world evaluation of the efficacy, safety, rationality and pharmaco-economics of old and newer antihypertensive drugs. J Hum Hypertens. 2003;17(4):277–285. doi:10.1038/sj.jhh.1001538
32. Wassertheil-Smoller S, Psaty B, Greenland P, et al. Association between cardiovascular outcomes and antihypertensive drug treatment in older women. J Am Med Assoc. 2004.
33. Webb AJS, Rothwell PM. Effect of dose and combination of antihypertensives on interindividual blood pressure variability: a systematic review. Stroke. 2011;42(10):2860–2865. doi:10.1161/STROKEAHA.110.611566
34. Jarari N, Rao N, Peela JR, et al. A review on prescribing patterns of antihypertensive drugs. Clin Hypertens. 2015;22(1). doi:10.1186/s40885-016-0042-0.
35. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V. The indian diabetes prevention programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia. 2006;49(2):289–297. doi:10.1007/s00125-005-0097-z
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
